Abstract
Background
Medicinal properties of the food species are one of the poorly documented and important areas of ethnopharmacology. The present survey quantitatively documented the medicinal foods prescribed by the non-institutionally trained siddha practitioners of Tiruvallur district of Tamil Nadu.
Methods
Field work was carried out between December 2014 and April 2017 using a questionnaire. The illnesses mentioned by the informants were grouped as illness categories on the basis of emic perceptions. Sufficiency of sampling of this survey was assessed by plotting the cumulative number of UR and Shannon-Wiener’s index. The indices such as informant consensus factor (FIC), Index of Agreement on Remedies (IAR), and Cultural Food Significance Index (CFSI) were calculated.
Results
This study documented 165 medicinal foods used by 82 non-institutionally trained siddha practitioners of Tiruvallur district, and 73.93% of these preparations were plant based. Among the animal taxa, 82.05% were represented by fish taxa. The illness category gastrointestinal ailments is the majorly cited illness category treated with plant-based formulations. The illness categories viz., gastrointestinal ailments, hemorrhoids, and neural ailments had high consensus under the group of plant-based medicinal foods. In animal-based medicinal foods, kapha ailments had gained 23.07% of UR. The illness categories such as bone fractures, male reproductive ailments, blood ailments, and anabolic had high FIC values.
Conclusions
Deeper studies on different dietary cultures of India may help to derive better interpretations on food-medicine continuum. This study identified some important claims such as the use of citron, pomegranate and Solanum americanum (gastrointestinal ailments), Abutilon indicum, onions and elephant foot yam (hemorrhoids), Boerhavia diffusa (urinary ailments), Moringa oleifera (anemia), Aloe vera (gynecological ailments), Eclipta prostrata (liver ailments), ivy gourd (diabetes), citron (hypertension), Centella asiatica (psychological ailments), spade nose shark (lactogogue), reticulate whipray (wheezing and bronchitis), Katelysia opima (impotence), Indian squid (anemia), and Indian oil sardine (anabolic). More studies on these claims will help identify novel functional foods to add to the field of medical nutrition therapy, with traditional brand identity. Robust studies on the documentation of the traditional knowledge on marine resources will yield a good database for various stakeholders and policy makers.
Electronic supplementary material
The online version of this article (10.1186/s13002-018-0240-9) contains supplementary material, which is available to authorized users.
Keywords: Medicinal foods, Functional foods, Traditional brand identity, Indian traditional medicine
Background
In many traditions, species which are used as medicine are also used as food and vice-versa; in many cases, ethnobiologists have documented this unclear delineation between food and medicine [1]. Ethnopharmacological surveys showed that the local people who gathered various wild species for food had knowledge about the health benefits of those species [2]. These health benefits go beyond from nutritional perspectives to health promoting phytochemicals [3] and many of them have been consumed by healthy people as a prophylactic measure. Local gastronomies are one of the important markers of regional identity and have been built upon various ecological, cultural, and religious beliefs [4]. Studies on the dietary patterns of a culture yield better clues on patterns of health and diseases observed in that population [5]. The importance of food-medicine interface in ethnopharmacology has been recognized for nearly 25 years [6, 7]. Many studies focused either on the dietary or pharmacological properties of the species and only limited studies addressed this food-medicine continuum [8].
India has a wide diversity of traditional cuisines; they contain whole grains, millets, wild gathered vegetables [9] and various spices for coloring, flavoring and preserving foods [10]. Besides cultural and religious beliefs, Indian cuisine was largely influenced by the principles of traditional medicinal systems. According to Indian philosophy, food was considered as the gift from god and it was classified into various categories [11]. The cuisine of Tamils is one of the important and oldest cuisine systems of India, and it is influenced largely by siddha system of traditional medicine [12]. The sangam (300BC–300AD) and post-sangam age (300–600AD) literatures such as tirukkuṟaḷ, pattuppāṭṭu, and ācārakkōvai describe various types foods and rules for eating. A classical siddha literature, patārtta kuṇa cintāmaṇi, describes the medicinal properties of various foods and drinks [13].
Diet diversification is one of the concepts to combat micronutrient malnutrition and to prevent chronic diseases [14, 15]. Various factors such as increasing healthcare costs, life expectancy, and desire for improving the quality of life among elders created a demand in global food industry to find novel foods with functional properties [16]. Globally, a significant increase in the consumption of functional foods for prevention and management of various chronic ailments was recorded. The market size of functional foods is expected to grow by 241 billion US$ by 2019. In India, the functional food industry is expected to grow by 20% and to reach a market size of 6.1 billion rupees by 2019–2020. Traditional diets are generally considered as holistic, healthy, and medicinal; thus, the demand and public interest on such foods are increasing rapidly, as in the case of herbal drugs [17]. Developing functional foods from traditional claims has been considered as an area for identifying novel functional foods [18]. In countries like India where traditional medicinal systems are looked with a nationalistic sentiment, the demand and the scope for functional foods with traditional brand identity are increasing. Besides these advantages, previous studies also demonstrated the adverse interactions of some functional foods with conventional therapies [19, 20]. In such scenario, it becomes important to document and inclusively evaluate the nutritional as well as functional properties of medicinal foods used locally and also to know the illnesses generally treated with these foods [8].
Siddha is one of the major traditional medical systems of India, which shares some commonalities with ayurveda. It has been majorly practiced in Tamil Nadu state and in its fringes; it has also been practiced in foreign countries such as Sri Lanka and Malaysia by Tamil people [21]. Previous studies indicated that the siddha literatures used in contemporary practice started from fourth to fifth century AD, though the practices emerged earlier [22]. The name siddha had also been coined recently in 1923 to delineate it from other systems of traditional medicines [23]. Literatures related to siddha are found exclusively in Tamil language as palm leaf manuscripts, and many of them remain undocumented. Institutional training on siddha system of medicine has been provided by the Government of India; however, the number of non-institutionally trained practitioners remains high [24]. Non-institutional training in siddha system of medicine is usually given from father to son and master to disciple forms [23]. This kind of knowledge transmission is usually done orally, and a lot of their recipes remain undocumented. Our previous survey in this area documented the medicinal plants used for the treatment of cardiometabolic diseases by non-institutionally trained siddha practitioners [25], and this survey aimed to document and analyze the medicinal foods prescribed by the non-institutionally trained siddha practitioners for prevention or management of various illnesses.
Methods
Study area
Tiruvallur district is located in the northern part of Tamil Nadu state between 12°15′–13°15′ N and 79°15′–80°20′ E, with an area of 3423 km2 (Fig. 1). The eastern part of this district is bounded by the Bay of Bengal, and the remaining parts are mostly flat and dry. The coastal part of this district occupies 498 km2 and has a costal line of 80 km for marine fisheries. The inland fresh water area is 750 km2, and brackish water area is 148 km2. This district has a forest cover of 197.8 km2 which occupies 5.8% of the total area; these forests mostly fall under the classes of dry thorn and dry evergreen. This district has nine taluks (sub-districts) and 14 revenue blocks. This district exhibits both urban and rural characteristics. Nearly 47% of the total human workforce deals with agriculture; this district is one of the fastest developing districts of Tamil Nadu in terms of industries. The average rainfall of the district is 1104 mm, out of which 52% is received from northeast monsoon and 41% is received from southwest monsoon. The State Government is providing siddha treatment in 12 hospitals with 37 institutionally trained siddha practitioners.
Fig. 1.
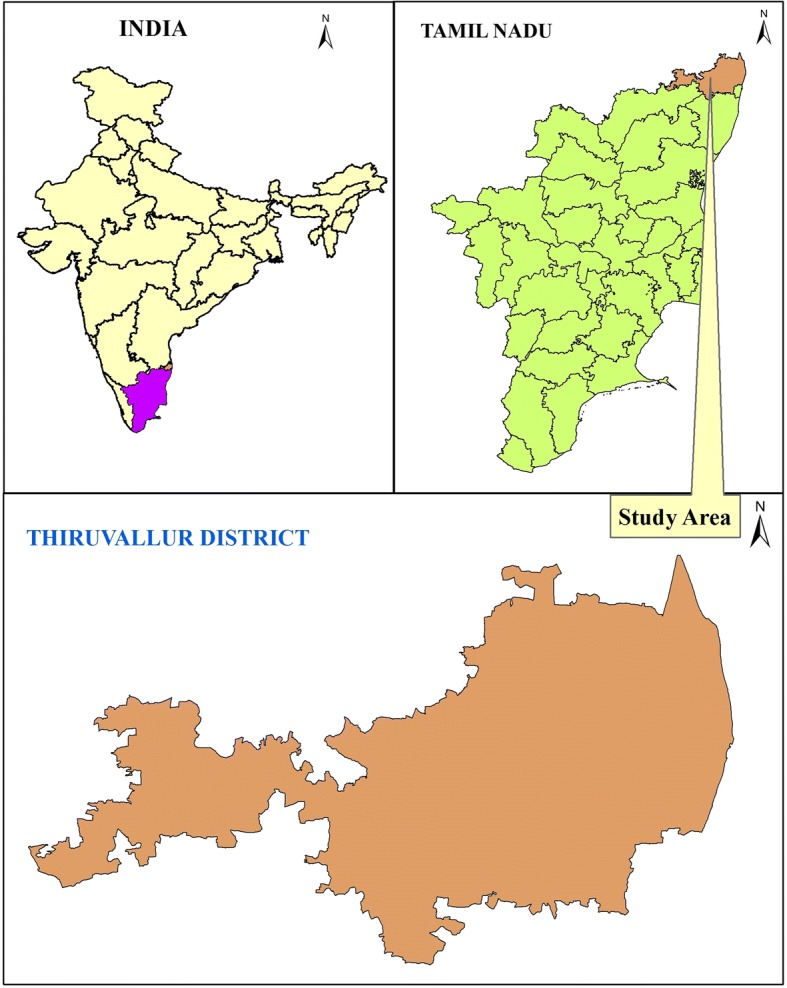
Map showing the location of the study area, Tiruvallur district in Tamil Nadu, India
Interviews
The local knowledge of non-institutionally trained siddha practitioners on medicinal foods was documented between December 2014 and April 2017 using a questionnaire. The interview protocols used for this survey were in accordance with the previously published methods [26–29] and also with the guidelines of ISE code of ethics for ethnobiological research [30]. This study focused on the local knowledge of siddha practitioners who learnt only through traditional methods of teaching (non-institutional training), practicing for a minimum of 5 years, and willing to share their knowledge. Snowball sampling method was used to recruit the informants, and the informants for this survey were recruited irrespective of age, gender, education, and nativity. The aim of this survey was explained to the participants in lay terms: one or two visits were taken to get familiarity, and the formal interviews were conducted after getting written informant consent to participate in this survey. By this way, the local knowledge of 82 non-institutionally trained siddha practitioners on medicinal foods was documented in this communication. The protocol used in this survey was approved by the Institutional Ethics Committee for Ethnobiological Research.
The questionnaire used for this survey consisted of two parts. In the first part, the data related to the demography of the informants such as age, gender, education, mode of learning traditional medicine, experience, nativity, residential area, and occupation were documented. In the second part of the questionnaire, the data regarding the medicinal foods that they are prescribing to their patients, the ingredients (plants/animals) used to prepare these foods, parts, mode of preparation, illnesses treated with these foods, dosage, and duration of consumption were documented. Under the ingredients section, the key medicinal taxa which were perceived to attribute the medicinal effect were also documented. Besides it, other details such as the perceived availability of resources (very common - rare), localization of the usage (ubiquity - rare), frequency of usage (frequent - no longer used), parts used, multi-functional usage (different eatable forms reported), taste score (best - terrible), and medicinal role (very high - not recognized) were also documented. The informants were taken to the fields from where they usually collected the samples, including local markets, and asked to show the specimens of the taxa that they mentioned either fresh or in dry condition. The interviews were conducted in the local language Tamil, and they were video-graphed. Questionnaires were cross-verified with the video-graphs for ambiguous entries. The data were translated into English in the laboratory. Equivalent English terms for the illnesses were fixed by correlating the Tamil terminologies and symptoms with the biomedical literature by consulting an institutionally trained siddha practitioner.
Specimens
Representative specimens of the fresh plants or crude drugs were collected, herborized, and stored at the museum of Entomology Research Institute, Loyola College, Chennai. The botanical authenticity of the plants was confirmed by the examination of the voucher specimens using local flora [31–34], and the valid names were confirmed with a website [35]. All the animals mentioned in this work were photographed, and their zoological names were confirmed by the Zoologist (MGP), who is one of the authors of this communication.
Quantification of the data
Medicinal plants/animals which were considered as key medicinal taxa by the informants were taken for the analysis. The illnesses mentioned by the informants were grouped as illness categories on the basis of emic perceptions. The illness category vadha ailments include the musculoskeletal disorders and kapha ailments include the pulmonary and respiratory diseases. The data were then converted into use reports (UR) and claims in accordance with our previous work. Briefly, UR can be described as “informant (i) prescribes a species (s) for a use category (u)” [36]; claims lack the informant (i) factor [37]. For example, if two informants mention a species for the treatment of an illness category, it yields two UR and a claim. Sufficiency of sampling of this survey was assessed by plotting the cumulative number of UR and Shannon Wiener’s index, which was calculated using PAST3 program.
Informant consensus over treating illnesses and on the taxa was assessed using informant consensus factor (FIC) and Index of Agreement on Remedies (IAR), respectively, [38] using the following formula.
FIC = (Nur − Nt)/(Nur − 1)
IAR = (nur − na)/(nr − 1)
where Nur is the number of UR for a particular illness category, Nt is the total number of taxa mentioned for that particular illness category, nur is the total number of UR registered for a taxon, and na is the number of illness categories that are treated with that taxon. These factors range from zero to one, where increasing values indicate high rate of informant consensus. Illness categories with high, average, and low consensus were calculated [39, 40]. Local uses of medicinal taxa having high IAR value and UR were compared with global usage pattern and scientific literature.
Humoral properties (cold and hot) of the medicinal plants and their uses in formal siddha medicine were taken from siddha materia medica [41–44]. If no report was available about a taxon, it was kept under the category “unspecified.” relative frequency of citation (RFC) on the basis of humors for each illness category was calculated using the following formula.
RFC = (number of UR for a humor/total number of UR) × 100
Cultural Food Significance Index (CFSI) of the key medicinal taxa was calculated in accordance with the method of Pieroni [45] with slight modifications (Table 1). For this calculation, key medicinal taxa with a minimum of two UR were considered. CFSI took seven indices into account, and it was calculated using the following formula.
Table 1.
Scores for Cultural Food Significance Index
| Indices | Attributes | Scores |
|---|---|---|
| Availability index (AI) | Availability | |
| Very common | 4.0 | |
| Common | 3.0 | |
| Middle | 2.0 | |
| Rare | 1.0 | |
| Localization of the use | ||
| Ubiquity | 0.0 | |
| Localized | − 0.5 | |
| Very localized | − 1.0 | |
| Frequency of utilization index (FUI) | > Once/week | 5.0 |
| Once/week | 4.0 | |
| Once/month | 3.0 | |
| > Once/year but < once/month | 2.0 | |
| Once/year | 1.0 | |
| No longer used during the past 30 years | 0.5 | |
| Part used index (PUI) | Whole aerial parts | 3.0 |
| Leaves with a few stems, whole aerial parts of very young plants | 2.0 | |
| Root/root stocks, bulbs, leaves, fruits | 1.5 | |
| Shoots | 1.25 | |
| Bark, younger part of roots, stems, leaf stalks, young whorls of leaves, seeds | 1.0 | |
| Younger part of shoots, buds, flowers, receptacles | 0.75 | |
| Multifunctional food use index (MFFI) | Chutney, dosa, gravy, sauce, salad | 1.5 |
| Jam, porridge, pickles, fried, syrups | 1.0 | |
| Soup, milk preparation | 0.75 | |
| Raw | 0.5 | |
| Taste Score Appreciation Index (TSAI) | Best | 10.0 |
| Very good | 9.0 | |
| Good | 7.5 | |
| Fair | 6.5 | |
| Poor | 5.5 | |
| Terrible | 4.0 | |
| Food Medicinal Role Index (FMRI) | IAR of the taxa > mean + SD | 5.0 |
| IAR of the taxa < mean + SD but IAR > mean − SD | 4.0 | |
| IAR < mean − SD | 3.0 | |
CFSI = QI) × AI) × FUI) × PUI) × MFFI) × TSAI) × FMRI × 10− 2
where Quotation index (QI) indicated the number of UR for a taxon. Availability index (AI) was obtained by subtracting scores of localization of the use from the scores of availability. Frequency of use index (FUI), part used index (PUI), multifunctional food use index (MFFI), Taste Score Appreciation Index (TSAI), and Food Medicinal Role Index (FMRI) were calculated as given in Table 1. In the case of FMRI, the taxa with IAR greater than mean plus standard deviation of the IAR of all taxa were given the highest score. The taxa with IAR value lower than mean plus standard deviation of the IAR were given the lowest score. Other taxa were given average FMRI score. For animal taxa, PUI was omitted from calculation.
Results
Demographic profile of the informants
Analysis of the informants’ demography indicated that the non-institutionally trained siddha tradition is a male dominant domain and a major portion of these practitioners had completed secondary or higher secondary schooling. Considerable portion (36.58%) of the practitioners had migrated to the study area from other districts. It also showed that major portion (71.94%) of practitioners was practicing in urban and semi-urban areas (Table 2).
Table 2.
Demographic profile of the informants interviewed in the survey (N = 82)
| Number | Percent | |
|---|---|---|
| Age | ||
| 35–40 | 7 | 8.53 |
| 41–50 | 44 | 53.65 |
| 51–60 | 26 | 31.70 |
| Above 60 | 5 | 6.09 |
| Gender | ||
| Male | 80 | 97.56 |
| Female | 2 | 2.43 |
| Education | ||
| Primary school | 5 | 6.09 |
| Secondary school | 20 | 24.39 |
| Higher secondary | 41 | 50.00 |
| Degree | 16 | 19.51 |
| Mode of learning | ||
| From family members | 13 | 15.85 |
| From traditional practitioners | 69 | 62.19 |
| Experience | ||
| 5 years | 1 | 1.21 |
| 6–20 years | 62 | 75.60 |
| 21–50 years | 19 | 23.17 |
| Nativity to the district | ||
| Native | 52 | 63.41 |
| Migrated | 30 | 36.58 |
| Residence | ||
| Urban | 35 | 42.68 |
| Semi-urban | 24 | 29.26 |
| Rural | 23 | 28.04 |
| Occupation | ||
| Full time practitioners | 82 | 100 |
Descriptive statistics of the medicinal foods
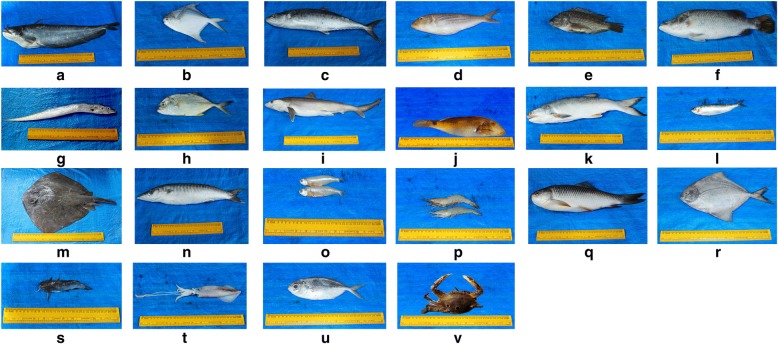
This study documented 165 medicinal foods used by the non-institutionally trained siddha practitioners of Tiruvallur district to treat various illnesses. Among them 73.93% were plant based, and 26.07% foods used animal taxa as the major key ingredients. To prepare these foods, 104 (72.72%) plant taxa and 39 (27.27%) animal taxa were used and major portion of the animals was represented by fish taxa. Sampling sufficiency analysis showed a clear asymptote of the curve which indicated the sufficiency of the sampling (Fig. 2). Analysis of the data yielded 588 UR and 381 claims. Plant-based formulations gained high number of UR (77.68%) and claims (76.64%). The plant and animal taxa cited by the non-institutionally trained siddha practitioners are given in Tables 3 and 4. The medicinal foods prescribed by the informants are given in Additional file 1: Table S1. The photographs of some animal taxa referred by the informants for the preparation of medicinal foods are given in Fig. 3.
Fig. 2.
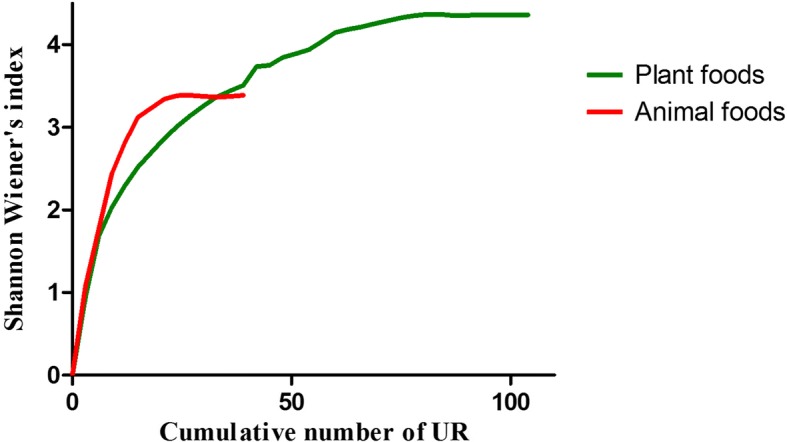
Assessing sampling sufficiency for the plant and animal species cited to prepare medicinal foods by the non-institutionally trained Siddha practitioners in Tiruvallur district using Species Accumulation Curve
Table 3.
List of plant taxa cited by the non-institutionally trained siddha practitioners of Tiruvallur district of Tamil Nadu for preparing medicinal foods
| S.No | Binomial name, Voucher number & Family | Vernacular name | Parts used | Humoral propertya | Reported pharmacological action in Siddhaa | Illnesses treated | Illnesses categories | IAR |
|---|---|---|---|---|---|---|---|---|
| 1. |
Abelmoschus esculentus (L.) Moench SE201 (Malvaceae) |
Veṇṭaikkāy | Tender fruits | Cold | Refrigerant, Aphrodisiac, Demulcent, Diuretic, Emollient, To treat diarrhea and dysentary | Diabetes (2), Coolant (1), Oligospermia (1) | Dia. (2), Coo. (1), Mal. (1) | 0.333 |
| 2. |
Abutilon indicum (Link) Sweet SE193 (Malvaceae) |
Tutti | Leaves | Cold | Demulcent, Tonic, Laxative, Diuretic, Sedative, To treat hemorrhoids, boils, gangrene and warts | Hemorrhoids (3) | Hem. (3) | 1.000 |
| 3. |
Acalypha indica L. SE188 (Euphorbiaceae) |
Kuppaimēṉi | Leaves | Hot | Anodyne, Anthelmintic, Cathartic, Diuretic, Emetic, Expectorant, Emmenagogue, To treat toothache, burns, organic poisons, stomachache, hemorrhoids, joint pain and bronchitis | Bronchitis (1), Hemorrhoids (2), Intestinal worms (1) | Hem. (2), Kap. (1), Gas. (1) | 0.333 |
| 4. |
Allium cepa L. SE170 (Amaryllidaceae) |
Veṅkāyam | Bulbs | Hot | Stimulant, Diuretic, Expectorant, Emmenagogue, Rubefacient, Demulcent, Aphrodisiac, To treat hemorrhoids, eczema, hypertension, mouth ulcers, polydipsia and diarrhea | Hemorroids (1), Bleeding through rectum (3), Oligospermia (2), Burning sensation (1) | Hem. (4), Mal. (2), Coo. (1) | 0.666 |
| 5. |
Allium sativum L. SE107 (Amaryllidaceae) |
Veḷḷaippūṇṭu | Bulbs | Hot | Carminative, Stomahic, Tonic, Alterative, Stimulant, Expectorant, Diuretic, Anthelmintic, To treat boils, cough, wheezing, intestinal worms and hemorrhoids | Indigestion (1), Dysmenorrhea (1), Diabetes (1), Heart ailments (1), Flatulance (1) | Gas. (2), Gyn. (1), Dia. (1), Hea. (1) | 0.250 |
| 6. |
Aloe vera (L.) Burm.f. SE108 (Asphodelaceae) |
Kaṟṟāḻai | Leaves | Cold | Tonic, Alterative, Purgative, Emmenagogue, To treat dermatological ailments, leprosy, hemorrhoids, anal fistula, urolithiasis | Obesity (1), Urolithiasis (1), Liver ailments (1), Dysmenorrhea (2), Metrorrhagia (1), Uteral ailments (1), Gastrointestinal ailments (1) | Gyn. (4), Obe. (1), Uri. (1), Liv. (1), Gas. (1) | 0.428 |
| 7. |
Alternanthera sessilis (L.) R.Br. ex DC. SE159 (Amaranthaceae) |
Poṉṉāṅkaṇṇi | Leaves | Cold | Alterative, Coolant, Good for eyes | Menstrual migraine (1), To increase memory and vision (1) | Gyn. (1), Psy. (1), Eye. (1) | 0.000 |
| 8. |
Amaranthus viridis L. SE117 (Amaranthaceae) |
Araikkīrai | Leaves | Hot | Stimulant, Aphrodisiac | Male infertility (1), Anemia (1), General weakness (2) | Wea. (2), Mal. (1), Blo. (1) | 0.333 |
| 9. |
Amorphophallus paeoniifolius (Dennst.) Nicolson SE113 (Araceae) |
Karuṇaikkiḻaṅku | Rhizomes | Cold | Alterative, Nutritive, Tonic, To treat pulmonary ailments, Hemorrhoids and anorexia | Hemorrhoids (3), Hypertension (1) | Hem. (3), Hpt. (1) | 0.666 |
| 10. |
Anacardium occidentale L. SE127 (Anacardiaceae) |
Muntiri | Seeds | Cold | Tonic, Aphrodisiac | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 11. |
Annona squamosa L. SE183 (Annonaceae) |
Cītāppaḻam | Fruits | Cold | Coolant | Coolant (1), Gastric ulcers (1) | Coo. (1), Gas. (1) | 0.000 |
| 12. |
Arachis hypogaea L. SE126 (Fabaceae) |
Vērkkaṭalai | Seeds | Hot | Nutrient, laxative, Emollient | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 13. |
Benincasa hispida (Thunb.) Cogn. SE200 (Cucurbitaceae) |
Veṇpūcaṇi | Tender fruits | Cold | Diuretic, Styptic, Tonic, Alterative, Nutrient, To treat dysuria, fever, dermatological ailments, leucorrhea, psychological ailments | Dysuria (1), To gain weight (1) | Uri. (1), Wea. (1) | 0.000 |
| 14. |
Beta vulgaris L. SE150 (Amaranthaceae) |
Pīṭrūṭ | Rhizomes | -- | -- | Anemia (2), Male infertility (1), Hypotension (1) | Blo. (2), Mal. (1), Hpo. (1) | 0.333 |
| 15. |
Boerhavia diffusa L. SE194 (Nyctaginaceae) |
Mūkkiraṭṭai | Leaves | Hot | Expectorant, Diuretic, Laxative, Coolant, Anthelmintic, Emetic | Dysuria (3) | Uri. (3) | 1.000 |
| 16. |
Borassus flabellifer L. SE168 (Arecaceae) |
Paṉai | Inflorescence | Cold | Coolant, Diuretic | Burning sensation (3), Jaundice (1) | Coo. (3), Jau. (1) | 0.666 |
| 17. |
Brassica oleracea var. gongylodes L. SE199 Brassicaceae |
Nūkkal | Stems | -- | -- | Diabetes (2) | Dia. (2) | 1.000 |
| 18. |
Cardiospermum halicacabum L. SE109 (Sapindaceae) |
Muṭakkottāṉ | Leaves | Hot | Diuretic, Laxative, Stomachic, Rubefacient, Antirheumatic, Nutritive, To treat musculo-skeletal and dermatological ailments | Rhinitis (1), Cough (1), Somatalgia (3) | Ana. (3), Kap. (2) | 0.750 |
| 19. |
Carica papaya L. SE182 (Caricaceae) |
Pappāḷi | Fruits | Hot | Laxative, Tonic, Diuretic, Lactogogue | Constipation (1), Lactogogue (1), Joint pain (1) | Gas. (1), Gyn. (1), Vad. (1) | 0.000 |
| 20. |
Cassia fistula L. SE197 (Fabaceae) |
Carakkoṉṟai | Flowers | Hot | Vermifuge, To treat leucorrhea, anemia, jaundice, dermatological infections and diabetes | Diabetes (1) | Dia. (1) | 0.000 |
| 21. |
Centella asiatica (L.) Urban SE157 (Apiaceae) |
Vallārai | Leaves | Cold | Alterative, Tonic, Diuretic, Stimulant, Emmenagogue, To treat fever, elephantiasis, scrotal swelling, Swollen lymph nodes, eczema, wounds and swellings | To strengthen memory (2), Hypothyroidism (1) | Psy. (2), Thy. (1) | 0.500 |
| 22. |
Cicer arietinum L. SE129 (Fabaceae) |
Koṇṭaikkaṭalai | Seeds | Cold | Antibilious, Diuretic, Aphrodisiac | General weakness (2), Fatigue (1), Menstrual cramps (1) | Wea. (2), Fat. (1), Gyn. (1) | 0.333 |
| 23. |
Cichorium intybus L. SE176 (Asteraceae) |
Kāciṉikkīrai | Leaves | -- | -- | Male infertility (1) | Mal. (1) | 0.000 |
| 24. |
Cissus quadrangularis L. SE137 (Vitaceae) |
Piraṇṭai | Stem | Hot | Alterative, Emmenagogue, Stomachic, To treat hemorrhoids, anorexia, ulcers, diarrhea and fatigue | Obesity (1), Gastric ulcers (1), Bone fractures (1), Hemorrhoids (3) | Hem. (3), Obe. (1), Gas. (1), Bon. (1) | 0.400 |
| 25. |
Citrullus lanatus (Thunb.) Matsum. & Nakai SE178 (Cucurbitaceae) |
Tarpūcaṇi | Fruits | Cold | Coolant, Diuretic | Hyperacidity (2), Dysuria (1) | Gas. (2), Uri. (1) | 0.500 |
| 26. |
Citrus limon (L.) Osbeck SE167 (Rutaceae) |
Elumiccai | Fruits | Hot | Carminative, Rubefacient, To treat fainting, nausea, polydipsia, psychological ailments, eye ailments | Indigestion (3), Constipation (1), Heart ailments (1), Acne (1), Diabetes (1), Arthritis (2), To increase vision (1), Hypothyroidism (1) | Gas. (4), Vad. (2), Hea. (1), Der. (1), Dia. (1), Eye. (1), Thy. (1) | 0.400 |
| 27. |
Citrus medica L. SE184 (Rutaceae) |
Nārattai | Fruits | Cold | Aromatic, Stomachic, Astringent, Sedative, Digestive, Good to treat hypertension | Hyperacidity (1), Heart ailments (2), Gastric ulcers (2), Hypertension (2), Anorexia (2), Dermatological ailments (1) | Gas. (5), Hea. (2), Hpt. (2), Der. (1) | 0.666 |
| 28. |
Citrus reticulata Blanco SE185 (Rutaceae) |
Ārañcu | Fruits | -- | -- | Heart ailments (1) | Hea. (1) | 0.000 |
| 29. |
Cleome gynandra L. SE190 (Cleomaceae) |
Nalla vēḷai | Leaves | Hot | Rubefacient, Anthelmintic, Antispasmodic, Carminative, Diaphoretic | Joint pain (1), Rhinitis (2), Fever (1), Heart ailments (1) | Kap. (2), Fev. (1), Vad. (1), Hea. (1) | 0.250 |
| 30. |
Coccinia grandis
(L.) Voigt SE147 (Cucurbitaceae) |
Kōvaikkāy | Tender fruits | Cold | Expectorant, Antispasmodic, Febrifuge, To treat anorexia, fever, bronchitis and eczema | Gastric ulcers (3), Mouth ulcers (2), Oliguria (1), Diabetes (5), Burning sensation (2), Bronchitis (1) | Gas. (5), Dia. (5), Coo. (2), Uri. (1), Kap. (1) | 0.692 |
| 31. |
Cocculus hirsutus (L.) Diels SE139 (Menispermaceae) |
Kaṭṭukkoṭi | Leaves | Hot | Alterative, Laxative, Demulcent, Coolant, To treat diarrhea, metrorrhagia, dysuria and gastric ulcers | Oligospermia (1), Coolant (1) | Mal. (1), Coo. (1) | 0.000 |
| 32. |
Cocos nucifera L. SE154 (Arecaceae) |
Tēṅkāy | Endosperm | Cold | Coolant, Aperient, Nutrient, Diuretic, To treat mouth ulcers | Male infertility (1), Hypotension (1), Gastric ulcers (1), Mouth ulcers (1) | Gas. (2), Mal. (1), Hpo. (1) | 0.333 |
| 33. |
Cucumis sativus L. SE174 (Cucurbitaceae) |
Veḷḷarikkāy | Tender fruits | Cold | Diuretic, Nutrient, Demulcent, Coolant | Hyperacidity (2) | Gas. (2) | 0.000 |
| 34. |
Cuminum cyminum L. SE134 (Apiaceae) |
Cīrakam | Seeds | Cold | Carminative, Stimulant, Stomachic, Astringent, To treat hypertension, liver ailments, urolithiasis, dysentery, wheezing, rhinitis, insomnia | Somatalgia (1), Anemia (1), Anorexia (1), Coolant (2), Hypertension (1), Gastric ulcers (2) | Gas. (3), Coo. (2), Ana. (1), Blo. (1), Hpt. (1) | 0.428 |
| 35. |
Daucus carota L. SE153 (Apiaceae) |
Kāraṭ | Rhizome | -- | -- | Male infertility (1), Hypotension (1), Bloating (1), Nausea (1) | Gas. (2), Mal. (1), Hpo. (1) | 0.333 |
| 36. |
Digera muricata (L.) Mart. SE192 (Amaranthaceae) |
Toyyakkīrai | Leaves | Cold | Coolant | Diarrhea (1), Dysentery (1) | Gas. (2) | 1.000 |
| 37. |
Echinochloa frumentacea Link SE123 (Poaceae) |
Kutiraivāli | Seeds | -- | -- | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 38. |
Eclipta prostrata (L.) L. SE177 (Asteraceae) |
Karicalāṅkaṇṇi | Leaves | Hot | Cholagogue, Tonic, Alterative, Emetic, Laxative, Deobstruent, Hepatoprotective, To treat throat ailments, jaundice, leprosy, ascites, anemia and toothache | To increase memory (1) and vision (1), Liver ailments (2), Anemia (2) | Liv. (2), Blo. (2), Psy. (1), Eye. (1) | 0.400 |
| 39. |
Eleusine coracana Gaertn. SE118 (Poaceae) |
Kēḻvaraku | Seeds | Cold | Nutrient, Astringent, To treat diabetes | General weakness (2), Fatigue (1), Diabetes (1), To strengthen memory (1), Anemia (2) | Wea. (2), Blo. (2), Fat. (1), Dia. (1), Psy. (1) | 0.333 |
| 40. |
Erythrina variegata L. SE138 (Fabaceae) |
Kalyāṇamuruṅkai | Leaves | Hot | Diuretic, Laxative, Emmenagogue, Lactogogue | Bronchitis (1) | Kap. (1) | 0.000 |
| 41. |
Ferula assa-foetida L. SE136 (Apiaceae) |
Peruṅkāyam | Resin | Hot | Stimulant, Carminative, Antispasmodic, Expectorant, Laxative, Anthelmintic, Diuretic, Aphrodisiac, Emmenagogue | Somatalgia (1) | Ana. (1) | 0.000 |
| 42. |
Ficus benghalensis L. SE142 (Moraceae) |
Āl | Fruits | Cold | Astringent, Tonic, Aphrodisiac | Oligospermia (1) | Mal. (1) | 0.000 |
| 43. |
Ficus racemosa L. SE140 (Moraceae) |
Atti | Fruits | Cold | Astringent, Laxative, Good to treat diarrhea, hemorrhoids and anemia | Oligospermia (1), Anemia (2), Male infertility (1), Constipation (1), Wheezing (1), Gastric ulcers (1), Hemorrhoids (1) | Mal. (2), Blo. (2), Gas. (2), Hem. (1), Kap. (1) | 0.428 |
| 44. |
Ficus religiosa L. SE141 (Moraceae) |
Aracu | Fruits | Cold | Laxative, Coolant | Oligospermia (1) | Mal. (1) | 0.000 |
| 45. |
Foeniculum vulgare Mill. SE114 (Apiaceae) |
Peruñcīrakam | Seeds | Hot | Carminative, Stomachic, To treat uteral ailments, fever, indigestion, bloating, cough, liver ailments, wheezing, rhinitis | Heart ailments (1) | Hea. (1) | 0.000 |
| 46. |
Garcinia gummi-gutta (L.) Roxb. SE101 (Clusiaceae) |
Koṭampuḷi | Fruits | Hot | Carminative, Digestive | Obesity (1) | Obe. (1) | 0.000 |
| 47. |
Gossypium spp. SE169 (Malvaceae) |
Parutti | Seeds | Hot | Laxative, Expectorant, Aphrodisiac | General weakness (1), Somatalgia (1) | Wea. (1), Ana. (1) | 0.000 |
| 48. |
Hibiscus cannabinus L. SE202 (Malvaceae) |
Puḷiccakīrai | Leaves | Hot | Emollient, Laxative, To treat anorexia and hypertension | Anorexia (1) | Gas. (1) | 0.000 |
| 49. |
Hibiscus rosa-sinensis L. SE102 (Malvaceae) |
Cemparattai | Flowers | Cold | Laxative, Aphrodisiac, Emmenagogue, Emollient, Demulcent, Coolant, To treat leucorrhea, metrorrhagia and hypertension | Male infertility (1), Heart ailments (2) | Hea. (2), Mal. (1) | 0.500 |
| 50. |
Hybanthus enneaspermus (G.Don) R.Br. ex Arn. SE162 (Violaceae) |
Oritaḻtāmarai | Flowers | Cold | Nutritive, Aphrodisiac | Oligospermia (1), Hypothyroidism (1) | Mal. (1), Hpo. (1) | 0.000 |
| 51. |
Ipomoea aquatica Forssk. SE191 (convolvulaceae) |
Vaḷḷaikkīrai | Leaves | Cold | Coolant, Lactogogue, Aphrodisiac, Antidiabetic | Mouth ulcers (1), Gastric ulcers (2), Oligospermia (2) | Gas. (3), Mal. (2) | 0.750 |
| 52. |
Lagenaria siceraria (Molina) Standl. SE104 (Cucurbitaceae) |
Curaikkāy | Tender fruits | Cold | Coolant, Diuretic, Nutritive, Antibilious | Obesity (1), Coolant (1), To strengthen memory (1), Swelling of the limbs (1), Dysuria (2) | Uri. (3), Obe. (1), Coo. (1), Psy. (1) | 0.500 |
| 53. |
Leucas aspera (Willd.) Link SE112 (Lamiaceae) |
Tumpai | Leaves | Hot | Laxative, Expectorant, Stimulant, Emmenagogue, To treat headache, throat ailments, polydipsia, cough, bronchitis, sinusitis, leucorrhea, fatigue, somatalgia | Rhinitis (1), Cough (1), Somatalgia (1) | Kap. (2), Ana. (1) | 0.500 |
| 54. |
Limonia acidissima Groff SE148 (Rutaceae) |
Viḷā | Fruit bulbs | Cold | Aromatic, Coolant, To treat anorexia, bloating, polydipsia, cough and bronchitis | Diabetes (3), Polydipsia (1), Hypertension (1) | Dia. (4), Hpt. (1) | 0.750 |
| 55. |
Macrotyloma uniflorum (Lam.) Verdc. SE100 (Fabaceae) |
Koḷḷu | Seeds | Hot | Astringent, Diuretic, Tonic | Obesity (1) | Obe. (1) | 0.000 |
| 56. |
Mangifera indica L. SE181 (Anacardiaceae) |
Mā | Fruits | Hot | Laxative, Diuretic, Tonic, Aphrodisiac | Male infertility (2), Heart ailments (4), Anorexia (3), To increase vision (1) | Hea. (4), Mal. (2), Gas. (3), Eye. (1) | 0.666 |
| 57. |
Marsilea quadrifolia L. SE195 (Marsileaceae) |
Āraikkīrai | Leaves | Cold | Coolant, Polyuria | Polyuria (2), Ulcers in urinary tract (2) | Dia. (2), Uri. (2) | 0.666 |
| 58. |
Melochia corchorifolia L. SE189 (Malvaceae) |
Puṇṇākkukkīrai | Leaves | Cold | Diuretic, Laxative | Pain during menopause (1) | Gyn. (1) | 0.000 |
| 59. |
Mentha arvensis L. SE171 (Lamiaceae) |
Putiṉā | Leaves | Hot | Stomachic, Diuretic, Stimulant, Carminative, Antispasmodic | Anemia (1), Anorexia (1) | Blo. (1), Ana. (1) | 0.000 |
| 60. |
Momordica charantia L. SE149 (Cucurbitaceae) |
Pākaṟkāy | Tender fruits | Hot | Tonic, Stomachic, Stimulant, Antibilious, Laxative, Alterative, Anthelmintic | Diabetes (1), Bloating (1), Intestinal worms (1) | Gas. (2), Dia. (1) | 0.500 |
| 61. |
Moringa oleifera Lam. SE111 (Moringaceae) |
Muruṅkai | Leaves | Cold | Antispasmodic, Stimulant, Expectorant, Diuretic, To treat anorexia, headache, fainting and eye ailments | Rhinitis (1), Cough (1), Somatalgia (2), Anemia (5), General weakness (1), To increase vision (1), Hypertension (2), Diabetes (1), Obesity (1), Anorexia (1), Menstrual migraine (2) | Blo. (5), Ana. (2), Hpt. (2), Gyn. (2), Kap. (2), Wea. (1), Eye. (1), Dia. (1), Obe. (1), Gas. (1) | 0.470 |
| 62. |
Mukia maderaspatana (L.) M.Roem. SE160 (Cucurbitaceae) |
Mucumucukkai | Leaves | Hot | Expectorant, To treat cough, bronchitis, wheezing, rhinitis | Asthma (2), Bronchitis (2), Cough (1) | Kap. (5) | 1.000 |
| 63. |
Murraya koenigii (L.) Sprengel SE106 (Rutaceae) |
Kaṟivēppilai | Leaves | Hot | Tonic, Stomachic, Diarrhea, Nausea, Fever, Psychological ailments | Indigestion (2), Dysmenorrhea (1), Diabetes (1), Anemia (1), Obesity (1), Anorexia (1), Bloating (1) | Gas. (4), Gyn. (1), Dia. (1), Blo. (1), Obe. (1) | 0.428 |
| 64. |
Musa paradisiaca L. SE145 (Musaceae) |
Vāḻai | Tender fruits, Flowers | Hot | Demulcent, Laxative, Nutritive, To treat hemorrhoids | Menstrual cramps (3), Gastric ulcers (3), Mouth ulcers (1), Hyperacidity (1), Hemorrhoids (2), Bleeding through rectum (1) | Gas. (5), Hem. (3), Gyn. (3) | 0.800 |
| 65. |
Nelumbo nucifera Gaertn. SE105 (Nelumbonaceae) |
Tāmarai | Flowers | Cold | Coolant, Astringent, Expectorant, Sedative, To treat fever, polydipsia and liver ailments | Heart ailments (1) | Hea. (1) | 0.000 |
| 66. |
Nigella sativa L. SE135 (Ranunculaceae) |
Karuñcīrakam | Seeds | Hot | Carminative, Diuretic, Emmenagogue, Lactogogue, Anthelmintic, Stomachic, Antibiotic, Emmollient, To treat eczema, headache, cough, vomiting, nausea and jaundice | Somatalgia (1), Amenorrhea (1) | Ana. (1), Gyn. (1) | 0.000 |
| 67. |
Oldenlandia umbellata L. SE161 (Rubiaceae) |
Impūral | Leaves | Cold | Expectorant, Styptic, Cholagogue, Good to treat internal bleeding | Productive cough (1), Bronchitis (1), Sinusitis (1) | Kap. (3) | 1.000 |
| 68. |
Oryza sativa L. SE130 (Poaceae) |
Arici | Seeds | Cold | Nutrient, Demulcent, Coolant | General weakness (2), Fatigue (1), Diabetes (1), Anemia (1) | Wea. (2), Fat. (1), Dia. (1), Blo. (1) | 0.250 |
| 69. |
Oxalis corniculata L. SE203 (Oxalidaceae) |
Puḷiyārai | Leaves | Cold | Stomachic, Coolant, Astringent, To treat fainting, diarrhea, bleeding through anus and hemorrhoids | Hypertension (2), Insomnia (1) | Hpt. (2), Psy. (1) | 0.500 |
| 70. |
Panicum sumatrense Roth ex Roem. & Schult. SE121 (Poaceae) |
Cāmai | Seeds | Cold | Demulcent, Tonic, To treat polydipsia, fever and musculo-skeletal disorders | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 71. |
Paspalum scrobiculatum L. SE120 (Poaceae) |
Varaku | Seeds | Cold | Chologogue | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 72. |
Pennisetum glaucum (L.)R.Br. SE119 (Poaceae) |
Kampu | Seeds | Cold | Tonic | General weakness (2), Fatigue (1), Anemia (1) | Wea. (2), Fat. (1), Blo. (1) | 0.333 |
| 73. |
Phoenix dactylifera L. SE156 (Arecaceae) |
Pērīṭcai | Fruits | Hot | Tonic, Nutritive, Demulcent, Laxative, Diuretic, Febrifuge, Coolant, Expectorant, Aphrodisiac, Good to treat polydipsia, anorexia and diabetes | Male infertility (1), Hypotension (1), General weakness (1) | Mal. (1), Hpo. (1), Wea. (1) | 0.000 |
| 74. |
Phyllanthus emblica L. SE152 (Phyllanthaceae) |
Nellikkāy | Fruits | Cold | Astringent, Coolant, Diuretic, Laxative, To treat bronchitis, sinusitis, nausea, vomiting, giddiness and hypertension | Heart ailments (2), Anemia (2), Constipation (1), Wheezing (1), Burning sensation (1), Diabetes (1), Anorexia (2), Rheumatalgia (1), To increase vision (2), Hypothyroidism (1) | Gas. (3), Hea. (2), Blo. (2), Eye. (2), Kap. (1), Coo. (1), Dia. (1), Vad. (1), Hpo. (1) | 0.384 |
| 75. |
Piper longum L. SE133 (Piperaceae) |
Tippili | Seeds | Hot | Stimulant, Carminative, To treat cough, gastric ulcers, wheezing, anemia, fainting, anorexia, bloating, headache, sinusitis, throat ailments and oligospermia | Somatalgia (1) | Ana. (1) | 0.000 |
| 76. |
Piper nigrum L. SE132 (Piperaceae) |
Miḷaku | Seeds | Hot | Acrid, Carminative, Febrifuge, Rubefacient, Stimulant, Resolvent, Antidote | Somatalgia (1), Anemia (1), Anorexia (1) | Ana. (1), Blo. (1), Gas. (1) | 0.000 |
| 77. |
Plectranthus amboinicus (Lour.) Spreng. SE143 (Lamiaceae) |
Ōmavalli | Leaves | Hot | Stimulant, Diaphoretic, Expectorant | Rhinitis (1), Bronchitis (1) | Kap. (2) | 1.000 |
| 78. |
Portulaca quadrifida L. SE173 (Portulacaceae) |
Ciṟu pacalai | Leaves | Cold | Diuretic, Stomachic, Aphrodisiac, Antibilious | Dysuria (2), Gastric ulcers (2), Hypertension (1), Anemia (1) | Uri. (2), Gas. (2), Hpt. (1), Blo. (1) | 0.400 |
| 79. |
Prunus dulcis (Mill.) D. A. Webb SE128 (Rosaceae) |
Vātumai | Seeds | Cold | Demulcent, Emollient, Nutrient | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 80. |
Psidium guajava L. SE179 (Myrtaceae) |
Koyyā | Fruits | Hot | Tonic, Astringent | Hyperacidity (1), Constipation (2), Diabetes (1) | Gas. (3), Dia. (1) | 0.666 |
| 81. |
Punica granatum L. SE166 (Lythraceae) |
Mātuḷai | Fruits | Cold | Astringent, Coolant | Bromhirdosis (1), Hyperacidity (1), Constipation (1), Gastric ulcers (1), Anorexia (2), Wheezing (1), Rheumatalgia (1), To increase vision (1), Hypothyroidism (1) | Gas. (5), Der. (1), Kap. (1), Vad. (1), Eye. (1), Thy. (1) | 0.444 |
| 82. |
Senna auriculata (L.) Roxb. SE103 (Fabaceae) |
Āvārai | Flowers | Cold | Astringent, Tonic, Good to treat Diabetes | Male infertility (1), Lumbago (1), Diabetes (2), Burning sensation (1) | Mal. (1), Vad. (1), Dia. (2), Coo. (1) | 0.000 |
| 83. |
Sesamum indicum L. SE116 Pedaliaceae |
Eḷ | Seeds | Hot | Emmenagogue, Stimulant, Tonic, Diuretic, Lactogogue, Laxative | Male infertility (1), Diabetes (1), Amenorrhea (1) | Mal. (1), Dia. (1), Gyn. (1) | 0.000 |
| 84. |
Sesbania grandiflora (L.) Poiret SE165 (Fabaceae) |
Akatti | Leaves | Cold | Antidote, Coolant, Laxative, Vermifuge | Obesity (1), Gastric ulcers (3), Hemorrhoids (1), Burning sensation (1), Dysuria (1), Hypertension (1) | Gas. (3), Obe. (1), Hem. (1), Coo. (1), Uri. (1), Hpt. (1) | 0.285 |
| 85. |
Setaria italica (L.) P. Beauvois SE122 (Poaceae) |
Tiṉai | Seeds | Hot | Nutrient, Diuretic, Astringent, Appitizer | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 86. |
Solanum americanum Mill. SE158 (Solanaceae) |
Maṇattakkāḷi | Leaves | Cold | Alterative, Diuretic, Diaphoretic, Expectorant, To treat mouth ulcers and bronchitis | Menstrual migraine (1), Strength bones (1) and nerves (1), Bronchitis (1), Somatalgia (2), Heart ailments (1), Wheezing (1), Gastric ulcers (2), Mouth ulcers (2), Fever (1), Fatigue (1), Convulsions (1), Headache (1), Liver diseases (1), Jaundice (1), Mumps (1), Cough (1), Dermatological ailments (1), Hypertension (1), Constipation (1) | Gas. (5), Kap. (3), Der. (2), Neu. (2), Ana. (2), Gyn. (1), Bon. (1), Hea. (1), Fev. (1), Fat. (1), Hed. (1), Liv. (1), Jau. (1), Hpt. (1) | 0.409 |
| 87. |
Solanum lycopersicum L. SE180 (Solanaceae) |
Takkāḷi | Fruits | Cold | Tonic, Coolant, To treat anemia | Constipation (1), Heart ailments (1), Diabetes (1), Anorexia (1), Rheumatalgia (1), To increase vision (1) | Gas. (2), Hea. (1), Dia. (1), Vad. (1), Eye. (1) | 0.200 |
| 88. |
Solanum torvum Sw. SE146 (Solanaceae) |
Cuṇṭaikkāy | Dried fruits | Hot | Expectorant, Germicide, Stomachic, To treat bloating, bronchitis, anorexia, intestinal worms and indigestion | Hypotension (1), Heart ailments (1), Bronchitis (1), Anemia (1), Wheezing (1), Diarrhea (1), Diabetes (1) | Kap. (2), Hpo. (1), Hea. (1), Blo. (1), Gas. (1), Dia. (1) | 0.166 |
| 89. |
Solanum trilobatum L. SE110 (Solanaceae) |
Tūtuvaḷai | Leaves | Hot | Stimulant, Expectorant, Tonic, Aphrodisiac, To treat bronchitis, cough and rhinitis | Rhinitis (1), Cough (1), Somatalgia (1), To increase memory (1), Male infertility (2), Oligospermia (1) | Mal. (3), Kap. (2), Ana. (1), Psy. (1) | 0.500 |
| 90. |
Sorghum bicolor (L.) Moench SE124 (Poaceae) |
Veḷḷaiccōḷam | Seeds | Cold | Nutrient, Laxative | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 91. |
Spinacia oleracea L. SE175 Amaranthaceae |
Pālakkīrai | Leaves | -- | -- | Hypertension (1) | Hpt. (1) | 0.000 |
| 92. |
Syzygium cumini (L.) Skeels SE151 (Myrtaceae) |
Nāval | Fruits | Cold | Stomachic, Diuretic, Tonic, Astringent, coolant, To treat polyuria, polydipsia and dysuria | Diabetes (2) | Dia. (2) | 1.000 |
| 93. |
Tamarindus indica L. SE198 (Fabaceae) |
Puḷi | Fruits | Hot | Laxative, To treat vomiting and hypertension | Anorexia (1), Nausea (1) | Gas. (2) | 1.000 |
| 94. |
Trachyspermum ammi Sprague. SE115 (Apiaceae) |
Ōmam | Seeds | Hot | Stomachic, Antispasmodic, Carminative, Antiseptic, Stimulant, Tonic, Sialogogue, to treat Cough, Diarrhea, Wheezing and Toothache | Heart ailments (1), Somatalgia (1) | Hea. (1), Ana. (1) | 0.000 |
| 95. |
Trianthema portulacastrum L. SE187 (Aizoaceae) |
Cāraṇai | Leaves | Hot | Laxative, Diuretic, To treat jaundice, swelling, anemia and bronchitis | Heart ailments (1) | Hea. (1) | 0.000 |
| 96. |
Tribulus terrestris L. SE196 (Zygophyllaceae) |
Ciṟu neruñcil | Leaves | Cold | Coolant, Diuretic, Demulcent, Tonic, Aphrodisiac, Astringent, To treat dysuria, fever, urolithiasis, enlargement of prostate, leucorrhea and polydipsia | Dysuria (2), Oligospermia (2), Burning sensation (1) | Uri. (2), Mal. (2), Coo. (1) | 0.500 |
| 97. |
Trichosanthes cucumerina L. SE172 (Cucurbitaceae) |
Puṭal | Tender fruits | Cold | Coolant, Aphrodisiac | Oliguria (1) | Uri. (1) | 0.000 |
| 98. |
Trigonella foenum-graecum L. SE163 (Fabaceae) |
Ventayam | Seeds | Cold | Coolant, Laxative, Diuretic, Demulcent, Astringent, Emollient, Aphrodisiac, Carminative, Tonic, To treat diarrhea, burning sensation, hypertension, fever, polydipsia and cough | Diabetes (1), Burning sensation (1), Anemia (2) | Blo. (2), Dia. (1), Coo. (1) | 0.333 |
| 99. |
Triticum aestivum L. SE164 (Poaceae) |
Kōtumai | Seeds | Cold | Nutritive, Demulcent, Aphrodisiac, Antirheumatic | Diabetes (1) | Dia. (1) | 0.000 |
| 100. |
Vigna mungo (L.) Hepper SE144 (Fabaceae) |
Uḷuntu | Seeds | Cold | Demulcent, Coolant, Aphrodisiac, Lactogogue, Nervine tonic, Nutritive, Good to strengthen pelvic bones | General weakness (3), Burning sensation (1), Cervicalgia (1), Lumbago (1), Ovulation problems (1), As supplement after puberty (1), Diabetes (1), Anemia (1) | Wea. (3), Vad. (2), Gyn. (2), Coo. (1), Dia. (1), Blo. (1) | 0.444 |
| 101. |
Vitis vinifera L. SE155 (Vitaceae) |
Tirāṭcai | Fruits | Cold | Laxative, Coolant, Diuretic, Nutritive, to treat anemia, bleeding and heart ailments | Male infertility (1), Hypotension (1), Anemia (2), Anorexia (2), Constipation (1), Wheezing (1), Rheumatalgia (1) | Gas. (3), Blo. (2), Mal. (1), Hpo. (1), Kap. (1), Vad. (1) | 0.375 |
| 102. |
Zea mays L. SE125 (Poaceae) |
Makkāccōḷam | Seeds | Cold | Tonic, Aphrodisiac | General weakness (2), Fatigue (1) | Wea. (2), Fat. (1) | 0.500 |
| 103. |
Zingiber officinale Roscoe. SE131 (Zingiberaceae) |
Iñci | Rhizomes | Hot | Carminative, Stomachic, Sialogogue, Digestive, Stimulant, Rubefacient | Somatalgia (1), Bloating (1) | Ana. (1), Gas. (1) | 0.000 |
| 104. |
Ziziphus jujuba Mill. SE186 (Rhamnaceae) |
Ilantai | Fruits | Cold | Astringent, Emollient, Appitizer, Antiemetic | Anorexia (3), Nausea (1), Diabetes (1) | Gas. (4), Dia. (1) | 0.750 |
Table 4.
List of animal taxa cited by the non-institutionally trained siddha practitioners of Tiruvallur district of Tamil Nadu for preparing medicinal foods
| S.No | Binomial name | Vernacular name | Parts used | Humoral propertya | Reported pharmacological action in Siddhaa | Illnesses treated | Illnesses categories | IAR |
|---|---|---|---|---|---|---|---|---|
| 1. | Anguilla bengalensis bengalensis (J. E. Gray, 1831) | Vilāṅku | Meat | Cold | Aphrodisiac | Fatigue (1), Joint pain (1) | Fat. (1). Vad. (1) | 0.000 |
| 2. |
Bos taurus
Linnaeus, 1758 |
Pacu | Milk | Cold | To treat fever, internal ulcers, pain, urinary ailments, fatigue and emaciation | To increase memory (1), Burning sensation (2), Oliguria (1), Indigestion (1) | Psy. (1), Coo. (2), Uri. (1), Gas. (1) | 0.500 |
| 3. |
Capra aegagrus hircus
(Linnaeus, 1758) |
Veḷḷāṭu | Meat | Cold | Nutritive, Aphrodisiac, To treat fever and tuberculosis | Oligospermia (1), Impotence (1), Gastric ulcers (1), Bone fractures (2) | Mal. (2), Gas. (1), Bon. (2) | 0.500 |
| 4. | Caranx melampygus Cuvier, 1833 | Pāṟai | Meat | -- | -- | Anabolic (1), Cough (1), Chest pain (1), Wheezing (1), Coolant (1) | Anb. (1), Kap. (2), Hea. (1), Coo. (1) | 0.250 |
| 5. | Channa spp. | Virāl | Meat | -- | -- | Anabolic (1), Oligospermia (1), Coolant (1) | Anb. (1), Mal. (1), Coo. (1) | 0.000 |
| 6. | Chanos chanos (Forsskal, 1775) | Pāl keṇṭai | Meat | Cold | -- | Lactogogue (1), Fatigue (1), Impotence (1) | Gyn. (1), Fat. (1), Mal.(1) | 0.000 |
| 7. | Eleutheronema tetradactylum (Shaw, 1804) | Kālā | Meat | -- | -- | Impotence (1), Heart diseases (1), Hypertension (1), Urolithiasis (2) | Uri. (2), Mal. (1), Hea. (1), Hpt. (1) | 0.250 |
| 8. | Euthynnus affinis (Cantor, 1849) | Nīla tuṭuppu cūṟai | Meat | -- | -- | Fever (1), Cough (2) | Kap. (2), Fev. (1) | 0.500 |
| 9. | Fenneropenaeus indicus (Milne-Edwards, 1837) | Veḷḷai iṟāl | Meat | Hot | Anabolic, To treat anemia | To improve vision (1), Anabolic (3), Lactogogue (1) | Anb. (3), Eye. (1), Gyn. (1) | 0.500 |
| 10 | Gallus gallus domesticus (Linnaeus, 1758) | Kōḻi | Eggs | Cold | Antirhematic, Aphrodisiac, To treat ulcers and bronchitis | Anemia (2), Bronchitis for children (1) | Blo. (2), Kap. (1) | 0.500 |
| 11. |
Gerres oyena
(Forsskal, 1775) |
Uṭuvāṉ | Meat | -- | -- | Somatalgia (1), Bronchitis (1), Lactogogue (1) | Anb. (1), Kap. (1), Gyn. (1) | 0.000 |
| 12. |
Gibelion catla
(Hamilton, 1822) |
Kaṭlā | Meat | Cold | -- | Fatigue (2), Somatalgia (1), Impotence (1), Lactogogue (2), To increase vision (1) | Fat. (2), Gyn. (2), Ana. (1), Mal. (1), Eye. (1) | 0.333 |
| 13. |
Himantura uarnak
(Forsskal, 1775) |
Tirukkai | Meat | Hot | Aphrodisiac | Somatalgia (1), Wheezing (3) | Kap. (3), Ana. (1) | 0.666 |
| 14. |
Katelysia opima
(Gmelin, 1791) |
Cippi | Meat | -- | -- | Bronchitis (1), Impotence (2) | Mal. (2), Kap. (1) | 0.500 |
| 15. |
Lactarius lactarius
(Bloch & Schneider, 1801) |
Cutumpu | Meat | -- | -- | Chest pain (1) | Hea. (1) | 0.000 |
| 16. |
Lates calcarifer
(Bloch, 1790) |
Koṭuvā | Meat | -- | -- | Rheumatalgia (3), Impotence (1) | Vad. (3), Mal. (1) | 0.666 |
| 17. |
Lebeo rohita
Hamilton, 1822 |
Kaṇṇādi kendai | Meat | -- | -- | Somatalgia (1), Heart disease (1), Eye disease (1), Obesity (1) | Ana. (1), Hea. (1), Eye. (1), Obe. (1) | 0.000 |
| 18. | Monodactylus argenteus (Linnaeus, 1758) | Puraṇṭi | Meat | -- | -- | Cough (1) | Kap. (1) | 0.000 |
| 19. | Mystus sp. | Keḷutti | Meat | Cold | Aphrodisiac | Bronchitis (1) | Kap. (1) | 0.000 |
| 20. |
Nemipterus japonicas
(Bloch, 1791) |
Caṅkarā | Meat | -- | -- | Chest pain (1) | Hea. (1) | 0.000 |
| 21. |
Oreochromis mossambicus
(Peters, 1852) |
Jilēppi | Meat | -- | -- | Bronchitis (1), Joint pain (1), Fatigue (1), Lactogogue (1), Chest pain (1) | Kap. (1), Vad. (1), Fat. (1), Gyn. (1), Hea. (1) | 0.000 |
| 22. | Pampus argenteus (Euphrasen, 1788) | Vavāl | Meat | -- | -- | Cough (2), Lactogogue (1) | Kap. (2), Gyn. (1) | 0.500 |
| 23. | Parastromateus niger (Bloch, 1795) | Karuppu vavāl | Meat | Hot | Aprhrodisiac and lactogogue | Wheezing (3), To increase memory (1) | Kap. (3), Psy. (1) | 0.666 |
| 24. | Parathelphusa hydrodromus (Bloch, 1795) | Cēṟṟu naṇṭu | Meat | Hot | Stimulant, Febrifuge, To treat bronchitis, rheumatism and indigestion | Fever (3) | Fev. (3) | 1.000 |
| 25. |
Parupeneus indicus
(Shaw, 1803) |
Nakarai/ mussara | Meat | -- | -- | Coolant (1) | Coo. (1) | 0.000 |
| 26. |
Portunus sanguinolentus
(Herbst, 1783) |
Kaṭal naṇṭu | Meat | Hot | -- | Bronchitis (3), Fever (2) | Kap. (3), Fev. (2) | 0.750 |
| 27. | Rachycentron canadus (Linnaeus, 1766) | Ney mīṉ | Meat | -- | -- | Good for pregnant women (1), Lactogogue (1) | Gyn. (2) | 1.000 |
| 28. | Rastrelliger kanagurta (Cuvier, 1816) | Kāṉaṅkattai | Meat | -- | -- | Bronchitis (3) | Kap. (3) | 1.000 |
| 29. |
Sardinella longiceps
Valenciennes, 1847 |
Peichālai | Meat | -- | -- | Anabolic (4), Fatigue (1) | Anb. (4), Fat. (1) | 0.750 |
| 30. | Scoliodon laticaudus Muller & Henle, 1838 | Piḷḷaiccuṟā | Meat | Hot | Appitizer, lactogogue, To treat rheumatism and bronchitis | Lactogogue (7) | Gyn. (7) | 1.000 |
| 31. | Scomberomorus guttatus (Bloch & Schneider, 1801) | Vañciram | Meat | -- | -- | Obesity (1), Fatigue (1), Chest pain (1), Rheumatalgia (1) | Obe. (1), Fat. (1), Hea. (1), Vad. (1) | 0.000 |
| 32. | Sphyraena jello Cuvier in Cuvier & Valenciennes, 1829 | Ūḻi | Meat | -- | -- | Lactogogue (1), Anabolic (2), Coolant (1) | Anb. (2), Gyn. (1), Coo. (1) | 0.333 |
| 33. | Stolephorus indicus (van Hasselt, 1823) | Nettili | Meat | -- | -- | Cough (1), Wheezing (2), Lactogogue (2) | Kap. (3), Gyn. (2) | 0.750 |
| 34. | Stolephorus spp. | -- | Meat | -- | -- | Oligospermia (2) | Mal. (2) | 1.000 |
| 35. | Thryssa malabarica (Bloch, 1795) | Poruvā | Meat | -- | -- | Arthritis (1) | Vad. (1) | 0.000 |
| 36. |
Trichiurus lepturus Linnaeus, 1758 Eupleurogrammus muticus (Gray, 1831) |
Ōlai vāḷai | Meat | Hot | Appitizer, To treat bronchitis and rheumatism | Giddiness (1), Bronchitis (2), Joint pain (1) | Kap. (2), Hyp. (1), Vad. (1) | 0.333 |
| 37. |
Upeneus sulphureus
Cuvier, 1829 |
Navarai | Meat | -- | -- | Joint pain (2) | Vad. (2) | 1.000 |
| 38. |
Uroteuthis duvauceli
(d’Orbigny, 1835) |
Ūci kaṉavā | Meat | -- | -- | Anemia (2), Rheumatalgia (1), Bronchitis (1) | Blo. (2), Vad. (1), Kap. (1) | 0.333 |
Fig. 3.
Photographs of some animal taxa referred by the non-institutionally trained siddha practitioners of Tiruvallur district for the preparation of medicinal foods. (a) Channa sp. (Virāl); (b) Pampus argenteus (Vavāl); (c) Scomberomorus guttatus (Vañciram); (d) Nemipterus japonicas (Caṅkarā); (e) Oreochromis mossambicus (Jilēppi); (f) Lates calcarifer (Koṭuvā); (g) Trichiurus lepturus (Ōlai vāḷai); (h) Caranx melampygus (Pāṟai); (i) Scoliodon laticaudus (Piḷḷaiccuṟā); (j) Parupeneus indicus (Nakarai); (k) Eleutheronema tetradactylum (Kālā); (l) Sardinella longiceps (Peichālai); (m) Himantura uarnak (Tirukkai); (n) Sphyraena jello (Ūḻi); (o) Stolephorus indicus (Nettili); (p) Fenneropenaeus indicus (Veḷḷai iṟāl); (q) Lebeo rohita (Kaṇṇādi kendai); (r) Parastromateus niger (Karuppu vavāl); (s) Mystus sp. (Keḷutti); (t) Uroteuthis duvauceli (Ūci kaṉavā); (u) Lactarius lactarius (Cutumpu); (v) Portunus sanguinolentus (Kaṭal naṇṭu)
Consensus over the use of plant-based medicinal foods
The illness categories viz., gastrointestinal ailments, hemorrhoids, and neural ailments were considered as illness categories with high consensus since they had higher FIC values than mean plus average FIC value. Sixteen illness categories such as kapha ailments, weakness, urinary, and ailments had average FIC values and were considered as illness categories with average consensus. Eight illness categories such as bone fractures, fatigue, fever, headache, hypotension, hypothyroidism, jaundice, and obesity were considered as illness categories with low consensus (Table 5).
Table 5.
FIC values for illness categories treated with plant-based medicinal foods by the non-institutionally trained siddha practitioners in Tiruvallur district
| Illness categories | Abbreviations used | N UR | % UR | N t | % T | N C | N VC | F ic |
|---|---|---|---|---|---|---|---|---|
| Analgesics | Ana. | 18 | 3.94 | 14 | 13.46 | 14 | 3 | 0.235 |
| Anabolic | Anb. | – | – | – | – | – | – | – |
| Blood ailments | Blo. | 29 | 6.35 | 18 | 17.30 | 18 | 8 | 0.379 |
| Bone fracture | Bon. | 2 | 0.43 | 2 | 1.92 | 2 | 0 | 0.000 |
| Coolants | Coo. | 18 | 3.94 | 14 | 13.46 | 14 | 3 | 0.235 |
| Dermatological ailments | Der. | 5 | 1.09 | 4 | 3.84 | 4 | 1 | 0.250 |
| Diabetes | Dia. | 35 | 7.67 | 24 | 23.07 | 24 | 6 | 0.323 |
| Eye ailments | Eye. | 9 | 1.97 | 8 | 7.69 | 8 | 1 | 0.125 |
| Fatigue | Fat. | 14 | 3.07 | 14 | 13.46 | 14 | 0 | 0.000 |
| Fever | Fev. | 2 | 0.43 | 2 | 1.92 | 2 | 0 | 0.000 |
| Gastrointestinal ailments | Gas. | 90 | 19.73 | 36 | 34.61 | 36 | 26 | 0.606 |
| Gynecological ailments | Gyn. | 20 | 4.38 | 13 | 12.50 | 13 | 4 | 0.368 |
| Headache | Hed. | 1 | 0.21 | 1 | 0.96 | 1 | 0 | 0.000 |
| Heart ailments | Hea. | 21 | 4.60 | 15 | 14.42 | 15 | 4 | 0.300 |
| Hemorrhoids | Hem. | 20 | 4.38 | 8 | 7.69 | 8 | 6 | 0.613 |
| Hypertension | Hpt. | 13 | 2.85 | 10 | 9.61 | 10 | 3 | 0.250 |
| Hypotension | Hpo. | 8 | 1.74 | 8 | 7.69 | 8 | 0 | 0.000 |
| Hypothyroidism | Thy. | 3 | 0.65 | 3 | 2.88 | 3 | 0 | 0.000 |
| Jaundice | Jau. | 2 | 0.43 | 2 | 1.92 | 2 | 0 | 0.000 |
| Kapha ailments | Kap. | 32 | 7.01 | 17 | 16.34 | 17 | 10 | 0.483 |
| Liver ailments | Liv. | 4 | 0.87 | 3 | 2.88 | 3 | 1 | 0.333 |
| Male reproductive ailments | Mal. | 28 | 6.14 | 21 | 20.19 | 21 | 6 | 0.259 |
| Neural ailments | Neu. | 2 | 0.43 | 1 | 0.96 | 1 | 1 | 1.000 |
| Obesity | Obe. | 8 | 1.74 | 8 | 7.69 | 8 | 0 | 0.000 |
| Psychological ailments | Psy. | 8 | 1.74 | 7 | 6.73 | 7 | 1 | 0.142 |
| Urinary ailments | Uri. | 18 | 3.94 | 11 | 10.57 | 11 | 5 | 0.411 |
| Vadha ailments | Vad. | 11 | 2.41 | 9 | 8.65 | 9 | 2 | 0.200 |
| Weakness | Wea. | 35 | 7.67 | 19 | 6.50 | 19 | 15 | 0.470 |
| Analgesics | Ana. | 4 | 3.076 | 4 | 10.526 | 4 | 1 | 0.000 |
| Anabolic | Anb. | 11 | 8.461 | 5 | 13.157 | 5 | 2 | 0.600 |
| Blood ailments | Blo. | 4 | 3.076 | 2 | 5.263 | 2 | 2 | 0.666 |
| Bone fracture | Bon. | 2 | 1.538 | 1 | 2.613 | 1 | 1 | 1.000 |
| Coolants | Coo. | 6 | 4.615 | 5 | 13.157 | 5 | 1 | 0.200 |
| Dermatological ailments | Der. | – | – | – | – | – | – | – |
| Diabetes | Dia. | – | – | – | – | – | – | – |
| Eye ailments | Eye. | 3 | 2.307 | 3 | 7.894 | 3 | 0 | 0.000 |
| Fatigue | Fat. | 7 | 5.384 | 6 | 15.789 | 6 | 1 | 0.375 |
| Fever | Fev. | 6 | 4.615 | 3 | 7.894 | 3 | 2 | 0.166 |
| Gastrointestinal ailments | Gas. | 2 | 0.769 | 2 | 2.613 | 2 | 0 | 0.000 |
| Gynecological ailments | Gyn. | 19 | 14.615 | 10 | 26.315 | 10 | 4 | 0.500 |
| Headache | Hed. | – | – | – | – | – | – | – |
| Heart ailments | Hea. | 7 | 5.384 | 7 | 18.421 | 7 | 0 | 0.000 |
| Hemorrhoids | Hem. | – | – | – | – | – | – | – |
| Hypertension | Hpt. | 1 | 1.538 | 1 | 5.263 | 1 | 0 | 0.000 |
| Hypotension | Hpo. | – | – | – | – | – | – | – |
| Hypothyroidism | Thy. | 1 | 1.538 | 1 | 5.263 | 1 | 0 | 0.000 |
| Jaundice | Jau. | – | – | – | – | – | – | – |
| Kapha ailments | Kap. | 30 | 23.076 | 16 | 44.736 | 16 | 9 | 0.482 |
| Liver ailments | Liv. | – | – | – | – | – | – | – |
| Male reproductive ailments | Mal. | 11 | 6.923 | 8 | 21.052 | 8 | 3 | 0.714 |
| Neural ailments | Neu. | – | – | – | – | – | – | – |
| Obesity | Obe. | 2 | 1.538 | 2 | 2.613 | 2 | 0 | 0.000 |
| Psychological ailments | Psy. | 2 | 1.538 | 2 | 2.613 | 2 | 0 | 0.000 |
| Urinary ailments | Uri. | 3 | 2.564 | 2 | 2.613 | 2 | 1 | 0.500 |
| Vadha ailments | Vad. | 11 | 8.461 | 8 | 23.684 | 9 | 2 | 0.222 |
| Weakness | Wea. | – | – | – | – | – | – | – |
NUR number of use reports, % UR % of use reports, Nt number of taxa, % T % of taxa, Nc number of claims, Nvc number of valid claims, – no UR and Fic value was not calculated
Consensus over the use of animal-based medicinal foods
Among the illness categories treated with animal-based medicinal foods, kapha ailments had gained high percentage (23.07%) of UR followed by gynecological ailments (14.61%). Nineteen illness categories were reported to be treated with animal-based medicinal foods. Analysis of the consensus showed that the categories viz., bone fractures, male reproductive ailments, blood ailments, and anabolic had high FIC values and were considered as illness categories with high consensus. Seven illness categories such as gynecological, urinary ailments, kapha ailments, fatigue, vadha ailments, coolants, and fever were grouped as illness categories with average consensus (Table 5).
Illness categories treated with plant-based medicinal foods having high consensus
These two illness categories had high FIC scores among the illness categories treated with plant-based medicinal foods. Gastrointestinal ailment is the majorly cited illness category that represented 19.73% of total UR. In this category, 36 plant taxa were used to prepare the medicinal formulations. Among them, 26 taxa had a minimum of two UR for treating gastrointestinal ailments. The taxa such as fruits of Citrus medica (citron), leaves, unripe fruits of Coccinia grandis (ivy gourd), and flowers of Musa paradisiaca (plantain) had high number of UR.
In the case of hemorrhoids, eight plant taxa were used; among them, six taxa had a minimum of two UR. In this category, Allium cepa (onion), Abutilon indicum, Amorphophallus paeoniifolius (elephant foot yam), and plantain had high number of UR and IAR values. In the case of neural ailments, Solanum americanum had high number of UR and was reported to strengthen the nerves (Table 6).
Table 6.
List of important plant and animal medicinal food taxa cited by the non-institutionally trained Siddha practitioners of Tiruvallur district, Tamil Nadu, to treat various ailments
| Illness categories | Plants | Animals |
|---|---|---|
| Analgesics | Cardiospermum halicacabum (0.750), Moringa oleifera (0.470), Solanum americanum (0.409) | – |
| Anabolic | – | Sardinella longiceps (1.000), Fenneropenaeus indicus (0.500), Sphyraena jello (0.333) |
| Blood ailments | Moringa oleifera (0.470), Beta vulgaris (0.333), Eclipta prostrata (0.400), Eleusine coracana (0.333), Ficus racemosa (0.428), Phyllanthus emblica (0.384), Trigonella foenum-graecum (0.333), Vitis vinifera (0.375) | Gallus gallus domesticus (0.500), Uroteuthis duvauceli (0.333) |
| Bone fracture | – | Capra aegagrus hircus (0.333) |
| Coolants | Borassus flabellifer (0.666), Coccinia grandis (0.692), Cuminum cyminum (0.428) | Bos taurus (0.500) |
| Dermatological ailments | Solanum americanum (0.409) | – |
| Diabetes | Coccinia grandis (0.692), Limonia acidissima (0.750), Abelmoschus esculentus (0.333), Brassica oleracea var. gongylodes (1.000), Marsilea quadrifolia (0.666), Syzygium cumini (1.000) | – |
| Eye ailments | Phyllanthus emblica (0.384) | – |
| Fatigue | – | Gibelion catla (0.333) |
| Fever | – | Parathelphusa hydrodromus (1.000), Portunus sanguinolentus (0.750) |
| Gastrointestinal ailments | Citrus medica (0.666), Coccinia grandis (0.692), Musa paradisiaca (0.800) Punica granatum (0.444), Solanum americanum (0.409), Citrus limon (0.400), Murraya koenigii (0.428), Ziziphus jujuba (0.750), Cuminum cyminum (0.428), Ipomoea aquatica (0.750), Mangifera indica (0.666), Phyllanthus emblica (0.384), Psidium guajava (0.666), Sesbania grandiflora (0.285), Vitis vinifera (0.375), Allium sativum (0.250), Citrullus lanatus (0.500), Cocos nucifera (0.333), Cucumis sativus (1.000), Daucus carota (0.333), Digera muricata (1.000), Ficus racemosa (0.428), Momordica charantia (0.500), Portulaca quadrifida (0.400), Solanum lycopersicum (0.200), Tamarindus indica (1.000) | – |
| Gynecological ailments | Aloe vera (0.428), Musa paradisiaca (0.800), Moringa oleifera (0.470), Vigna mungo (0.444) | Scoliodon laticaudus (1.000), Gibelion catla (0.333), Rachycentron canadus (1.000), Stolephorus indicus (0.750) |
| Headache | – | – |
| Heart ailments | Mangifera indica (0.666), Citrus medica (0.666), Hibiscus rosa-sinensis (0.500), Phyllanthus emblica (0.384) | – |
| Hemorrhoids | Allium cepa (0.666), Abutilon indicum (1.000), Amorphophallus paeoniifolius (0.666), Cissus quadrangularis (0.400), Musa paradisiaca (0.800), Acalypha indica (0.333) | – |
| Hypertension | Citrus medica (0.666), Moringa oleifera (0.470), Oxalis corniculata (0.500) | – |
| Hypotension | – | – |
| Hypothyroidism | – | – |
| Jaundice | – | – |
| Kapha ailments | Mukia maderaspatana (1.000), Solanum americanum (0.409), Cardiospermum halicacabum (0.750), Cleome gynandra (0.250), Leucas aspera (0.250), Moringa oleifera (0.470), Plectranthus amboinicus (1.000), Solanum torvum (0.166), Solanum trilobatum (0.500) | Himantura uarnak (0.500), Parastromateus niger (0.666), Rastrelliger kanagurta (1.000), Stolephorus indicus (0.750), Euthynnus affinis (0.500), Pampus argenteus (0.500), Trichiurus lepturus Eupleurogrammus muticus (0.333) |
| Liver ailments | Eclipta prostrata (0.400) | – |
| Male reproductive ailments | Solanum trilobatum (0.500), Allium cepa (0.666), Ficus racemosa (0.428), Ipomoea aquatica (0.750), Mangifera indica (0.666), Tribulus terrestris (0.500) | Capra aegagrus hircus (0.500), Katelysia opima (0.500), Stolephorus spp. (1.000) |
| Neural ailments | Solanum americanum (0.409) | – |
| Obesity | – | – |
| Psychological ailments | Centella asiatica (0.500) | – |
| Urinary ailments | Boerhavia diffusa (1.000), Lagenaria siceraria (0.500), Marsilea quadrifolia (0.666), Portulaca quadrifida (0.400), Tribulus terrestris (0.500) | Eleutheronema tetradactylum (0.250) |
| Vadha ailments | Citrus limon (0.400), Vigna mungo (0.444) | Lates calcarifer (1.000), Upeneus sulphureus (1.0) |
| Weakness | Vigna mungo (0.444), Amaranthus viridis (0.333), Anacardium occidentale (0.500), Arachis hypogaea (0.500), Cicer arietinum (0.333), Echinochloa frumentacea (0.500), Eleusine coracana (0.333), Oryza sativa (0.250), Panicum sumatrense (0.500), Paspalum scrobiculatum (0.500), Pennisetum glaucum (0.333), Prunus dulcis (0.500), Setaria italica (0.500), Sorghum bicolor (0.500), Zea mays (0.500) | – |
The values mentioned within the parentheses indicate the IAR values. Taxa are arranged in descending order of UR
Illness categories treated with plant-based medicinal foods having average consensus
Kapha (pulmonary and respiratory) ailments gained 7.01% of total UR and 17 taxa. In this category, Mukia maderaspatana had high IAR score and UR. In the case of general weakness, the flour of Vigna mungo seeds (black gram) had high number of UR. The use of Boerhavia diffusa leaves had high UR to treat urinary ailments. The leaves of Moringa oleifera scored high UR under the category of blood ailments for the treatment of anemia. The gel of Aloe vera had high UR under the category of gynecological ailments and given to treat general ailments of uterus, dysmenorrhea, and metrorrhagia. In this category, the flowers and tender fruits of plantain had a high IAR score.
Cooked leaves of Eclipta prostrata were given to treat the liver ailments, and it had high number of UR in this category. In the case of diabetes, the plants such as stems of Brassica oleracea var. gongylodes (kohlrabi) and the fruits of Syzygium cumini had high IAR score. In this category, the leaves and fruits of ivy gourd had high number of UR. The fruits such as mango and citron had high number of UR and IAR score under the category of heart ailments. In the case of male reproductive ailments, the leaves of Ipomoea aquatica (water spinach) and onion had high IAR score; the use of flowers of Solanum trilobatum had high UR. The use of citron had high UR and IAR for the treatment of hypertension. Other important plants under this group were Solanum americanum (dermatological ailments), Cardiospermum halicacabum (analgesics), Borassus flabellifer (coolants), Citrus limon (vadha ailments), Centella asiatica (psychological ailments), and Phyllanthus emblica (eye ailments) (Table 6).
Illness categories treated with animal-based medicinal foods having high consensus
The hoofs of Capra aegagrus hircus (goat) had been given to treat bone fractures. The use of milk and testes of goat, and the meat of Katelysia opima to treat male reproductive ailments had high UR; and the use of Stolephorus meat had high IAR score. The use of Gallus gallus domesticus eggs (chicken) and Uroteuthis duvauceli (Indian squid) had high UR under the category of blood ailments and were used to treat anemia. Sardinella longiceps (Indian oil sardine) and Fenneropenaeus indicus (Indian prawn) had high UR under the anabolics (Table 6).
Illness categories treated with animal-based medicinal foods having average consensus
In the case of gynecological ailments, Scoliodon laticaudus (spade nose shark) had high UR and IAR value; it was reported to increase lactation. In the case of urinary ailments, Eleutheronema tetradactylum (fourfinger threadfin) had high UR and was reported to treat urolithiasis. In the case of kapha ailments, Himantura uarnak (reticulate whipray) had high number of UR; Rastrelliger kanagurta (Indian mackerel) and Stolephorus indicus (Indian anchovy) had high IAR values. In the case of fever, Parathelphusa hydrodromus and Portunus sanguinolentus (blood spotted swimming crab) had high UR and IAR scores. Other important animals under this category were Gibelion catla (catla) to treat fatigue, Lates calcarifer (barramundi) and Upeneus sulphureus to treat vadha ailments, and the buttermilk of Bos taurus (cow) as coolant (Table 6).
Relationship between the humoral properties and illnesses
In the case of plant-based medicinal foods, the RFC for plants with cold humor was comparatively high (64.08%) compared to the plants with cold humor. In animal-based medications, no such variation was found. The illness categories such as analgesics, hemorrhoids, and kapha ailments had comparatively high RFC for plants with hot humor. In the case of animal-based foods, the categories such as fever, gynecological ailments, and kapha ailments have high RFC for plants with hot humor (Table 7).
Table 7.
Frequency of URs for illness categories treated with plant and animal medicinal food taxa on the basis of humors
| Illness categories | Plant food taxa | Animal food taxa | ||||
|---|---|---|---|---|---|---|
| Hot | Cold | Unspecified | Hot | Cold | Unspecified | |
| Analgesics | 72.22 | 27.78 | – | 25 | 25 | 50 |
| Anabolic | – | – | – | 9.09 | – | 90.90 |
| Blood ailments | 24.13 | 68.97 | 6.90 | – | 50 | 50 |
| Bone fracture | 50 | 50 | – | – | 100 | – |
| Coolants | 11.11 | 88.89 | – | – | 33.33 | 66.66 |
| Dermatological ailments | 20 | 80 | – | – | – | – |
| Diabetes | 22.86 | 71.42 | 5.72 | – | – | – |
| Eye ailments | 33.33 | 66.67 | – | 33.33 | 33.33 | 33.33 |
| Fatigue | 14.28 | 78.58 | 7.14 | – | 57.14 | 42.85 |
| Fever | 50 | 50 | – | 83.33 | – | 16.66 |
| Gastrointestinal ailments | 35.56 | 62.22 | 2.22 | – | 100 | – |
| Gynecological ailments | 40 | 60 | – | 42.10 | 15.78 | 42.10 |
| Headache | 0 | 100 | – | – | – | – |
| Heart ailments | 52.35 | 42.65 | 5.00 | 0 | 0 | 100 |
| Hemorrhoids | 60 | 40 | – | – | – | – |
| Hypertension | 0 | 92.30 | 7.70 | 0 | 0 | 100 |
| Hypotension | 25 | 50 | 25 | – | – | – |
| Hypothyroidism | 33.33 | 66.67 | – | 100 | 0 | 0 |
| Jaundice | 0 | 100 | – | – | – | – |
| Kapha ailments | 59.37 | 40.63 | – | 36.66 | 6.66 | 56.66 |
| Liver ailments | 50 | 50 | – | – | – | – |
| Male reproductive ailments | 39.28 | 50 | 10.72 | 0 | 36.36 | 63.63 |
| Neural ailments | 50 | 50 | – | – | – | – |
| Obesity | 50 | 50 | – | 0 | 0 | 100 |
| Psychological ailments | 25 | 75 | – | 50 | 50 | 0 |
| Urinary ailments | 16.66 | 83.33 | – | 0 | 33.33 | 66.66 |
| Vadha ailments | 36.37 | 63.63 | – | 9.09 | 9.09 | 81.81 |
| Weakness | 22.85 | 71.42 | 5.73 | – | – | – |
– No UR and frequency was not calculated
CFSI scores of the medicinal foods
List of plant and animal taxa having top ten CFSI scores are given in Table 8, and the CFSI scores for all taxa are given in Additional file 1: Table S2. It showed that the average CFSI score of the plant taxa was higher than that of the animal taxa.
Table 8.
List of plant and animal taxa which got top ten CFSI score
| Name of the taxa | CFSI |
|---|---|
| Plants | |
| Solanum americanum | 110.28 |
| Murraya koenigii | 97.20 |
| Moringa oleifera | 95.64 |
| Cuminum cyminum | 63.84 |
| Musa paradisiaca | 55.68 |
| Coccinia grandis | 45.67 |
| Phyllanthus emblica | 45.36 |
| Solanum lycopersicum | 40.50 |
| Vitis vinifera | 40.24 |
| Punica granatum | 39.96 |
| Animals | |
| Portunus sanguinolentus | 33.75 |
| Sardinella longiceps | 29.25 |
| Fenneropenaeus indicus | 27.00 |
| Stolephorus indicus | 22.50 |
| Bos taurus | 19.50 |
| Rastrelliger kanagurta | 18.22 |
| Sphyraena jello | 16.20 |
| Scoliodon laticaudus | 15.75 |
| Himantura uarnak | 13.50 |
| Parastromateus niger | 13.50 |
Discussion
In Indian systems of traditional medicine, diet recommendation is an integral and important part of the therapy; it is considered as an ally for strengthening the drug efficacy [46]. However, this knowledge is poorly documented and under-utilized. Our previous studies in other districts of Tamil Nadu also indicated that non-institutional training of siddha system is a male dominant domain [37], and cultural reasons play a vital role on low women’s participation. Such unevenness was also recorded in some ethnobiological studies in other geographical parts [47]. Traditional medicine was often perceived as the healthcare option only for the poor and marginalized communities; a recent work in Nepal indicated that these practices prevailed both in rural and semi-urban areas, and it showed positive correlation with household income and traditional medicine use [48]. The data of this study also indirectly substantiated the previous work by showing relatively high percentage of traditional healers in urban and semi-urban areas.
Sampling sufficiency and the representativeness of the samples collected are considered as major concerns of modern ethnobiology research [49], and various methods are employed to ascertain them. Application of species richness curve was one of the methods, and in this study, it was done by plotting Shannon-Wiener’s index in ordinate axis (y) and cumulative number of UR in abscissa axis (x). Reaching a clear asymptote of the curve was considered as an indicator for the sufficiency of sampling. Comparatively low Shannon-Wiener score for the animal-based foods indicated the lack of diversity in the animal foods than plant foods. The traditional medical literatures of ayurveda and siddha described about the health benefits of animal-based foods; however, the cultural and spiritual beliefs along with better understanding of the nutritional properties of plants caused a preference of vegetarianism in India [50]. Our previous study on ethnodietetics among non-institutionally trained siddha practitioners of Virudhunagar district had also yielded high number of UR for plant-based foods [12]. The same trend was reflected in this survey, and plant taxa got high UR and average IAR values. The CFSI scores for the plant taxa were comparatively higher than that of animal taxa. Our previous surveys in inland of Tamil Nadu showed low UR for fish taxa [12, 51]. In this survey, comparatively better availability of fish taxa caused more UR towards them.
Gastrointestinal ailments are one of the illnesses which got high number of UR in many ethnopharmacological explorations [52]. Food is directly related with various gastrointestinal illnesses, and the use of medicinal foods among subjects with functional gastrointestinal disorders was also high [53, 54]. The use of citron got a high number of UR in this study; it has also been used to treat gastrointestinal ailments in ayurveda and Chinese system of traditional medicine [55]. It has also been used for the treatment of the same in countries such as Nepal [56] and Pakistan [57]. A small clinical study with 37 subjects having recurrent aphthous stomatitis indicated that the application of citrus essential oil alleviated the pain in oral ulcers [58]. Some preliminary scientific experiments on Citrus fruits revealed the effectiveness on Helicobacter pylori [59]. From Citrus fruits, the compounds such as nobiletin [60], hesperidin, neohesperidin [61], β-myrcene [62], limonene, β-pinene [63], and 7,8-dimethoxycoumarin [64] were reported to have gastroprotective effects. Despite its traditional usage in many geographical areas and preclinical evidences, this claim lacks robust clinical data. Preliminary preclinical evidences supported the use of ivy gourd [65] and plantain for the treatment of gastric ulcer [66], but no clinical studies were available. The use of pomegranate was reported for the treatment of gastrointestinal ailments in Mexico [67] and Algeria [68]. Solanum americanum is one of the important plants of Tamil Nadu used to treat gastrointestinal ailments [69], and it is also used to treat gastrointestinal ailments in some other groups [70, 71]. Our previous ethnobotanical explorations had also documented the use of onion, Abutilon indicum, and elephant foot yam to treat hemorrhoids [37, 40, 72]; no scientific validation was reported.
Our previous surveys documented the use of Mukia maderaspatana in treating various pulmonary ailments [37, 40, 51, 72]. Boerhavia diffusa had been used to treat renal illnesses also in other geographic regions, and preclinical investigations showed its nephroprotective and antilithiasis effects [73, 74]. Moringa oleifera leaves are used as a supplement to treat anemia in other regions also [75], and according to a preclinical study, the dietary iron in M. oleifera is reported as superior to ferric citrate [76]. In ayurveda also, Aloe vera has been used to treat various gynecological ailments [77].
Eclipta prostrata is one of the important plants used in Indian as well as Chinese systems of traditional medicine for hepatoprotection [55]. Kohlrabi is an exotic taxon to India; it was not mentioned in the siddha materia medica, but it was prescribed by the informants of this study. Studies on such claims may yield some clues on knowledge transmission about the uses of exotic flora. Antidiabetic effect of Brassica oleracea was reported [78]; the antidiabetic effect of red kohlrabi was found to be superior to the green variety by a preclinical experiment [79]. A randomized, double blind trial with 63 type 2 diabetic subjects showed that the administration of broccoli (a variety of Brassica oleracea) powder at 10 g/day significantly lowered the insulin resistance [80]. Though Syzygium cumini was reported for diabetes by many previous studies, its antidiabetic efficacy was inconclusive [81]. The use of ivy gourd for the treatment of diabetes was also documented in Sri Lanka [82], Bangladesh [83], and Pakistan [84]. A small, double blinded phase I trial with 61 healthy volunteers indicated that consumption of 20 g of ivy gourd leaves significantly lowered the fasting and post-prandial glucose levels [85]. Pretreatment with mangiferin to isoproterenol induced myocardial infarcted rats prevented the alterations in mitochondrial energy metabolism and structural integrity of the heart tissues [86]. Cardioprotective effect of citron was recently reviewed [87]; no clinical reports were available to substantiate the cardioprotective effect of mango and citron supplementation. The use of Citrus fruits for the management of hypertension by Polish migrants in Argentina was already reported [88], and small double-blind, cross-over study with 12 stage I hypertensive patients indicated its usefulness [25]. Two small clinical studies showed the anxiolytic potential of Centella asiatica [89, 90].
The principle of using meat of an organ to treat the illnesses of the similar organ (similia similibus curantur) was reported in previous ethnopharmacological surveys [51, 91]. Previous studies in various geographical locations documented the use of testes and bones of goat to treat male reproductive [92] and bone [93] ailments, respectively. Geographic accessibility was one of the important factors that determined the popularity of zootherapy [94]; this study also represented that the accessibility of marine taxa caused more UR for them among the animal-based foods. Deb and Haque [95] documented the importance of fish taxa in the culture of people in coastal region; however, the ethnopharmacology of fish taxa in India still has to be documented thoroughly. Various medicinal properties of molluscs were recently reviewed [96]; this study documented the use of two molluscs viz., Katelysia opima and Indian squid for the treatment of impotence and anemia, respectively. Indian oil sardine has high ω-3 fatty acid content, high ω-3/ω-6 ratio, eicosapentaenoic acid, and docosahexaenoic acid [97], which may help to gain healthy weight.
The use of spade nose shark to improve lactation had got high UR and IAR under gynecological ailments; however, no scientific report is available to validate this claim. The study by Deb and Haque [95] documented the use of catla as lactogogue, Anguilla bengalensis bengalensis for the treatment of arthritis, and Channa spp., for oligospermia. They also documented reticulate whipray as lactogogue and for the treatment of dysentery; this survey documented its usefulness to treat wheezing and bronchitis.
Conclusions
This preliminary report quantitatively documented the food-medicine continuum among the non-institutionally trained siddha practitioners of Tiruvallur district. Collectivistic cultures, influence of traditional norms, and medicinal beliefs caused Indian dietary habits to be very unique; this provides ample scope for further research to anthropologists and ethnobiologists. Deeper studies on different dietary cultures of India may help derive better interpretations on food-medicine continuum.
This study identified some important plant-based medicinal claims such as citron, pomegranate and Solanum americanum (gastrointestinal ailments), Abutilon indicum, onions and elephant foot yam (hemorrhoids), Boerhavia diffusa (urinary ailments), Moringa oleifera (anemia), Aloe vera (gynecological ailments), Eclipta prostrata (liver ailments), ivy gourd (diabetes), citron (hypertension), and Centella asiatica (psychological ailments). More studies on these claims will help identify novel functional foods to add to the field of medical nutrition therapy, with traditional brand identity.
This study also documented some important marine animal taxa such as spade nose shark (lactogogue), reticulate whipray (wheezing and bronchitis), Katelysia opima (impotence), Indian squid (anemia), and Indian oil sardine (anabolic) for the treatment of various illnesses. Generally, ethnopharmacological validations on ethnozoological claims are very meager and Indian marine resources are still under-utilized. Scientific studies on these claims may yield some novel and affordable functional foods.
Documentation of ethnopharmacological knowledge of marine resources is comparatively low in India. Indian coastal line spreads over 7516 km, and robust studies on the documentation of the traditional knowledge on marine resources will yield a good database for various stakeholders and policy makers.
Among zootherapy, the use of organs to treat illnesses of similar organs was documented in many instances. Future-specific studies will reveal the cultural and pharmacological importance of this claim.
Additional file
Table S1. List of medicinal foods prescribed by the non-institutionally trained siddha practitioners of Tiruvallur district of Tamil Nadu. The taxa given in bold emphasis are mentioned as the key taxa for the reported medicinal activity of the food by the informants. The values given within the parentheses indicate the number of the UR for the respective illness. Table S2. Cultural Food Significance Index of the plant and animal taxa cited by the non-institutionally trained siddha practitioners of Tiruvallur district of Tamil Nadu for preparing medicinal foods. Taxa having a minimum of two UR were taken for the analysis. AI Availability Index, QI Quotation Index, UFI Utilization Frequency Index, PUI Parts Used Index, MFFI Multi-Functional Food Use Index, TASI Taste Score Appreciation Index, FMRI Food-Medicinal Role Index, CFSI Cultural Food Significance Index (DOCX 74 kb).
Acknowledgements
The authors acknowledge the non-institutionally trained siddha practitioners of Tiruvallur district for sharing their valuable knowledge. The authors thank the three anonymous reviewers for their comments which helped extensively to improve the quality of our manuscript.
Funding
The authors are grateful to Loyola College - Times of India Research Grant (sanction number 7LCTOIERI004) for the partial financial support. We also extend our appreciation to the International Scientific Partnership Program (ISPP) at King Saud University for partially funding this research work through ISPP#0020.
Availability of data and materials
All the data generated in this study are included with this article. Field notebooks and herbarium specimens were available at the museum of Entomology Research Institute, Loyola College, Chennai, Tamil Nadu, 600034, India.
Abbreviations
- AI
Availability index
- CFSI
Cultural Food Significance Index
- FIC
Informant Consensus Factor
- FMRI
Food Medicinal Role Index
- FUI
Frequency of use index
- IAR
Index of Agreement on Remedies
- MFFI
Multifunctional food use index
- na
Number of illness categories treated with that taxon
- Nt
Number of taxa
- Nur
Number of UR
- nur
Number of UR registered for taxa
- PUI
Part used index
- QI
Quotation index
- RFC
Relative Frequency of Citation
- TSAI
Taste Score Appreciation Index
- UR
Use report
Authors’ contributions
SI, PP, and NAA conceived the idea and designed the study. SE, SD, SM, PP, and MGP were involved in the field study and species confirmation. SE, SI, PP, and NAA processed and analyzed the data and prepared the manuscript. All the authors read and approved the manuscript.
Ethics approval and consent to participate
This study is approved by the Institutional Ethics Committee for Ethnobiological Research (sanction number ERI/IEEC/2014/01). Written informant consent was obtained from all informants who were willing to participate.
Consent for publication
Consent for publication was obtained from the informants.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s13002-018-0240-9) contains supplementary material, which is available to authorized users.
Contributor Information
S. Esakkimuthu, Email: esakkimuthu541991@gmail.com
S. Sylvester Darvin, Email: darvin.dsc@gmail.com
S. Mutheeswaran, Email: muthees2009@gmail.com
M. Gabriel Paulraj, Email: gabriel_paulraj@yahoo.com
P. Pandikumar, Phone: +91-44-2817 8348, Email: pkr_eri@hotmail.com
S. Ignacimuthu, Phone: +91-44-2817 8348, Email: eriloyola@hotmail.com
N. A. Al-Dhabi, Email: naldhabi@ksu.edu.sa
References
- 1.Jennings HM, Merrell J, Thompson JL, Heinrich M. Food or medicine? The food-medicine interface in households in Sylhet. J Ethnopharmacol. 2014;167:97–104. doi: 10.1016/j.jep.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Sansanelli S, Ferri M, Salinitro M, Tassoni A. Ethnobotanical survey of wild food plants traditionally collected and consumed in the Middle Agri Valley (Basilicata region, southern Italy) J Ethnobiol Ethnomed. 2017;13:50. doi: 10.1186/s13002-017-0177-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arnason T, Hebda RJ, Johns T. Use of plants for food and medicine by native peoples of eastern Canada. Can J Bot. 1981;59:2189–2325. doi: 10.1139/b81-287. [DOI] [Google Scholar]
- 4.Timothy DJ, Ron AS. Heritage cuisines, regional identity and sustainable tourism. In: Hall CM, Gossling S, editors. Sustainable Culinary Systems: Local Foods, Innovation, Tourism and Hospitality. London: Routledge; 2013. pp. 275–290. [Google Scholar]
- 5.Iwu MM. Embrical investigations of dietary plants used in Igbo ethnomedicine. In: Etkin NL, editor. Plants in Indigenous Medicine and Diet. New York: Biobehavioral approaches, Redgrave Publishing Company; 1986. pp. 131–150. [Google Scholar]
- 6.Etkin NL, Ross PJ. Should we set a place for diet in ethnopharmacology? J Ethnopharmacol. 1991;32:25–36. doi: 10.1016/0378-8741(91)90100-R. [DOI] [PubMed] [Google Scholar]
- 7.Alarcon R, Pardo-de-Santayana M, Priestley C, Morales R, Heinrich M. Medicinal and local food plants in the south of Alava (Basque Country, Spain) J Ethnopharmacol. 2015;176:207–224. doi: 10.1016/j.jep.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Towns AM, van Andel T. Wild plants, pregnancy, and the food-medicine continuum in the southern regions of Ghana and Benin. J Ethnopharmacol. 2016;179:375–382. doi: 10.1016/j.jep.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Mohan V, Radhica G, Vijayalakshmi P, Sudha V. Can the diabetes/cardio-vascular disease epidemic in India be explained, at least in part, by excess refined grain (rice) intake? Indian J Med Res. 2010;131:369–372. [PubMed] [Google Scholar]
- 10.Jain A, Rakhi NK, Bagler G. Analysis of food pairing in regional cuisines of India. PLoS One. 2015;10:e0139539. doi: 10.1371/journal.pone.0139539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarkar P, Kumar DHL, Dhumal C, Panigrahi SS, Choudhary R. Traditional and ayurvedic foods of Indian origin. J Ethnic Foods. 2015;2:97–109. doi: 10.1016/j.jef.2015.08.003. [DOI] [Google Scholar]
- 12.Mutheeswaran S, Esakkimuthu S, Pandikumar P, Ignacimuthu S, Al-Dhabi NA. Quantification of ethnodietetic knowledge among noninstitutionally trained Siddha practitioners of Virudhunagar District, Tamil Nadu, India. J Ethnic Foods. 2016;3:263–269. doi: 10.1016/j.jef.2016.11.007. [DOI] [Google Scholar]
- 13.Anonymous . Aṟputa Cintāmaṇi eṉṉum Patārtta Kuṇa Cintāmaṇi (mūlamum uraiyum) Chennai: B. Rathina nayagar & Sons; 1932. [Google Scholar]
- 14.World Health Organization, Food and Agriculture Organization of the United Nations . Diet, Nutrition and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation (WHO Technical Report Series 916) Geneva: World Health Organization; 2003. [PubMed] [Google Scholar]
- 15.Keatinge JDH, Waliyar F, Jamnadass RH, Moustafa A, Andrade M, Drechsel P, Hughes JA, Kadirvel P, Luther K. Relearning old lessons for the future of food by bread alone no longer: diversifying diets with fruit and vegetables. Crop Sci. 2010;50:S51–S62. doi: 10.2135/cropsci2009.09.0528. [DOI] [Google Scholar]
- 16.Bigliardi B, Galati F. Innovation trends in the food industry: the case of functional foods. Trends Food Sci Technol. 2013;31:118–129. doi: 10.1016/j.tifs.2013.03.006. [DOI] [Google Scholar]
- 17.Cencic A, Chingwaru W. The role of functional foods, nutraceuticals, and food supplements in intestinal health. Nutrients. 2010;2:611–625. doi: 10.3390/nu2060611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozen AE, Pons A, Tur JA. Worldwide consumption of functional foods: a systematic review. Nutr Res. 2012;70:472–481. doi: 10.1111/j.1753-4887.2012.00492.x. [DOI] [PubMed] [Google Scholar]
- 19.De Boer A, Hunsel F, Bast A. Adverse food-drug interactions. Regul Toxicol Pharmacol. 2015;73:859–865. doi: 10.1016/j.yrtph.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Mouly S, Lloret-Linares C, Sellier PO, Sene D, Bergmann JF. Is the clinical relevance of drug-food and drug-herb interactions limited to grapefruit juice and Saint-John’s Wort? Pharmacol Res. 2017;118:82–92. doi: 10.1016/j.phrs.2016.09.038. [DOI] [PubMed] [Google Scholar]
- 21.Mutheeswaran S, Pandikumar P, Chellappandian M, Ignacimuthu S, Duraipandiyan V, Logamanian M. Consensus analysis of sastric formulations used by the non-institutionally trained Siddha medical practitioners of Virudhunagar and Tirunelveli districts of Tamil Nadu, India. J Ethnopharmacol. 2014;153:290–296. doi: 10.1016/j.jep.2014.02.043. [DOI] [PubMed] [Google Scholar]
- 22.Zysk KG. Siddha medicine in Tamil Nadu. Kobenhavn: Nationalmuseets Tranquebar Initiative; 2008. [Google Scholar]
- 23.Sebastia B. Governmental Institutions vs. Associations: The Multifaceted Expression of Siddha Medicine in Tamil Nadu. Available from: https://halshs.archives-ouvertes.fr/halshs-00408677/document. Accessed: 02 Nov 2017.
- 24.WHO . WHO Country Cooperation Strategy 2006–2011. Supplement on Traditional Medicine. New Delhi: WHO country office for India; 2007. [Google Scholar]
- 25.Esakkimuthu S, Mutheeswaran S, Arvinth S, Gabriel Paulraj M, Pandikumar P, Ignacimuthu S. Quantitative ethnomedicinal survey of medicinal plants given for cardiometabolic diseases by the noninstitutionally trained siddha practitioners of Tiruvallur district, Tamil Nadu, India. J Ethnopharmacol. 2016;186:329–342. doi: 10.1016/j.jep.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 26.Alexiades MN, Sheldon JW, editors. Selected guidelines for ethnobotanical research: a field manual. New York: New York Botanical Gardens; 1996. [Google Scholar]
- 27.Bernard RH. Research Methods in Anthropology. Qualitative and Quantitative Approaches. 4. Walnut Creek: Altamira Press; 2006. [Google Scholar]
- 28.Heinrich M, Edwards S, Moerman DE, Leonti M. Ethnopharmacological field studies: a critical assessment of their conceptual basis and methods. J Ethnopharmacol. 2009;124:1–17. doi: 10.1016/j.jep.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 29.Weckerle CS, de Boer HJ, Puri RK, Andel T, Bussmann RW, Leonti M. Recommended standards for conducting and reporting ethnopharmacological field studies. J Ethnopharmacol. 2018;210:125–132. doi: 10.1016/j.jep.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 30.International Society of Ethnobiology. International Society of Ethnobiology Code of Ethics (with 2008 additions). http://ethnobiology.net/code-of-ethics/. Accessed: 15 Oct 2014.
- 31.Gamble JS. The Flora of the Presidency of Madras, vol. I–III (reprinted ed). Dehradun, India: Bishen Singh Mahendhra Pal Singh, 1997.
- 32.Nair NC, Henry AN. Flora of Tamil Nadu, India, Vol. I., Botanical Survey of India. Coimbatore: Southern Circle; 1983. [Google Scholar]
- 33.Henry AN, Kumari GR, Chithra V. Flora of Tamil Nadu, India, Vol. II. Botanical Survey of India. Coimbatore: Southern Circle; 1987. [Google Scholar]
- 34.Henry AN, Chithra V, Balakrishnan NP. Flora of Tamil Nadu, India, Vol. III. Botanical Survey of India. Coimbatore: Southern Circle; 1989. [Google Scholar]
- 35.The Plant List; 2010). Version 1.1. Published on the Internet; http://www.theplantlist.org/. Accessed 02 Nov 2017
- 36.Kufer J, Forther H, Poll E, Heinrich M. Historical and modern medicinal plant uses-the example of the Ch’orti’ Maya and Ladinos in eastern Guatemala. J Pharm Pharmacol. 2005;57:1127–1152. doi: 10.1211/jpp.57.9.0008. [DOI] [PubMed] [Google Scholar]
- 37.Chellappandian M, Mutheeswaran S, Pandikumar P, Duraipandiyan V, Ignacimuthu S. Quantitative ethnobotany of traditional Siddha medical practitioners from Radhapuram taluk of Tirunelveli District, Tamil Nadu, India. J Ethnopharmacol. 2012;143:540–547. doi: 10.1016/j.jep.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 38.Trotter R, Logan M. Informant consensus: a new approach for identifying potentially effective medicinal plants. In: Etkin NL, editor. Plants in Indigenous Medicine and Diet: Biobehavioural Approaches. Bedfort Hills, NY: Redgrave Publishers; 1986. pp. 91–112. [Google Scholar]
- 39.Moerman DE. North American Food and Drug Plants. In: Etkin NL, editor. Eating on the Wild Side. Tucson, Arizona: The University of Arizona Press; 1994. pp. 1–21. [Google Scholar]
- 40.Pandikumar P, Chellappandian M, Mutheeswaran S, Ignacimuthu S. Consensus of local knowledge on medicinal plants among traditional healers in Mayiladumparai block of Theni District, Tamil Nadu, India. J Ethnopharmacol. 2011;134:354–362. doi: 10.1016/j.jep.2010.12.027. [DOI] [PubMed] [Google Scholar]
- 41.Mudaliar KSM. Siddha Materia Medica––Plant Kingdom. Chennai, India: Department of Indian Medicine and Homeopathy; 1936. [Google Scholar]
- 42.Pillai CK. Siddha Materia Medica – Plant Kingdom. Chennai, India: B. Rathina nayagar & Sons. 1939.
- 43.Pillai CK. Siddha Materia Medica––Animal Kingdom. Chennai, India: B. Rathina nayagar & Sons; 1941. [Google Scholar]
- 44.Thiagarajan R. Siddha Materia Medica––Animal Kingdom. Chennai, India: Department of Indian Medicine and Homeopathy; 1989. [Google Scholar]
- 45.Pieroni A. Evaluation of the cultural significance of wild food botanicals consumed in northwestern Tuscany. Italy J Ethnobiol. 2001;21:89–104. [Google Scholar]
- 46.Sebastia B. Coping with diabetic patients in Tamil Nadu. Case study of two traditional siddha practitioners. 2011. [Google Scholar]
- 47.Mati E, De Boer HJ. Trade and commercialization of herbal medicine in the Qaysari market, Kurdish Autonomous Region. Iraq J Ethnopharmacol. 2011;133:490–510. doi: 10.1016/j.jep.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 48.Thorsen RS, Pouliot M. Traditional medicine for the rich and knowledgeable: challenging assumptions about treatment-seeking behaviour in rural and peri-urban Nepal. Health Policy Plan. 2016;31:314–324. doi: 10.1093/heapol/czv060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Araujo TA, Almeida AL, Melo JG, Medeiros MF, Ramos MA, Silva RR, Almeida CF, Albuquerque UP. A new technique for testing distribution of knowledge and to estimate sampling sufficiency in ethnobiology studies. J Ethnobiol Ethnomed. 2012;8:11. doi: 10.1186/1746-4269-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Manohar R, Kessler CS. Ayurveda’s contributions to vegetarian nutrition in medicine. Forsch Komplementmed. 2016;23:89–94. doi: 10.1159/000445400. [DOI] [PubMed] [Google Scholar]
- 51.Chellappandian M, Pandikumar P, Mutheeswaran S, Paulraj MG, Prabakaran S, Duraipandiyan V, Ignacimuthu S, Al-Dhabi NA. Documentation and quantitative analysis of local ethnozoological knowledge among traditional healers of Theni district, Tamil Nadu, India. J Ethnopharmacol. 2014;154:116–130. doi: 10.1016/j.jep.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 52.Kadir MF, Sayeed MSB, Mia MM. Ethnopharmacological survey of medicinal plants used by traditional healers in Bangladesh for gastrointestinal disorders. J Ethnopharmacol. 2013;147:148–156. doi: 10.1016/j.jep.2013.02.023. [DOI] [PubMed] [Google Scholar]
- 53.Acker BW, Cash BD. Medicinal foods for functional GI disorders. Curr Gastroenterol Rep. 2017;19:62. doi: 10.1007/s11894-017-0601-x. [DOI] [PubMed] [Google Scholar]
- 54.Ciampa BP, Ramos RE, Borum M, Doman DB. The emerging therapeutic role of medical foods for gastrointestinal disorders. Gastroenterol Hepatol (NY) 2017;13:104–115. [PMC free article] [PubMed] [Google Scholar]
- 55.Jaiswal Y, Liang Z, Zhao Z. Botanical drugs in Ayurveda and traditional Chinese medicine. J Ethnopharmacol. 2016;194:245–259. doi: 10.1016/j.jep.2016.06.052. [DOI] [PubMed] [Google Scholar]
- 56.Rokaya MB, Uprety Y, Poudel RC, Timsina B, Munzbergova Z, Asselin H, Tiwari A, Shrestha SS, Sigdel SR. Traditional uses of medicinal plants in gastrointestinal disorders in Nepal. J Ethnopharmacol. 2014;158:221–229. doi: 10.1016/j.jep.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 57.Zaidi SF, Muhammad JS, Shahryar S, Usmanghani K, Gilani AH, Jafri W, Sugiyama T. Anti-inflammatory and cytoprotective effects of selected Pakistani medicinal plants in Helicobacter pylori-infected gastric epithelial cells. J Ethnopharmacol. 2012;141:403–410. doi: 10.1016/j.jep.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 58.Kurklu-Gurleyen E, Ogut-Erisen M, Cakir O, Uysal O, Ak G. Quality of life in patients with recurrent aphthous stomatitis treated with a mucoadhesive patch containing citrus essential oil. Patient Prefer Adherence. 2016;10:967–973. doi: 10.2147/PPA.S106530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mandalari G, Bisignano C, Cirmi S, Navarra M. Effectiveness of Citrus Fruits on Helicobacter pylori. Evid Based Complement Altern Med. 2017; Article ID: 8379262. [DOI] [PMC free article] [PubMed]
- 60.Li W, Wang X, Zhi W, Zhang H, He Z, Wang Y, Liu F, Niu X, Zhang X. The gastroprotective effect of nobiletin against ethanol-induced acute gastric lesions in mice: impact on oxidative stress and inflammation. Immunopharmacol Immunotoxicol. 2017;39(6):354–363. doi: 10.1080/08923973.2017.1379088. [DOI] [PubMed] [Google Scholar]
- 61.Hamdan DI, Mahmoud MF, Wink M, El-Shazly AM. Effect of hesperidin and neohesperidin from bittersweet orange (Citrus aurantium var. bigaradia) peel on indomethacin-induced peptic ulcers in rats. Environ Toxicol Pharmacol. 2014;37(3):907–915. doi: 10.1016/j.etap.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 62.Bonamin F, Moraes TM, dos Santos RC, Kushima H, Faria FM, Silva MA Junior IV, Nogueira L, Bauab TM, Brito ARS. The effect of a minor constituent of essential oil from Citrus aurantium: the role of β-myrcene in preventing peptic ulcer disease. Chem Boil Interact. 2014;212:11–19. doi: 10.1016/j.cbi.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 63.Rozza AL, Moraes TM, Kushima H, Tanimoto A, Marques MOM, Bauab TM, Hiruma-Lima CA, Pellizzon CH. Gastroprotective mechanisms of Citrus lemon (Rutaceae) essential oil and its majority compounds limonene and β-pinene: involvement of heat-shock protein-70, vasoactive intestinal peptide, glutathione, sulfhydryl compounds, nitric oxide and prostaglandin E2. Chem Biol Int. 2011;189(1):82–89. doi: 10.1016/j.cbi.2010.09.031. [DOI] [PubMed] [Google Scholar]
- 64.Sood S, Muthuraman A, Gill NS, Bali M, Sharma PD. Role of 7, 8-dimethoxycoumarin in anti-secretary and anti-inflammatory action on pyloric ligation-induced gastritis in rats. J Asian Nat Prod Res. 2010;12:593–599. doi: 10.1080/10286020.2010.486377. [DOI] [PubMed] [Google Scholar]
- 65.Mazumder PM, Sasmal D, Nambi RA. Antiulcerogenic and antioxidant effects of Coccinia grandis (Linn.) Voigt leaves on aspirin-induced gastric ulcer in rats. Indian J Nat Prod Res. 2008;7(1):15–18. [Google Scholar]
- 66.Rao USM, Ahmad B, Mohd KS, Zin T. Antiulcer activity of Musa paradisiaca (banana) tepal and skin extracts in ulcer induced albino mice. Malaysian J Analytical Sci. 2016;20(5):1203–1216. doi: 10.17576/mjas-2016-2005-27. [DOI] [Google Scholar]
- 67.Calzada F, Yepez-Mulia L, Aguilar A. In vitro susceptibility of Entamoeba histolytica and Giardia lamblia to plants used in Mexican traditional medicine for the treatment of gastrointestinal disorders. J Ethnopharmacol. 2006;108:367–370. doi: 10.1016/j.jep.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 68.Ouelbani R, Bensari S, Mouas TN, Khelifi D. Ethnobotanical investigations on plants used in folk medicine in the regions of Constantine and Mila (North-East of Algeria) J Ethnopharmacol. 2016;194:196–218. doi: 10.1016/j.jep.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 69.Jain RAS, Gupta SSPI, Gabrani R. Solanum nigrum: current perspectives on therapeutic properties. Altern Med Rev. 2011;16:78–85. [PubMed] [Google Scholar]
- 70.Nasab KF, Khosravi AR. Ethnobotanical study of medicinal plants of Sirjan in Kerman Province, Iran. J Ethnopharmacol. 2014;154:190–197. doi: 10.1016/j.jep.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 71.Johns T, Faubert GM, Kokwaro JO, Mahunnah RL, Kimanani EK. Anti-giardial activity of gastrointestinal remedies of the Luo of East Africa. J Ethnopharmacol. 1995;46:17–23. doi: 10.1016/0378-8741(95)01224-2. [DOI] [PubMed] [Google Scholar]
- 72.Mutheeswaran S, Pandikumar P, Chellappandian M, Ignacimuthu S. Documentation and quantitative analysis of the local knowledge on medicinal plants among traditional Siddha healers in Virudhunagar district of Tamil Nadu, India. J Ethnopharmacol. 2011;137:523–533. doi: 10.1016/j.jep.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 73.Kasote DM, Jagtap SD, Thapa D, Khyade MS, Russell WR. Herbal remedies for urinary stones used in India and China: a review. J Ethnopharmacol. 2017;203:55–68. doi: 10.1016/j.jep.2017.03.038. [DOI] [PubMed] [Google Scholar]
- 74.Patil KS, Bhalsing SR. Ethnomedicinal uses, phytochemistry and pharmacological properties of the genus Boerhavia. J Ethnopharmacol. 2016;182:200–220. doi: 10.1016/j.jep.2016.01.042. [DOI] [PubMed] [Google Scholar]
- 75.Gopalakrishnan L, Doriya K, Kumar DS. Moringa oleifera: a review on nutritive importance and its medicinal application. Food Sci Human Wellness. 2016;5:49–56. doi: 10.1016/j.fshw.2016.04.001. [DOI] [Google Scholar]
- 76.Saini RK, Manoj P, Shetty NP. Dietary iron supplements and Moringa oleifera leaves influence the liver hepcidin messenger RNA expression and biochemical indices of iron status in rats. Nutr Res. 2014;34:630–638. doi: 10.1016/j.nutres.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 77.Jadhav AN, Bhutani KK. Ayurveda and gynecological disorders. J Ethnopharmacol. 2005;97:151–159. doi: 10.1016/j.jep.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 78.Maggioni L, Bothmer R, Poulsen G, Lipman E. Domestication, diversity and use of Brassica oleracea L., based on ancient Greek and Latin texts. Genet Resour Crop Evol. 2018;65:137–159. doi: 10.1007/s10722-017-0516-2. [DOI] [Google Scholar]
- 79.Jung HA, Karki S, Ehom N, Yoon M, Kim EJ, Choi JS. Anti-diabetic and anti-inflammatory effects of green and red kohlrabi cultivars (Brassica oleracea var. gongylodes) Prev Nutr Food Sci. 2014;19:281–290. doi: 10.3746/pnf.2014.19.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bahadoran Z, Tohidi M, Nazeri P, Mehran M, Azizi F, Mirmiran P. Effect of broccoli sprouts on insulin resistance in type 2 diabetic patients: a randomized double-blind clinical trial. Int J Food Sci Nutr. 2012;63:767–771. doi: 10.3109/09637486.2012.665043. [DOI] [PubMed] [Google Scholar]
- 81.Teixeira CC, Fuchs FD, Weinert LS, Esteves J. The efficacy of folk medicines in the management of type 2 diabetes mellitus: results of a randomized controlled trial of Syzygium cumini (L.) Skeels. J Clin Pharm Ther. 2006;31(1):1–5. doi: 10.1111/j.1365-2710.2006.00700.x. [DOI] [PubMed] [Google Scholar]
- 82.Sathasivampillai SV, Rajamanoharan PRS, Munday M, Heinrich M. Plants used to treat diabetes in Sri Lankan Siddha Medicine––an ethnopharmacological review of historical and modern sources. J Ethnopharmacol. 2017;198:531–599. doi: 10.1016/j.jep.2016.07.053. [DOI] [PubMed] [Google Scholar]
- 83.Kadir MF, Bin Sayeed MS, Shams T, Mia MM. Ethnobotanical survey of medicinal plants used by Bangladeshi traditional health practitioners in the management of diabetes mellitus. J Ethnopharmacol. 2012;144:605–611. doi: 10.1016/j.jep.2012.09.050. [DOI] [PubMed] [Google Scholar]
- 84.Yaseen G, Ahmad M, Zafar M. Traditional management of diabetes in Pakistan: ethnobotanical investigation from traditional health practitioners. J Ethnopharmacol. 2015;174:91–117. [DOI] [PubMed]
- 85.Munasinghe MA, Abeysena C, Yaddehige IS, Vidanapathirana T, Piyumal KP. Blood sugar lowering effect of Coccinia grandis (L.) J. Voigt: path for a new drug for diabetes mellitus. Exp Diabetes Res. 2011; Article ID: 978762. [DOI] [PMC free article] [PubMed]
- 86.Prabhu S, Jainu M, Sabitha KE, Devi CSS. Effect of mangiferin on mitochondrial energy production in experimentally induced myocardial infarcted rats. Vasc Pharmacol. 2006;44:519–525. doi: 10.1016/j.vph.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 87.Chhikara N, Kour R, Jaglan S, Gupta P, Gata Y, Panghal A. Citrus medica: nutritional, phytochemical composition and health benefits––a review. Food Funct. 2018;9:1978–1992. doi: 10.1039/C7FO02035J. [DOI] [PubMed] [Google Scholar]
- 88.Kujawska M, Pieroni A. Plants used as food and medicine by polish migrants in Misiones, Argentina. Ecol Food Nutr. 2015;54:255–279. doi: 10.1080/03670244.2014.983498. [DOI] [PubMed] [Google Scholar]
- 89.Bradwejn J, Zhou Y, Kosycki D, Shlik J. A double blind, placebo-controlled study on the effects of Gotu Kola (Centella asiatica) on acoustic startle response in healthy subjects. J Clin Psychopharmacol. 2000;20:680–684. doi: 10.1097/00004714-200012000-00015. [DOI] [PubMed] [Google Scholar]
- 90.Jana U, Sur TK, Maity LN. A clinical study on the management of generalized anxiety disorder with Centella asiatica. Nepal Med Coll J. 2010;12:8–11. [PubMed] [Google Scholar]
- 91.Gonzalez JA, Vallejo JR. The scorpion in Spanish folk medicine: a review of traditional remedies for stings and its use as a therapeutic resource. J Ethnopharmacol. 2013;146:62–74. doi: 10.1016/j.jep.2012.12.033. [DOI] [PubMed] [Google Scholar]
- 92.Kim G, Kim H, Song M-J. Ethnopharmacological implications of quantitative and network analysis for traditional knowledge regarding the medicinal use of animals by indigenous people in Wolchulsan National Park, Korea. J Ethnopharmacol. 2018;213:1–11. doi: 10.1016/j.jep.2017.10.033. [DOI] [PubMed] [Google Scholar]
- 93.Mootoosamy A, Mahomoodally MF. A quantitative ethnozoological assessment of traditionally used animal-based therapies in the tropical island of Mauritius. J Ethnopharmacol. 2014;154:847–857. doi: 10.1016/j.jep.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 94.Alves RRN, Rosa IL. Zootherapeutic practices among fishing communities in North and Northeast Brazil: a comparison. J Ethnopharmacol. 2007;111:82–103. doi: 10.1016/j.jep.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 95.Deb AK, Haque CE. Every mother is a mini-doctor: ethnomedicinal uses of fish, shellfish and some other aquatic animals in Bangladesh. J Ethnopharmacol. 2011;134:259–267. doi: 10.1016/j.jep.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 96.Ahmad TB, Liu L, Kotiw M, Benkendorff K. Review of anti-inflammatory, immune-modulatory and wound healing properties of molluscs. J Ethnopharmacol. 2018;210:156–178. doi: 10.1016/j.jep.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 97.Mohanty BP, Mahanty A, Ganguly S, Mitraa T, Karunakarana D, Anandan R. Nutritional composition of food fishes and their importance in providing food and nutritional security. Food Chem. 2017; 10.1016/j.foodchem.2017.11.039. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. List of medicinal foods prescribed by the non-institutionally trained siddha practitioners of Tiruvallur district of Tamil Nadu. The taxa given in bold emphasis are mentioned as the key taxa for the reported medicinal activity of the food by the informants. The values given within the parentheses indicate the number of the UR for the respective illness. Table S2. Cultural Food Significance Index of the plant and animal taxa cited by the non-institutionally trained siddha practitioners of Tiruvallur district of Tamil Nadu for preparing medicinal foods. Taxa having a minimum of two UR were taken for the analysis. AI Availability Index, QI Quotation Index, UFI Utilization Frequency Index, PUI Parts Used Index, MFFI Multi-Functional Food Use Index, TASI Taste Score Appreciation Index, FMRI Food-Medicinal Role Index, CFSI Cultural Food Significance Index (DOCX 74 kb).
Data Availability Statement
All the data generated in this study are included with this article. Field notebooks and herbarium specimens were available at the museum of Entomology Research Institute, Loyola College, Chennai, Tamil Nadu, 600034, India.