Abstract
Purpose
After a radical gastrectomy, patients may experience severe pain. Some studies have reported that the use of propofol significantly reduced postoperative pain, while others have argued that this effect was not significant. Thus, we aimed to assess whether anesthesia with propofol could help to reduce pain after an open radical gastrectomy procedure.
Patients and methods
Sixty patients who were scheduled to undergo a laparotomy for radical gastrectomy were randomly assigned to either the propofol or sevoflurane group (n=30 each). A target-controlled infusion of propofol or inhalation of sevoflurane, titrated to bispectral index of 40–60, was maintained. All patients were administered a standardized multimodal analgesic plan, including intraoperative dexmedetomidine, dexamethasone, and postoperative flurbiprofen axetil, as well as patient-controlled fentanyl. Hemodynamics, pain scores, fentanyl consumption, adverse events, and the incidence of chronic pain 1 month and 3 months following hospital discharge were recorded.
Results
The intensity of postoperative pain was relatively low to moderate in all the patients. The propofol group showed lower pain scores, at rest and while coughing, up to 48 h postoperatively compared to the sevoflurane group (P<0.05). Cumulative fentanyl consumption 0–24 h after surgery was lower for the propofol group (364.4 ± 139.1 vs. 529.3 ± 237.9 µg; P=0.002). However, for fentanyl consumption 0–48 h, the difference between the two groups was not significant (710.9 ± 312.8 vs. 850.9 ± 292.0 µg; P=0.078). There were no differences in the incidences of adverse events or chronic pain between the groups.
Conclusions
Overall, the multimodal analgesic approach reduced postoperative pain after an open radical gastrectomy procedure in all patients anesthetized with either propofol or sevoflurane. Furthermore, our results indicated better analgesic outcome for the propofol group, especially in the early postoperative period.
Keywords: anesthesia, propofol, sevoflurane, postoperative pain, gastrectomy, intravenous anesthesia, inhalational anesthesia
Introduction
Despite recent advances, the management of postoperative pain remains a major challenge.1,2 Furthermore, acute postoperative pain has a strong correlation with the severity and increased risk of chronic pain.3 After a radical gastrectomy procedure, patients often experience acute pain due to the upper abdominal incision and extensive surgical manipulations. In our previous study, patients have reported moderate to severe pain and need for high fentanyl consumption.4
The use of intraoperative general anesthetics, either injectable (propofol) or volatile (sevoflurane), could influence peripheral nociception, thereby controlling postoperative pain. There are contrasting reports regarding the benefits of propofol: while some studies noted a significant reduction in postoperative pain,5–8 others suggest that this effect was not significant.9–11 In a recent meta-analysis, no significant differences between propofol and inhalational anesthesia (isoflurane, sevoflurane, and desflurane) were identified in postoperative pain control, possibly due to substantial heterogeneity among the studies included.12
Therefore, the present study aimed to compare the benefits of propofol and sevoflurane in postoperative pain control and analgesic consumption in patients after a radical gastrectomy. In addition, the study also reports the incidence of chronic pain during a follow-up of 1 and 3 months after discharge from hospital.
Patients and methods
Patients
The study has been registered at www.chictr.org.cn (ChiCTR-IOR-15006472), and approval from the institutional review board of the First Affiliated Hospital of Soochow University (Approval No. 2015-225) was obtained. The adherence to the updated guidelines for reporting parallel group randomized trials according to CONSORT 2010 is ensured.
The study included patients (aged 18–65 years) with American Society of Anesthesiologists (ASA) physical status I–II, who were scheduled to undergo an open radical gastrectomy procedure, after obtaining written informed consent. The exclusion criteria included uncontrolled hypertension, ASA≥III, body mass index (BMI)>35 kg/m2, cardiopulmonary disease, renal or liver disease, pregnancy, chronic pain, current use of opioids, allergies to medications discussed in this study, or need for reoperation. All patients received instructions a priori regarding the use of patient-controlled analgesia (PCA) and the verbal analog scale (VAS) for pain assessment (0=no pain, 10=extreme pain).
Using a computer-generated random table, patients were assigned to either of the two study groups (propofol or sevoflurane). All the procedures were performed by the same surgical and anesthesia teams. Due to the crucial differences between the anesthetic techniques, the attending anesthesiologist was aware of the patient grouping. However, postoperative observers and researchers responsible for data extraction and analyses were blinded to patient grouping.
Protocol
Patients were prohibited from use of any medication prior to the procedure. At the operating room, blood pressure, pulse oximetry, electrocardiogram, and bispectral index (BIS) were monitored for all patients. For arterial blood pressure monitoring, an arterial line was introduced into the radial artery, and for central venous pressure monitoring, a catheter was introduced via the right subclavian vein.
To induce general anesthesia, propofol 2 mg/kg (Diprivan, AstraZeneca, Italy) and fentanyl 3 µg/kg (RenFu Medicine, China) were used. Cisatracurium 0.2 mg/kg (HengRui Medicine) was administered for tracheal intubation and an additional bolus of 0.1 mg/kg was used for intraoperative muscle relaxation. Following intubation, the lungs were mechanically ventilated with 80% oxygen in air to maintain the end-tidal CO2 at 30–40 mmHg. Patients in the propofol group received a target-controlled infusion of propofol (2–4 µg/mL), and those in the sevoflurane group (HengRui Medicine) received sevoflurane inhalation (1–3%). Anesthesia depth was titrated to BIS 40–60. After anesthetic induction, dexmedetomidine (1 µg/kg; HengRui Medicine) was administered slowly for 30 min.
Heart rate (HR) and mean arterial pressure (MAP) were maintained within 20% of baseline values. If clinical signs of inadequate analgesia were present, such as movement, hypertension, or tachycardia, an additional dose of fentanyl 1 µg/kg was administered. If hypotension (systolic arterial pressure [SAP]<90 mmHg or MAP<65 mmHg) or bradycardia (HR<40 bpm) occurred, ephedrine 5 mg or atropine 0.5 mg was given.
All patients received dexamethasone 10 mg and ondansetron 8 mg at the end of surgery for prophylaxis of postoperative nausea and vomiting (PONV). At skin closure, a PCA containing fentanyl (20 µg/kg) in 100 mL saline was started, with a background infusion of 1 mL/h and a bolus dose of 2 mL for a lockout time of 10 min. Following extubation, patients were transferred to a post-anesthesia care unit (PACU) and monitored for 90 min. All patients received flurbiprofen axetil 50 mg intraoperatively and every 12 h for the next two days in the ward. All patients were encouraged to self-administer fentanyl through the PCA device for pain relief. An additional bolus of fentanyl 1 µg/kg was given for rescue analgesia. No use of other opioids was permitted throughout the study. Dosages of analgesics were standardized for all the participants.
HR and MAP were recorded at seven time points: baseline, skin closure, after extubation, PACU discharge, as well as at 2, 4, and 12 h postoperatively. Fentanyl use was recorded at three time points: 4, 24, and 48 h postoperatively. VAS scores at rest and while coughing were recorded at six time points: extubation, PACU discharge, and at 4, 12, 24, and 48 h postoperatively.
Patient demographics, duration of surgery, time to extubation, length of PACU stay, length of hospital stay, intraoperative fentanyl administration, fluids infused, blood loss, urine output, and ephedrine or atropine use were recorded. Postoperative adverse events, including PONV, abdominal hemorrhage, reoperation, and incision infection, were also recorded. Patients were followed telephonically to enquire about the incidence of chronic pain 1 and 3 months after discharge from hospital.
The primary outcome of interest for this study was postoperative fentanyl use. The secondary outcomes were scoring based on VAS, incidences of adverse events, and patients’ perception of chronic pain postoperatively.
Statistics
Sample size was calculated using PASS software (version 11.0.7; NCSS, Kaysville, UT, USA). Based on the sample size arrived at for our previous study in which fentanyl 498 µg (SD 176 µg) was administered for the first 24 h after an open radical gastrectomy procedure under sevoflurane anesthesia,4 it was estimated that it was necessary to enroll 26 patients for the present study under each group to demonstrate a 25% reduction in fentanyl consumption with an α value of 0.05 and 80% power. However, we enrolled 38 patients under each group to account for the possibility of a 30% dropout.
Statistical analyses were performed using SPSS software (version 19.0; IBM, Armonk, NY, USA). The Kolmogorov–Smirnov test was used to evaluate the normal distribution of continuous data. Normally distributed variables such as age, BMI, duration of surgery, time to extubation, PACU stay, intra-operative fentanyl use, fluids infused, blood loss, urine output, MAP, HR, and cumulative fentanyl consumption were presented as mean (SD) and compared using an independent samples t-test. Non-normally distributed variables such as VAS scores, ephedrine or atropine use, and need for rescue analgesics were presented as median (interquartile range [IQR]) and compared using a Mann–Whitney U-test or Friedman’s test. Gender, ASA class, comorbidities, chronic pain, and adverse events were compared using Pearson’s chi-squared test or Fisher’s exact test. P-values <0.05 were considered statistically significant.
Results
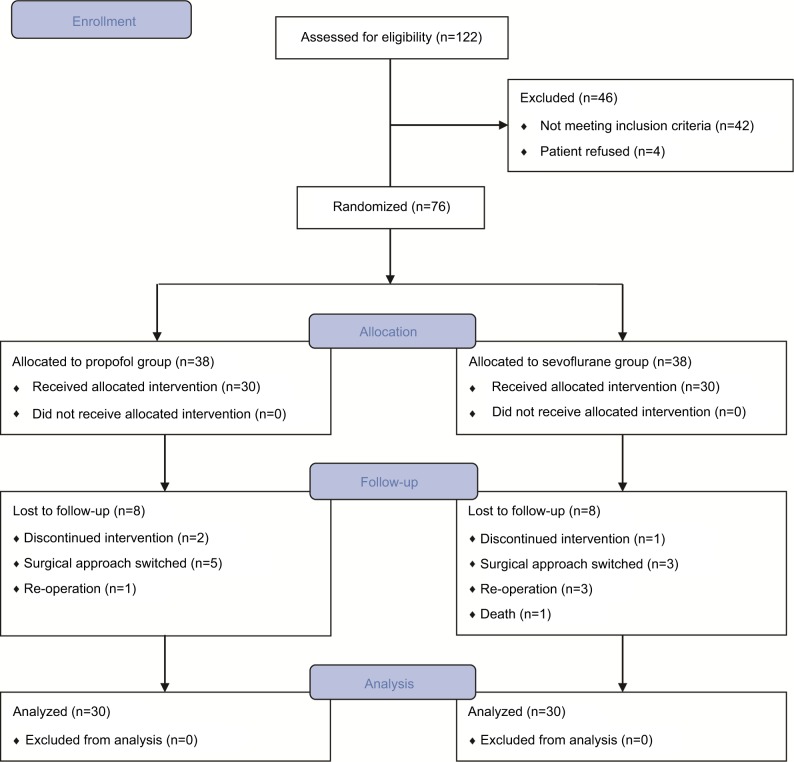
Of 122 patients evaluated, 76 were identified to be eligible and randomly assigned to two groups. Of those excluded from the study, 42 failed to meet the inclusion criteria (34 due to ASA≥III, SAP>180 mmHg, BMI>35 kg/m2, cardiopulmonary disease, or chronic renal disease; 2 due to current use of opioids; and 6 due to change in surgical approach or cancellation of procedure) and 4 refused to enroll. After excluding 16 patients for various reasons, 60 patients remained till the study end. In those who left the study prematurely, PCA was terminated early in 3 patients, surgical procedures were switched intraoperatively in 8 patients, 4 patients underwent reoperation, and 1 patient died of postoperative hemorrhage on the first postoperative day. Thirty patients in each group remained in the final analyses (Figure 1).
Figure 1.
CONSORT flow diagram.
Patient demographics and surgical characteristics are shown in Table 1. The propofol group had lower HRs compared to the sevoflurane group after extubation (76.9 ± 11.0 vs. 84.2 ± 16.0 beats/min, P=0.043; Figure 2). There were no significant differences in HR or MAP between the groups at any other time point.
Table 1.
Demographics and surgical characteristics
| Parameters | Propofol (n=30) | Sevoflurane (n=30) | P-values |
|---|---|---|---|
| Gender (male/female) | 7/23 | 10/20 | 0.390 |
| Age (years) | 54.3 ± 9.4 | 53.0 ± 9.3 | 0.593 |
| BMI (kg/m2) | 22.6 ± 3.3 | 22.6 ± 3.4 | 0.963 |
| ASA (I/II) | 13/17 | 15/15 | 0.605 |
|
| |||
| Comorbidity (n, %) | |||
| Hypertension | 12 (40%) | 6 (20%) | 0.091 |
| Diabetes mellitus | 3 (10%) | 5 (16.7%) | 0.706 |
| COPD | 0 (0%) | 1 (3.3%) | 1.000 |
|
| |||
| Duration of surgery (min) | 162.5 ± 35.5 | 155.7 ± 30.3 | 0.430 |
| Time to extubation (min) | 42.3 ± 14.6 | 38.0 ± 15.7 | 0.279 |
| PACU stay (min) | 57.4 ± 20.9 | 54.4 ± 21.3 | 0.580 |
| Intraoperative fentanyl (µg) | 613.3 ± 62.9 | 588.3 ± 92.6 | 0.226 |
| Intraoperative cisatracurium (mg) | 29.8 ± 6.2 | 27.5 ± 5.8 | 0.143 |
| Fluid infused (mL) | 1,030.0 ± 186.0 | 1,088.3 ± 225.8 | 0.279 |
| Blood loss (mL) | 211.0 ± 144.4 | 188.3 ± 73.9 | 0.447 |
| Urine output (mL) | 388.3 ± 202.9 | 381.7 ± 186.8 | 0.895 |
| Ephedrine use (n) | 0 (0–1) | 1 (0–1) | 0.232 |
| Atropine use (n) | 0 (0–0) | 0 (0–0) | 0.981 |
Note: Data are presented as total number (%), mean ± standard deviation, or median (interquartile range).
Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; PACU, post-anesthesia care unit.
Figure 2.
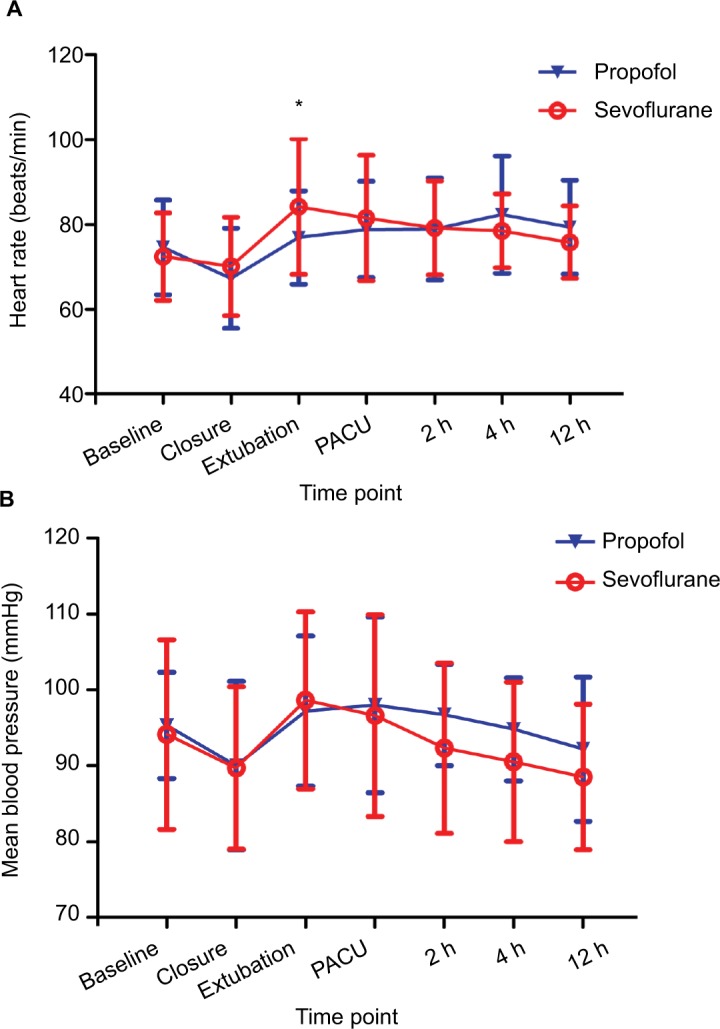
(A) Heart rate and (B) mean arterial pressure.
Notes: Data are presented as mean ± SD. *P<0.05 between groups.
Abbreviation: PACU, post-anesthesia care unit.
For the propofol group, VAS scores at rest and while coughing were significantly lower at all time points compared to the sevoflurane group (P<0.05; Table 2, Figure 3). The cumulative fentanyl consumption 0–24 h after surgery was also lower for the propofol group compared to the sevoflurane group (364.4 ± 139.1 vs. 529.3 ± 237.9 µg; P=0.002; Table 3). However, for fentanyl consumption 0–48 h, the difference between groups was not significant (710.9 ± 312.8 vs. 850.9 ± 292.0 µg; P=0.078).
Table 2.
VAS pain scores
| Propofol (n=30) | Sevoflurane (n=30) | P-values | |||
|---|---|---|---|---|---|
| After extubation | At rest | 1 (0–1) | 1.5 (1–4) | 0.001* | |
| With coughing | 2 (1–2.25) | 2.5 (2–5.25) | 0.002* | ||
|
| |||||
| PACU discharge | At rest | 1 (0–1) | 3 (1–4) | 0.001* | |
| With coughing | 2 (1–3) | 4 (2–6) | 0.001* | ||
|
| |||||
| 4 h after surgery | At rest | 0 (0–1) | 1 (1–3) | 0.001* | |
| With coughing | 1 (1–2) | 3 (2–4) | 0.001* | ||
|
| |||||
| 12 h after surgery | At rest | 0.5 (0–1.25) | 1 (1–3) | 0.005* | |
| With coughing | 2 (1–2.25) | 3 (2–4) | 0.001* | ||
|
| |||||
| 24 h after surgery | At rest | 0 (0–1) | 1 (0–2) | 0.010* | |
| With coughing | 2 (1–2.25) | 2 (2–3) | 0.028* | ||
|
| |||||
| 48 h after surgery | At rest | 0 (0–0) | 0 (0–1) | 0.010* | |
| With coughing | 1 (0.75–2) | 2 (1–3) | 0.018* | ||
Notes: Data are presented as median (interquartile range).
P<0.05 indicates significant differences.
Abbreviations: PACU, post-anesthesia care unit; VAS, verbal analog scale.
Figure 3.
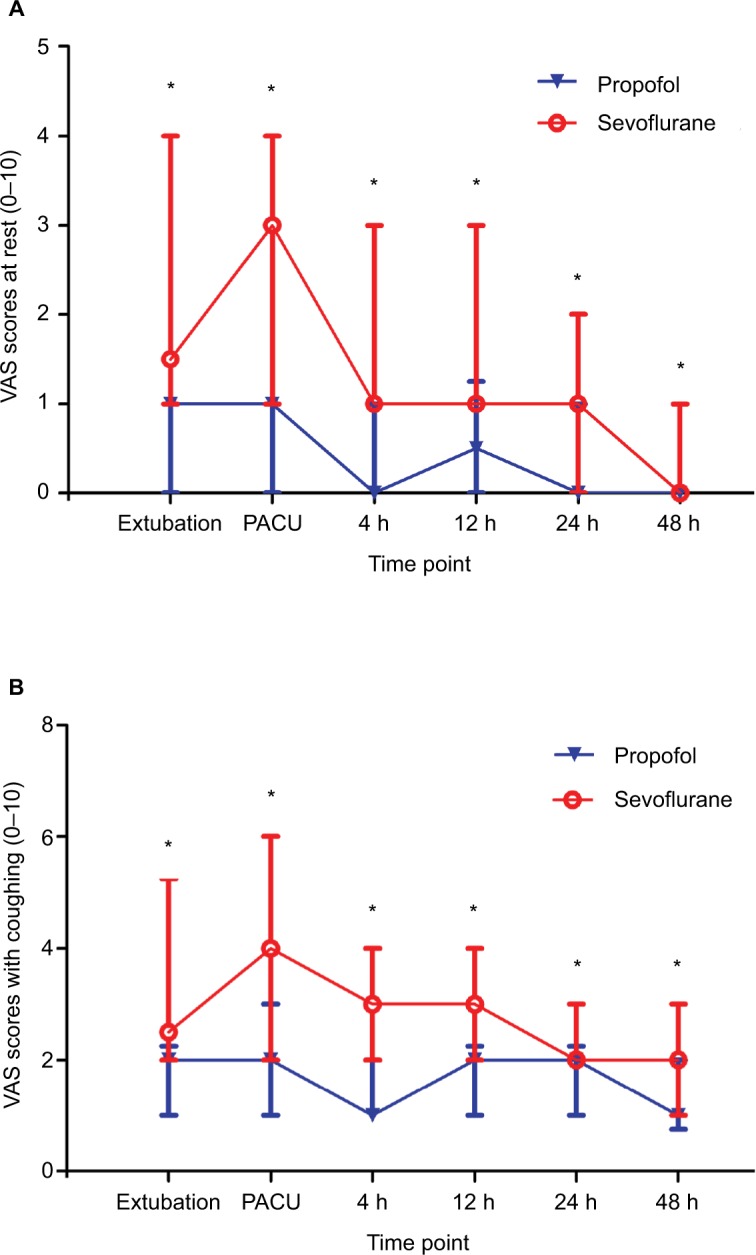
VAS scores for pain (A) at rest and (B) with coughing.
Notes: Data are presented as median (interquartile range). *P<0.05 between groups.
Abbreviations: PACU, post-anesthesia care unit; VAS, verbal analog scale.
Table 3.
Postoperative fentanyl consumption and other variables
| Propofol (n=30) | Sevoflurane (n=30) | P-values | |
|---|---|---|---|
| Cumulative fentanyl consumption (µg) | |||
| 0–24 h after surgery | 364.4 ± 139.1 | 529.3 ± 237.9 | 0.002* |
| 0–48 h after surgery | 710.9 ± 312.8 | 850.9 ± 292.0 | 0.078 |
|
| |||
| Need for rescue analgesics (n) | 1 (1–2) | 2 (1–3) | 0.061 |
| Hospital stay (days) | 8.8 ± 2.7 | 9.5 ± 2.7 | 0.301 |
|
| |||
| Adverse events (n, %) | |||
| PONV | 2 (6.7%) | 4 (13.3%) | 0.671 |
| Abdominal hemorrhage | 1 (3.3%) | 1 (3.3%) | 1.000 |
| Incision infection | 1 (3.3%) | 0 (0%) | 1.000 |
| Reoperation | 1 (3.3%) | 3 (10%) | 0.612 |
| Mortality | 0 (0%) | 1 (3.3%) | 1.000 |
|
| |||
| Chronic pain (n, %) | |||
| 1 month after discharge | 3 (10%) | 2 (6.7%) | 1.000 |
| 3 months after discharge | 1 (3.3%) | 1 (3.3%) | 1.000 |
Notes: Data are presented as total number (%), mean ± standard deviation, or median (interquartile range).
P<0.05 indicates significant differences.
Abbreviation: PONV, post-operative nausea and vomiting.
There were no differences in the use of rescue analgesia, length of hospital stays, adverse events, or chronic pain between the propofol and sevoflurane groups (Table 3).
Discussion
Using a multimodal analgesic approach, this study reports that pain was greatly reduced in all patients anesthetized with either propofol or sevoflurane in a radical gastrectomy procedure. Our results showed that propofol was able to better reduce pain intensity and fentanyl usage in comparison to sevoflurane, especially in the early postoperative period. However, the incidence of chronic pain 1 month and 3 months after discharge did not differ between the groups. To the best of our knowledge, this present study was the first to report on the analgesic effects of propofol on this patient population.
Whether propofol is superior over inhalation anesthetics has remained a matter of much clinical debate. However, only two systematic reviews, including one by our own group, have been published to date.12,13 The first meta-analysis by Qiu et al13 involving 14 trials suggested that a statistically significant but marginal reduction in postoperative pain scores at 24 h (mean difference of −0.134) was reported after propofol use. In our meta-analysis, patients anesthetized with propofol reported lower pain scores (from 0.48 at 30 min to 0.08 at 24 h postoperatively) and reduced opioid consumption in the first 24 h (2.68 mg of morphine-equivalent) as compared to those anesthetized with inhalational anesthetics. However, our results were affected by substantial heterogeneity, suggesting that further adequately sized, randomized, and controlled studies are needed to establish clinical relevance.
Propofol is a short-acting anesthetic agent used intravenously for sedation.14,15 For improved PONV prophylaxis, propofol is preferred over inhalation anesthetics.16–19 In addition to its anesthetic and anti-emetic effects, anti-nociceptive effects of propofol are well known.20–25 In a group of healthy volunteers for whom acute pain was induced by intracutaneous electrical stimulation, the use of propofol lowered pain scores by 38% and reduced areas of hyperalgesia and allodynia.20 However, there was an abrupt loss in analgesic effects after infusion was stopped. Propofol reduced pain and dorsal horn responses to noxious stimulation in rats and goats in a dose-dependent manner.21,22 A systemic delivery of propofol would cause anti-nociceptive effects due to the activation of gamma-aminobutyric acid type A receptors, and its anti-oxidant and anti-inflammatory effects.23–25 Adverse interactions between propofol and other drugs, including opioid analgesics, have also been reported.26,27
Sevoflurane has comparable analgesic properties as well. At an optimal concentration of 0.8%, it has been recommended for sedation during labor pain.28 However, inhalation anesthetics have been reported to have hyperalgesic effects at a minimum alveolar concentration of 0.1, which may account for increased pain perception.29 The effects of volatile anesthetics may be moderated by the modulation of serotonin (5-HT3) receptor-mediated currents and by central adrenergic and cholinergic transmission.30–32
Our multimodal analgesic approach involving a combination of fentanyl, dexmedetomidine, dexamethasone, and non-steroidal anti-inflammatory drugs is thus proved to be effective in controlling pain in patients after a radical gastrectomy. We used intraoperative dexmedetomidine based on our previous finding that it could reduce pain and analgesic requirements after various surgical procedures.33–35 In the present study, lower pain scores were reported after radical gastrectomy in patients anesthetized with either propofol or sevoflurane.
Limitations
This study has several limitations. First, a multimodal analgesic approach was used, and hence complex drug interactions among analgesics could have resulted in improved results than each of the anesthetics might have demonstrated individually. Second, the study considered only those patients who underwent radical gastrectomy, and so the findings cannot be generalized to other types of surgeries. Third, an optimal dose of propofol either alone or as a multimodal analgesic was not reported by this study. Fourth, due to its relatively small sample size, the study may have had potential bias. The study did not have significant power to detect differences between the groups over a long term postoperatively, including chronic pain. Lastly, although a reduction in postoperative pain and fentanyl consumption was noted for the propofol group as compared to the sevoflurane group, we caution that clinical differences may not be as much as statistical differences.
Conclusion
In this single-center study, pain after an open radical gastrectomy procedure was significantly reduced in all patients anesthetized with either propofol or sevoflurane. Furthermore, our results indicated better analgesic outcome for the propofol group especially in the early postoperative period. However, due to the limitation in the enrollment of participants to this study, more evidence is required to further establish power for our results.
Acknowledgments
This work was supported, in part, by grants from the National Natural Science Foundation of China (81601659 to KP, 81471835 and 81671880 to FHJ, and 81601666 to JZ) and the Jiangsu Provincial Medical Youth Talents Program (QNRC2016741 to KP).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Argoff CE. Recent management advances in acute postoperative pain. Pain Pract. 2014;14(5):477–487. doi: 10.1111/papr.12108. [DOI] [PubMed] [Google Scholar]
- 2.Wu CL, Raja SN. Treatment of acute postoperative pain. Lancet. 2011;377(9784):2215–2225. doi: 10.1016/S0140-6736(11)60245-6. [DOI] [PubMed] [Google Scholar]
- 3.Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618–1625. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Xu X, Liu H, Ji F. Effects of dexmedetomidine on patients undergoing radical gastrectomy. J Surg Res. 2015;194(1):147–153. doi: 10.1016/j.jss.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Chan AC, Qiu Q, Choi SW, et al. Effects of intra-operative total intravenous anaesthesia with propofol versus inhalational anaesthesia with sevoflurane on post-operative pain in liver surgery: a retrospective case-control study. PLoS One. 2016;11(2):e0149753. doi: 10.1371/journal.pone.0149753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li M, Mei W, Wang P, et al. Propofol reduces early post-operative pain after gynecological laparoscopy. Acta Anaesthesiol Scand. 2012;56(3):368–375. doi: 10.1111/j.1399-6576.2011.02603.x. [DOI] [PubMed] [Google Scholar]
- 7.Tan T, Bhinder R, Carey M, Briggs L. Day-surgery patients anesthetized with propofol have less postoperative pain than those anesthetized with sevoflurane. Anesth Analg. 2010;111(1):83–85. doi: 10.1213/ANE.0b013e3181c0ee9e. [DOI] [PubMed] [Google Scholar]
- 8.Cheng SS, Yeh J, Flood P. Anesthesia matters: patients anesthetized with propofol have less postoperative pain than those anesthetized with isoflurane. Anesth Analg. 2008;106(1):264–269. doi: 10.1213/01.ane.0000287653.77372.d9. table of contents. [DOI] [PubMed] [Google Scholar]
- 9.Boccara G, Mann C, Pouzeratte Y, Bellavoir A, Rouvier A, Colson P. Improved postoperative analgesia with isoflurane than with propofol anaesthesia. Can J Anaesth. 1998;45(9):839–842. doi: 10.1007/BF03012216. [DOI] [PubMed] [Google Scholar]
- 10.Fassoulaki A, Melemeni A, Paraskeva A, Siafaka I, Sarantopoulos C. Postoperative pain and analgesic requirements after anesthesia with sevoflurane, desflurane or propofol. Anesth Analg. 2008;107(5):1715–1719. doi: 10.1213/ane.0b013e318182d84e. [DOI] [PubMed] [Google Scholar]
- 11.Pokkinen SM, Yli-Hankala A, Kalliomaki ML. The effects of propofol vs. sevoflurane on post-operative pain and need of opioid. Acta Anaesthesiol Scand. 2014;58(8):980–985. doi: 10.1111/aas.12366. [DOI] [PubMed] [Google Scholar]
- 12.Peng K, Liu HY, Wu SR, Liu H, Zhang ZC, Ji FH. Does propofol anesthesia lead to less postoperative pain compared with inhalational anesthesia?: A systematic review and meta-analysis. Anesth Analg. 2016;123(4):846–858. doi: 10.1213/ANE.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 13.Qiu Q, Choi SW, Wong SS, Irwin MG, Cheung CW. Effects of intra-operative maintenance of general anaesthesia with propofol on postoperative pain outcomes - a systematic review and meta-analysis. Anaesthesia. 2016;71(10):1222–1233. doi: 10.1111/anae.13578. [DOI] [PubMed] [Google Scholar]
- 14.Fulton B, Sorkin EM. Propofol. An overview of its pharmacology and a review of its clinical efficacy in intensive care sedation. Drugs. 1995;50(4):636–657. doi: 10.2165/00003495-199550040-00006. [DOI] [PubMed] [Google Scholar]
- 15.Smith I, White PF, Nathanson M, Gouldson R. Propofol. An update on its clinical use. Anesthesiology. 1994;81(4):1005–1043. [PubMed] [Google Scholar]
- 16.Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350(24):2441–2451. doi: 10.1056/NEJMoa032196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Habib AS, White WD, Eubanks S, Pappas TN, Gan TJ. A randomized comparison of a multimodal management strategy versus combination antiemetics for the prevention of postoperative nausea and vomiting. Anesth Analg. 2004;99(1):77–81. doi: 10.1213/01.ANE.0000120161.30788.04. [DOI] [PubMed] [Google Scholar]
- 18.Hofer CK, Zollinger A, Buchi S, et al. Patient well-being after general anaesthesia: a prospective, randomized, controlled multi-centre trial comparing intravenous and inhalation anaesthesia. Br J Anaesth. 2003;91(5):631–637. doi: 10.1093/bja/aeg243. [DOI] [PubMed] [Google Scholar]
- 19.Mukherjee K, Seavell C, Rawlings E, Weiss A. A comparison of total intravenous with balanced anaesthesia for middle ear surgery: effects on postoperative nausea and vomiting, pain, and conditions of surgery. Anaesthesia. 2003;58(2):176–180. doi: 10.1046/j.1365-2044.2003.02964_4.x. [DOI] [PubMed] [Google Scholar]
- 20.Bandschapp O, Filitz J, Ihmsen H, et al. Analgesic and antihyperalgesic properties of propofol in a human pain model. Anesthesiology. 2010;113(2):421–428. doi: 10.1097/ALN.0b013e3181e33ac8. [DOI] [PubMed] [Google Scholar]
- 21.Guindon J, LoVerme J, Piomelli D, Beaulieu P. The antinociceptive effects of local injections of propofol in rats are mediated in part by cannabinoid CB1 and CB2 receptors. Anesth Analg. 2007;104(6):1563–1569. doi: 10.1213/01.ane.0000263278.05423.a3. table of contents. [DOI] [PubMed] [Google Scholar]
- 22.Antognini JF, Wang XW, Piercy M, Carstens E. Propofol directly depresses lumbar dorsal horn neuronal responses to noxious stimulation in goats. Can J Anaesth. 2000;47(3):273–279. doi: 10.1007/BF03018926. [DOI] [PubMed] [Google Scholar]
- 23.Samir A, Gandreti N, Madhere M, Khan A, Brown M, Loomba V. Anti-inflammatory effects of propofol during cardiopulmonary bypass: a pilot study. Ann Card Anaesth. 2015;18(4):495–501. doi: 10.4103/0971-9784.166451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma X, Hu YW, Zhao ZL, et al. Anti-inflammatory effects of propofol are mediated by apolipoprotein M in a hepatocyte nuclear factor-1α-dependent manner. Arch Biochem Biophys. 2013;533:1–2. 1–10. doi: 10.1016/j.abb.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 25.Daskalopoulos R, Korcok J, Farhangkhgoee P, Karmazyn M, Gelb AW, Wilson JX. Propofol protection of sodium-hydrogen exchange activity sustains glutamate uptake during oxidative stress. Anesth Analg. 2001;93(5):1199–1204. doi: 10.1097/00000539-200111000-00030. [DOI] [PubMed] [Google Scholar]
- 26.Nemmani KV, Mogil JS. Serotonin-GABA interactions in the modulation of mu- and kappa-opioid analgesia. Neuropharmacology. 2003;44(3):304–310. doi: 10.1016/s0028-3908(02)00374-x. [DOI] [PubMed] [Google Scholar]
- 27.Goldstein FJ. Adjuncts to opioid therapy. J Am Osteopath Assoc. 2002;102(9 Suppl 3):S15–S21. [PubMed] [Google Scholar]
- 28.Yeo ST, Holdcroft A, Yentis SM, Stewart A. Analgesia with sevoflurane during labour: i. Determination of the optimum concentration. Br J Anaesth. 2007;98(1):105–109. doi: 10.1093/bja/ael326. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Y, Eger EI, 2nd, Dutton RC, Sonner JM. Inhaled anesthetics have hyperalgesic effects at 0.1 minimum alveolar anesthetic concentration. Anesth Analg. 2000;91(2):462–466. doi: 10.1097/00000539-200008000-00044. [DOI] [PubMed] [Google Scholar]
- 30.Stevens RJ, Rusch D, Davies PA, Raines DE. Molecular properties important for inhaled anesthetic action on human 5-HT3A receptors. Anesth Analg. 2005;100(6):1696–1703. doi: 10.1213/01.ANE.0000151720.36988.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rowley TJ, Daniel D, Flood P. The role of adrenergic and cholinergic transmission in volatile anesthetic-induced pain enhancement. Anesth Analg. 2005;100(4):991–995. doi: 10.1213/01.ANE.0000147708.73945.B3. [DOI] [PubMed] [Google Scholar]
- 32.Kingery WS, Agashe GS, Guo TZ, et al. Isoflurane and nociception: spinal alpha2A adrenoceptors mediate antinociception while supra-spinal alpha1 adrenoceptors mediate pronociception. Anesthesiology. 2002;96(2):367–374. doi: 10.1097/00000542-200202000-00023. [DOI] [PubMed] [Google Scholar]
- 33.Peng K, Liu HY, Liu SL, Ji FH. Dexmedetomidine-fentanyl compared with midazolam-fentanyl for conscious sedation in patients undergoing lumbar disc surgery. Clin Ther. 2016;38(1):192–201.e2. doi: 10.1016/j.clinthera.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 34.Peng K, Liu HY, Wu SR, Cheng H, Ji FH. Effects of combining dexmedetomidine and opioids for postoperative intravenous patient-controlled analgesia: a systematic review and meta-analysis. Clin J Pain. 2015;31(12):1097–1104. doi: 10.1097/AJP.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 35.Peng K, Jin XH, Liu SL, Ji FH. Effect of intraoperative dexmedetomidine on post-craniotomy pain. Clin Ther. 2015;37(5):1114–1121.e1. doi: 10.1016/j.clinthera.2015.02.011. [DOI] [PubMed] [Google Scholar]