ABSTRACT
Objective:
To determine the reliability of two classification methods for wound hematoma after total hip replacement.
Methods:
This prospective cohort study was conducted on patients who underwent total hip replacement for hip osteoarthritis between May 2014 and April 2015. Epidemiological, surgical, and functional data were assessed. Two experienced hip surgeons evaluated 75 pictures of wounds taken 24 hours after surgery. Both evaluators performed the analysis twice, with a 6-week interval between the two analyses. The subjective classification was divided into four different categories describing the hematoma: absent, mild, moderate, and severe. The objective classification was derived from mathematical calculation of the area of the hematoma using a grid superimposed on a picture of the wound.
Results:
The subjective classification demonstrated an intra-rater agreement of more than 70%, while kappa values showed poor to moderate inter-rater reliability. The objective classification based on mathematical measurements of the hematoma area was more reliable, with good to excellent intra- and inter-rater reliability.
Conclusion:
The objective classification demonstrated higher intra- and inter-rater reliability. The classification methods used in this study could serve as a useful instrument for orthopedic surgeons, researchers, and health care providers when assessing wound hematomas after total hip replacement. Level of Evidence II; Development of diagnostic criteria on consecutive patients (with universally applied reference ‘‘gold’’ standard).
Keywords: Hip injuries; Arthroplasty, replacement, hip; Hematoma; Postoperative complications; Wound infection; Reliability of results
RESUMO
Objetivo:
Determinar a confiabilidade de dois métodos de classificação dos hematomas de ferida cirúrgica após artroplastia total do quadril.
Métodos:
Este estudo prospectivo de coorte foi conduzido em pacientes com osteoartrose do quadril submetidos à artroplastia total do quadril entre maio de 2014 e abril de 2015. Foram analisados dados epidemiológicos, cirúrgicos e funcionais. Dois experientes cirurgiões de quadril avaliaram 75 fotografias de feridas obtidas 24 horas após a cirurgia. Ambos os avaliadores analisaram as fotografias duas vezes, em intervalo de seis semanas. A classificação subjetiva consistiu em quatro categorias descrevendo o hematoma: ausente, leve, moderado e grave. A classificação objetiva foi obtida pelo cálculo matemático da área do hematoma, sobrepondo-se uma retícula a cada fotografia de ferida.
Resultados:
A classificação subjetiva mostrou concordância intra-avaliador de mais de 70%, enquanto que os valores de kappa mostraram concordância inter-avaliador baixa a moderada. A classificação objetiva baseada em cálculo matemático da área do hematoma foi mais confiável, com excelente concordância intra e inter- avaliador.
Conclusão:
A classificação objetiva demonstrou melhor concordância intra e inter-avaliador. Os métodos de classificação usados neste estudo podem ser um instrumento útil para cirurgiões ortopedistas, pesquisadores e profissionais de saúde para avaliar hematomas de feridas cirúrgicas após artroplastia total de quadril. Nível de Evidência II; Desenvolvimento de critérios diagnósticos em pacientes consecutivos (com padrão de referência "ouro" aplicado).
Descritores: Lesões do quadril, Artroplastia de quadril, Hematoma, Complicações pós-operatórias, Infecção dos ferimentos, Confiabilidade dos Resultados
INTRODUCTION
Several factors are associated with hematoma formation after total hip replacement (THR). The administration of fresh-frozen plasma, vitamin K, perioperative anticoagulation, or hormonal therapy are independent predictors for hematoma formation. 1 The length of the incision and the skin blood flow are surgical parameters that could possibly influence the severity of soft tissue damage. 2 , 3 Most hematomas are small and do not cause additional complications. However, this postoperative complication increases the risk of surgical site infection, 4 , 5 which may require intravenous treatment with antibiotics and a prolonged hospital stay. Mortazavi et al. 1 found that 0.41% of the hematomas after THR required reoperation.
A clinically evident hematoma can be described as a condition presenting edema, ecchymosis, and serosanguinous wound drainage. 6 The causes of the hematoma should be investigated. Possible etiologies include the following: postoperative trauma, anticoagulation drug complications, or irritation of the iliopsoas tendon. 7 - 9 In more severe cases, hematomas can lead to vascular and neurological injuries. 10 , 11 Readmissions for hematoma surgical treatment negatively impact referral hospitals, increasing health care costs and patient morbidity. 12 - 14
Given that hematomas can lead to serious postoperative complications and considering its important role in patient recovery, it is crucial to have a classification system to define the severity and extent of postoperative hematomas following THR. The correct identification of a hematoma could provide an outline for proper therapeutic measures and serve as an instrument for optimizing communication between surgeons and health care providers. The goal of the current study was to compare two methods of hematoma classification (subjective and objective) after THR.
METHODS
This study was approved by the local Institutional Review Board under the protocol number CEP 1055. Between May 2014 and April 2015, 81 patients who had THR were included in this prospective cohort study. Informed consent was obtained from all patients. Patients were included if they presented primary or secondary hip osteoarthritis and had failed conservative treatment. Patients with anticoagulant disorders, previous orthopedic surgeries in the ipsilateral limb, and patients in whom a surgical incision greater than 20 cm was performed were excluded from this study. Epidemiological data collected included the following: body mass index (BMI), comorbidities such cardiovascular diseases (CVD) and diabetes mellitus (DM), preoperative etiology of hip osteoarthritis, and smoking. (Table 1)
Table 1. Baseline characteristics.
| Parameter | Participants (n = 75) |
| Mean age (SD) | 56.2 years (13.28 years) |
| Gender | 31 Males; 44 Females |
| Mean BMI (SD) | 27.54 Kg/m2 (4.87 Kg/m2) |
| Primary diagnosis | 5 RA; 22 ON; 48 OA |
| Incision length (SD) | 16.3 cm (2.02 cm) |
| Comorbidities | 17 AH; 8 DM |
| Smoking | 18 |
| Alcohol abuse | 10 |
RA, rheumatoid arthritis; ON, osteonecrosis of the femoral head; OA, osteoarthritis; AH, arterial hypertension; DM, diabetes mellitus; SD, standard deviation.
Surgery was performed through a direct lateral Hardinge approach. 15 A non-cemented porous titanium alloy coated with hydroxyapatite THR (MBA Targos, Groupe Lépine, Genay, France) was used. The same protocol for wound closure and dressing was followed in all cases. Closed suction drainage was used based on a subjective evaluation of bleeding at the end of the procedure. Additionally, the length of the surgical incision was recorded. Chemical prophylaxis for deep vein thrombosis consisted of Enoxaparin (40 mg) administered 12 hours after the procedure and continued for four weeks. The intraoperative bleeding control was achieved with biterminal electrocoagulation or manual compression. No additional drugs for bleeding control (epinephrine or tranexamic acid) were used. One day after the surgery, all patients were encouraged to perform assisted passive mobilization of the lower limb as a mechanical anti-thrombotic prophylaxis. The dressings were not changed before the hematoma evaluation.
One of the authors (LF), assisted by a nurse, inspected and took standardized pictures of 81 surgical wounds at 24 hours postoperatively in the Intensive Care Unit or infirmary beds. After dressing removal, the patients were positioned in lateral decubitus to allow full visualization of the thigh. Pictures were taken with the same digital camera (iPhone 4STM, 8-megapixel, Apple Inc., Cupertino, USA) one meter away from the patient, centered on the surgical incision, and with similar settings (zoom, brightness and luminosity).
All pictures were rated according to an objective and a subjective classification by an evaluator. To obtain an objective classification, the Adobe Photoshop CC 2015 software (Adobe Systems Inc., San Jose, USA) was used to draw a grid of 1 cm2 squares superimposed on the pictures. The grid was green in color to differentiate from the color of the skin or the hematoma (Figure 1A-B). This grid was then used to estimate the total area of the hematoma post-surgery. According to the rater, a 1 cm2 square was included in the calculation of total hematoma area when the hematoma filled 50% or more of the grid square. Squares that met inclusion criteria were then summed together to obtain total estimated area of the hematoma.
Figure 1. A) Wound hematoma 24 hours after THR. B) A 1 cm2 grid was superimposed on each picture for the objective classification of the hematoma.
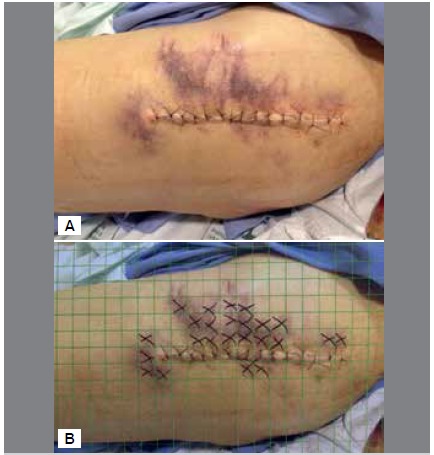
To obtain the real area of the hematoma (HA Real), the real length of the surgical incision was used as a proportional factor to relate the area of the pictured hematoma to the area of the real hematoma. Calculations of HA Real and HA Printed were as follows:
HA Real = HA Picture x (IL Real ÷ IL Picture)2
HA Real = Hematoma area in cm2
HA Printed = Hematoma area in the picture, which is the sum of all of the inclusion squares of 1 cm2.
IL Real = real surgical incision length
IL Printed = surgical incision length measured in the printed picture from the workbook
The following example shows how the formula was used for the calculation of the real hematoma area. Data were collected from a patient who presented a moderate hematoma 24 hours after the procedure. (Figure 1A) The real surgical incision length (IL Real) was 17 cm. In the printed version, under a 1 cm2 grid, the incision length was 8 cm. In this case, Rater 2 marked 24 inclusion squares. (Figure 1B)
HA Real = HA Picture x (IL Real ÷IL Picture)2
HA Real = 24 x (17 ÷ 8)2
HA Real = 108.38cm2
The subjective classification was based on an analysis of the pictures considering the intensity and extent of the hematoma. A PowerPoint presentation (Microsoft® PowerPoint 2011, Redmond, USA) was created, where all of the wound pictures were placed in sequential order. Raters were asked to estimate the hematoma in each picture according to the following descriptions: absent, mild, moderate, and severe.
Two authors (LE and HG), experienced hip surgeons, rated all pictures according to both classification methods. Evaluation of both classifications was performed separately. The order of the pictures was randomized between the PowerPoint presentation used for the subjective evaluation and the printed workbook used for the objective evaluation. After six weeks, raters again evaluated all pictures according to both methods. The raters were told to avoid returning to previous pictures once they started with measurements, and they were recommended to avoid interruptions. The mean period of time each rater took to complete each classification was also recorded.
Finally, all values obtained from the first hematoma evaluation performed by the first rater were used to correlate both the objective and subjective classifications.
Statistical analysis
SPSS software version 20.0 (SPSS, Chicago, USA) was used for the analyses. Categorical data were expressed as absolute numbers, continuous variables with normal distributions were expressed as the mean ± standard deviation (SD). A Chi-squared test or Fisher’s exact test were used to compare distributions. We considered P<0.05 to be statistically significant. A regression model was developed using the STATA version 14.2 (StataCorp, College Station, USA) software for correlating both the objective and subjective classifications. The minimal and maximal values are reported as range, and the confidence interval (CI) value used was 95%.
RESULTS
Out of the 81 pictures analyzed, 6 were excluded due to inadequate picture quality. A total of 75 patients were then evaluated, comprising 31 males (41.3%) and 44 females (58.7%) with a mean age of 56.2 years. The baseline characteristics of these patients are shown in Table 1.
In the objective classification, for the first measurement, Rater 1 found an area of hematoma ranging from 0 to 729 cm2 (mean = 177.8, median = 130.4), and Rater 2, an area ranging from 0 to 892 cm2 (mean = 152, median = 107). After six weeks, the values ranged from 0 to 833 cm2 (mean = 245.3, median = 130.4) and 0 to 879 cm2 (mean = 171.3, median = 102.8) for Rater 1 and Rater 2, respectively, as shown in Table 2. Rater 1 took 70 and 75 minutes for the first and second measurement phases, respectively, and Rater 2 took 65 and 50 minutes, respectively (P>0.05). The interclass correlation coefficient (ICC) revealed high intra-rater consistency. For Rater 1, the value of ICC was 0.89. The value of ICC for Rater 2 was 0.87. The inter-rater reliability ranged between 0.79 for the first measurement and 0.78 for the second measurement.
Table 2. The Intra- and Inter-Rater Reliability for the objective classification.
| First Evaluation | Rater 1 (cm2) | Rater 2 (cm2) | Inter-rater reliability ICC [95% CI] |
| Mean | 177.8 ± 185.8 | 152 ± 169 | 0.79 [0.69 - 0.86] |
| 95% CI | 135.1 - 220.5 | 113.2 - 190.9 | |
| Median | 130.4 | 107.7 | |
| Second Evaluation | Rater 1 (cm2)* | Rater 2 (cm2)* | Inter-rater reliability ICC [95% CI] |
| Mean | 245.3 ± 212.86 | 171.3 ± 191.1 | 0.78 [0.67 - 0.85] |
| CI 95% | 196.4 - 294.3 | 127.3 - 215.3 | |
| Median | 203.2 | 102.8 | |
| Intra-rater reliability ICC [95% CI] | 0.89 [0.83 - 0.93] | 0.87 [0.8 - 0.92] |
* Time between the first and second measurements was six weeks.
The intra-rater reliability in the subjective classification (Table 3) showed moderate agreement for both the first and second raters (kappa value of 0.69, P<0.001, and 0.56, P<0.001, respectively). Additionally, 80% and 72% of the grades were consistent between Rater 1 and 2, respectively. In the first measurement, the inter-rater reliability was low (kappa = 0.44, P<0.001). Here, the raters agreed on 65% of the cases. In the second evaluation, the raters agreed on 73% of their grades, and the inter-rater reliability was higher (kappa = 0.60, P<0.001). With respect to the first and the second measurement, the first rater took 13 and 25 minutes, respectively, and the second rater took 20 and 30 minutes, respectively (P>0.05).
Table 3. The Intra- and Inter-Rater Reliability for the subjective classification.
| Intra-Rater Reliability Rater 1 N (highest % of agreement) | Intra-Rater Reliability Rater 2 N (highest % of agreement) | Inter-Rater Reliability N, first measurement (highest % of agreement) | Inter-Rater Reliability N, second measurement (highest % of agreement) | |
| Absent | 9 (100) | 2 (50) | 3 (75)* | 4 (57.1)* |
| Mild | 28 (90.3) | 27 (75; 75) | 25 (69.4) | 25 (80.6) |
| Moderate | 20 (80) | 20 (83.3) | 18 (72) | 21 (87.5) |
| Severe | 3 (100) | 5 (100) | 3 (100) | 5 (100) |
| Kappa | 0.69 (P<0.001) | 0.56 (P<0.001) | 0.44 (P<0.001) | 0.6 (P<0.001) |
| Total % of agreement | 80 | 72 | 65 | 73 |
* Time between the first and second measurements was six weeks.
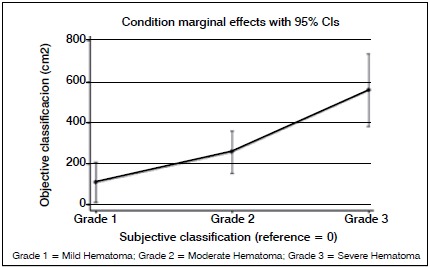
All values obtained from the first measurement of Rater 1 for both the objective and the subjective classifications were compared and are shown in Table 4 and Figure 2. A mild, moderate and severe hematoma were associated with a hematoma area of 107.6 cm2 (P=0.032), 256.8 cm2 (P<0.001) and 558.5 cm2 (P<0.001), respectively.
Table 4. Correlation between objective and subjective classifications.
| Subjective | Objective (cm2) | P value | 95% Confidence Interval |
| Mild Hematoma | 107.6 | 0.032 | 9.61 - 205.54 |
| Moderate Hematoma | 256.8 cm2 | < 0.001 | 154.07 - 359.52 |
| Severe Hematoma | 558.5 | < 0.001 | 382.29 - 734.64 |
Data obtained from Rater 1, first hematoma measurement.
Figure 2. Correlation between the subjective and the objective classifications.
DISCUSSION
The current study evaluated the reliability of two different classification methods for wound hematoma measurement in patients undergoing THR. The most important finding of this study was that good to excelent intra- and inter-rater agreement was found for the objective classification. To our knowledge, after a thorough review of the literature, this is the first study to propose a classification system on this topic. These classifications were designed to help orthopedic surgeons and health care providers standardize the evaluation of the intensity and extent of hematomas, especially with regards to scientific research.
Hematomas after THR can reach a substantial size, possibly due to injuries of the musculature during surgery. Damage to the gluteus medius tendon is a known complication of the lateral transgluteal approach. Additional muscle and ligament injuries can also occur depending on type of approach and technique, even those that are minimally invasive. 16
Hematomas following joint replacement can be a predictive risk factor for wound infection. 4 , 17 Wound complications may increase patients’ length of hospital stay and morbidity. 4 , 18 A high rate of hospital readmission following primary THR initially led to the creation of institutional programs based on preventive and educational measures, 19 . Hematomas account for 10% of the causes for readmission after THR. 12 Therefore, hematoma formation following THR can potentially lead to a significant economic burden. 19 , 20
A classification system for post-THR hematomas is needed and It could be used as a tool for other studies on hip surgery. We expect to facilitate the measurement and interpretation of hematomas in clinical practice and bring awareness to this topic, helping orthopedic surgeons and health care providers to better handle postoperative complications.
In the current study, a high rate of hematomas was found, which was possibly because the study site was a university hospital where residents perform surgeries under supervision. This might lead to longer surgeries, thereby increasing hematoma formation. The same approach, direct lateral, was performed in all cases. This approach may be related to greater damage to the soft tissue, and therefore, a higher rate of hematoma formation might occur.
The objective classification presented better intra- and inter-rater reliability and could be used as a tool for postoperative hematoma measurement. Previous studies described hematoma formation as a complication after THR; however, none of these studies described a method for the accurate clinical evaluation of the hematoma’s extent. 1 , 3 , 5 - 9 In our opinion, the method described in the current study is a reliable and easy method to measure the size of a hematoma, which can be particularly useful in research. Future studies should investigate if the proposed classification presents a correlation with complication rates or clinical parameters such as post-operative pain.
The subjective classification presents some advantages. It is faster, easier for the evaluator, and does not require the use of a computer program to add a grid to the picture. However, as it presented a lower kappa value, we believe the objective evaluation is more suitable for research. Nevertheless, the subjective evaluation can be used in day-to-day clinical settings because of its simplicity. When this classification was correlated with the objective one, a statistically significant relation was found. These findings might facilitate communication between surgeons and other healthcare providers, as well as draw attention to the need for a better understanding of the role of hematoma after joint replacement.
A professional camera could be used to obtain clearer pictures. However, a cellular phone camera was chosen because of its availability and easier reproducibility of the methods. Both of the reviewers were experienced hip surgeons, which could have led to higher inter-rater reliability. Future research can investigate if less experienced surgeons or other health professionals present the same scores. The pictures for the wound evaluation were taken 24 hours after the surgery. Since hematomas present a quick evolution, this early assessment could have underestimated its true size. The ideal moment for this evaluation remains to be determined.
CONCLUSIONS
This study proposes two classifications (subjective and objective) for the measurement of postoperative hematomas after THR. The objective classification demonstrated higher intra- and inter-rater reliability.
ACKNOWLEDGMENTS
We thank Fernando Rosas Brito for technical support, Marcos Antonio Almeida Santos for assistance with statistical analysis and Zachary Aman for editing contributions.
Footnotes
Work conducted at the Hip Group, Instituto de Ortopedia e Traumatologia, Hospital das Clinicas HCFMUSP, Faculdade de Medicina, Universidade de São Paulo, SP, Brazil.
REFERENCES
- 1.Mortazavi SM, Hansen P, Zmistowski B, Kane PW, Restrepo C, Parvizi J. Hematoma following primary total hip arthroplasty a grave complication. J Arthroplasty. 2013;28(3):498–503. doi: 10.1016/j.arth.2012.07.033. [DOI] [PubMed] [Google Scholar]
- 2.Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ. Comparison of primary total hip replacements performed with a standard incision or a mini incision. J Bone Joint Surg Am. 2004;86(7):1353–1358. doi: 10.2106/00004623-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Kiyama T, Naito M, Shitama H, Shinoda T, Maeyama A. Comparison of skin blood flow between mini- and standard-incision approaches during total hip arthroplasty. J Arthroplasty. 2008;23(7):1045–1049. doi: 10.1016/j.arth.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Saleh K, Olson M, Resig S, Bershadsky B, Kuskowski M, Gioe T. Predictors of wound infection in hip and knee joint replacement results from a 20 year surveillance program. J Orthop Res. 2002;20(3):506–515. doi: 10.1016/S0736-0266(01)00153-X. [DOI] [PubMed] [Google Scholar]
- 5.Cordero-Ampuero J, de Dios M. What are the risk factors for infection in hemiarthroplasties and total hip arthroplasties. Clin Orthop Relat Res. 2010;468(12):3268–3277. doi: 10.1007/s11999-010-1411-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neviaser AS, Chang C, Lyman S, Della Valle AG, Haas SB. High incidence of complications from enoxaparin treatment after arthroplasty. Clin Orthop Relat Res. 2010;468(1):115–119. doi: 10.1007/s11999-009-1020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pouliot MA, Lee KB, Goodman SB. Retroperitoneal hematoma: an unusual cause of pain after total hip arthroplasty. J Arthroplasty. 2009;24(7):1144.e9–1144.12. doi: 10.1016/j.arth.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Bartelt RB, Sierra RJ. Recurrent hematomas within the iliopsoas muscle caused by impingement after total hip arthroplasty. J Arthroplasty. 2011;26(4):665.e1–665.e5. doi: 10.1016/j.arth.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Hannon MG, Lamont JG. Compartment syndrome due to massive leg hematoma after primary total hip arthroplasty: a previously unreported complication of fondaparinux. J Arthroplasty. 2012;27(7):1414.e9–1414.e11. doi: 10.1016/j.arth.2011.10.032. [DOI] [PubMed] [Google Scholar]
- 10.Butt AJ, McCarthy T, Kelly IP, Glynn T, McCoy G. Sciatic nerve palsy secondary to postoperative haematoma in primary total hip replacement. J Bone Joint Surg Br. 2005;87(11):1465–1467. doi: 10.1302/0301-620X.87B11.16736. [DOI] [PubMed] [Google Scholar]
- 11.Khattar NK, Parry PV, Agarwal N, George HK, Kretz ES, Larkin TM. Total hip arthroplasty complicated by a gluteal hematoma resulting in acute foot drop. Orthopedics. 2016;39(2):e374–e376. doi: 10.3928/01477447-20160307-04. [DOI] [PubMed] [Google Scholar]
- 12.Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):464–470. doi: 10.1007/s11999-013-3121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clement RC, Derman PB, Graham DS, Speck RM, Flynn DN, Levin LS. Risk factors, causes, and the economic implications of unplanned readmissions following total hip arthroplasty. J Arthroplasty. 2013;28(8 Suppl):7–10. doi: 10.1016/j.arth.2013.04.055. [DOI] [PubMed] [Google Scholar]
- 14.Cullen C, Johnson DS, Cook G. Re-admission rates within 28 days of total hip replacement. Ann R Coll Surg Engl. 2006;88(5):475–478. doi: 10.1308/003588406X116909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64(1):17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 16.van Oldenrijk J, Hoogland PV, Tuijthof GJ, Corveleijn R, Noordenbos TW, Schafroth MU. Soft tissue damage after minimally invasive THA. Acta Orthop. 2010;81(6):696–702. doi: 10.3109/17453674.2010.537804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung EV, Sperling JW, Cofield RH. Infection associated with hematoma formation after shoulder arthroplasty. Clin Orthop Relat Res. 2008;466(6):1363–1367. doi: 10.1007/s11999-008-0226-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(1):33–38. doi: 10.2106/JBJS.F.00163. [DOI] [PubMed] [Google Scholar]
- 19.Jordan CJ, Goldstein RY, Michels RF, Hutzler L, Slover JD, Bosco 3rd JA. Comprehensive program reduces hospital readmission rates after total joint arthroplasty. Am J Orthop (Belle Mead NJ) 2012;41(11):E147–E151. [PubMed] [Google Scholar]
- 20.Merollini KM, Crawford RW, Whitehouse SL, Graves N. Surgical site infection prevention following total hip arthroplasty in Australia a cost-effectiveness analysis. Am J Infect Control. 2013;41(9):803–809. doi: 10.1016/j.ajic.2012.11.015. [DOI] [PubMed] [Google Scholar]


