Abstract
One purpose of this study was to determine the cumulative rates of excellent recovery for borderline patients and axis II comparison subjects followed prospectively for 20 years. Another purpose was to find the best set of baseline predictors of excellent recovery for borderline patients. A total of 290 inpatients meeting rigorous criteria for borderline personality disorder and 72 axis II comparison subjects completed semistructured interviews and self-report measures during their index admission. Subjects were reassessed prospectively over 10 contiguous two-year waves of follow-up. Thirty-nine percent of borderline patients and 73% of personality-disordered comparison subjects met our operationalized definition of excellent recovery (concurrent remission of borderline or another primary personality disorder, good social and full-time vocational functioning, and absence of an axis I disorder associated decreased social and/or vocational functioning). Five variables formed our multivariate predictive model of excellent recovery for borderline patients: higher IQ, good childhood work history, good adult vocational record, lower trait neuroticism, and higher trait agreeableness. The results of this study suggest that complete recovery is difficult for borderline patients to achieve even over long periods of time. They also suggest that competence displayed in both childhood and adulthood is the best predictor of this important outcome.
1. Introduction
Four large-scale follow-back studies of the long-term course of borderline personality disorder were conducted in the 1980s (McGlashan, 1986; Paris et al., 1987; Plakun et al., 1985; Stone, 1990). They each found that borderline patients, who were diagnosed by retrospective chart review, were, on average, functioning reasonably well a mean of 14-16 years after their index admission. More specifically, subjects in these studies were rated as having either a mean Health Sickness Rating Scale score (Luborsky, 1962) or a mean Global Assessment Score (Endicott et al., 1976) of 63-67 (i.e., a score in the good range).
NIMH funded two prospective studies of the long-term course of borderline personality disorder in the 1990s that addressed some of the methodological limitations inherent in the follow-back design of these older studies. The McLean Study of Adult Development, which began in 1992, followed these earlier studies from the 1980s by using a Global Assessment of Functioning (GAF) score of 61 or higher to denote a good recovery. However, such a good recovery was operationalized to require a concurrent remission of borderline personality disorder and good social functioning as well as good full-time vocational functioning. It was found that 50% of borderline patients achieved this outcome after 10 years of prospective follow-up (Zanarini et al., 2010) and 60% achieved this outcome after 16 years of prospective follow-up (Zanarini et al., 2012). It was also found that 84% of axis II comparison subject achieved this outcome after 10 years of prospective follow-up and 85% achieved this outcome after 16 years of prospective follow-up (Zanarini et al., 2010; Zanarini et al., 2012).
The Collaborative Longitudinal Personality Disorders Study began four years after the McLean Study of Adult Development (Gunderson et al., 2011). A GAF score of 71 or higher was chosen to represent a good global outcome. However, this score was not operationalized but rather relied on the scale’s brief narrative definition. After 10 years of prospective follow-up, it was found that 21% of borderline patients met this outcome. It was also found that 48% of subjects in a comparison group with an avoidant and/or obsessive-compulsive personality disorder were rated as having a GAF score in this range.
In terms of predictors, each of the follow-back studies (Paris et al., 1987; Stone, 1990; McGlashan, 1985; Plakun, 1991; Paris et al., 1988) tried to determine the best predictors of general outcome a mean of 14-16 years after index admission. Five factors were found to be associated with a good long-term outcome: high IQ (Stone, 1990; McGlashan, 1985), being unusually talented or physically attractive (if female) (Stone 1990), the absence of parental divorce and narcissistic entitlement (Plakun, 1991), and the presence of physically self-destructive acts during the index admission (McGlashan, 1985). Nine factors were found to be associated with a poor long-term outcome: affective instability (McGlashan, 1985), chronic dysphoria (Paris et al., 1987), younger age at first treatment (Paris et al., 1987), length of prior hospitalization (McGlashan, 1985), antisocial behavior (Stone, 1990), substance abuse (Stone, 1990), parental brutality (Stone, 1990), a family history of psychiatric illness (Paris et al., 1987), and a problematic relationship with one’s mother (but not one’s father) (Paris et al., 1988).
At 16-year follow-up, the McLean Study of Adult Development studied the best predictors of a good recovery (Zanarini et al., 2014). Variables related to lack of chronicity, temperament, and adult competence were the best multivariate predictors of this outcome.
The current study examined rates of good and excellent recovery achieved by both borderline patients and axis II comparison subjects over 20 years of prospective follow-up—two different definitions of recovery that may have different clinical implications. It also examined the relationship between a wide array of clinically relevant predictor variables assessed at baseline and time-to-excellent recovery in borderline patients, which was assessed at 10 contiguous two-year time periods. In addition, the sample of borderline patients being studied is large, carefully diagnosed, and socioeconomically diverse.
2. Method
As noted above, the current study is part of the McLean Study of Adult Development, a multifaceted longitudinal study of the course of borderline personality disorder. The methodology of this study, which was reviewed and approved by the McLean Hospital Institutional Review Board, has been described in detail elsewhere (Zanarini et al., 2003). Briefly, all subjects were initially inpatients at McLean Hospital in Belmont, Massachusetts. Each patient was screened to determine that he or she was between the ages of 18-35; had a known or estimated IQ of 71 or higher; and had no history or current symptomatology of schizophrenia, schizoaffective disorder, bipolar I disorder, or an organic condition (e.g., lupus, MS) that could cause serious psychiatric symptoms.
After the study procedures were explained, written informed consent was obtained. Each patient then met with a masters-level interviewer blind to the patient’s clinical diagnoses for a thorough psychosocial and treatment history as well as diagnostic assessment. Four semistructured interviews were administered. These interviews were: 1) the Background Information Schedule (Zanarini, 1992), 2) the Structured Clinical Interview for DSM-III-R Axis I Disorders (Spitzer et al., 1992), 3) the Revised Diagnostic Interview for Borderlines (Zanarini et al., 1989a), and 4) the Diagnostic Interview for DSM-III-R Personality Disorders (Zanarini et al., 1987). The inter-rater and test-retest reliability of the Background Information Schedule (Zanarini et al., 2004a; 2005) and of the three diagnostic measures (Zanarini et al., 2001; 2002) have all been found to be good-excellent.
Childhood history of pathological and protective experiences was assessed during each subject’s index admission using a semistructured interview by a second rater blind to all previously collected information–the Revised Childhood Experiences Questionnaire (Zanarini et al., 1989b). The inter-rater reliability of this interview has also been found to be good-excellent (Zanarini et al., 1989b). In addition, self-report measures with well-established psychometric properties assessing temperament and intelligence were administered: the NEO Five Factor Inventory (Costa et al., 1992) and the Shipley Institute of Living Scale, which assesses IQ using sections focused on vocabulary and abstract reasoning skills (Zachary, 1994).
At each of 10 follow-up waves, separated by 24 months, psychosocial functioning and treatment utilization as well as axis I and II psychopathology were reassessed via interview methods similar to the baseline procedures by staff members blind to previously collected information. After informed consent was obtained, our diagnostic battery was readministered as well as the Revised Borderline Follow-up Interview—the follow-up analog to the Background Information Schedule administered at baseline (Zanarini et al., 1994). Good-excellent follow-up (within a generation of raters) and longitudinal (between generations of raters) inter-rater reliability was maintained throughout the course of the study for variables pertaining to psychosocial functioning and treatment use (Zanarini et al., 2004a; 2005). Good-excellent follow-up and longitudinal inter-rater reliability was also maintained for both axis I and II disorders (Zanarini et al., 2001; 2002).
2.1 Definition of Good Recovery from Borderline Personality Disorder or Another Axis II Disorder
As noted above, we selected a GAF score of 61 or higher as our measure of good recovery because it was used in the four follow-back studies conducted in the 1980s. We also selected it because it offers a reasonable description of a good overall outcome (i.e., “some mild symptoms or some difficulty in social, occupational, or school functioning, but generally functioning pretty well, has some meaningful interpersonal relationships”). We operationalized this score to enhance its reliability and meaning. More specifically, to be given this score or higher, a subject had to be in remission from his or her primary axis II diagnosis for a period of least two years, have at least one emotionally sustaining relationship with a close friend or life partner/spouse, and be able to work or go to school consistently, competently, and on a full-time basis (which included being a houseperson).
2.3 Definition of Excellent Recovery from Borderline Personality Disorder or Another Axis II Disorder
We selected a GAF score of 71 or higher as our measure of excellent recovery because it was used as the primary overall outcome in the Collaborative Longitudinal Personality Disorders Study. We also selected it because it offers a reasonable description of an excellent overall outcome (i.e., “If symptoms are present, they are transient and expectable reactions to psychosocial stressors; no more than slight impairment in social, occupational, or school functioning”). We operationalized this score to enhance its reliability and meaning. More specifically, to be given this score or higher, a subject had to meet the three concurrent criteria for a good recovery described above. In addition, absence of a co-occurring disorder that was serious enough that it was associated with a decrement social or vocational functioning was required.
2.4 Statistical Analyses
The Kaplan-Meier product-limit estimator (of the survival function) was used to assess time-to-good recovery and time-to-excellent recovery from borderline personality disorder (or another primary personality disorder for axis II comparison subjects). We defined time-to-attainment of these outcomes as the follow-up period at which these outcomes were first achieved. Thus, possible values for these outcomes were 2, 4, 6, 8, 10, 12, 14, 16, 18, and 20 years, with time=2 years for persons first achieving one of these types of recovery from borderline personality disorder (or another primary personality disorder for comparison subjects) during the first follow-up period, time=4 years for persons first achieving one of these types of recovery from borderline personality disorder (or another primary personality disorder for comparison subjects) during the second follow-up period, etc.
Cox proportional hazards survival analyses were also used to assess both bivariate and multivariate predictors of time-to-excellent recovery. All of the Cox regression analyses adjusted for the effects of overall baseline severity (as assessed by baseline GAF scores) and provided estimates of the hazard ratios (HR) and their 95% confidence intervals (95% CIs).
In carrying out the time-to-excellent recovery analyses summarized in this report, we first assessed the relationship between each baseline predictor variable and time-to-excellent recovery. These 27 variables are laid out in six groupings or “families” of predictors and these families are similar to those used in studies of the course of dysthymic disorder (Hayden & Klein, 2001) and bipolar I disorder (Nolen et al., 2004). These families of predictors are: demographic characteristics, pathological childhood experiences, protective childhood experiences, lifetime axis I disorders, aspects of temperament, and aspects of adult competence.
Because the choice of hypothesized predictors of time-to-excellent recovery was scientifically driven, we made adjustment for multiple testing of their bivariate relationships by controlling the false discovery rate (Benjamini & Hochberg, 1995; Glickman et al., 2014). That is, among the bivariate tests of association that are declared significant in our study, the false discovery rate is the expected proportion of those tests in which the null hypothesis is true; we specified the threshold at the conventional 0.05 level and present false discovery rate-adjusted p-values for the bivariate associations.
To select the most salient subset of factors that are predictive of time-to-excellent recovery, we entered all the significant (false discovery rate-adjusted p<0.05, 2-tailed) variables from the bivariate analyses simultaneously. We then followed a backward deletion procedure retaining the subset of predictors that were significant at the two-tailed 0.01 significance level.
3. Results
The sample and its diagnostic characteristics have been described before (Zanarini et al., 2003). Two hundred and ninety patients met both Revised Diagnostic Interview for Borderlines and DSM-III-R criteria for borderline personality disorder and 72 met DSM-III-R criteria for at least one nonborderline axis II disorder (and neither criteria set for borderline personality disorder). The following diagnoses were found for these comparison subjects (N=34): antisocial personality disorder (N=10, 13.9%), narcissistic personality disorder (N=3, 4.2%), paranoid personality disorder (N=3, 4.2%), avoidant personality disorder (N=8, 11.1%), dependent personality disorder (N=7, 9.7%), self-defeating personality disorder (N=2, 2.8%), and passive-aggressive personality disorder (N=1, 1.4%). Another 38 (52.8%) met criteria for personality disorder not otherwise specified (which was operationally defined in the Diagnostic Interview for DSM-III-R Personality Disorders as meeting all but one of the required number of criteria for at least two of the 13 axis II disorders described in DSM-III-R).
Baseline demographic data have also been reported before (Zanarini et al., 2003). Briefly, 279 (77%) of the participants were female and 315 (87%) were white. The average age of the participants was 27 years (SD=6.3), the mean socioeconomic status was 3.3 (SD=1.5) (where 1=highest and 5=lowest), and their mean GAF score was 39.8 (SD=7.8) (indicating major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood).
In terms of continuing participation, 220/259 (85%) of surviving patients with borderline personality disorder (13 died by suicide and 18 died of other causes) were reinterviewed at all ten follow-up waves. A similar rate of participation was found for axis II comparison participants, with 58/70 (83%) of surviving patients in this study group (one died by suicide and one died of other causes) being reassessed at all ten waves of follow-up.
Figure 1 details the rates of attaining a good recovery for borderline patients and personality-disordered comparison subjects by 20-year follow-up. As can be seen, 59% of borderline patients and 92% of axis II comparison subjects attained this outcome by 20-year follow-up. Borderline patients were significantly less likely to attain this outcome and to attain it at a significantly slower rate than personality-disordered comparison subjects (HR=0.30; 95%CI 0.21, 0.43; z=−6.52; p<0.001).
Figure 1.
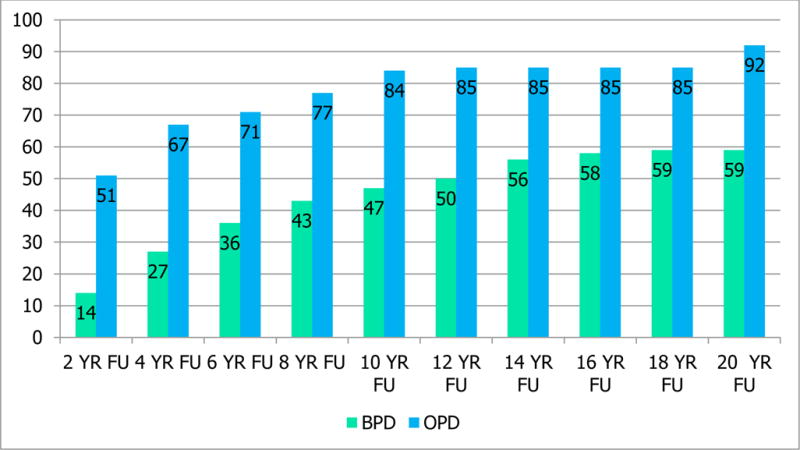
Cumulative Rates of Good Recovery over 20 Years
Figure 2 details the rates of attaining an excellent recovery for borderline patients and personality-disordered comparison subjects by 20-year follow-up. As can be seen, 39% of borderline patients and 73% of axis II comparison subjects attained this outcome by 20-year follow-up. As with good recovery, borderline patients were significantly less likely to attain this outcome and to attain it at a significantly slower rate than personality-disordered comparison subjects (HR=0.31; 95%CI 0.21, 0.46; z=−5.98; p<0.001).
Figure 2.
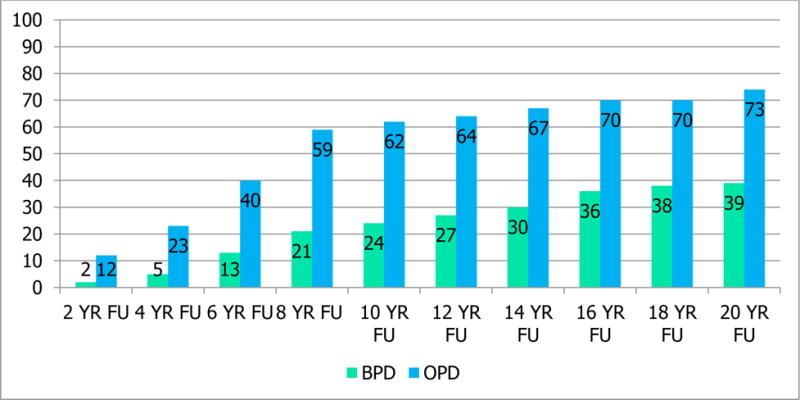
Cumulative Rates of Excellent Recovery over 20 Years
Table 1 details the bivariate predictors of time-to-excellent recovery for borderline patients followed prospectively for 20 years. As can be seen, 27 variables were studied and of these, 10 were statistically significant and 17 were non-significant. The significant variables were: younger age, severity of other forms of abuse, higher IQ, work competence under the age of 18, popularity in childhood, lower neuroticism, higher extraversion, higher agreeableness, good vocational record as an adult, and number of friends as an adult.
Table 1.
Baseline Predictors of Time-to-Excellent Recovery over 20 Years of Prospective Follow-up
| % (N) | Mean (SD) | Hazard Ratioa | Z | Pb | 95% CI | |
|---|---|---|---|---|---|---|
| Demographic Characteristics | ||||||
| 25 Years Old or Younger at Index Admission (median age=26) | 44.5 (N=129) |
2.19 | 3.53 | 0.003 | 1.42, 3.37 | |
| Female | 80.3 (N=233) |
1.03 | 0.11 | 0.912 | 0.58, 1.84 | |
| Non-white | 12.28 (N=37) |
0.55 | −2.12 | 0.076 | 0.31, 0.95 | |
| Pathological Childhood Experiences | ||||||
| Absence of Sexual Abuse | 37.6 (N=109) |
1.64 | 2.28 | 0.055 | 1.07, 2.51 | |
| Severity of Other Forms of Abuse | 7.3 (SD=5.3) |
0.95 | −2.40 | 0.044 | 0.91, 0.99 | |
| Severity of Neglect | 14.7 (SD=11) |
0.98 | −1.94 | 0.101 | 0.96, 1.00 | |
| Protective Childhood Experiences/Factors | ||||||
| Higher IQ | 104.2 (SD=12) |
1.06 | 5.05 | <0.001 | 1.04, 1.09 | |
| No Attention Deficit Hyperactivity Disorder | 72.4 (N=210) |
0.68 | −1.46 | 0.205 | 0.40, 1.14 | |
| Academic Competence | 58.6 (N=170) |
1.52 | 1.80 | 0.072 | 0.96. 2.40 | |
| Athletic Competence | 58.3 (N=169) |
1.08 | 0.71 | 0.561 | 0.87, 1.33 | |
| Leadership Competence | 36.9 (N=107) |
1.50 | 1.88 | 0.108 | 0.98, 2.30 | |
| Work Competence in Childhood | 73.1 (N=212) |
2.85 | 3.42 | 0.003 | 1.57, 5.19 | |
| Popularity in Childhood | 44.8 (N=130) |
1.68 | 2.42 | 0.044 | 1.10, 2.56 | |
| Lifetime Axis I Disorders | ||||||
| Absence of Mood Disorder | 3.1 (N=9) |
1.56 | 0.71 | 0.561 | 0.46, 5.27 | |
| Absence of Substance Use Disorder | 37.9 (N=110) |
0.97 | −0.16 | 0.907 | 0.63, 1.49 | |
| Absence of PTSD | 41.7 (N=121) |
1.45 | 1.70 | 0.134 | 0.95, 2.21 | |
| Absence of Another Anxiety Disorder | 19.7 (N=57) |
1.31 | 1.07 | 0.384 | 0.80, 2.16 | |
| Absence of Eating Disorder | 46.2 (N=134) |
1.18 | 0.77 | 0.561 | 0.78, 1.79 | |
| Aspects of Normal Temperament | ||||||
| Neuroticism | 35.1 (SD=7.0) |
0.94 | −4.38 | <0.001 | 0.92, 0.97 | |
| Extraversion | 22.6 (SD=7.0) |
1.06 | 3.48 | 0.003 | 1.02, 1.09 | |
| Openness | 29.8 (SD=6.6) |
1.03 | 2.01 | 0.092 | 1.00, 1.07 | |
| Agreeableness | 30.4 (SD=6.7) |
1.06 | 3.63 | 0.003 | 1.03, 1.10 | |
| Conscientiousness | 28.6 (SD=7.8) |
1.03 | 1.84 | 0.111 | 1.00, 1.05 | |
| Aspects of Adult Competence (in the two years prior to index admission) | ||||||
| Good Vocational Record (worked or went to school competently, consistently, and on a full-time basis) | 34.5 (N=100) |
2.09 | 3.23 | 0.005 | 1.34, 1.09 | |
| Emotionally Sustaining Relationship with Partner | 33.5 (N=97) |
1.56 | 0.66 | 0.573 | 0.75, 1.78 | |
| Emotionally Sustaining Relationship with Parent(s) | 42.4 (N=123) |
0.89 | −0.52 | 0.651 | 0.59, 1.36 | |
| Number of Friends | 3.9 (SD=3.5) |
1.07 | 2.89 | 0.013 | 1.02, 1.13 | |
Hazard ratio > 1.0 indicates greater likelihood of earlier recovery. All analyses control for GAF at baseline.
FDR-adjusted P-value: adjustment for multiple testing by controlling the false discovery rate (FDR).
Table 2 details the multivariate predictors of time-to- excellent recovery for borderline patients followed prospectively for 20 years. These significant predictors were: higher IQ, childhood work competence, good vocational functioning in adulthood, lower trait neuroticism, and higher trait agreeableness.
Table 2.
Multivariate Predictors of Time-to-Excellent Recovery
| Factor | Hazarda Ratio | SE | Z | P | 95% CI |
|---|---|---|---|---|---|
| Higher IQ | 1.06 | 0.014 | 4.52 | <0.001 | 1.03, 1.09 |
| Childhood Work Competence | 2.43 | 0.772 | 2.79 | 0.005 | 1.30, 4.53 |
| Good Vocational Record in Adulthood | 1.88 | 0.446 | 2.66 | 0.008 | 1.18, 2.99 |
| Lower Trait Neuroticism | 0.94 | 0.014 | −3.83 | <0.001 | 0.92, 0.97 |
| Higher Trait Agreeableness | 1.05 | 0.019 | 2.56 | 0.010 | 1.01, 1.08 |
Hazard ratio > 1.0 indicates greater likelihood of earlier recovery. All analyses control for GAF at baseline.
4. Discussion
Three main findings have emerged from this study. The first is that about 60% of borderline patients (and 92% of axis II comparison subjects) had achieved a good recovery over 20 years of prospective follow-up. This is the same percentage of borderline patients who achieved this outcome after 16 years of follow-up (Zanarini et al., 2012) and only 10% higher than had achieved it by 10-year follow-up (Zanarini et al., 2010). This result indicates that this outcome seems to be static as this study added four additional years of prospective follow-up. Our 22-year and 24-year waves of prospective assessment are ongoing and it may be that this outcome remains static over the next four years of prospective assessment as well, indicating a stable ceiling in terms of this overall outcome.
The second main finding is that only 39% of borderline patients (and 73% of axis II comparison subjects) achieved an excellent recovery—an outcome that we have never studied before. However, the Collaborative Longitudinal Personality Disorders study found that only 21% of its borderline patients achieved this outcome after 10 years of prospective follow-up (Gunderson et al., 2011). Our results are consistent with this finding. More specifically, 24% of our borderline patients achieved a GAF score of 71 or higher after 10 years of prospective follow-up.
Whether the percentage of borderline patients achieving an excellent recovery will increase with time is an open question. By 16-year follow-up, 36% of borderline patients had achieved this important outcome—a 3% difference with the 39% who achieved an excellent recovery by 20-year follow-up. This suggests, as with good recovery, that substantial growth in a clinically meaningful overall outcome seems possible but unlikely.
In some ways, the 20% difference for both study groups between good and excellent recovery is somewhat surprising as the narratives for these GAF bands are not dramatically different. “Mild symptoms” is only somewhat more serious than “If symptoms are present, they are transient and expectable reactions to psychosocial stressors.” In a similar manner, “Some difficulty in social, occupational, or school functioning, but generally functioning pretty well, has some meaningful interpersonal relationships” is not that different than “No more than slight impairment in social, occupational, or school functioning.” However, we believe that it is the fourth element of our operationalized definition of excellent recovery concerning co-occurring disorders that accounts for the 20% decline in those achieving excellent recovery vs. good recovery.
It is important to note that comparison subjects achieved higher rates of both good and excellent recovery than borderline patients. It is not clear what factor or factors account for this set of differences. However, these results are consistent with the view that BPD is a more severe disorder symptomatically and psychosocially than the heterogeneous personality disorder diagnoses that comprise our comparison group.
Which type of recovery is the best for clinicians to encourage and even expect their borderline patients to attain? A good recovery seems to be a “good enough” outcome. However, an excellent recovery seems to be describing a uniformly high functioning person. Is a good recovery asking too little of a borderline patient or is an excellent recovery expecting too much, particularly from someone who was initially hospitalized in a tertiary care facility and typically had multiple comorbidities on axis I and II (Zanarini et al., 2004b; 2004c)?
In addition, is recovery even a relevant outcome? It certainly seems to be in psychiatry and mental health care defined more broadly. Following Links (1993), we ourselves have called for a rehabilitation model for those borderline patients who have achieved a two-year remission (99%) but have not achieved a good recovery (40%) by the time of the 16-year follow-up (Zanarini et al., 2012). By contrast, in most other medical specialties remission or symptom relief is the desired outcome, and social and vocational functioning are only relevant if they interfere with or support treatment compliance.
The third main finding of this study is that competence in both childhood and adulthood seems the best predictor of attaining an excellent recovery. Predictors related to competence were: higher IQ, good childhood work history, and good adult vocational history (in two years prior to index admission). Other predictors were temperamental in nature and inverse to the typical temperamental view of borderline patients (Distel et al., 2009): higher neuroticism and lower agreeableness. This inverse pattern of lower neuroticism and higher agreeableness could be seen as temperamental competence or a personality that would increase one’s chances of being successful as a child and as an adult. This is so because the subject would not be unduly burdened by negative emotions and would have some capacity to “mentalize” the thoughts and feelings of others as well as his or her own.
Looking at these results in another way, achieving an excellent recovery is more about who you are and not what other people have done to you or failed to do for you. It also suggests clearly that the trajectory of borderline patients is not guided solely or mainly by psychopathology or childhood adversity but that being capable or competent both as a child and as an adult is critically important. However, results might have differed if time-varying predictors assessing comorbidity and adversity (adult) had been studied rather than baseline predictors.
Previously, we have suggested that treatment modules aimed at the vocational functioning (Zanarini et al., 2014) and temperamental symptoms (Zanarini et al., 2007) of borderline patients be developed. These predictive results suggest that training in improving resilience might be extremely important. This is so because resilience or grit (Duckworth et al., 2007) is fundamental to both vocational competence and dealing with less than optimal aspects of temperament. Improving the levels of determination and persistence of lower functioning borderline patients might well allow them to use more of their competence and overcome some of their temperamental difficulties, such as becoming easily overwhelmed or overly discouraged. It might also alleviate some of the shame and suffering of these particularly challenging patients.
This study has two main limitations. One limitation of this study is that all of the patients were seriously ill inpatients at the start of the study. Another limitation is that about 90% of those in both patient groups were in individual therapy and taking psychotropic medications at baseline and about 70% were participating in each of these outpatient modalities during each follow-up period (Zanarini et al., 2015). Thus, it is difficult to know if these results would generalize to a less disturbed group of patients. It is also difficult to know if these results would generalize to people meeting criteria for borderline personality disorder who were not in treatment, which in the current study was typically non-intensive outpatient treatment as usual in the community.
Taken together, the results of this study suggest that a complete recovery is difficult for borderline patients to achieve even over long periods of time. They also suggest that competence displayed in both childhood and adulthood is the best predictor of this important outcome.
Highlights.
After 20 years of prospective follow-up, borderline patients had a significantly lower rate of good recovery than axis II comparison subjects
This rate was the same as the rate achieved by borderline patients at 16-year follow-up
Borderline patients also had a significantly lower rate of excellent recovery than comparison subjects
The best multivariate predictors of excellent recovery among borderline patients were—higher IQ, good childhood work history, good adult vocational record, lower trait neuroticism, and higher trait agreeableness.
Acknowledgments
This study was supported by NIMH grants MH47588 and MH62169.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57:289–300. [Google Scholar]
- Costa PT, McCrae RR. Revised NEO Personality Inventory and NEO Five-Factor Inventory Professional Manual. Psychological Assessment Resources; Odessa, Florida: 1992. [Google Scholar]
- Distel MA, Trull TJ, Willemsen G, Vink JM, Derom CA, Lynskey M, Martin NG, Boomsma DI. The five-factor model of personality and borderline personality disorder: a genetic analysis of comorbidity. Biol Psychiatry. 2009;66:1131–1138. doi: 10.1016/j.biopsych.2009.07.017. [DOI] [PubMed] [Google Scholar]
- Duckworth AL, Peterson C, Matthews MD, Kelly DR. Grit: perseverance and passion for long-term goals. J Pers Soc Psychol. 2007;92:1087–1101. doi: 10.1037/0022-3514.92.6.1087. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: a procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol. 2014;67:850–857. doi: 10.1016/j.jclinepi.2014.03.012. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, Zanarini MC, Yen S, Markowitz JC, Sanislow C, Ansell E, Pinto A, Skodol AE. Ten-year course of borderline personality disorder: Psychopathology and function from the collaborative longitudinal personality disorder study. Arch Gen Psychiatry. 2001;68:827–837. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden EP, Klein DN. Outcome of dysthymic disorder at 5-year follow-up: the effect of familial psychopathology, early adversity, personality, comorbidity, and chronic stress. Am J Psychiatry. 2001;158:1864–1870. doi: 10.1176/appi.ajp.158.11.1864. [DOI] [PubMed] [Google Scholar]
- Links PS. Psychiatric rehabilitation model for borderline personality disorder. Can J Psychiatry. 1993;38(Suppl 1):S35–3830. [PubMed] [Google Scholar]
- Luborsky L. Clinician’s judgements of mental health: a proposed scale. Arch Gen Psychiatry. 1962;7:407–417. doi: 10.1001/archpsyc.1962.01720060019002. [DOI] [PubMed] [Google Scholar]
- McGlashan TH. The prediction of outcome in borderline personality disorder: art V of the Chestnut Lodge follow-up study. In: McGlashan TH, editor. The Borderline: Current Empirical Research. American Psychiatric Press; Washington, DC: 1985. pp. 61–98. [Google Scholar]
- McGlashan TH. The Chestnut Lodge follow-up study. III Long-term outcome of borderline personalities. Arch Gen Psychiatry. 1986;43:20–30. doi: 10.1001/archpsyc.1986.01800010022003. [DOI] [PubMed] [Google Scholar]
- Nolen WA, Luckenbaugh DA, Altshuler LL, Suppes T, McElroy SL, Frye MA, Kupka RW, Keck PE, Leverich GS, Post RM. Correlates of 1-year prospective outcome in bipolar disorder: results from the Stanley Foundation Bipolar Network. Am J Psychiatry. 2004;161:1447–1454. doi: 10.1176/appi.ajp.161.8.1447. [DOI] [PubMed] [Google Scholar]
- Paris J, Brown R, Nowlis D. Long-term follow-up of borderline patients in a general hospital. Compr Psychiatry. 1987;28:530–536. doi: 10.1016/0010-440x(87)90019-8. [DOI] [PubMed] [Google Scholar]
- Paris J, Nowlis D, Brown R. Developmental factors in the outcome of borderline personality disorder. Compr Psychiatry. 1988;29:147–150. doi: 10.1016/0010-440x(88)90007-7. [DOI] [PubMed] [Google Scholar]
- Plakun EM. Prediction of outcome in borderline personality disorder. J Personal Disord. 1991;5:93–101. [Google Scholar]
- Plakun EM, Burkhardt PE, Muller JP. 14-year follow-up of borderline and schizotypal personality disorders. Compr Psychiatry. 1985;26:448–455. doi: 10.1016/0010-440x(85)90081-1. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R (SCID). I: history, rational, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Stone MH. The Fate of Borderline Patients. Guilford Press; New York: 1990. [Google Scholar]
- Zachary RA. Shipley Institute of Living Scale: Revised Manual. Psychological Services; Los Angeles, CA: 1994. [Google Scholar]
- Zanarini MC. Background Information Schedule. McLean Hospital; Belmont, MA: 1992. [Google Scholar]
- Zanarini MC, Frankenburg FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Compr Psychiatry. 2001;42:369–374. doi: 10.1053/comp.2001.24556. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG. The Diagnostic Interview for Personality Disorders: inter-rater and test-retest reliability. Compr Psychiatry. 1987;28:467–480. doi: 10.1016/0010-440x(87)90012-5. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry. 2004b;161:2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Silk KR. Mental health service utilization by borderline personality disorder patients and axis II comparison subjects followed prospectively for 6 years. J Clin Psychiatry. 2004a;65:28–36. doi: 10.4088/jcp.v65n0105. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Psychosocial functioning of borderline patients and axis II comparison subjects followed prospectively for six years. J Pers Disord. 2005;19:19–29. doi: 10.1521/pedi.19.1.19.62178. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: a 10-year follow-up study. Am J Psychiatry. 2007;164:929–935. doi: 10.1176/ajp.2007.164.6.929. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice GM. Time to attainment of recovery from borderline personality disorder and stability of recovery: A 10-year prospective follow-up study. Am J Psychiatry. 2010;167:663–667. doi: 10.1176/appi.ajp.2009.09081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice GM. Attainment and stability of sustained symptomatic remission and recovery among patients with borderline personality disorder and axis II comparison subjects: a 16-year prospective follow-up study. Am J Psychiatry. 2012;169:476–483. doi: 10.1176/appi.ajp.2011.11101550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Wedig MM, Conkey LC, Fitzmaurice GM. Prediction of time-to-attainment of recovery for borderline patients followed prospectively for 16 years. Acta Psychiatr Scand. 2014;130:205–213. doi: 10.1111/acps.12255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Conkey LC, Fitzmaurice GM. Treatment rates for patients with borderline personality disorder and other personality disorders: a 16-year study. Psychiatr Serv. 2015;66:15–20. doi: 10.1176/appi.ps.201400055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Vujanovic AA. The inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines (DIB-R) J Pers Disord. 2002;16:270–276. doi: 10.1521/pedi.16.3.270.22538. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Vujanovic AA, Hennen J, Reich DB, Silk KR. Axis II comorbidity of borderline personality disorder: Description of 6-year course and prediction of time-to-remission. Acta Psychiatr Scand. 2004;110:416–420. doi: 10.1111/j.1600-0447.2004.00362.x. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The Revised Diagnostic Interview for Borderlines: discriminating BPD from other Axis II disorders. J Pers Disord. 1989a;3:10–18. [Google Scholar]
- Zanarini MC, Gunderson JG, Marino MF, Schwartz EO, Frankenburg FR. Childhood experiences of borderline patients. Compr Psychiatry. 1989b;30:18–25. doi: 10.1016/0010-440x(89)90114-4. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Sickel AE, Yong L, Glazer LJ. Revised Borderline Follow-up Interview. McLean Hospital; Belmont, MA: 1994. [Google Scholar]


