Abstract
Ipilimumab is an immunotherapeutic agent used in the treatment of metastatic melanoma, and is known to cause hypophysitis in some patients. Magnetic resonance imaging of ipilimumab-induced hypophysitis typically shows diffuse enlargement of the pituitary gland with variable enhancement or enlargement of the infundibulum. This often produces a diagnostic dilemma as melanoma not uncommonly metastasizes to the pituitary gland due to the rich vascular plexus of the hypophyseal portal system, and has a similar imaging appearance to autoimmune hypophysitis. We present a case of a 49-year-old man with a Clark level 4 melanoma of the left calf with inguinal nodal metastases that was treated with resection and 2 cycles of ipilimumab, and subsequently developed a “cystic” pituitary mass. To our knowledge, all of the described cases of ipilimumab-induced hypophysitis to date have shown solid enhancement on imaging. Because metastatic melanoma to the pituitary gland often has internal hemorrhage that produces a “cystic” appearance, and ipilimumab-induced hypophysitis is typically a solidly enhancing abnormality, this presented a significant diagnostic and therapeutic dilemma. Our patient's symptoms, although significant, did not necessitate immediate surgical intervention, and a conservative approach of withholding the ipilimumab and administering therapeutic corticosteroids was pursued. The patient's symptoms abated and follow-up magnetic resonance imaging 1 month later showed near complete resolution of the pituitary abnormalities. As such, this is a unique case of ipilimumab-induced hypophysitis presenting as a “cystic” pituitary mass.
Keywords: Hypophysitis, Ipilimumab, Pituitary mass, Pituitary inflammation
Case report
A 49-year-old man was found to have spitzoid-type Clark level 4 malignant melanoma of the posterior left calf with locally advanced, node-positive disease. He underwent wide local excision of the lesion with left inguinal sentinel lymph node biopsy and was started on ipilimumab immunotherapy. Three months after beginning the treatment, he presented to the emergency department with headache and nausea. Laboratory analysis showed several hormonal abnormalities, including depressed luteinizing hormone of 0.9 mIU/mL (normal, 1.7-8.6 mIU/mL), testosterone <3 ng/dL (normal, 348-1197 ng/dL), cortisol 1.71 mcg/dL (normal, 6.02-18.4 mcg/dL), and thyroid-stimulating hormone of 0.04 (normal, 0.27-4.20 mcU/mL).
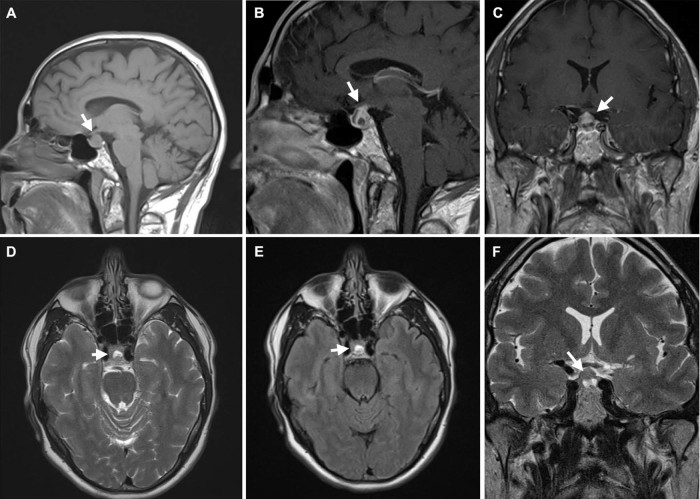
Magnetic resonance imaging (MRI) of the brain was performed and showed a solitary heterogeneously enhancing sellar mass (Fig. 1A). Within the sellar mass, a well-defined T2-hyperintense focus that did not completely suppress on fluid attenuation inversion recovery imaging (T2 FLAIR) (Fig. 1E), indicative of proteinaceous fluid, potentially subacute hematoma. The differential diagnosis for this lesion was a hemorrhagic melanoma metastasis versus an atypical “cystic” presentation of ipilimumab-induced hypophysitis.
Fig. 1.
Magnetic resonance imaging of the pituitary gland after 2 cycles of ipilimumab obtained in the setting of new headache. Sagittal T1 precontrast (A), sagittal T1 postcontrast (B), and coronal T1 postcontrast (C) images demonstrate a 1.5 cm heterogeneously enhancing mass filling the sella and extending into the suprasellar cistern and up the pituitary infundibulum to abut the undersurface of the midportion of the optic chiasm. Axial T2 (D), axial T2 fluid attenuation inversion recovery (E), and coronal T2 (F) images demonstrate a 7 mm pocket of fluid signal within the sellar portion of the mass, likely representing a small internal subacute hematoma versus other proteinaceous fluid.
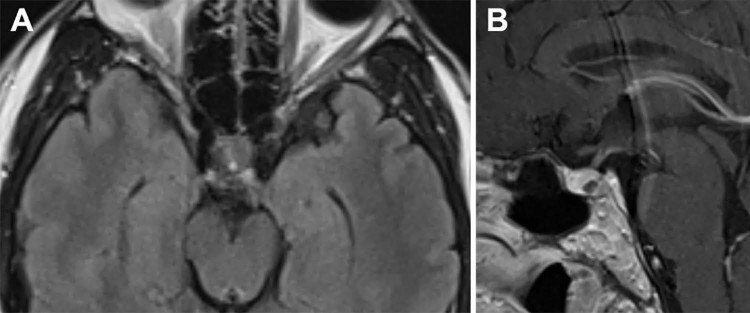
This diagnosis presented a therapeutic dilemma because surgical resection is typically the therapy for hemorrhagic pituitary metastasis causing acute symptoms; whereas, the treatment for ipilimumab-induced hypophysitis is to withdraw the medication and assess for regression of the hypophysitis. In this case, despite the atypical imaging features, a conservative approach was pursued, mainly because the patient's symptoms were not severe enough to necessitate urgent surgical intervention. The patient discontinued the ipilimumab, and underwent corticosteroid therapy to treat the potential ipilimumab-induced hypophysitis. His headaches resolved within a few days, and a repeat MRI one month later showed significant improvement, with only a small focus of residual abnormal T2 signal in the pituitary gland (Fig. 2A). The infiltrative and enlarged appearance of the pituitary had resolved (Fig. 2B).
Fig. 2.
One-month follow-up magnetic resonance imaging of the pituitary gland after the ipilimumab was given and corticosteroid therapy was initiated. Axial T2 fluid attenuation inversion recovery (A) and sagittal T1 postcontrast (B) images demonstrate resolution of sellar mass with only a small focus of residual T2 signal abnormality.
Discussion
Ipilimumab (Yervoy; Bristol-Myers Squibb, New York, NY) is a human monoclonal antibody that acts as a CTLA-4 receptor blocker, potentiating the cytotoxic T-cell response to tumor cells and increasing the propagation of T-cell populations. Although this mechanism does not specifically target any tumor marker unique to melanoma, T cell augmentation amplifies the patient's own immune response to the cancer cells [1]. In 2011, ipilimumab was fast-track FDA-approved for the treatment of metastatic melanoma due to its promising results in phase 3 experimental trials [2]. The drug demonstrated improved overall survival in patients with metastatic melanoma with a 1-year survival rate of 46% in those taking ipilimumab, versus 22-38% with the various other therapies available [3].
Hypophysitis has been well documented as a potential complication of ipilimumab in up to 11% of patients in 1 retrospective cohort [4]. The diagnosis can be challenging due to the wide range of potential imaging features, which include diffuse enlargement of the pituitary gland, enlargement of just the pituitary infundibulum, and variable enhancement patterns from focal and homogeneous to diffuse and heterogeneous [5], [6], [7].
To date, there are no reports of hypophysitis with cystic imaging features in patients taking ipilimumab. The cystic appearance makes the differentiation of hypophysitis from metastatic disease more difficult because internal hemorrhage is reasonably common in melanoma metastatic to the pituitary gland. In our patient, the symptoms were not severe enough to necessitate immediate surgical intervention, and the reasonable possibility of an atypical presentation of ipilimumab-induced hypophysitis warranted a conservative approach. Once the ipilimumab was discontinued and corticosteroids were administered, the pituitary lesion resolved, and the diagnosis of an atypical presentation of ipilimumab-induced hypophysitic with “cystic” features was confirmed.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Robert C., Ghiringhelli F. What is the role of cytotoxic T lymphocyte – associated antigen 4 blockade in patients with metastatic melanoma? Oncologist. 2009;14:848–861. doi: 10.1634/theoncologist.2009-0028. [DOI] [PubMed] [Google Scholar]
- 2.FDA FY 2011 innovative drug approvals. http://www.biopreneur.org/images/FY%202011%20Innovative%20Drug%20Approvals.pdf
- 3.Hodi F.S., O'Day S.J., McDermott D.F., Weber R.W., Sosman J.A., Haanen J.B. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faje A.T., Sullivan R., Lawrence D., Tritos N.A., Fadden R., Klibanski A. Ipilimumab-induced hypophysitis: a detailed longitudinal analysis in a large cohort of patients with metastatic melanoma. J Clin Endocrinol Metab. 2014;99:4078–4085. doi: 10.1210/jc.2014-2306. [DOI] [PubMed] [Google Scholar]
- 5.Rodrigues B.T., Otty Z., Sangla K., Shenoy V.V. Ipilimumab-induced autoimmune hypophysitis: a differential for sellar mass lesions. Endocrinol Diabetes Metab Case Rep. 2014;2014:140098. doi: 10.1530/EDM-14-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carpenter K.J., Murtagh R.D., Lilienfeld H., Weber J., Murtagh F.R. Ipilimumab-induced hypophysitis: MR imaging findings. AJNR Am J Neuroradiol. 2009;30:1751–1753. doi: 10.3174/ajnr.A1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bronstein Y., Ng C.S., Hwu P., Hwu W.-J. Radiologic manifestations of immune- related adverse events in patients with metastatic melanoma undergoing anti–CTLA-4 Antibody therapy. AJR Am J Roentgenol. 2011;197:W992–1000. doi: 10.2214/AJR.10.6198. [DOI] [PubMed] [Google Scholar]