Abstract
Objective
The study aimed to determine the prevalence and identify determinants of TB among People living with HIV/AIDS (PLWHAs) through reviewing and analyzing patient case files from the anti-retro viral treatment (ART) clinic of Yirgalem General Hospital, southern Ethiopia.
Results
Of the total PLWHAs involved in the study, 51 (36.9%) of them were found to have TB, and of which, 37 (72.5%) were smear negative cases. The multivariate analysis showed that PLWHA’s who are at WHO clinical stage 3 (AOR = 5.82; 95% CI 1.04–32.30), CD4 level of 200–500 cells/mm3 (AOR = 4.85; 95% CI 1.95–12.05) and < 200 cells/mm3 (AOR = 7.34; 95% CI 2.75–19.58) at ART initiation, and who didn’t take INH prophylaxis (AOR = 12.36; 95% CI 4.47–34.14) were significantly associated with TB-HIV co-infection. Rapid and sensitive diagnostic techniques should be implemented to early detect co-infections, and also INH prophylactic preventive measures should be strengthened to reduce TB incidence.
Electronic supplementary material
The online version of this article (10.1186/s13104-018-3530-3) contains supplementary material, which is available to authorized users.
Keywords: Tuberculosis, HIV/AIDS, Co-infection, PLWHA, Southern Ethiopia
Introduction
Tuberculosis (TB) remains a major public health problem in resource-limited countries and it is the largest cause of death among People living with HIV/AIDS (PLWHAs) worldwide. According to the WHO Global TB Report, there were an estimated 9 million new cases of TB occurred worldwide, of which 13% were associated with HIV/AIDS infection, and 78% of these HIV/AIDS associated cases occurred in Africa. It is further estimated that 1.49 million deaths from TB, including 0.36 million among PLWHAs, and 96% of the deaths occurred in developing countries. Ethiopia has been classified 7th among the 22 high burden countries with TB and HIV/AIDS infection in the world [1, 2].
HIV/AIDS predisposes for Mycobacterium tuberculosis (MTB) infection and increases the probability of recently acquired TB infection to progress to the status of active disease and increases the rate of recurrent TB. The lifetime risk of developing active TB in immune-competent adults is estimated to be 10%, but in PLWHAs who infected with MTB the annual risk of developing active TB disease exceeds 10% [3].
The current increasing HIV/AIDS associated tuberculosis shifted the clinical pattern of TB towards smears negative pulmonary TB (PTB) and extra-pulmonary TB (EPTB), which in turn, causes difficulties in the diagnosis and treatment of TB due to unusual clinical picture with increased smear negative acid fast Bacilli (AFB) PTB, atypical finding on chest radiography and increased prevalence of EPTB [4, 5].
Several studies documented that the clinical manifestations of TB in PLWHAs are quite varied and generally show different patterns as a function of the CD4+ T cell count. In addition, TB can appear at any stage of HIV/AIDS infection, and its presentation varies with the WHO stage and CD4+ lymphocyte count, although it is more frequent at CD4+ T cell count of < 300 cells/mm3 [6, 7].
In the study area, there is no adequate and recent data on the prevalence and determinants of TB in PLWHAs. Even though it is expected that the prevalence of TB among PLWHAs in the study area is assumed to be higher than other sites in the region due to the large number of PLWHAs treated in the ART clinic, this expectation should be supported by area specific study. The objective of the study was to determine the prevalence of TB and its determinant factors among PLWHAs in a local context that will help to reduce the burden of the disease by facilitating the early detection of at-risk patients and to serve as a reference document for further studies.
Main text
Methods
The study was conducted in Yirgalem General Hospital, which is found in Yirgalem town, Sidama Zone, southern Ethiopia. It serves around 4.2 million populations of Sidama Zone and part of southern Oromia region. A total of 5944 PLWHAs were registered since the ART clinic in the hospital had started its function in 2001. The trend of HIV/AIDS cases has decreased over time and the highest number of cases was registered in 2005/2006 with a total of 1219 cases.
A facility-based retrospective cross-sectional study was carried out to determine the prevalence of TB and identify its determinant factors among PLWHAs through reviewing and analyzing a 2 year (from January 1, 2015 to December 30, 2016) patient case files from the ART clinic of Yirgalem General Hospital. All PLWHAs attending the ART clinic of Yirgalem General Hospital during the study period were eligible for the study, and a total of 182 PLWHAs were diagnosed and treated during the period.
Taking the estimated proportion (P) of TB among PLWHAs = 0.1 [1], margin of error = 5% and confidence level = 95%; the calculated sample size became 138. The 2 years HIV/AIDS patients’ case files were identified and the study participants were selected by lottery method after excluding patients with incomplete medical records.
Data was collected from patients’ case files using a checklist which was prepared by adopting previous studies [6–8]. The checklist was pre-tested before the actual data collection and some variables like adherence to ART medications and nutritional status were omitted because of incomplete medical records. Otherwise, the checklist was inclusive of the different variables (age, sex, occupation, residence, INH prophylaxis, CD4 count, ART status) which were assumed as possible determinants of TB occurrence among PLWHAs.
The data were entered, cleaned and analyzed using SPSS version 19 statistical software. Frequencies and percentages were calculated for descriptive analysis of socio-demographic, clinical and laboratory profile of the study participants. Binary and multiple logistic regression analyses were applied to determine associations and identify risk factors of TB occurrence among PLWHAs taking P ≤ 0.05 for statistical significance.
Results
A total of 138 PLWHA’s medical records were reviewed and most of the participants were females (57.9%), aged 16–45 years (83.3%), urban residents (56.5%) and Protestants (52.2%) by religion. Moreover, 65 (48.9%) of the study participants were married and 73 (54.9%) of them attended primary school (Additional file 1: Table S1).
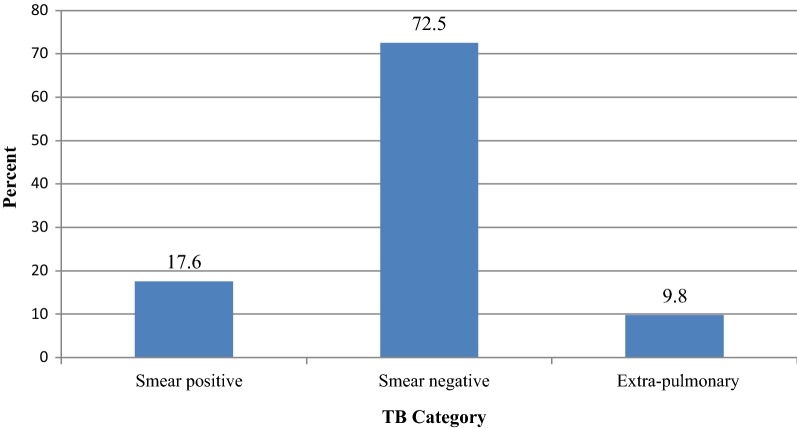
Of the total PLWHAs involved in the study, 51 (36.9%) of them were found to have TB; and of the 51 with TB, 37 (72.5%) were smear negative cases (Fig. 1). In addition, 37 (72.5%), 9 (17.6%) and 3 (5.9%) of the TB positive patients were diagnosed by chest x-ray, microscopy (AFB) and biopsy, respectively.
Fig. 1.
Types of TB among PLWHAs, Yirgalem General Hospital, southern Ethiopia; January 2015 to December 2016.
 TB category
TB category
Out of the total selected PLWHAs, 47 (34%) of them didn’t take INH prophylaxis; and among them, 35 (74.5%) were TB positive patients. Furthermore, 126 (91.3%) of the study participants had started ART, and of them 61 (48.4%) had CD4 level of < 200 cells/mm3 at ART initiation (Table 1).
Table 1.
Clinical and laboratory profiles of study participants in Yirgalem General Hospital, southern Ethiopia; January 2015 to December 2016
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| TB diagnosis | Positive | 51 | 37.0 |
| Negative | 87 | 63.0 | |
| Total | 138 | 100 | |
| INH prophylaxis | Yes | 91 | 65.9 |
| No | 47 | 34.1 | |
| Total | 138 | 100 | |
| WHO stage | Stage 1 | 66 | 47.8 |
| Stage 2 | 30 | 21.7 | |
| Stage 3 | 29 | 21.0 | |
| Stage 4 | 13 | 9.4 | |
| Total | 138 | 100 | |
| ART status | Pre-ART | 12 | 8.7 |
| ART | 126 | 91.3 | |
| Total | 138 | 100 | |
| CD4 level at ART initiation | > 500 | 21 | 16.7 |
| 200–500 | 44 | 34.9 | |
| < 200 | 61 | 48.4 | |
| Total | 126 | 100 | |
| CD4 level during diagnosis | > 500 | 27 | 19.9 |
| 200–500 | 49 | 36.0 | |
| < 200 | 60 | 44.1 | |
| Total | 136 | 100 |
The bivariate analysis result showed that residence, INH prophylaxis status, WHO clinical stage and CD4 level at ART initiation were associated with TB-HIV/AIDS co-infection. In the multivariate analysis, multiple logistic regression was used to identify determinants of TB occurrence among PLWHAs. Being at WHO clinical stage 3 (AOR = 5.82; 95% CI 1.04–32.30), not taking INH prophylaxis (AOR = 12.36; 95% CI 4.47–34.14), CD4 level of < 200 cells/mm3 (AOR = 7.34; 95% CI 2.75–19.58) and a CD4 level of 200–500 cells/mm3 (AOR = 4.85; 95% CI 1.95–12.05) at ART initiation were significant determinants of increased risk of TB co-infection among PLWHAs (Table 2).
Table 2.
Determinant factors of TB-HIV co-infection among PLWHAs, Yirgalem General Hospital, southern Ethiopia, 2017
| Variables | TB disease | COR (95% CI) | AOR (95% CI) | P value | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Age (years) | |||||
| < 15 | 2 | 3 | 1.12 (1.16–9.01) | ||
| 16–45 | 41 | 74 | 1.44 (0.52–9.94) | ||
| ≥ 46 | 8 | 10 | 1 | ||
| Sex | |||||
| Male | 21 | 37 | 1.05 (0.52–2.13) | ||
| Female | 30 | 50 | 1 | ||
| Residence | |||||
| Urban | 24 | 54 | 1 | 1 | |
| Rural | 27 | 33 | 0.54 (0.27–1.09) | 0.65 (0.23–1.77) | 0.40 |
| Occupation | |||||
| Housewife | 18 | 31 | 1 | ||
| Government employee | 4 | 8 | 1.16 (0.30–4.40) | ||
| Merchant | 9 | 12 | 0.77 (0.27–2.19) | ||
| Farmer | 6 | 11 | 1.06 (0.33–3.36) | ||
| Student | 5 | 4 | 0.46 (0.11–1.95) | ||
| Daily laborer | 3 | 2 | 0.38 (0.05–2.54) | ||
| Unemployed | 3 | 1 | 1.19 (0.01–2.00) | ||
| Marital status | |||||
| Married | 26 | 47 | 1 | ||
| Single | 10 | 17 | 0.94 (0.37–2.35) | ||
| Divorced | 11 | 15 | 0.75 (0.30–1.88) | ||
| Widowed | 3 | 4 | 0.73 (0.5–3.55) | ||
| INH prophylaxis | |||||
| Yes | 16 | 75 | 1 | 1 | |
| No | 35 | 12 | 13.67 (5.84–31.96) | 12.36 (4.47–34.14) | < 0.01* |
| ART profile | |||||
| Pre-ART | 3 | 9 | 1.84 (0.47–7.15) | ||
| ART | 48 | 78 | 1 | ||
| WHO stage | |||||
| Stage 1 | 0 | 66 | 1 | 1 | |
| Stage 2 | 10 | 20 | 0.61 (0.15–2.42) | 0.74 (0.12–4.32) | 0.16 |
| Stage 3 | 21 | 8 | 7.20 (2.00–25.90) | 5.82 (1.04–32.30) | 0.002* |
| Stage 4 | 8 | 5 | 3.20 (0.82–12.35) | 2.10 (0.35–12.37) | 0.06 |
| CD4 level at ART initiation | |||||
| > 500 | 5 | 16 | 1 | 1 | |
| 200–500 | 13 | 31 | 2.30 (1.01–5.23) | 4.85 (1.95–12.05) | < 0.01* |
| < 200 | 30 | 31 | 3.09 (1.00–9.51) | 7.34 (2.75–19.58) | < 0.01* |
* Statistically significant at P < 0.05
Discussion
Tuberculosis is a well-recognized opportunistic infection in patients with HIV/AIDS. In our study, we found that TB-HIV/AIDS co-infection was 36.9% and it was higher than the findings of other studies [5, 8–10]. This variation in the magnitude of tuberculosis in PLWHAs may be due to high TB detection rate as a result of availability of TB-diagnostic facilities or due to differences in HIV/AIDS infection rate at the population level.
The other relevant finding is that 72.5% of the TB-HIV/AIDS co-infected cases were smear-negative and this result is higher than the findings of other studies conducted elsewhere [7, 8]. This higher smear negativity indicates the importance of TB diagnostic techniques, other than AFB microscopy. In the study area, clinical data is supplemented with chest radiography to diagnose suspicious smear negative cases.
INH prophylaxis status, being at WHO clinical stage of 3, having a CD4 level of 200–500 and < 200 cells/mm3 at ART initiation were identified as risk factors of TB occurrence among PLWHAs. These findings are in line with other Hospital-based studies in Ethiopia [7, 8].
Our study revealed a poor INH prophylactic management for PLWHAs. But, the role of INH prophylaxis in the reduction of TB incidence has been reported in many clinical trials and found to be important [3]. The most important determinant factor for development of TB in PLWHAs is the immunologic state of the person and maintaining the CD4+ lymphocyte cell count level as high as possible helps the person to have a low risk of infection.
Conclusions
In our study, the prevalence of TB and the proportion of smear negative TB among PLWHAs was high. The risk of TB occurrence was found to be high among PLWHAs with WHO clinical stage 3, low CD4 level at ART initiation and PLWHAs who didn’t receive INH prophylaxis.
The high proportion of smear negative TB cases among PLWHAs requires special attention for confirming clinically suspected TB cases; and in addition to clinical and radiological investigations, rapid and sensitive diagnostic techniques like Culture, Fluorescent Microscopy and Xpert MTB/RIF should be implemented by Yirgalem General Hospital. Furthermore, our study revealed a poor INH prophylactic management for PLWHAs, and therefore, INH prophylactic preventive measures should be strengthened in the Hospital to reduce TB incidence among PLWHAs.
Limitations
Despite the study’s endeavor of identifying determinants of TB infection among PLWHAs, as the study is a facility based study undertaken in a single hospital with limited number of patients, it is difficult to make generalizations and future community-based studies are needed to substantiate the study findings.
Additional file
Additional file 1: Table S1. Socio-demographic profile of study participants in Yirgalem General Hospital, southern Ethiopia; January 2015 to December 2016.
Authors’ contributions
Conceived and designed the study: AN, TB, DD, FT. Performed the data collection: TB, DD, FT. Analysed the data: AN, TB, DD, FT. Supervised the conduct of the study: AN. Wrote the manuscript: AN. All authors read and approved the final manuscript.
Acknowledgements
We would like to acknowledge Yirgalem Hospital Medical College for funding this research. We are grateful to Yirgalem General Hospital and ART clinic staffs for their support and cooperation.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research protocol was approved by the Ethical Review Committee of Yirgalem Hospital Medical College and prior permission to collect data was obtained from Yirgalem General Hospital. The study subjects were identified using codes and no identifier information was recorded to ensure confidentiality.
Funding
This study was funded by Yirgalem Hospital Medical College, Ethiopia. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- AFB
acid fast Bacilli
- AOR
adjusted odds ratio
- ART
anti-retro viral treatment
- EPTB
extra-pulmonary tuberculosis
- MTB
Mycobacterium tuberculosis
- PLWHA
People living with HIV/AIDS
- PTB
pulmonary tuberculosis
- TB
tuberculosis
- WHO
World Health organization
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s13104-018-3530-3) contains supplementary material, which is available to authorized users.
Contributor Information
Abel Negussie, Email: abelnegussie@ymail.com.
Damene Debalke, Email: damene.d@yahoo.com.
Teshome Belachew, Email: teshomebelachew5@gmail.com.
Fetlework Tadesse, Email: fetleworktadesse@gmail.com.
References
- 1.Federal Ministry of Health (Ethiopia) Guidelines for clinical and programmatic management of TB, TB/HIV/AIDS and leprosy in Ethiopia. 5. Addis Ababa: Federal Ministry of Health; 2013. [Google Scholar]
- 2.World Health Organization . Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV/AIDS infection: recommendations for a public health approach. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 3.Kasper DL, Hauser SL, Jameson JL, Fauci AS, Longo DL, Loscalzo J. Harrison’s principles of internal medicine. 19. New York: McGraw-Hill Education; 2015. [Google Scholar]
- 4.Ejeta E. HIV co-infection among tuberculosis patients on Directly Observed Treatment Short Course in Western Ethiopia. Nat Sci. 2014;12(9):68–72. doi: 10.3855/jidc.5963. [DOI] [PubMed] [Google Scholar]
- 5.Giri PA, Deshpande D, Phalke DB. Prevalence of pulmonary tuberculosis among HIV positive patients attending antiretroviral therapy clinic. N Am J Med Sci. 2013;5(6):367–370. doi: 10.4103/1947-2714.114169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ngowi BJ, Mfinanga SG, Bruun JN, Morkve O. Pulmonary tuberculosis among people living with HIV/AIDS attending care and treatment in rural northern Tanzania. BMC Public Health. 2008;8:341. doi: 10.1186/1471-2458-8-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wondimeneh Y, Muluye D, Belyhun Y. Prevalence of pulmonary tuberculosis and immunological profile of HIV co-infected patients in Northwest Ethiopia. BMC Res Notes. 2012;5:331. doi: 10.1186/1756-0500-5-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fekadu S, Teshome W, Alemu G. Prevalence and determinants of tuberculosis among HIV infected patients in south Ethiopia. J Infect Dev Ctries. 2015;9(8):898–904. doi: 10.3855/jidc.5667. [DOI] [PubMed] [Google Scholar]
- 9.Mitku AA, Dessie ZG, Muluneh EK, Workie DL. Prevalence and associated factors of TB/HIV co-infection among HIV Infected patients in Amhara region, Ethiopia. Afr Health Sci. 2016;16(2):588–595. doi: 10.4314/ahs.v16i2.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mekonnen D, Derbie A, Desalegn E. TB/HIV co-infections and associated factors among patients on directly observed treatment short course in Northeastern Ethiopia: a 4 years retrospective study. BMC Res Notes. 2015;8:666. doi: 10.1186/s13104-015-1664-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Socio-demographic profile of study participants in Yirgalem General Hospital, southern Ethiopia; January 2015 to December 2016.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.