Abstract
IMPORTANCE
Previous epidemiologic research on concussions has primarily been limited to patient populations presenting to sport concussion clinics or to emergency departments (EDs) and to those high school age or older. By examining concussion visits across an entire pediatric health care network, a better estimate of the scope of the problem can be obtained.
OBJECTIVE
To comprehensively describe point of entry for children with concussion, overall and by relevant factors including age, sex, race/ethnicity, and payor, to quantify where children initially seek care for this injury.
DESIGN, SETTING, AND PARTICIPANTS
In this descriptive epidemiologic study, data were collected from primary care, specialty care, ED, urgent care, and inpatient settings. The initial concussion-related visit was selected and variation in the initial health care location (primary care, specialty care, ED, or hospital) was examined in relation to relevant variables. All patients aged 0 to 17 years who received their primary care from The Children’s Hospital of Philadelphia’s (CHOP) network and had 1 or more in-person clinical visits for concussion in the CHOP unified electronic health record (EHR) system (July 1, 2010, to June 30, 2014) were selected.
MAIN OUTCOMES AND MEASURES
Frequency of initial concussion visits at each type of health care location. Concussion visits in the EHR were defined based on International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes indicative of concussion.
RESULTS
A total of 8083 patients were included (median age, 13 years; interquartile range, 10–15 years). Overall, 81.9% (95% CI, 81.1%–82.8%; n = 6624) had their first visit at CHOP within primary care, 5.2% (95% CI, 4.7%–5.7%; n = 418) within specialty care, and 11.7% (95% CI, 11.0%–12.4%; n = 947) within the ED. Health care entry varied by age: 52% (191/368) of children aged 0 to 4 years entered CHOP via the ED, whereas more than three-quarters of those aged 5 to 17 years entered via primary care (5–11 years: 1995/2492; 12–14 years: 2415/2820; and 15–17 years: 2056/2403). Insurance status also influenced the pattern of health care use, with more Medicaid patients using the ED for concussion care (478/1290 Medicaid patients [37%] used the ED vs 435/6652 private patients [7%] and 34/141 self-pay patients [24%]).
CONCLUSIONS AND RELEVANCE
The findings suggest estimates of concussion incidence based solely on ED visits underestimate the burden of injury, highlight the importance of the primary care setting in concussion care management, and demonstrate the potential for EHR systems to advance research in this area.
Concussion in youth has received heightened attention owing to emerging evidence that this common injury can affect academics and cause behavioral changes and neurocognitive deficits in working memory, concentration, processing speed, and eye and motor function.1–3 Reported estimates of the number of youth with concussion have increased in recent years, likely owing in part to increased involvement in youth sports, introduction of return-to-play legislation, and increased awareness of concussion by clinicians, parents, and youth themselves.1,4–6
Concussion diagnosis remains symptom-based and does not require advanced diagnostic tools such as imaging.7 Thus, unlike many other types of traumatic injuries, children with concussion potentially enter the health care system through a variety of portals, including primary care or specialty care such as sports medicine or neurology, in addition to the emergency department (ED) and urgent care. A previous study highlighted the diversity of health care use for youth with concussion and minor head injury based on private insurance data, emphasizing the importance of primary care clinicians.8 However, pediatricians noted that they lack up-to-date concussion training and/or resources needed for timely and accurate diagnosis and ongoing case management.9 A more complete understanding of the distribution of point of health care entry for children with concussion is needed to guide both health care networks and clinicians where targeted training and resources need to be deployed.
In addition, an Institute of Medicine (IOM) report highlighted the lack of data on concussions treated outside the ED setting or sustained outside organized high school or collegiate athletics.1,10–12 Prior efforts have either focused on a single sport, used EDs as the sole site of identification, or studied a broader spectrum of head injury.13–22 In response to the IOM report, several initiatives are under way that are attempting to better estimate youth concussion incidence. To give guidance as to the needed breadth of those efforts and to identify locations in the health care system that need to be skilled in concussion diagnosis and initial management, we leveraged the linked electronic health record (EHR) system at The Children’s Hospital of Philadelphia (CHOP) to comprehensively describe point of entry into a large, regional, pediatric health care network for CHOP primary care patients who sustained concussions from July 2010 through June 2014; distributions were assessed over time across broad age, demographic, and socioeconomic characteristics.
Methods
Description of CHOP Network
The CHOP network encompasses more than 50 locations throughout southeastern Pennsylvania and southern New Jersey, including 31 primary care centers, 14 specialty care centers, a 535-bed inpatient hospital, 2 EDs, and 2 urgent care centers supporting more than 1 million visits annually. The CHOP network serves a socioeconomically and racially/ethnically diverse population and accepts most insurance plans, including Medicaid. In addition to primary care clinicians, sports medicine, neurology, and trauma care clinicians at CHOP evaluate and manage concussions using a linked EHR system(Epic-Care; Epic Systems Inc). The EHR is used for all aspects of clinical care, from inpatient to outpatient settings, as well as initial and follow-up office visits.
This study was reviewed and approved by the CHOP institutional review board. Consent was waived because the research was limited to existing data and involved no more than minimal risk to the patient, and the research could not be practicably carried out without the waiver.
Case Identification
We queried CHOP’s EHR database to identify all CHOP primary care patients who were aged 0 to 17 years and who had an initial in-person medical visit at CHOP related to concussion from July 1, 2010, through June 30, 2014. Concussion visits were defined as those assigned an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code indicative of concussion (Table 1). Primary care patients were identified as those with at least 1 primary care visit to a CHOP primary care network location during the study period; the study was limited to patients whose primary care is normally delivered by the CHOP network because we expect the distribution of entry locations for this group to be amore accurate representation of patient behavior in using the CHOP health care system for concussion than all patients of the CHOP health care network. Initial visits were defined as the first clinical encounter for a concussion as determined by date and time of the encounter. Because we could not separate multiple concussions that may have been sustained by an individual patient owing to limitations of CHOP’s EHR system, each patient was counted only once in analyses.
Table 1.
Concussion-Related ICD-9-CM Codes
| ICD-9-CM Code | Description |
|---|---|
| 800.02 | Fracture of vault of skull with brief (< 1 h) LOC |
| 800.09 | Closed fracture of vault of skull without mention of intracranial injury, with concussion, unspecified |
| 800.52 | Open fracture of vault of skull without mention of intracranial injury, with brief (< 1 h) LOC |
| 800.59 | Open fracture of vault of skull without mention of intracranial injury, with concussion, unspecified |
| 801.02 | Closed fracture of base of skull without mention of intracranial injury, with brief (< 1 h) LOC |
| 801.09 | Closed fracture of base of skull without mention of intracranial injury, with concussion, unspecified |
| 801.39 | Closed fracture of base of skull with concussion, unspecified |
| 801.52 | Open fracture of base of skull without mention of intracranial injury with brief (< 1 h) LOC |
| 801.56 | Open fracture of base of skull without mention of intracranial injury with LOC of unspecified duration |
| 801.59 | Open fracture of base of skull without mention of intracranial injury, with concussion, unspecified |
| 803.02 | Other and unqualified skull fractures with brief (<1 h) LOC |
| 803.09 | Other and unqualified skull fractures with concussion, unspecified |
| 803.52 | Other open skull fracture without mention of intracranial injury with brief (<1 h) LOC |
| 803.59 | Other open skull fracture without mention of intracranial injury, with concussion, unspecified |
| 804.02 | Closed fractures involving skull or face with other bones, without mention of intracranial injury, with brief (<1 h) LOC |
| 804.09 | Closed fractures involving skull of face with other bones, without mention of intracranial injury, with concussion, unspecified |
| 804.52 | Open fractures involving skull or face with other bones, without mention of intracranial injury, with brief (<1 h) LOC |
| 850 | Concussion |
| 850.0 | Concussion with no LOC |
| 850.1 | Concussion with brief LOC |
| 850.10 | Concussion with brief LOC |
| 850.11 | Concussion, with LOC of ≤30 min |
| 850.5 | Concussion with LOC of unspecified duration |
| 850.9 | Concussion, unspecified |
Abbreviations: ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; LOC, loss of consciousness.
Given that the focus of this analysis was on patients whose concussion was their only traumatic brain injury, as well as to minimize concussion misclassification, we excluded patients who were also assigned an ICD-9-CM code for a more severe traumatic brain injury (codes included the following key words/phrases: contusion, laceration, subarachnoid, subdural, epidural, other and unspecified intracranial hemorrhage, and moderate or prolonged loss of consciousness) within 2 weeks of the initial concussion visit (n = 20). In addition, patients with clinically important injuries to body regions other than the brain were excluded (n = 298); this was assessed by identifying ICD- 9-CM codes corresponding to other injuries on the same day as the initial concussion visit. Last, patients who were receiving ongoing concussion treatment during the study period but whose initial concussion visit occurred prior to July 1, 2010, were excluded (n = 121).
Variable Definitions
Potential points of entry within the CHOP health care network included (1) 1 of the primary care network offices; (2) outpatient specialty care, including orthopedics/sports medicine, trauma, and neurology; (3) 1 of 2 EDs or 2 urgent care centers; and (4) direct admission to the hospital. Race/ethnicity, sex, age, and payor (Medicaid, private, vs self-pay) at time of initial concussion visit were ascertained from the EHR.
Statistical Analysis
The distribution of initial concussion visit location was described by age, sex, payor, and race/ethnicity; Wald 95% CIs based on a normal approximation to the binomial distribution were calculated using the surveyfreq procedure in SAS. In addition, during May and June 2012, extensive training was provided to CHOP primary care clinicians on the current standard of care and approach for diagnosing and managing concussions. Therefore, analyses were conducted looking both at the overall 4-year period, as well as stratified by date of initial concussion visit: July 2010 to June 2012 and July 2012 to June 2014. All analyses were conducted in SAS version 9.3 (SAS Institute Inc).
Results
A total of 8083 children aged 17 years and younger had an initial in-person clinical visit for concussion (without a more severe head injury or other clinically significant injury) within the CHOP network during the 4-year study period. The frequency and proportion of relevant characteristics at the time of initial concussion visit are shown in Table 2. The median age of patients was 13 years (interquartile range, 10–15 years); 4.6% (n = 368) were aged 0 to 4 years, 30.8% (n = 2492) were aged 5 to 11 years, 34.9% (n = 2820) were aged 12 to 14 years, and 29.7% (n = 2403) were aged 15 to 17 years. Most were non-Hispanic white (n = 5729; 70.9%) and had private insurance (n = 6652; 82.3%). Almost two-thirds of all visits occurred from July 2012 to June 2014 (n = 5026).
Table 2.
Patient Characteristics at Time of Initial Concussion Visit to CHOP Health Care Network
| Characteristic | CHOP Primary Care Patients (N = 8083), No. (%) |
|---|---|
| Age at first concussion-related encounter, y | |
| 0–4 | 368 (4.6) |
| 5–11 | 2492 (30.8) |
| 12–14 | 2820 (34.9) |
| 15–17 | 2403 (29.7) |
| Sex | |
| Male | 4494 (55.6) |
| Female | 3589 (44.4) |
| Race/ethnicity | |
| Non-Hispanic white | 5729 (70.9) |
| Non-Hispanic black | 1383 (17.1) |
| Hispanic | 257 (3.2) |
| Non-Hispanic Asian/Asian Pacific Islander/other/multiple race | 134 (1.7) |
| Unknown | 580 (7.2) |
| Payor of encounter | |
| Private | 6652 (82.3) |
| Medicaid | 1290 (16.0) |
| Self-pay | 141 (1.7) |
Abbreviation: CHOP, The Children’s Hospital of Philadelphia.
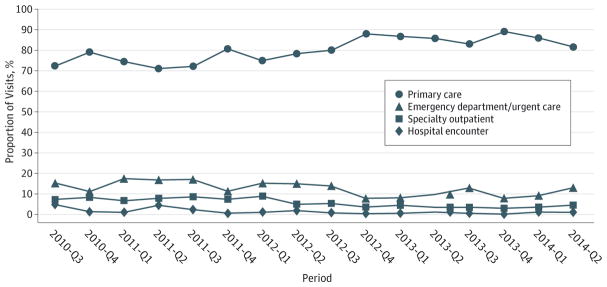
Overall, 81.9% (95% CI, 81.1%–82.8%; n = 6624) of patients had their first concussion visit at CHOP within primary care, 5.2% (95% CI, 4.7%–5.7%; n = 418)within specialty care, 11.7% (95% CI, 11.0%–12.4%; n = 947)within the ED, and 1.2% (95% CI, 0.9%–1.4%; n = 94) direct admit to the hospital (Table 3). The proportion of CHOP primary care patients who sought care at their primary care office increased 13% between July to September 2010 and April to June 2014 (72.4%, 184/254 to 81.7%, 503/616), while the proportion seeking care at the ED decreased 16% over the same period (15.4%, 39/254 to 13.0%, 80/616) (Figure).
Table 3.
Distribution of Health Care Location of Initial Concussion Visit, Overall and by Relevant Factors, for CHOP Primary Care Patients Only (N = 8083)
| Factor | Overall (N = 8083) | July 2010–June 2012 (n = 3057) | July 2012–June 2014 (n = 5026) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||
| No. | No. (%) | No. | No. (%) | No. | No. (%) | ||||||||||
|
|
|
|
|||||||||||||
| ED/Urgent Care |
Hospital Encounter |
Primary Care |
Specialty Outpatient |
ED/Urgent Care |
Hospital Encounter |
Primary Care |
Specialty Outpatient |
ED/Urgent Care |
Hospital Encounter |
Primary Care |
Specialty Outpatient |
||||
| Age at first concussion-related encounter, y | |||||||||||||||
|
| |||||||||||||||
| All age groups | 8083 | 947 (11.7) | 94 (1.2) | 6624 (81.9) | 418 (5.2) | 3057 | 445 (14.6) | 58 (1.9) | 2325 (76.1) | 229 (7.5) | 5026 | 502 (10.0) | 36 (0.7) | 4299 (85.5) | 189 (3.8) |
|
| |||||||||||||||
| 0–4 | 368 | 191 (51.9) | 16 (4.3) | 158 (42.9) | 3 (0.8) | 183 | 103 (56.3) | 9 (4.9) | 69 (37.7) | 2 (1.1) | 185 | 88 (47.6) | 7 (3.8) | 89 (48.1) | 1 (0.5) |
|
| |||||||||||||||
| 5–11 | 2492 | 371 (14.9) | 45 (1.8) | 1995 (80.1) | 81 (3.3) | 853 | 168 (19.7) | 27 (3.2) | 613 (71.9) | 45 (5.3) | 1639 | 203 (12.4) | 18 (1.1) | 1382 (84.3) | 36 (2.2) |
|
| |||||||||||||||
| 12–14 | 2820 | 222 (7.9) | 18 (0.6) | 2415 (85.6) | 165 (5.9) | 1036 | 93 (9.0) | 11 (1.1) | 845 (81.6) | 87 (8.4) | 1784 | 129 (7.2) | 7 (0.4) | 1570 (88.0) | 78 (4.4) |
|
| |||||||||||||||
| 15–17 | 2403 | 163 (6.8) | 15 (0.6) | 2056 (85.6) | 169 (7.0) | 985 | 81 (8.2) | 11 (1.1) | 798 (81.0) | 95 (9.6) | 1418 | 82 (5.8) | 4 (0.3) | 1258 (88.7) | 74 (5.2) |
|
| |||||||||||||||
| Sex | |||||||||||||||
|
| |||||||||||||||
| Male | 4494 | 604 (13.4) | 56 (1.2) | 3601 (80.1) | 233 (5.2) | 1822 | 291 (16.0) | 36 (2.0) | 1361 (74.7) | 134 (7.4) | 2672 | 313 (11.7) | 20 (0.7) | 2240 (83.8) | 99 (3.7) |
|
| |||||||||||||||
| Female | 3589 | 343 (9.6) | 38 (1.1) | 3023 (84.2) | 185 (5.2) | 1235 | 154 (12.5) | 22 (1.8) | 964 (78.1) | 95 (7.7) | 2354 | 189 (8.0) | 16 (0.7) | 2059 (87.5) | 90 (3.8) |
|
| |||||||||||||||
| Race/ethnicity | |||||||||||||||
|
| |||||||||||||||
| Non-Hispanic white | 5729 | 280 (4.9) | 32 (0.6) | 5073 (88.5) | 344 (6.0) | 2144 | 133 (6.2) | 20 (0.9) | 1794 (83.7) | 197 (9.2) | 3585 | 147 (4.1) | 12 (0.3) | 3279 (91.5) | 147 (4.1) |
|
| |||||||||||||||
| Non-Hispanic black | 1383 | 586 (42.4) | 55 (4.0) | 698 (50.5) | 44 (3.2) | 585 | 284 (48.5) | 32 (5.5) | 249 (42.6) | 20 (3.4) | 798 | 302 (37.8) | 23 (2.9) | 449 (56.3) | 24 (3.0) |
|
| |||||||||||||||
| Hispanic | 257 | 32 (12.5) | 3 (1.2) | 215 (83.7) | 7 (2.7) | 97 | 14 (14.4) | 2 (2.1) | 77 (79.4) | 4 (4.1) | 160 | 18 (11.3) | 1 (0.6) | 138 (86.3) | 3 (1.9) |
|
| |||||||||||||||
| Non-Hispanic Asian/Asian Pacific Islander/other/multiple race | 134 | 24 (17.9) | 2 (1.5) | 99 (73.9) | 9 (6.7) | 39 | 9 (23.1) | 2 (5.1) | 26 (66.7) | 2 (5.1) | 95 | 15 (15.8) | 0 (0) | 73 (76.8) | 7 (7.4) |
|
| |||||||||||||||
| Unknown | 580 | 25 (4.3) | 2 (0.3) | 539 (92.9) | 14 (2.4) | 192 | 5 (2.6) | 2 (1.0) | 179 (93.2) | 6 (3.1) | 388 | 20 (5.2) | 0 (0) | 360 (92.8) | 8 (2.1) |
|
| |||||||||||||||
| Payor of encounter | |||||||||||||||
|
| |||||||||||||||
| Private | 6652 | 435 (6.5) | 47 (0.7) | 5789 (87.0) | 381 (5.7) | 2502 | 208 (8.3) | 31 (1.2) | 2057 (82.2) | 206 (8.2) | 4150 | 227 (5.5) | 16 (0.4) | 3732 (89.9) | 175 (4.2) |
|
| |||||||||||||||
| Medicaid | 1290 | 478 (37.1) | 45 (3.5) | 735 (57.0) | 32 (2.5) | 499 | 225 (45.1) | 26 (5.2) | 229 (45.9) | 19 (3.8) | 791 | 253 (32.0) | 19 (2.4) | 506 (64.0) | 13 (1.6) |
|
| |||||||||||||||
| Self-pay | 141 | 34 (24.1) | 2 (1.4) | 100 (70.9) | 5 (3.5) | 56 | 12 (21.4) | 1 (1.8) | 39 (69.6) | 4 (7.1) | 85 | 22 (25.9) | 1 (1.2) | 61 (71.8) | 1 (1.2) |
Abbreviations: CHOP, The Children’s Hospital of Philadelphia; ED, emergency department.
Figure 1.
Proportion of Concussion Visits by Initial Point of Health Care Entry Over Time Among The Children’s Hospital of Philadelphia Primary Care Patients (N = 8083)
Table 3 illustrates the distribution of health care entry location by age, sex, race/ethnicity, payor, and period. Location of entry varied significantly by age. More than half of children aged 0 to 4 years entered the CHOP network via the ED (51.9%; 95% CI, 46.8%–57.0%; 191/368), a significantly higher proportion than for older children (14.9% [371/2492] of those aged 5–11 years [95% CI, 13.5%–16.3%]; 7.9% [222/2820] of those aged 12–14 years [95% CI, 6.9%–8.9%]; and 6.8% [163/2403] of those aged 15–17 years [95% CI, 5.8%–7.8%]). Conversely, more than three-quarters of those aged 5 to 17 years (5–11 years: 1995/2492; 12–14 years: 2415/2820; and 15–17 years: 2056/2403) initially sought care at CHOP via primary care. There were also important differences by race/ethnicity and payor: 42.4% (95% CI, 39.8%–45.0%; 586/1383) of non-Hispanic black patients entered via the ED compared with 4.9% (95% CI, 4.3%–5.4%; 280/5729) of non-Hispanic white patients. Similarly, 37.1% (95% CI, 34.4%–39.7%; 478/1290) of children insured by Medicaid and 24.1% (95% CI, 17.1%–31.2%; 34/141) who were self-pay entered through the ED compared with 6.5% (95% CI, 5.9%–7.1%; 435/6652) with private insurance.
Discussion
While our understanding of concussion as an important public health issue among children has grown tremendously over the last decade, as highlighted in a recent IOM report,1 the epidemiology of youth concussion has been limited primarily to those who are high school age or older, participate in organized sports, and/or are treated in EDs. In this study, we leveraged the strength of a linked EHR system throughout a large health care network to provide a comprehensive description of the point of health care entry specific for pediatric concussion across the developmental age spectrum—the first such US assessment to include a diverse demographic and socioeconomic sample. By doing so, we discovered important insights into the variations in point of entry by age, payor, and race/ethnicity that will provide guidance to the future development of youth concussion surveillance systems being designed to provide national incidence estimates. In addition, our results highlighted the potential of EHR systems to facilitate research in this field.
First, the findings confirmed that concussions occur among children of all ages: approximately one-third of patients (2860/8083)were younger than 12 years. In contrast, most pediatric concussion research has focused on youth of high school age, resulting in limited knowledge about the natural history of concussion in a middle or elementary school population.23 Owing to the evolving neuropsychology and neurophysiology across the pediatric age range, it is likely that children manifest concussion symptoms differently across the age continuum.24 Our findings underscore the critical need for future research ensuring validated, age-appropriate diagnostic and treatment strategies are available across the entire pediatric age range.
Second, our results illustrate that more than three-fourths of the patients (6624/8083) had their first concussion visit within the CHOP network with primary care and just over 10% (947/8083) within the ED, suggesting that concussion estimates based solely on ED visits likely substantially underestimate the true incidence of this injury in children. A study linking multiple population-based health administration databases in Canada25 and a study using data on private insurance claims in Massachusetts8 documented a similar increase over time in concussions and minor head injuries treated during office visits (eg, primary care and specialty care) compared with treatment within EDs. Our study uniquely extends these findings in 2 ways. First, we used a stricter definition of concussion by excluding minor head injuries that were not diagnosed as concussions. More importantly, by capturing cases across broad demographics and socioeconomics throughout an entire health care network, we identified important variations in health care use by insurance payor and other demographic subgroups.
Our results highlight the critical importance of primary care clinicians in concussion care. This may be driven in part by insurance reasons or the fact that patients can often be scheduled for office appointments in the primary care setting sooner and at lesser expense than in specialty care or the ED. Regardless of the reason, these data provide critical guidance to health care networks, alerting them that the primary care setting is increasingly being used for concussion care and those clinicians may be in need of augmented training or increased resources. For primary care clinicians, these data provide evidence they can use to advocate for concussion clinical decision support tools in their health care system. Because specialized equipment is currently not needed for diagnosis, primary care clinicians can be well positioned to provide the initial evaluation for most patients with concussion. In some geographic areas, they may be the only available clinical resource. Preliminary findings suggest that primary care clinicians can in fact provide quality care to children with concussion.26 The care partnership between specialists and primary care that has occurred in the diagnosis and treatment of pediatric mental health disorders, such as attention-deficit/hyperactivity disorder, suggests there are models for successful clinical collaboration.
We also observed important variations in health care use among different subgroups. Children younger than 5 years old were more likely than older children to have the ED as their initial point of entry into the CHOP system for concussion. This aligns with previous research describing high rates of ED use for injuries in younger children.27 Concussion is challenging to diagnose in infants and toddlers as they are often unable to reliably relay their symptoms to the clinician, which may make their parents more likely to seek ED care for more urgent evaluation and concern for more serious brain injuries. Others have noted that ED use can be influenced by parental understanding of the primary care clinician as a comprehensive source of care,28 parental anxiety during the relatively high-stress period of infancy,29 or misperceptions of illness/injury severity.30 Our findings suggest the need for specialized training for concussion diagnosis and/or development of special screening tools in EDs for this difficult-to-diagnose population. These assessments may need to be age modified as evidence suggests different symptom constellations among pediatric age groups.24 Enhancement of the triage process that occurs in most primary care settings via telephone nurse triage may be advantageous in reassuring parents that many instances of minor head trauma, even in the very young, can be appropriately managed by primary care. Future work might focus on delineation of concussion characteristics in this youngest age group aimed at providing the foundation for these interventions.
Patterns of health care entry point also varied by payor and race/ethnicity, a finding congruent with previous research related to pediatric injuries in general.27,31 Patients with Medicaid were disproportionately more likely to use the ED setting as an initial point of entry into the CHOP network for concussion, as were non-Hispanic black patients. This may be owing to the fact that specific state-level Medicaid provisions may direct the patient where they can seek care, or it may be owing to existing beliefs as to the appropriateness of the ED for injury care for particular demographic subgroups. This suggests that concussion epidemiology based on ED records may overestimate the incidence of concussion among these groups and underestimate the incidence among other groups.
There were several limitations of this study. First, inherent to the use of a single health care network’s EHR system as a data source is the fact that visits outside that network are not included. Some patients may have had a prior visit at a community ED or non-CHOP provider before seeking care at CHOP and, therefore, this analysis may not fully characterize the health care use of a well-defined underlying population. To explore the extent of this limitation, we conducted sensitivity analyses that limited the sample only to patients of primary care practices that were within 20 miles driving distance from the CHOP ED as these might be more likely to use the CHOP ED rather than another community ED. Despite being more likely to be minority and receiving Medicaid than the entire sample, 69% of these patients first sought care at their primary care office, reinforcing our primary findings. Previous analyses indicated that the CHOP primary care population is similar in key demographic variables to the Philadelphia metropolitan area32 and likely is representative of the general patient population in the Mid-Atlantic region. Second, this assessment did not take into account those who did not seek care for their concussion, either because they did not recognize or want to disclose their symptoms or because their family did not perceive their injury required medical care. As highlighted by the IOM, this “culture of resistance” is prevalent and, although not the focus of this analysis, is a significant societal issue in need of further study. Third, only the initial CHOP visit for the first concussion occurring during the study period was identified for each patient. Certainly, some proportion of patients experienced multiple concussions during the study period. Unfortunately, the EHR was not set up to systematically separate multiple concussions within a given patient’s record. To estimate the extent to which we underestimated the number of unique concussions, we selected 3% of concussion patients (n = 218) for manual medical record review; we randomly selected patients within strata based on the number of concussion visits and the length of time between the first and last visits; patients with more visits and a longer time between the first and last visits were more likely to be selected. Based on this review, we estimated that 16% of our patients (1289/8083) sought treatment for more than 1 concussion during the study period, indicating that we likely underestimated the true number of unique concussions by that percentage over the 4-year period. A more complete assessment of the patterns of health care use for the entire course of care, including subsequent concussions, is under way to complement the analyses contained herein. Last, it is important to note that these analyses were conducted on patients with a primary care clinician; the distribution of health care location initially used for concussion may be different in those without a primary care clinician.
Conclusions
In summary, using a novel method to leverage rich data captured in a unified EHR system on a diverse demographic and socioeconomic population, this study suggests that incidence estimates of pediatric concussion that rely solely on ED records substantially underestimate the true incidence of this injury. Most pediatric patients with concussion sought their initial concussion care within the CHOP network with a primary care clinician, illustrating the need to provide up-to-date training and clinical decision support tools to these clinicians. Important variations in the point of health care entry by age, race/ethnicity, and payor also suggest the accuracy of incidence estimates based on a single point of health care entry may vary for these different subgroups. These differences may lead to targeted interventions to improve recognition and management of concussion in these populations. In addition, the increased use of EHRs may provide an opportunity to leverage health records for research into the natural history of concussion that may lead to improvements in the prevention, diagnosis, and management of this common childhood injury.
Key Points.
Question
Across a broad health care network, where do children initially seek health care for concussion?
Findings
In this descriptive epidemiology study, 82% of patients sought initial care for concussion with primary care and only 12% within the emergency department. Younger children and those insured by Medicaid were more likely to use the emergency department as their initial point of health care entry.
Meaning
Efforts to measure the incidence of concussion cannot solely be based on emergency department visits, and primary care clinicians must be trained in concussion diagnosis and management.
Acknowledgments
Additional Contributions: We thank Ronni Kessler, MS, and Julia Vanni for their role in project coordination and Marianne Chilutti, MS, for her data management (The Children’s Hospital of Philadelphia). Ms Chilutti and Ms Kessler received compensation from a funding sponsor.
Funding/Support: This research was supported by an intergovernmental personnel act agreement between the US Department of Health and Human Services (HHS) Centers for Disease Control and Prevention (CDC) and The Children’s Hospital of Philadelphia.
Footnotes
Conflict of Interest Disclosures: None reported.
Role of the Funder/Sponsor: Beyond the coauthors, the CDC had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: This article does not reflect the official policy or opinions of the CDC or the US Department of HHS and does not constitute an endorsement of the individuals or their programs—by the CDC, HHS, or other components of the federal government—and none should be inferred.
Author Contributions: Drs Arbogast and Curry had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Arbogast, Curry, Zonfrillo, Haarbauer-Krupa, Breiding, Coronado, Master.
Acquisition, analysis, or interpretation of data: Arbogast, Curry, Pfeiffer, Haarbauer-Krupa, Coronado, Master.
Drafting of the manuscript: Arbogast, Curry, Pfeiffer, Master.
Critical revision of the manuscript for important intellectual content: Arbogast, Curry, Pfeiffer, Zonfrillo, Haarbauer-Krupa, Breiding, Coronado, Master.
Statistical analysis: Curry, Pfeiffer.
Obtained funding: Arbogast, Master.
Administrative, technical, or material support: Zonfrillo, Haarbauer-Krupa, Coronado, Master.
Study supervision: Arbogast, Curry, Master.
References
- 1.Institute of Medicine. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington, DC: Institute of Medicine and National Research Council of the National Academies; 2013. [PubMed] [Google Scholar]
- 2.Ransom DM, Vaughan CG, Pratson L, Sady MD, McGill CA, Gioia GA. Academic effects of concussion in children and adolescents. Pediatrics. 2015;135(6):1043–1050. doi: 10.1542/peds.2014-3434. [DOI] [PubMed] [Google Scholar]
- 3.Corwin DJ, Wiebe DJ, Zonfrillo MR, et al. Vestibular deficits following youth concussion. J Pediatr. 2015;166(5):1221–1225. doi: 10.1016/j.jpeds.2015.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Metzl JD. Concussion in the young athlete. Pediatrics. 2006;117(5):1813. doi: 10.1542/peds.2006-0480. [DOI] [PubMed] [Google Scholar]
- 5.Zonfrillo MR, Kim KH, Arbogast KB. Emergency department visits and neuroimaging for concussion patients from 2006–2011. Acad Emerg Med. 2015;22(7):872–877. doi: 10.1111/acem.12696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chrisman SP, Schiff MA, Chung SK, Herring SA, Rivara FP. Implementation of concussion legislation and extent of concussion education for athletes, parents, and coaches in Washington State. Am J Sports Med. 2014;42(5):1190–1196. doi: 10.1177/0363546513519073. [DOI] [PubMed] [Google Scholar]
- 7.Master CL, Balcer L, Collins M. In the clinic: concussion. Ann Intern Med. 2014;160(3):ITC2-1. doi: 10.7326/0003-4819-160-3-201402040-01002. [DOI] [PubMed] [Google Scholar]
- 8.Taylor AM, Nigrovic LE, Saillant ML, et al. Trends in ambulatory care for children with concussion and minor head injury from eastern Massachusetts between 2007 and 2013. J Pediatr. 2015;167(3):738–744. doi: 10.1016/j.jpeds.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 9.Zonfrillo MR, Master CL, Grady MF, Winston FK, Callahan JM, Arbogast KB. Pediatric providers’ self-reported knowledge, practices, and attitudes about concussion. Pediatrics. 2012;130(6):1120–1125. doi: 10.1542/peds.2012-1431. [DOI] [PubMed] [Google Scholar]
- 10.Kerr ZY, Dompier TP, Snook EM, et al. National Collegiate Athletic Association Injury Surveillance System: review of methods for 2004–2005 through 2013–2014 data collection. J Athl Train. 2014;49(4):552–560. doi: 10.4085/1062-6050-49.3.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Covassin T, Swanik CB, Sachs ML. Epidemiological considerations of concussions among intercollegiate athletes. Appl Neuropsychol. 2003;10(1):12–22. doi: 10.1207/S15324826AN1001_3. [DOI] [PubMed] [Google Scholar]
- 12.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 13.Mannix R, O’Brien MJ, Meehan WP., III The epidemiology of outpatient visits for minor head injury: 2005 to 2009. Neurosurgery. 2013;73(1):129–134. doi: 10.1227/01.neu.0000429846.14579.41. [DOI] [PubMed] [Google Scholar]
- 14.Kontos AP, Elbin RJ, Fazio-Sumrock VC, et al. Incidence of sports-related concussion among youth football players aged 8–12 years. J Pediatr. 2013;163(3):717–720. doi: 10.1016/j.jpeds.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 15.O’Kane JW, Schiff MA. Concerns about concussion rates in female youth soccer-reply. JAMA Pediatr. 2014;168(10):968. doi: 10.1001/jamapediatrics.2014.780. [DOI] [PubMed] [Google Scholar]
- 16.Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126(3):e550–e556. doi: 10.1542/peds.2009-3101. [DOI] [PubMed] [Google Scholar]
- 17.Meehan WP, III, Mannix R. Pediatric concussions in United States emergency departments in the years 2002 to 2006. J Pediatr. 2010;157(6):889–893. doi: 10.1016/j.jpeds.2010.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marin JR, Weaver MD, Yealy DM, Mannix RC. Trends in visits for traumatic brain injury to emergency departments in the United States. JAMA. 2014;311(18):1917–1919. doi: 10.1001/jama.2014.3979. [DOI] [PubMed] [Google Scholar]
- 19.Howard AF, Costich JF, Mattacola CG, Slavova S, Bush HM, Scutchfield FD. A statewide assessment of youth sports- and recreation-related injuries using emergency department administrative records. J Adolesc Health. 2014;55(5):627–632. doi: 10.1016/j.jadohealth.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 20.Stewart TC, Gilliland J, Fraser DD. An epidemiologic profile of pediatric concussions: identifying urban and rural differences. J Trauma Acute Care Surg. 2014;76(3):736–742. doi: 10.1097/TA.0b013e3182aafdf5. [DOI] [PubMed] [Google Scholar]
- 21.Gilchrist J, Thomas KE, Xu L, McGuire LC, Coronado V Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years: United States, 2001–2009. MMWR Morb Mortal Wkly Rep. 2011;60(39):1337–1342. [PubMed] [Google Scholar]
- 22.Dompier TP, Kerr ZY, Marshall SW, et al. Incidence of concussion during practice and games in youth, high school, and collegiate American football players. JAMA Pediatr. 2015;169(7):659–665. doi: 10.1001/jamapediatrics.2015.0210. [DOI] [PubMed] [Google Scholar]
- 23.Davis GA, Purcell LK. The evaluation and management of acute concussion differs in young children. Br J Sports Med. 2014;48(2):98–101. doi: 10.1136/bjsports-2012-092132. [DOI] [PubMed] [Google Scholar]
- 24.Sady MD, Vaughan CG, Gioia GA. Psychometric characteristics of the postconcussion symptom inventory in children and adolescents. Arch Clin Neuropsychol. 2014;29(4):348–363. doi: 10.1093/arclin/acu014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Macpherson A, Fridman L, Scolnik M, Corallo A, Guttmann A. A population-based study of paediatric emergency department and office visits for concussions from 2003 to 2010. Paediatr Child Health. 2014;19(10):543–546. doi: 10.1093/pch/19.10.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lott A, Zonfrillo MR, Wiebe DW, Arbogast KB, Grady MF, Master CL. Post-intervention study of concussion education and clinical support implementation with primary care providers. Poster presented at: Pediatric Academic Societies Annual Meeting; April 27, 2015; San Diego, California. [Google Scholar]
- 27.Alpern ER, Clark AE, Alessandrini EA, et al. Pediatric Emergency Care Applied Research Network (PECARN) Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med. 2014;21(4):365–373. doi: 10.1111/acem.12347. [DOI] [PubMed] [Google Scholar]
- 28.Romaire MA, Bell JF, Grossman DC. Health care use and expenditures associated with access to the medical home for children and youth. Med Care. 2012;50(3):262–269. doi: 10.1097/MLR.0b013e318244d345. [DOI] [PubMed] [Google Scholar]
- 29.Goldman SL, Owen MT. The impact of parental trait anxiety on the utilization of health care services in infancy: a prospective study. J Pediatr Psychol. 1994;19(3):369–381. doi: 10.1093/jpepsy/19.3.369. [DOI] [PubMed] [Google Scholar]
- 30.Fieldston ES, Alpern ER, Nadel FM, Shea JA, Alessandrini EA. A qualitative assessment of reasons for nonurgent visits to the emergency department: parent and health professional opinions. Pediatr Emerg Care. 2012;28(3):220–225. doi: 10.1097/PEC.0b013e318248b431. [DOI] [PubMed] [Google Scholar]
- 31.Owens PL, Zodet MW, Berdahl T, Dougherty D, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: focus on injury-related emergency department utilization and expenditures. Ambul Pediatr. 2008;8(4):219–240 e17. doi: 10.1016/j.ambp.2008.03.032. [DOI] [PubMed] [Google Scholar]
- 32.Feemster KA, Li Y, Grundmeier R, Localio AR, Metlay JP. Validation of a pediatric primary care network in a US metropolitan region as a community-based infectious disease surveillance system. Interdiscip Perspect Infect Dis. 2011;2011:219859. doi: 10.1155/2011/219859. [DOI] [PMC free article] [PubMed] [Google Scholar]