ABSTRACT
Objective:
To evaluate the efficacy of tranexamic acid in reducing blood loss in total knee arthroplasty by examining the existing literature.
Method:
This literature review investigated the use of tranexamic acid in knee arthroplasty. The search was performed in the Pubmed, Science Direct, Google Scholar, and Lilacs databases over a 20-year period using the keywords: “knee arthroplasty, tranexamic acid, and efficacy”. Only randomized clinical trials published between 2000 and 2016 in English, Spanish, or Portuguese were accepted, and only trials which scored above 3 on the Jadad scale were selected.
Results:
A total of 7 randomized clinical trials met the inclusion criteria, with a sample of 948 patients.
Conclusion:
The use of tranexamic acid in total knee arthroplasty (unilateral or bilateral) reduces perioperative and postoperative blood loss more than other available antifibrinolytics. With this reduction in total blood loss and the need for blood transfusions without any increase in side effects, the use of tranexamic acid can be considered safe and effective in controlling bleeding after knee arthroplasties. Level of Evidence II; Systematic review.
Keywords: Tranexamic acid; Arthroplasty, replacement, knee; Efficacy; Bleeding
RESUMO
Objetivo:
Avaliar a eficácia do ácido tranexâmico na redução da perda sanguínea em artroplastia total de joelho com relação à literatura existente.
Método:
O presente artigo é uma revisão da literatura a respeito da utilização do ácido tranexâmico nas artroplastias de joelho. A busca foi realizada nas bases de dados do Pubmed, Science Direct, Google Scholar e Lilacs com os descritores: “knee arthroplasty”, “tranexamic acid”, and “efficacy”, ao longo de 20 anos. Foram aceitos apenas ensaios clínicos randomizados, publicados entre o período de 2000 e 2016, nos idiomas inglês, espanhol e português. Somente os ensaios graduados acima de três pela escala de Jadad foram selecionados.
Resultados:
No total, sete ensaios clínicos randomizados satisfizeram os critérios de inclusão, com uma amostra de 948 pacientes.
Conclusão:
O uso do ácido tranexâmico na artroplastia total do joelho, tanto uni quanto bilateral, reduz a perda de sangue no peri e no pós-operatório em comparação com outros antifibrinolíticos usados. Com a redução da perda total de sangue e da necessidade de transfusões sanguíneas, sem qualquer aumento dos efeitos colaterais, a utilização do uso do ácido tranexâmico pode ser considerada segura e eficaz no controle do sangramento depois de artroplastias do joelho. Nível de Evidência II; Revisão sistemática.
Descritores: Ácido tranexâmico, Artroplastia do joelho, Eficácia, Sangramento
INTRODUCTION
Total knee arthroplasty (TKA) is a procedure which is subject to a series of postoperative complications; excessive blood loss is one of the main complications in the intraoperative and immediate postoperative period, and is related to prolonged hospital stay, increased hospitalization costs, and possible patient dissatisfaction. 1 Blood loss in TKA may vary from 800 ml to 1800 ml, and 10-38% of patients may require blood transfusions. 2
Even when tourniquets are used in TKA, there is considerable bleeding and this procedure may even be considered controversial. 3 Zhang et al. 4 demonstrated that when the tourniquet is released, fibronolysis is activated at the site, increasing blood loss. 2
Alternatives are continuously being assessed to minimize intraoperative and postoperative bleeding as well as complications. These include the use of tranexamic acid (TA), epinephrine, fibrin glue, Floseal hemostatic matrix, and transfusion. TA is gaining wide attention from surgeons because of its low cost, easy access and use, and is a medication which is widely known in the literature. 5 Considering this scenario, studies on the clinical effectiveness of TA in reducing blood loss during TKA are extremely important, since there is no consensus regarding the best application protocol or dosage in the current literature. 6
TA, which is a synthetic antifibrinolytic agent, contains the trans isomer of 4-amino-carboxylic methyl cyclohexane (Transamin), a synthetic derivative of the amino acid lysine, 7 , 8 which acts through competition to inhibit the activation of plasminogen to plasmin. This formula has a strong attraction to the site where lysine connects to the plasminogen and plasmin, thus inhibiting the activation and competing action of plasmin. Its action is primarily based on slowing down the fibrinolytic process (it is a potent inhibitor of the fibrinolytic action of plasmin) after clot formation, extending the time of dissolution of the fibrin network, thus preserving the clot and not resulting in the activation of the coagulation cascade. These properties increase the efficiency of the hemostatic substance, reducing the intensity and the risks of bleeding in surgical procedures, trauma and diseases where bleeding is likely. 7 , 9 TA has rapid absorption of approximately 90% of an intravenous dose excreted in the urine in 24 hours, a plasma half-life of approximately 2 hours, and therapeutic levels maintained for 6-8 hours. 5 , 10
Many techniques have been proposed to minimize blood loss and the need for blood transfusions in TKA, and this review consequently analyzes the effectiveness of TA in reducing blood loss in TKA and compares it with other methods presented in the literature.
METHODS
This systematic review was performed according to the PRISMA Statement protocol 11 to select scientific articles analyzing the effectiveness of TA in primary knee arthroplasty. The search was performed in the Pubmed, Medline, and Lilacs databases using the keywords “knee arthroplasty, “tranexamic acid,” and “efficacy” over a 20-year period. Only randomized clinical trials in English, Spanish, or Portuguese were accepted. The pre-selected trials were graded according to the Jadad scale 9 and only trials with scores over three were selected. Since this is a review article, the institutional review board approval for clinical studies was not necessary.
RESULTS
Using the keywords “knee arthroplasty,” “tranexamic acid,” and “efficacy,” we obtained 31 articles from Pubmed, 27 articles from Medline, and only 1 article from Lilacs, with a total of 59 articles to be reviewed, as shown in Figure 1. After excluding duplicate articles, we were left with 7 articles from Pubmed and Medline, and none from Lilacs. (Table 1) The other articles were excluded because they did not meet the pre-established inclusion criteria, i.e., a score above three on the Jadad scale. The selected studies were summarized and are shown in Table 2, while the type of intervention as well as the dosage used in the studies are shown in Table 3.
Figure 1. Flowchart of results.
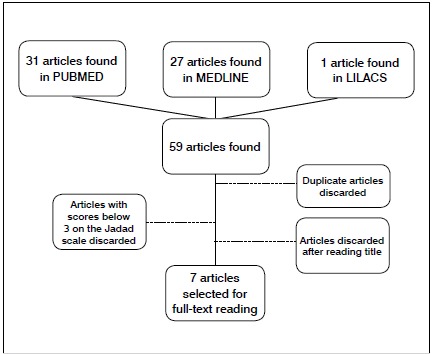
Table 1. Studies included in the review.
| Author and Year of Publication | Location | Type of Study | Sample |
|---|---|---|---|
| Pachauri et al., 8 2013 | Lucknow, India | Randomized clinical trial | 99 |
| Aguilera et al., 12 2013 | Barcelona, Spain | Randomized clinical trial | 172 |
| Kim et al., 13 2014 | Gyeonggido, Korea | Randomized clinical trial | 326 |
| Wong et al., 14 2010 | Toronto, Canada | Randomized clinical trial | 124 |
| Roy et al., 15 2012 | New Delhi, India | Randomized clinical trial | 50 |
| Kankar et al., 16 2009 | New Delhi, India | Randomized clinical trial | 50 |
| Camarasa et al., 17 2006 | Barcelona, Spain | Randomized clinical trial | 127 |
Table 2. Table summarizing the results of the studies included in the review.
| Author | Procedure | Type of intervention | Results |
| Pachauri et al., 8 2013 | Total knee arthroplasty | Tranexamic acid | Reduction in hemoglobin drop |
| Aguilera et al., 12 2013 | Total knee arthroplasty | Fibrin glue, fibrinogen with thrombin, intravenous tranexamic acid | Less blood loss when used tranexamic acid used |
| Kim et al., 13 2014 | Total knee arthroplasty, bilateral and unilateral | Tranexamic acid | Reduction in total blood loss when tranexamic acid used, reduction in rate of blood transfusion varies according to procedure performed |
| Wong et al., 14 2010 | Total knee arthroplasty | Tranexamic acid | Reduction in postoperative hemorrhage |
| Roy et al., 15 2012 | Total knee arthroplasty, unilateral | Tranexamic acid | Reduction in blood transfusion when tranexamic acid used |
| Kankar et al., 16 2009 | Total knee arthroplasty, bilateral and unilateral | Tranexamic acid | Reduction in total blood loss and blood transfusion rate when tranexamic acid used |
| Camarasa et al., 17 2006 | Total knee arthroplasty, unilateral | Tranexamic acid | Reduction in total blood loss and blood transfusion |
Table 3. Tranexamic acid dose and method of application.
| Author and Year of Publication | Type of intervention |
|---|---|
| Pachauri et al., 8 2013 | 2 doses of tranexamic acid, injection, first dose one hour post-procedure and six hours post-procedure |
| Aguilera et al., 12 2013 | Fibrin glue, fibrinogen with troponin, intravenous tranexamic acid |
| Kim et al., 13 2014 | More than one dose (10 mg.kg-1) of tranexamic acid before deflation of the tourniquet |
| Wong et al., 14 2010 | Tranexamic acid 1.5 to 3.0g applied in the joint for five minutes at the end of surgery |
| Roy et al., 15 2012 | Tranexamic acid 5ml, applied in the joint after the procedure |
| Kankar et al., 16 2009 | Tranexamic acid 10 mg.kg-1 applied shortly before inflation of the tourniquet, followed by 1 mg.kg-1 until the end of the procedure |
| Camarasa et al., 17 2006 | Intravenous tranexamic acid 10 mg.kg-1 applied shortly before deflation of the tourniquet and three hours later, or use of epsilon aminocaproic acid 100 mg.kg-1 |
The study by Aguilera et al. 12 described a randomized clinical trial (RCT) with 166 patients, who were separated into four groups by use of fibrin glue, fibrinogen with troponin, and intravenous tranexamic acid (IVTA), and the last group without any hemostatic mechanism (control). These authors concluded at the end of the study that IVTA can reduce blood loss in the postoperative period.
The study by Pachauri et al. 8 used a RCT with 99 patients receiving two doses of IVTA: the first applied one hour before incision and the second applied six hours after wound closure. After reviewing the results, Pachauri et al. 8 concluded that IVTA can be regarded as an effective method to control and minimize blood loss in TKA.
Kim et al. 13 performed a RCT with 326 patients: one group undergoing unilateral hip arthroplasty received more than one dose (10 mg/kg) IVTA before deflation of the tourniquet during surgery and again three hours after surgery, and a second group which underwent bilateral arthroplasty received more than one dose (10 mg/kg) before deflation of the tourniquet. This study concluded that the use of IVTA significantly reduced blood loss, but the transfusion rate may vary depending on whether the procedure is unilateral or total arthroplasty.
Wong et al. 14 published a study based on a RCT with 124 patients who received 1.5 or 3.0g of TA in 100ml of saline solution or an equivalent volume of placebo applied in the joint at the end of the surgery. They concluded that the use of TA reduces bleeding and increases hemoglobin levels after the procedure compared with the placebo.
Roy et al. 15 conducted a RCT with 50 patients in two groups: the first group received TA topically applied to the joint through infusion via suction drain after skin closure, and the second group (control) received intra-articular application of saline as a placebo. After analysis of the results, the authors concluded that TA reduced postoperative bleeding by almost half in patients undergoing TKA, reducing the need for blood transfusion in these patients.
Kakar et al. 16 conducted a RCT with 50 patients divided into four groups according to procedure, with bilateral and unilateral hip arthroplasty, and their respective control groups. A test dose of 1 ml was used, then a dose of 10 mg.kg-1 IV followed by an infusion of 1 mg.kg-11hr-1 of TA after skin closure. The control groups received an equivalent amount of saline. Kakar et al. 16 concluded that the use of TA significantly reduced blood loss when compared with the control groups.
In 2006, Camarasa et al. 17 conducted a RCT with 127 patients divided into two groups, one using IVTA shortly before deflating the tourniquet and three hours after the end of the procedure in the first group, and a control group, which received epsilon aminocaproic acid (EACA). In the conclusion of the article, these authors described a significant reduction in blood loss when antifibrinolytic agents were used in patients undergoing TKA, along with a reduction in the number of blood transfusions.
DISCUSSION
In previous reviews, Kim et al. 13 found 28 RCTs, Zhang et al. 4 reviewed 15 RCTs with a total of 842 patients, and Panteli et al. 18 found 7 articles in their review. The present review, which includes seven articles analyzing a total sample of 948 patients, also demonstrated the positive effects in reducing bleeding in TKA, decreased the need for blood transfusions, and low rates of complications when using tranexamic acid.
Aguilera et al. 12 analyzed 172 adult patients undergoing TKA for the first time. Their study investigated the efficacy of IVTA and fibrin glue (FG), comparing two types of FG with TA. The first group used FG from the Catalonia tissue bank, the second group used Tissucol (fibrinogen, aprotinin, and thrombin; Baxter AG, Vienna, Austria), a third group used TA, and a fourth group was a control. The results of this study showed lower blood loss in the group which used TA as hemostasis than in the groups that used the two types of FG and the control. No complications were reported from the use of hemostatic agents. The numbers of patients in each group were small in this study, which may have influenced the results observed.
Pachauri et al. 8 conducted a RCT with a total of 99 patients to evaluate the efficacy of TA in reducing intraoperative and postoperative bleeding in knee arthroplasties, and concluded that there was a significant reduction in hemoglobin drop in these patients.
In 2013, Kim et al. 13 performed another RCT to analyze the efficacy of TA in reducing blood loss and transfusion rates in unilateral TKA (uTKA) and bilateral TKA (bTKA). They included 180 patients who underwent uTKA and 146 patients who underwent bTKA. The results showed that TA use decreased the total blood loss, but its effects on transfusion rate may vary; the transfusion rate decreased when TA was used during bTKA, but there was no effect in uTKA.
Like Kim et al., 13 Kakar et al. 16 conducted a similar study, but with 24 patients who underwent uTKA and 26 patients who underwent bTKA. This study also found reduction in blood loss in both groups, although this reduction was more significant in patients who underwent bTKA. The authors also concluded that the use of TA led to a reduction in postoperative blood transfusions in both groups. This aspect differs from the conclusion by Kim et al., 13 which only demonstrated this reduction in patients who underwent the bilateral procedure. This divergence may be related to sample size. The protocol for application and dosage of TA also differed significantly between the studies. Other studies included in this review with similar results corroborated the findings of Kakar et al. 16
The analysis conducted by Roy et al. 15 involving 50 patients who underwent uTKA evaluated the efficacy of topical intra-articular TA in reducing blood loss during the postoperative period when compared with the control group. Roy et al. 15 found a similar reduction in blood transfusion in patients who underwent uTKAu, like Kakar et al. 16 The parameters used in this analysis were drop in hemoglobin and hematocrit. The results showed that the control group received six times more blood transfusions than the group that received TA.
Like Kakar et al., 16 Kim et al., 13 and Roy et al., 15 Camarasa et al., 17 obtained similar results. Based on a study with 127 patients, Camarasa et al. 17 evaluated the efficacy of fibrinolytics during treatment, in this case TA, to reduce perioperative blood loss during uTKA, and concluded that antifibrinolytics significantly decrease blood loss in patients undergoing TKA, which is reflected in a reduced number of blood transfusions.
In a study of 124 patients undergoing TKA, Wong et al. 14 analyzed topical use of TA directly in the knee joint, and demonstrated that topical application of TA can reduce postoperative hemorrhage by approximately 20-25%.
The limitations of this review include a wide divergence of protocols of use, dose, and time of administration of TA. A small number of studies were used, because of the design (RCT) and the use of this medication in only TKA. The total number of patients analyzed was suitable for a review study. Patient follow-up in the studies evaluated was also short, and new RCTs with longer follow-up are necessary; these should investigate the occult bleeding rate, as well as the occurrence of late complications such as deep venous thrombosis (DVT) and pulmonary embolism (PE). 19
The studies found did not permit a conclusion as to whether intravenous application is better than topical in terms of effectiveness. The choice between the two methods can be based on the surgeon’s preference, considering that the rate of complications did not increase when IVTA was used in comparison with topical application. The main complications such as DVT, pulmonary embolism, stroke, or acute myocardial infarction are not greater with IVTA than with topical use of this medication, and adverse effects also are not more likely. As a result, this review and others found in the literature 2 - 4 , 20 , 21 allow us to conclude that TA is an effective medication for controlling bleeding in knee arthroplasty procedures, regardless of how it is applied.
CONCLUSION
After analysis and comparison of the studies included in this review, we can conclude that the use of tranexamic acid in total knee arthroplasty (whether unilateral or bilateral) significantly reduces blood loss in the perioperative and postoperative periods when compared to other antifibrinolytic agents, and no difference was seen between intravenous or topical application. Because of this reduction in total blood loss and the reduced rate of hemoglobin and hematocrit as well as blood transfusion, and no increase in adverse effects, TA can be considered safe to use. The use of TA as a hemostasis mechanism can reduce costs, decrease hospitalization time, and avoid the need for blood transfusions.
Footnotes
Work conducted at the Center for Studies in Orthopedics and Traumatology at the Clínica Ortopédica Traumatológica (CEOT COT), João das Botas, 28, Canela, Salvador, BA, Brazil.
REFERENCES
- 1.Marra F, Rosso F, Bruzzone M, Bonasia DE, Dettoni F, Rossi R. Use of tranexamic acid in total knee arthroplasty. Joints. 2017;4(4):202–213. doi: 10.11138/jts/2016.4.4.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen T-P, Chen Y-M, Jiao J-B, Wang Y-F, Qian L-G, Guo Z. Comparison of the effectiveness and safety of topical versus intravenous tranexamic acid in primary total knee arthroplasty a meta-analysis of randomized controlled trials. J Orthop Surg. 2017;12(1):11–11. doi: 10.1186/s13018-017-0512-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Z, Shen X. The efficacy of combined intra-articular and intravenous tranexamic acid for blood loss in primary total knee arthroplasty A meta-analysis. Medicine (Baltimore) 2017;96(42):e8123. doi: 10.1097/MD.0000000000008123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang H, Chen J, Chen F, Que W. The effect of tranexamic acid on blood loss and use of blood products in total knee arthroplasty a meta-analysis. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2012;20(9):1742–1752. doi: 10.1007/s00167-011-1754-z. [DOI] [PubMed] [Google Scholar]
- 5.Kim TK, Chang CB, Koh IJ. Practical issues for the use of tranexamic acid in total knee arthroplasty a systematic review. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2014;22(8):1849–1858. doi: 10.1007/s00167-013-2487-y. [DOI] [PubMed] [Google Scholar]
- 6.Fu Y, Shi Z, Han B, Ye Y, You T, Jing J. Comparing efficacy and safety of 2 methods of tranexamic acid administration in reducing blood loss following total knee arthroplasty. Medicine (Baltimore) 2016;95(50):e5583. doi: 10.1097/MD.0000000000005583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunn CJ, Goa KL. Tranexamic acid a review of its use in surgery and other indications. Drugs. 1999;57(6):1005–1032. doi: 10.2165/00003495-199957060-00017. [DOI] [PubMed] [Google Scholar]
- 8.Pachauri A, Acharya KK, Tiwari AK. The effect of tranexamic acid on hemoglobin levels during total knee arthroplasty. Am J Ther. 2014;21(5):366–370. doi: 10.1097/MJT.0b013e318250f85a. [DOI] [PubMed] [Google Scholar]
- 9.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ. Assessing the quality of reports of randomized clinical trials is blinding necessary? Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 10.Hoylaerts M, Lijnen HR, Collen D. Studies on the mechanism of the antifibrinolytic action of tranexamic acid. Biochim Biophys Acta. 1981;673(1):75–85. [PubMed] [Google Scholar]
- 11.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions Explanation and Elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aguilera X, Martinez-Zapata MJ, Bosch A, Urrútia G, González JC, Jordan M. Efficacy and safety of fibrin glue and tranexamic acid to prevent postoperative blood loss in total knee arthroplasty a randomized controlled clinical trial. J Bone Joint Surg Am. 2013;95(22):2001–2007. doi: 10.2106/JBJS.L.01182. [DOI] [PubMed] [Google Scholar]
- 13.Kim TK, Chang CB, Kang YG, Seo ES, Lee JH, Yun JH. Clinical value of tranexamic acid in unilateral and simultaneous bilateral TKAs under a contemporary blood-saving protocol a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2014;22(8):1870–1878. doi: 10.1007/s00167-013-2492-1. [DOI] [PubMed] [Google Scholar]
- 14.Wong J, Abrishami A, El Beheiry H, Mahomed NN, Roderick Davey J, Gandhi R. Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty a randomized, controlled trial. J Bone Joint Surg Am. 2010;92(15):2503–2513. doi: 10.2106/JBJS.I.01518. [DOI] [PubMed] [Google Scholar]
- 15.Roy SP, Tanki UF, Dutta A, Jain SK, Nagi ON. Efficacy of intra-articular tranexamic acid in blood loss reduction following primary unilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2012;20(12):2494–2501. doi: 10.1007/s00167-012-1942-5. [DOI] [PubMed] [Google Scholar]
- 16.Kakar PN, Gupta N, Govil P, Shah V. Efficacy and Safety of Tranexamic Acid in Control of Bleeding Following TKR A randomized clinical trial. Indian J Anaesth. 2009;53(6):667–671. [PMC free article] [PubMed] [Google Scholar]
- 17.Camarasa MA, Ollé G, Serra-Prat M, Martín A, Sánchez M, Ricós P. Efficacy of aminocaproic, tranexamic acids in the control of bleeding during total knee replacement a randomized clinical trial. Br J Anaesth. 2006;96(5):576–582. doi: 10.1093/bja/ael057. [DOI] [PubMed] [Google Scholar]
- 18.Panteli M, Papakostidis C, Dahabreh Z, Giannoudis PV. Topical tranexamic acid in total knee replacement a systematic review and meta-analysis. The Knee. 2013;20(5):300–309. doi: 10.1016/j.knee.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Sadigursky D, Andion D, Boureau P, Ferreira MC, Carneiro RJF, Colavolpe PO. Effect Of Tranexamic Acid On Bleeding Control In Total Knee Arthroplasty. Acta Ortop Bras. 2016;24(3):131–136. doi: 10.1590/1413-785220162403149200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin C, Qi Y, Jie L, Li H-B, Zhao X-C, Qin L. Is combined topical with intravenous tranexamic acid superior than topical, intravenous tranexamic acid alone and control groups for blood loss controlling after total knee arthroplasty A meta-analysis. Medicine (Baltimore) 2016;95(51):e5344. doi: 10.1097/MD.0000000000005344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhao-Yu C, Yan G, Wei C, Yuejv L, Ying-Ze Z. Reduced blood loss after intra-articular tranexamic acid injection during total knee arthroplasty a meta-analysis of the literature. Knee Surg Sports Traumatol Arthrosc. 2014;22(12):3181–3190. doi: 10.1007/s00167-013-2814-3. [DOI] [PubMed] [Google Scholar]


