Abstract
Background
Cough is a common symptom experienced by athletes, particularly after exercise. We performed a systematic review to assess the following in this population: (1) the main causes of acute and recurrent cough, either exercise-induced or not, (2) how cough is assessed, and (3) how cough is treated in this population. From the systematic review, suggestions for management were developed.
Methods
This review was performed according to the CHEST methodological guidelines and Grading of Recommendations Assessment, Development and Evaluation framework until April 2015. To be included, studies had to meet the following criteria: participants had to be athletes and adults and adolescents aged ≥ 12 years and had to complain of cough, regardless of its duration or relationship to exercise. The Expert Cough Panel based their suggestions on the data extracted from the review and final grading by consensus according to a Delphi process.
Results
Only 60 reports fulfilled the inclusion criteria, and the results of our analysis revealed only low-quality evidence on the causes of cough and how to assess and treat cough specifically in athletes. Although there was no formal evaluation of causes of cough in the athletic population, the most common causes reported were asthma, exercise-induced bronchoconstriction, respiratory tract infection (RTI), upper airway cough syndrome (UACS) (mostly from rhinitis), and environmental exposures. Cough was also reported to be related to exercise-induced vocal cord dysfunction among a variety of less common causes. Although gastroesophageal reflux disease (GERD) is frequent in athletes, we found no publication on cough and GERD in this population. Assessment of the causes of cough was performed mainly with bronchoprovocation tests and suspected disease-specific investigations. The evidence to guide treatment of cough in the athlete was weak or nonexistent, depending on the cause. As data on cough in athletes were hidden in a set of other data (respiratory symptoms), evidence tables were difficult to produce and were done only for cough treatment in athletes.
Conclusions
The causes of cough in the athlete appear to differ slightly from those in the general population. It is often associated with environmental exposures related to the sport training environment and occurs predominantly following intense exercise. Clinical history and specific investigations should allow identification of the cause of cough as well as targeting of the treatment. Until management studies have been performed in the athlete, current guidelines that exist for the general population should be applied for the evaluation and treatment of cough in the athlete, taking into account specific training context and anti-doping regulations.
Key Words: athletes, cough, evidence-based medicine, exercise, guidelines, sports
Abbreviations: DRO, Drug Reference Online; EIB, exercise-induced bronchoconstriction; EIVCD, exercise-induced vocal cord dysfunction; GERD, gastroesophageal reflux disease; RTI, respiratory tract infection; UACS, upper airway cough syndrome; WADA, World Anti-Doping Agency
Summary of Suggestions
1. In adult and adolescent athletes (≥ 12 years of age) complaining of acute or recurrent cough, we suggest to initially evaluate for the most commonly reported causes of cough in this group such as asthma, exercise-induced bronchoconstriction (EIB), respiratory tract infections (RTIs), upper airway cough syndrome (UACS) due to rhinosinus conditions, and environmental exposures related to the sport training environments (Ungraded, Consensus Based).
2. In adult and adolescent athletes (≥ 12 years of age) complaining of acute or recurrent cough, we suggest that pulmonary function tests, particularly bronchoprovocation challenges, and assessment of allergy to common airborne allergens be performed in the investigation of cough to identify common etiologies such as asthma and EIB, and to evaluate the effects of environmental exposures such as allergens, respiratory irritants, and pollutants (Grade 2B).
3. In adult and adolescent athletes (≥ 12 years of age) complaining of acute or recurrent cough, we suggest to proceed with a systematic investigation based on suspected cause(s) from initial clinical assessment, with specific attention to the athlete’s particular sport and training environment and context (exercise related or not) in which cough occurs, to determine its etiology (Ungraded, Consensus Based).
4. In adult and adolescent athletes (≥ 12 years of age) complaining of cough, we suggest a treatment trial directed at the suspected causes of cough similarly to the general population, but taking into account the sport performed and training environment. The anti-doping regulations and potential side effects of medications that could interfere with training performances should be reviewed and considered when appropriate (Ungraded, Consensus Based).
Remarks: Anti-doping regulations are provided by the World Anti-Doping Agency (WADA) (https://www.wada-ama.org). The World Anti-Doping Code is a document that brings consistency to anti-doping rules, regulations, and policies worldwide. It is updated annually and the Prohibited List identifies the substances and methods prohibited to athletes in and out of competition. The Global Drug Reference Online (Global DRO) provides athletes and support personnel with information about the prohibited status of specific substances based on the current WADA Prohibited List. The Global DRO provides specific information on products sold in the United Kingdom, Canada, and the United States. The Global DRO is created through a partnership between UK Sport, the Canadian Centre for Ethics in Sport, and the US Anti-Doping Agency (http://www.globaldro.com).
5. In adult and adolescent athletes (≥ 12 years of age) complaining of acute and recurrent cough, we suggest that investigators perform randomized control trials to assess the effects of disease-specific and/or environment-specific (eg, cold-air-induced cough) treatments on cough because there are minimal data on how to optimally treat cough in these groups (Ungraded, Consensus Based).
Cough is a symptom frequently reported by athletes and even more so in those involved in endurance sports.1, 2, 3, 4, 5, 6, 7, 8, 9 Conditions known to be responsible for cough in the general population may also be responsible for cough in athletes.10, 11, 12 However, in this population, cough may also be associated with the inherent characteristics of specific sports and their training environments. For example, exercise-induced cough is particularly prevalent in swimmers and winter-sports athletes.13, 14 In winter athletes, cough following exercise was more frequently reported during winter (71%) than during summer (44%).9 Regarding other sports, a prevalence of exercise-induced cough was reported in 14% of football players.15 In addition, the large ventilatory volumes required by intense exercise may increase lung penetration of allergens or pollutants and cause airway dehydration.10, 12, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25 Airway rewarming may also possibly modulate airway responses.
As part of the global effort of the American College of Chest Physicians (CHEST) to develop guidelines for the management of cough, it was decided to fill a gap in the literature by developing a clinical practice guideline on how to assess and treat cough in athletes. To do so, we performed a systematic review of the available publications on this topic to search for evidence to make specific recommendations or suggestions about identification of the cause of cough as well as the assessment and treatment of cough in this population. It was suggested that evaluation and management of cough in athletes should take into account many specific characteristics and special considerations for athletes, such as daily training, training environment, doping regulations, and frequent traveling. As each cause of cough might have a specific treatment, accurate diagnosis is essential to avoid using unnecessary medication.
Methods
Search Strategy
Systematic review of the literature was performed. Studies published in PubMed, Scopus, and the Cochrane Library were identified using the following search terms: (cough OR exercise induced asthma OR rhinitis OR sinusitis OR laryngitis OR GERD OR gastro-esophageal reflux OR gastroesophageal reflux OR “chronic eosinophilic bronchitis” OR bronchoconstriction OR “environmental exposures” OR “vocal cord” OR “upper airway diseases” OR allergies) AND (athlete OR athletes OR skiers OR skiing OR swimmers OR swimming OR runners OR rowing OR marathon OR Olympic OR “competitive sports”) were identified. The search was limited to articles in French and English; it began with the initiation of these databases and ended in April 2015.
Study Selection
Being aware that there were only a few clinical trials on cough in the athlete, we included all types of study designs in our list of articles to review. References of included studies were searched to identify additional relevant publications. The study characteristics and inclusion/exclusion criteria were selected from the patient problem or population, intervention, comparison, and outcome (PICO) elements for all key clinical questions26 (Table 1). To be included, studies had to meet the following criteria: subjects were described as athletes, adults and adolescents aged ≥ 12 years who complained of acute or recurrent cough, regardless of the duration and relationship to exercise. A subject was considered an athlete if he/she participated in an organized team or individual sport and took part in regular sport competitions against other athletes. Ideally, the sport had to require some form of systematic and usually intense training, regardless of the level of competition or number of training hours.27
Table 1.
Cough in Athletes PICO Questions: In Adult and Adolescent Athletes 12 Years of Age or Older, (1) What Are the Main Causes of Recurrent or Acute Cough? (2) How Is Acute or Recurrent Cough Usually Evaluated? (3) How Should Recurrent and Acute Cough Be Treated?
| Category | Inclusion Requirements | No | Yes |
|---|---|---|---|
| Study design | Is the article an evaluation study that uses one of the following designs?
|
Exclude | Continue |
| Populations | Does the article report on patient groups that have all of the following characteristics?
|
Exclude | Continue |
| Intervention | Does the article report on the causes of cough, the results of diagnostic evaluation for cough, and the treatments of cough? | Exclude | Continue |
| Outcomes | Does the article report on:
|
Exclude | Continue |
Data Extraction and Quality Assessment
Two authors (L-P. B. and J. T.) independently analyzed the titles and content of the abstracts recovered to assess inclusion criteria. From the selected titles and abstracts, full reports about potentially relevant studies were obtained, and the authors independently assessed eligibility of the studies. Disagreements were discussed and resolved by consensus. A third author, R. S. I., was available to help resolve disagreements if necessary.
For randomized controlled trials, the reviewers independently assessed the risk of bias criteria using criteria in the Cochrane Reviews. The criteria used were random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias) to the study protocol, blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), and selective reporting (reporting bias).28 Quality assessment of observational studies was also performed.29
Guideline Framework
Grading of recommendations/suggestions was made according to the Grading of Recommendations Assessment, Development and Evaluation framework as adopted by CHEST.30 This framework separates the process of rating the quality of evidence from that of determining the strength of the recommendation. The quality of evidence was based on risk of bias, inconsistency, indirectness, reporting bias, and imprecision.31 The quality of evidence (ie, the confidence in estimates) was rated as high (A), moderate (B), and low or very low (C). The strength of recommendation was determined based on the quality of evidence and the balance of benefits and harms, patients’ values and preferences, and availability of resources.32 Level 1 represented strong recommendations in which benefits or harms clearly outweighed the other. Level 2 represented a weak recommendation in which it was not clear that the benefits outweighed the harms (or vice versa), and new research could change the direction or strength of these recommendations.
Developing Recommendations/Suggestions
To be included in this guideline, a recommendation or suggestion had to be voted on by 75% of the eligible members of the entire Cough Expert Panel and achieve ratings of “strongly agree” or “agree” by 80% of the voting panelists. No cough panel member was excluded from voting.
Results
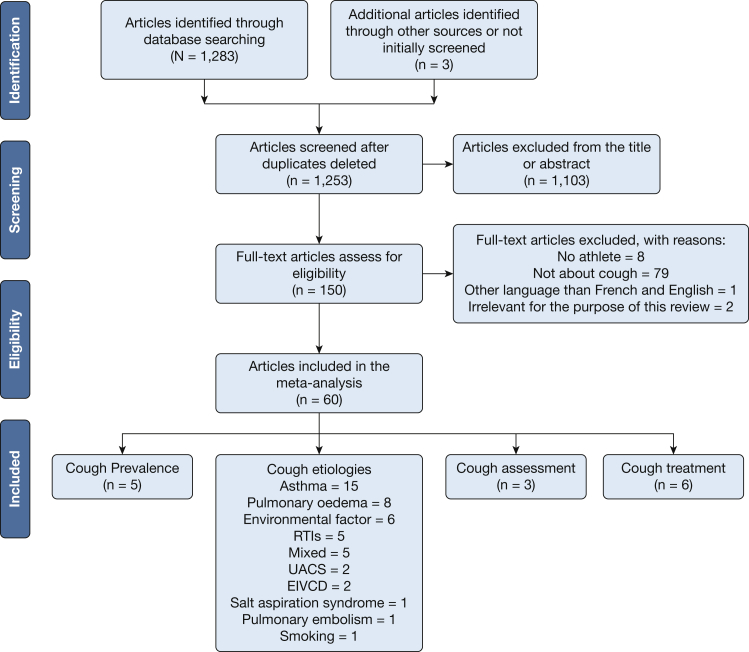
Of 1,283 references identified by our search string and screened, 60 articles were included in the analysis. The process of study selection is outlined in Figure 1. Five articles reported cough prevalence, 46 articles reported causes of cough, three papers discussed cough assessment, and six papers were on the treatment of respiratory symptoms in athletes. Although there were five randomized clinical trials on the treatment of respiratory symptoms in athletes, only one specifically assessed cough. Although the systematic review revealed many records of causes of cough in athletes, very few specifically addressed how to evaluate or treat cough in the athlete. As data on cough in athletes were often hidden in a set of other data (respiratory symptoms), evidence tables were difficult to produce and were done only for cough treatment in athletes. In general, the studies were randomized placebo-controlled, double-blind trials, and four of six were considered to be at low risk of bias.
Figure 1.
Preferred Reporting Items for Systematic Reviews flow diagram for the study selection. EIVCD = exercise-induced vocal cord dysfunction; RTIs = respiratory tract infections; UACS = upper airway cough syndrome.
Key Clinical Question 1: In adult and adolescent athletes 12 years of age or older, what are the main causes of recurrent or acute cough?
Causes of Cough
Although there has been no formal study on the comparative prevalence of causes of cough in athletes, cough in the athlete was mainly associated with asthma and EIB in 15 reports.1, 7, 8, 11, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43 Other associations were reported with airway dehydration and environmental exposures in six studies,21, 22, 23, 24, 44, 45 RTIs in five studies,46, 47, 48, 49, 50 UACS due to rhinosinus conditions in two studies,13, 51 and exercise-induced vocal cord dysfunction (EIVCD) in two studies.52, 53 Although it is very common in athletes, we found no study on the effects of GERD on cough in this population. Eleven manuscripts reported less common causes of cough: exercise-induced pulmonary edema including nonimmersion sports in two publications,20, 54 immersion sports in five studies,55, 56, 57, 58, 59 high-altitude pulmonary edema in one publication,60 as well as pulmonary embolism in one report,61 salt water aspiration syndrome in one study,62 and passive smoking in one case.63 No publication was found on heart conditions that induced cough in athletes.
Practice Recommendations/Suggestions
1. In adult and adolescent athletes (≥ 12 years of age) complaining of acute or recurrent cough, we suggest to initially evaluate for the most commonly reported causes of cough in this group such as asthma, exercise-induced bronchoconstriction (EIB), respiratory tract infections (RTIs), upper airway cough syndrome (UACS) due to rhinosinus conditions, and environmental exposures related to the sport training environments (Ungraded, Consensus Based).
Key Clinical Question 2: In adult and adolescent athletes (≥ 12 years of age), how is acute or recurrent cough usually evaluated?
Assessment of Cough
Although there were no systematic evaluations of cough specifically proposed for athletes, the publications suggested that a search for causes of cough in athletes should take into account the history and temporal relationships between cough and exercise, its sudden onset or recurrence, and the training environment.
One study evaluated the seasonal variability of cough reflex sensitivity to capsaicin in winter athletes.9 The prevalence of cough within 1 hour after exercise was higher in athletes compared with nonathletes, and cough was reported more frequently during winter in athletes. However, cough was not associated with cough reflex hypersensitivity to capsaicin, bronchoconstriction, or airway inflammation.9
Although the Allergy Questionnaire for Athletes64 can be used as a predictor of allergy in athletes,65 self-reported respiratory symptom questionnaires have not been shown to be reliable predictors for the diagnosis of exercise-induced asthma and airway hyperresponsiveness.5, 6, 66
Practice Recommendations/Suggestions
2. In adult and adolescent athletes (≥ 12 years of age) complaining of acute or recurrent cough, we suggest that pulmonary function tests, particularly bronchoprovocation challenges, and assessment of allergy to common airborne allergens be performed in the investigation of cough to identify common etiologies such as asthma and EIB, and to evaluate the effects of environmental exposures such as allergens, respiratory irritants, and pollutants (Grade 2B).
3. In adult and adolescent athletes (≥ 12 years of age) complaining of acute or recurrent cough, we suggest to proceed with a systematic investigation based on suspected cause(s) from initial clinical assessment, with specific attention to the athlete’s particular sport and training environment and context (exercise related or not) in which cough occurs, to determine its etiology (Ungraded, Consensus Based).
Key Clinical Question 3: In adult and adolescent athletes (≥ 12 years of age), how should recurrent and acute cough be treated?
Treatment of Cough
There were only six studies looking at the effect of treatments on cough in the athlete (Table 2). Usually, treatment targeted the suspected or confirmed causes, but the effects of therapy were usually noted for the whole spectrum of respiratory symptoms and not only cough, or they were not specifically reported for cough. In these six studies, the effects of different treatments on respiratory symptoms were evaluated in 201 athletes, mostly young men (mean age, 20 years; 84% men). Medications assessed included ipratropium,67 albuterol,68 ciclesonide,69 montelukast,70 and budesonide.71 Compared with placebo, these drugs had modest or no effects on exercise-induced respiratory symptoms, including cough. Only a subgroup of cross-country skiers experienced a decrease in cough frequency and perception of cough intensity following exercise with pretreatment with 80 mg of inhaled ipratropium.67 Finally, in a randomized double-blind, placebo-controlled clinical trial, a daily supplement of 600 mg of vitamin C for 21 days was reported to lead to a reduction in the duration and incidence of symptoms of upper RTIs, including cough, before and following a 90-km run.72
Table 2.
Studies That Evaluated the Effect of Different Treatments on Respiratory Symptoms in Athletes
| Author/Year | Study Design | Symptoms Assessed | Patients | No. of Patients | Age (y) | Sex (M/F) | Control Group (Nonathlete) | Intervention | Outcomes | Efficacy | WADA status | Quality of the evidence |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bordeleau et al67/2014 | RCT | Cough, breathlessness, sputum, chest tightness, wheezing | Cross-country skiers who reported exercise-induced respiratory symptoms | 22 | 17 ± 3 | 10/12 | No | Ipratropium (80 mg) vs placebo before cross-country skiing (3 min sprint preceded by 30-min warm-up) | Number of cough (the number of coughs following exercise was recorded for 1 hour with microphone headsets), Borg score for symptom intensity and bronchoconstriction (FEV1) | No influence on the post-exercise maximal fall in FEV1, the frequency of cough following exercise and the perception of cough intensity. However, a subgroup of athletes seems to show beneficial response to ipratropium (decrease in number of cough). | Permitted | Moderate |
| Gong et al68/1988 | RCT | Cough, sputum, substernal soreness, shortness of breath, wheezing, chest tightness, sore throat, nasal discharge | Endurance cyclists and triathletes without active asthma or the use of bronchodilators or other medication | 15 | 23 ± 5 | 14/1 | No | Albuterol (180 mg) vs placebo, ozone exposure (0.21 ppm) or filtered air during ergocycle (40-km time trial, preceded by warm-up) in an environmental chamber | Ozone exercise-induced symptoms, bronchoconstriction (FEV1, FVC, FEF25-75%), impairment of exercise performance (Ve, Vo2, RR, HR), and airways reactivity to inhaled histamine | The pre-treatment with albuterol did not significantly block or attenuate the effects of 0.21 ppm O3 on symptoms, exercise performance, lung function, and airways reactivity to histamine. | Permitted | Moderate |
| Peters et al72/1993 | RCT | Common cold symptoms (runny nose, sneezing, sore throat, cough, and fever) | Runners (90-km race) and nonathletic subjects who were not regular runners | Athletes = 84 Control subjects = 73 |
5 < 25 y; 57 ≥ 25 y and < 40y; 22 ≥ 40 y (athletes) |
82/2 (athletes) | Yes Similar age, not regular runners |
21 days before the race 600 mg of vitamin C daily (runners = 43; control group = 34) vs placebo containing citric acid (runners = 41, control group = 39) | The incidence of post-race URT symptoms during post-race period | The duration of the symptoms was shorter in the vitamin C supplemented runners and their matched control subjects, decreased incidence of symptoms of URT before and for 3-wk post-race (running nose, sneezing, sore throat, cough, and fever), but the duration and the severity were less in control group receiving Vitamin C. | Permitted | Moderate |
| Koya et al69/2009 | Retrospective review | Respiratory symptoms at rest and on exercise | Regional athletes; junior and high-school students with asthma | 39 | 18 | 28/11 | No | Ciclesonide (200 or 400 μg/d) vs montelukast (10 mg/d) Duration of treatment: Ciclesonide (5.2 mo) Montelukast (5.6 mo) |
The rate of improvement of the symptoms at rest and during exercise in accordance with the global assessment of efficacy, rate of change of therapy, pulmonary function test parameters, and Feno values | Better symptom control and fewer changes of therapy in the Ciclesonide group, but not statistically significant. Significant improvement in %FVC, %FEV1 and %MMF in the Ciclesonide group in comparison with baseline values. Significant decrease of Feno values in the Ciclesonide group in comparison with baseline values. |
Permitted | Low |
| Helenius et al70/2004 | RCT | Asthma-like symptoms (wheeze, cough, shortness of breath) | Ice hockey players from the Finnish Junior National League who reported at least 2 exercise-induced bronchial symptoms | 16 | 18 ± 1 | 16/0 | No | 4 wk of montelukast 10 mg, 1 wk washout, and 4 wk placebo | The effect of montelukast on asthma-like symptoms, bronchial and responsiveness and on indices of airway inflammation Daily diary on exercise-induced asthma-like symptoms (scale 0-10) |
No difference between placebo and Montelukast in weekly or monthly scores for exercise-induced symptoms, especially cough. Montelukast had no effect on lung function or indices of airway inflammation in symptomatic ice hockey players has compared with placebo. |
Permitted | Moderate |
| Sue-Chu et al71/2000 | RCT | Asthma-like symptoms (wheeze, abnormal breathlessness, chest tightness) | Elite competitive cross-country skiers with 2 or more asthma-like symptoms on exertion, at rest, or on exposure to irritants |
25 | 18 (16-20) | 19/6 | No | Inhaled budesonide 400 μg twice daily vs placebo Duration of treatment: budesonide (22.3 wk) placebo (22.8 wk) |
The effect of budesonide during the competitive season on indices of inflammation in the bronchial mucosa and BAL fluid and on tenascin immunoreactivity in the reticular basement membrane |
No difference between placebo and budesonide on airway inflammation, tenascin expression or clinical manifestations. Asthma-like symptoms were unchanged in 17 (68%) skiers. |
Permitted | Moderate |
FEF25-75% = forced expiratory flow in the midexpiratory phase; Feno = fractional exhaled nitric oxide; HR = heart rate; MMF = maximum mid-expiratory flow; O3 = ozone; RCT = randomized controlled trial; RR = respiratory rate; URT = upper respiratory tract; e = ventilation (L/min); o2 = oxygen consumption; WADA = World Anti-Doping Agency.
Practice Recommendations/Suggestions
4. In adult and adolescent athletes (≥ 12 years of age) complaining of cough, we suggest a treatment trial directed at the suspected causes of cough similarly to the general population, but taking into account the sport performed and training environment. The anti-doping regulations and potential side effects of medications that could interfere with training performances should be reviewed and considered when appropriate (Ungraded, Consensus Based).
Remarks: Anti-doping regulations are provided by WADA. The World Anti-Doping Code is a document that brings consistency to anti-doping rules, regulations, and policies worldwide. It is updated annually and the Prohibited List identifies the substances and methods prohibited to athletes in and out of competition (see Table 3).
Table 3.
Current Anti-Doping Status of Common Drugs Used for Cough in Different Conditions
| Causes of Cough | Drug | WADA Status |
|---|---|---|
| Asthma | Inhaled β2-agonists | |
| Salbutamol | Permitteda | |
| Formoterol | Permitteda | |
| Terbutaline | Prohibited | |
| Inhaled anticholinergic agents | Permitted | |
| Inhaled corticosteroids | Permitted | |
| Leukotriene antagonists | Permitted | |
| Oral corticosteroids | Prohibitedb | |
| RTIs | Antibiotics | Permitted |
| First-generation antihistamines with or without oral decongestant | Permittedc | |
| Nasal ipratropium | Permitted | |
| Nasal corticosteroids | Permitted | |
| Codeine (short-term use) | Permitted | |
| Dextromethorphan | Permitted | |
| UACS | Nasal corticosteroids | Permitted |
| First-generation antihistamines with or without oral decongestant | Permittedc | |
| Second-generation antihistamines (nonsedative) | Permittedc | |
| Nasal ipratropium | Permitted | |
| Topical decongestants (eg, xylometazoline, phenylephrine) | Permitted | |
| EIVCD | Proton pump inhibitors | Permitted |
It is essential always to check that the drugs that have been prescribed are permitted by the World Anti-Doping Agency on the site Global DRO at http://www.globaldro.com.
Prohibited drugs can be used by athletes only if a Therapeutic Use Exemption (TUE) is granted in accordance with the International Standards on TUE. The athlete should, however, list all medication used on the doping control form.
RTIs = respiratory tract infections; WADA = World Anti-Doping Agency. See Table 3 legend for expansion of other abbreviations.
The use of this drug is conditional; maximum daily doses of salbutamol and formoterol permitted are 1,600 and 54 μg/d, respectively. A urinary concentration of salbutamol > 1,000 ng/mL or of formoterol > 40 ng/mL is considered by the WADA to be an adverse analytic finding unless the athlete proves the drug was used therapeutically. There will be a presumption that the substance was not taken by inhalation therapeutically, and the athlete will have the burden of demonstrating by means of a controlled pharmacokinetic study that the level found in the athlete’s urine sample was the result of therapeutic inhaled use.
These drugs are prohibited during competition only.
The use of pseudoephedrine in competition is conditional; a maximum daily dose of 240 mg/d is permitted. The urinary concentration of pseudoephedrine should not be > 150 μg/mL. Athletes must stop taking pseudoephedrine at least 24 hours before competition.
The Global DRO provides athletes and support personnel with information about the prohibited status of specific substances based on the current WADA Prohibited List. The Global DRO provides specific information on products sold in the United Kingdom, Canada, and the United States. The Global DRO is created through a partnership between UK Sport, the Canadian Centre for Ethics in Sport, and the US Anti-Doping Agency.
5. In adult and adolescent athletes (≥ 12 years of age) complaining of acute and recurrent cough, we suggest that investigators perform randomized control trials to assess the effects of disease-specific and/or environment-specific (eg, cold-air-induced cough) treatments on cough because there are minimal data on how to optimally treat cough in these groups (Ungraded, Consensus Based).
Discussion
There is a lack of evidence on the optimal management of cough in the athlete. Although we were able to find some observations about the main causes of cough in this population, there has been no systematic approach to its evaluation. Moreover, some causes of cough were not addressed in the publications screened. For example, despite its high prevalence in endurance athletes, ranging between 30% and 70%, no report looked at GERD and cough in this population.73, 74, 75 As GERD is indeed recognized to be a frequent cause of cough in the general population,76 there is a need to look at this potential cause of cough in the athlete.
As asthma, EIB, and environmental exposure were the most common conditions associated with persistent cough, we suggest that pulmonary function tests, particularly bronchoprovocation challenges, and assessment of allergy to common airborne allergens should be considered in the investigation of cough in athletes. Investigation should, however, be guided by the probable cause of cough as determined by the initial clinical assessment (see Table 4).
Table 4.
Common Causes of Cough According to Sport Training Environment
| Sport Training Environment | Sport | Possible Stimuli | Causes of Cough |
|---|---|---|---|
| Outdoor winter sports | Cross-country skiing, biathlon, speed skating | Cold and dry air | Asthma, UACS, EIVCD |
| Indoor ice rink | Speed skating, figure skating, hockey | Nitrogen dioxide, other indoor pollutants | Asthma, UACS |
| Indoor pool | Swimming, water polo, diving, synchronized swimming | Chlorine derivatives | Asthma, UACS |
| Outdoor sports | Cycling, running | Ozone, sulfur dioxide, nitrogen dioxide, aeroallergens | Asthma, UACS, EIVCD |
| Indoor gymnasium | Track and field, combat sports | Aeroallergens | Asthma, UACS |
| Sea and lake | Open water swimming, triathlon, scuba diving | Immersion, cold, salt water | Pulmonary edema |
| Mountains, high altitude | Skiing, hiking | Cold, hypoxemia | Pulmonary edema |
EIVCD = exercise-induced vocal cord dysfunction; UACS = upper airway cough syndrome.
Strengths and Limitations
Even though cough is a very commonly reported respiratory symptom in athletes, our analysis of the literature stresses the paucity of data on cough in the athlete. The strengths of this analysis include the extensive review of > 1,200 publications obtained according to the key words selected, the methodology used to perform the analysis, and its review by the CHEST Expert Cough Panel.
Its limitations are associated with the lack of high-quality studies, the variable definition of an athlete among reports (resulting in a relatively heterogeneous group of athletes), the lack of specific analysis of cough among other types of respiratory symptoms, and the variable outcomes chosen to assess cough response to treatment. In addition, the number of patients enrolled in the studies was small.
Future Research
Many gaps in knowledge need to be addressed regarding cough in the athlete. They include the following:
-
•
Determination of the prevalence of specific causes of cough in athletes according to the type of sport
-
•
Evaluation of the mechanisms underlying exercise-induced cough in athletes
-
•
Documenting the incidence of cough in exercise and bronchoprovocation challenges
-
•
Determination of the optimal way to assess cough in the athlete
-
•
Determination of the role of GERD as a cause of cough in the athlete
-
•
Performance of randomized controlled trials to assess the effects of current treatment options for cough in the athlete in the presence or absence of an identifiable pathologic condition
-
•
Performance of well-designed, high-quality studies to determine the benefits of therapies when specific causes of cough have been identified in the athlete, also taking into account the type of sport and environmental exposures
Conclusions
Cough appears to be a common symptom in the athlete, is often related to environmental exposures during training, and occurs predominantly following intense exercise. Clinical history and specific investigations should allow identification of the cause of cough and targeting of treatment. Because there is a lack of evidence about how to best investigate and manage cough in the athlete, current guidelines produced for the general population should be applied in the athlete, taking into account the training-specific context and anti-doping regulations.
Acknowledgments
Author Contributions: L-P. B. is the guarantor of the paper. L-P. B. and J. T. selected the studies and performed the data extraction and systematic analysis and drafted the manuscript. R. S. I. initiated and supervised the project and participated in writing and reviewing the manuscript.
Financial/nonfinancial disclosures: L-P. B. has received nonprofit grants for research funding provided to the Institut universitaire de cardiologie et de pneumologie de Québec for participating in multicenter studies from Altair, Amgen, Asmacure, AstraZeneca, Boehringer Ingelheim, Boston Scientific, Genentech, GlaxoSmithKline, Novartis, Ono Pharma, Sanofi, and Wyeth and support for investigator-generated studies from Takeda, Merck, and Boehringer Ingelheim; has served on consulting/advisory boards for Astra Zeneca and Novartis; has received nonprofit grants for production of educational materials from AstraZeneca, GlaxoSmithKline, Merck Frosst, Boehringer Ingelheim, and Novartis; has received lecture fees from AstraZeneca, GlaxoSmithKline, Merck, and Novartis; has received travel sponsorship to meetings for presentation of studies and for committees from Novartis and Takeda. Although R. S. I. is the Editor in Chief of CHEST, the review and all editorial decisions regarding this manuscript were made independently by others. None declared (J. T., R. S. I.).
Collaborators: Kenneth W. Altman, MD, PhD (Baylor College of Medicine, Houston, TX), Alan F. Barker, MD (Oregon Health & Science University, Portland, OR), Surinder S. Birring, MB ChB, MD (Division of Asthma, Allergy and Lung Biology, King’s College London, London, UK), Fiona Blackhall, MD, PhD (University of Manchester, Department of Medical Oncology, Manchester, England), Donald C. Bolser, PhD (College of Veterinary Medicine, University of Florida, Gainesville, FL), Louis-Philippe Boulet, MD, FCCP (Institut universitaire de cardiologie et de pneumologie de Québec, Quebec, QC, Canada), Sidney S. Braman, MD, FCCP (Mount Sinai Hospital, New York, NY), Christopher Brightling, MBBS, PhD, FCCP (University of Leicester, Glenfield Hospital, Leicester, UK), Priscilla Callahan-Lyon, MD (Adamstown, MD), Anne B. Chang, MBBS, PhD, MPH (Royal Children’s Hospital, Queensland, Australia), Terrie Cowley (The TMJ Association, Milwaukee, WI), Paul Davenport, PhD (Department of Physiological Sciences, University of Florida, Gainesville, FL), Satoru Ebihara, MD, PhD (Department of Rehabilitation Medicine, Toho University School of Medicine, Tokyo, Japan), Ali A. El Solh, MD, MPH (University at Buffalo, State University of New York, Buffalo, NY), Patricio Escalante, MD, MSc, FCCP (Mayo Clinic, Rochester, MN), Anthony Feinstein, MPhil, PhD (Sunnybrook Health Sciences Centre, Toronto, ON, Canada), Stephen K. Field, MD (University of Calgary, Calgary, AB, Canada), Dina Fisher, MD, MSc (Department of Respiratory Medicine, University of Calgary, Calgary, AB, Canada), Cynthia T. French, PhD, FCCP (UMass Memorial Medical Center, Worcester, MA), Peter Gibson, MBBS (Hunter Medical Research Institute, New South Wales, Australia), Philip Gold, MD, MACP, FCCP (Loma Linda University, Loma Linda, CA), Cameron Grant, MB ChB, PhD (University of Auckland School of Medicine, Auckland, New Zealand), Susan M. Harding, MD, FCCP (Division of Pulmonology, Allergy, and Critical Care Medicine, University of Alabama at Birmingham, Birmingham, AL), Anthony Harnden, MB ChB, MSc (University of Oxford, Oxford, England), Adam T. Hill, MB ChB, MD (Royal Infirmary and University of Edinburgh, Edinburgh, Scotland), Richard S. Irwin, MD, Master FCCP (UMass Memorial Medical Center, Worcester, MA), Peter J. Kahrilas, MD (Feinberg School of Medicine, Northwestern University, Chicago, IL), Karina A. Keogh, MD (Mayo Clinic, Rochester, MN), Kefang Lai, MD, PhD (First Affiliated Hospital of Guangzhou Medical College, Guangzhou, China), Andrew P. Lane, MD (Johns Hopkins University School of Medicine, Baltimore, MD), Kaiser Lim, MD (Mayo Clinic, Rochester, MN), Mark A. Malesker, PharmD, FCCP (Creighton University School of Pharmacy and Health Professions, Omaha, NE), Peter Mazzone, MD, MPH, FCCP (The Cleveland Clinic, Cleveland, OH), Lorcan McGarvey, MD (The Queen’s University Belfast, Belfast, United Kingdom), M. Hassan Murad, MD, MPH (Mayo Clinic, Rochester, MN), Peter Newcombe, PhD (School of Psychology, University of Queensland, Queensland, Australia), Huong Q. Nguyen, PhD, RN (Kaiser Permanente, Pasadena, CA), John Oppenheimer, MD (University of Medicine and Dentistry of New Jersey/Rutgers University, Newark, NJ), Mark Rosen, MD, Master FCCP (American College of Chest Physicians, Glenview, IL), Bruce Rubin, MEngr, MD, MBA (Virginia Commonwealth University, Richmond, VA), Jay H. Ryu, MD, FCCP (Mayo Clinic, Rochester, MN), Jaclyn Smith, MB ChB, PhD (University of Manchester, Manchester, England), Susan M. Tarlo, MBBS, FCCP (Toronto Western Hospital, Toronto, ON, Canada), Anne E. Vertigan, PhD, MBA, BAppSc (SpPath) (John Hunter Hospital, New South Wales, Australia), Gang Wang, MD, PhD (Sichuan University, West China Hospital, Chengdu, China), Miles Weinberger, MD, FCCP (University of Iowa Hospitals and Clinics, Iowa City, IA), Kelly Weir, MsPath (Queensland Children’s Medical Research Institute, Queensland, Australia)
Other Contributions: The authors thank Nancy Harger, MLS, and Judy Nordberg, MLS, Education and Clinical Services Librarians working in the University of Massachusetts Medical School Library who undertook all the searches for this systematic review.
Role of Sponsors: The American College of Chest Physicians was the sole supporter of these guidelines, this article, and the innovations addressed within.
Footnotes
DISCLAIMER: American College of Chest Physician guidelines are intended for general information only, are not medical advice, and do not replace professional medical care and physician advice, which always should be sought for any medical condition. The complete disclaimer for this guideline can be accessed at http://www.chestnet.org/Guidelines-and-Resources/Guidelines-and-Consensus-Statements/CHEST-Guidelines.
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
Contributor Information
Louis-Philippe Boulet, Email: lpboulet@med.ulaval.ca.
CHEST Expert Cough Panel:
Kenneth W. Altman, Alan F. Barker, Surinder S. Birring, Fiona Blackhall, Donald C. Bolser, Louis-Philippe Boulet, Sidney S. Braman, Christopher Brightling, Priscilla Callahan-Lyon, Anne B. Chang, Terrie Cowley, Paul Davenport, Satoru Ebihara, Ali A. El Solh, Patricio Escalante, Anthony Feinstein, Stephen K. Field, Dina Fisher, Cynthia T. French, Peter Gibson, Philip Gold, Cameron Grant, Susan M. Harding, Anthony Harnden, Adam T. Hill, Richard S. Irwin, Peter J. Kahrilas, Karina A. Keogh, Kefang Lai, Andrew P. Lane, Kaiser Lim, Mark A. Malesker, Peter Mazzone, Lorcan McGarvey, M. Hassan Murad, Peter Newcombe, Huong Q. Nguyen, John Oppenheimer, Mark Rosen, Bruce Rubin, Jay H. Ryu, Jaclyn Smith, Susan M. Tarlo, Anne E. Vertigan, Gang Wang, Miles Weinberger, and Kelly Weir
References
- 1.Paivinen M.K., Keskinen K.L., Tikkanen H.O. Swimming and asthma: differences between women and men. J Allergy. 2013;2013:520913. doi: 10.1155/2013/520913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Batista C., Soares J.M. Are former athletes more prone to asthma? J Asthma. 2013;50(4):403–409. doi: 10.3109/02770903.2013.776075. [DOI] [PubMed] [Google Scholar]
- 3.Romberg K., Tufvesson E., Bjermer L. Asthma is more prevalent in elite swimming adolescents despite better mental and physical health. Scand J Med Sci Sports. 2012;22(3):362–371. doi: 10.1111/j.1600-0838.2010.01177.x. [DOI] [PubMed] [Google Scholar]
- 4.Turcotte H., Langdeau J.B., Thibault G., Boulet L.P. Prevalence of respiratory symptoms in an athlete population. Respir Med. 2003;97(8):955–963. doi: 10.1016/s0954-6111(03)00123-9. [DOI] [PubMed] [Google Scholar]
- 5.Rundell K.W., Im J., Mayers L.B., Wilber R.L., Szmedra L., Schmitz H.R. Self-reported symptoms and exercise-induced asthma in the elite athlete. Med Sci Sports Exerc. 2001;33(2):208–213. doi: 10.1097/00005768-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Rundell K.W., Wilber R.L., Szmedra L., Jenkinson D.M., Mayers L.B., Im J. Exercise-induced asthma screening of elite athletes: field versus laboratory exercise challenge. Med Sci Sports Exerc. 2000;32(2):309–316. doi: 10.1097/00005768-200002000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Lund T., Pedersen L., Larsson B., Backer V. Prevalence of asthma-like symptoms, asthma and its treatment in elite athletes. Scand J Med Sci Sports. 2009;19(2):174–178. doi: 10.1111/j.1600-0838.2007.00753.x. [DOI] [PubMed] [Google Scholar]
- 8.Drobnic F., Casan P., Banquells M., Miralda R., Sanchis J. Cough after exercise in the elite athlete. Sports Med Training Rehab. 1996;6(4):309–315. [Google Scholar]
- 9.Turmel J., Bougault V., Boulet L.P. Seasonal variations of cough reflex sensitivity in elite athletes training in cold air environment. Cough. 2012;8(1):2. doi: 10.1186/1745-9974-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Katz R.M., Siegel S.C., Rachelefsky G.S. Chronic cough in athletes. Clin Rev Allergy. 1988;6(4):431–441. [PubMed] [Google Scholar]
- 11.Boulet L.P., O'Byrne P.M. Asthma and exercise-induced bronchoconstriction in athletes. N Engl J Med. 2015;372(7):641–648. doi: 10.1056/NEJMra1407552. [DOI] [PubMed] [Google Scholar]
- 12.Bussotti M., Di Marco S., Marchese G. Respiratory disorders in endurance athletes—how much do they really have to endure? Open Access J Sports Med. 2014;5:47–63. doi: 10.2147/OAJSM.S57828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boulet L.P. Cough and upper airway disorders in elite athletes: a critical review. Br J Sports Med. 2012;46(6):417–421. doi: 10.1136/bjsports-2011-090812. [DOI] [PubMed] [Google Scholar]
- 14.Heir T., Oseid S. Self-reported asthma and exercise-induced asthma symptoms in high-level competitive cross-country skiers. Scand J Med Sci Sports. 1994;4:128–133. [Google Scholar]
- 15.Weiler J.M., Metzger W.J., Donnelly A.L., Crowley E.T., Sharath M.D. Prevalence of bronchial hyperresponsiveness in highly trained athletes. Chest. 1986;90(1):23–28. doi: 10.1378/chest.90.1.23. [DOI] [PubMed] [Google Scholar]
- 16.Hull J.H., Ansley L., Robson-Ansley P., Parsons J.P. Managing respiratory problems in athletes. Clin Med. 2012;12(4):351–356. doi: 10.7861/clinmedicine.12-4-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh A.M., McGregor R.S. Differential diagnosis of chest symptoms in the athlete. Clinical Rev Allergy Immunol. 2005;29(2):87–96. doi: 10.1385/CRIAI:29:2:087. [DOI] [PubMed] [Google Scholar]
- 18.Pope J.S., Koenig S.M. Pulmonary disorders in the training room. Clin Sports Med. 2005;24(3):541–564. doi: 10.1016/j.csm.2005.05.003. viii. [DOI] [PubMed] [Google Scholar]
- 19.Truwit J. Pulmonary disorders and exercise. Clin Sports Med. 2003;22(1):161–180. doi: 10.1016/s0278-5919(02)00042-x. [DOI] [PubMed] [Google Scholar]
- 20.Rasmussen B.S., Hanel B., Jensen K., Serup B., Secher N.H. Decrease in pulmonary diffusion capacity after maximal exercise. J Sports Sci. 1986;4(3):185–188. doi: 10.1080/02640418608732117. [DOI] [PubMed] [Google Scholar]
- 21.Koskela H.O. Cold air-provoked respiratory symptoms: the mechanisms and management. Int J Circumpolar Health. 2007;66(2):91–100. doi: 10.3402/ijch.v66i2.18237. [DOI] [PubMed] [Google Scholar]
- 22.Florida-James G., Donaldson K., Stone V. Athens 2004: the pollution climate and athletic performance. J Sports Sci. 2004;22(10):967–980. doi: 10.1080/02640410400000272. discussion 980. [DOI] [PubMed] [Google Scholar]
- 23.Paul D.W., Bogaard J.M., Hop W.C. The bronchoconstrictor effect of strenuous exercise at low temperatures in normal athletes. Int J Sports Med. 1993;14(8):433–436. doi: 10.1055/s-2007-1021205. [DOI] [PubMed] [Google Scholar]
- 24.Pierson W.E. Impact of air pollutants on athletic performance. Allergy Proc. 1989;10(3):209–214. doi: 10.2500/108854189778960144. [DOI] [PubMed] [Google Scholar]
- 25.Seys S.F., Hox V., Gerven L.V. Damage associated molecular pattern and innate cytokine release in the airways of competitive swimmers. Allergy. 2015;70(2):187–194. doi: 10.1111/all.12540. [DOI] [PubMed] [Google Scholar]
- 26.Thompson M, Tiwari A, Fu R, Moe E, Buckley DI. A framework to facilitate the use of systematic reviews and meta-analyses in the design of primary research studies. Rockville, MD, 2012. Agency for Healthcare Research and Quality (US); 2012. Report No.: 12-EHC009-EF. AHRQ Methods for Effective Health Care. [PubMed]
- 27.Maron B.J., Zipes D.P. Bethesda Conference #36 and the European Society of Cardiology Consensus Recommendations revisited a comparison of U.S. and European criteria for eligibility and disqualification of competitive athletes with cardiovascular abnormalities. J Am Coll Cardiol. 2005;45:2–64. doi: 10.1016/j.jacc.2008.08.055. [DOI] [PubMed] [Google Scholar]
- 28.Higgins J.P.T., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 [updated March 2011] The Cochrane Collaboration; 2011. www.handbook.cochrane.org Accessed December 21, 2016. [Google Scholar]
- 29.Reeves B.C., Deeks J.J., Higgins J.P.T., Wells G.A. Chapter 13: Including non-randomized studies. In: Higgins J.P.T., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0 (updated March 2011) The Cochrane Collaboration; 2011. www.handbook.cochrane.org Accessed December 21, 2016. [Google Scholar]
- 30.Lewis S.Z., Diekemper R.L., French C.T. Methodologies for the development of the management of cough: CHEST guideline and expert panel report. Chest. 2014;146(5):1395–1402. doi: 10.1378/chest.14-1484. [DOI] [PubMed] [Google Scholar]
- 31.Balshem H., Helfand M., Schunemann H.J. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 32.Andrews J.C., Schunemann H.J., Oxman A.D. GRADE guidelines: 15. Going from evidence to recommendation-determinants of a recommendation's direction and strength. J Clin Epidemiol. 2013;66(7):726–735. doi: 10.1016/j.jclinepi.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Couto M., Moreira A., Delgado L. Diagnosis and treatment of asthma in athletes. Breathe. 2012;8(4):287–296. [Google Scholar]
- 34.Lund T.K., Pedersen L., Anderson S.D., Sverrild A., Backer V. Are asthma-like symptoms in elite athletes associated with classical features of asthma? Br J Sports Med. 2009;43(14):1131–1135. doi: 10.1136/bjsm.2008.054924. [DOI] [PubMed] [Google Scholar]
- 35.McKenzie D.C., Boulet L.P. Asthma, outdoor air quality and the Olympic Games. CMAJ. 2008;179(6):543–548. doi: 10.1503/cmaj.080982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eichner E.R. Asthma in athletes: scope, risks, mimics, trends. Curr Sports Med Rep. 2008;7(3):118–119. doi: 10.1097/01.CSMR.0000319713.71416.6f. [DOI] [PubMed] [Google Scholar]
- 37.Mansournia M.A., Jamali M., Mansournia N., Yunesian M., Moghadam K.G. Exercise-induced bronchospasm among students of Tehran University of Medical Sciences in 2004. Allergy Asthma Proc. 2007;28(3):348–352. doi: 10.2500/aap.2007.28.2943. [DOI] [PubMed] [Google Scholar]
- 38.Rundell K.W., Spiering B.A., Evans T.M., Baumann J.M. Baseline lung function, exercise-induced bronchoconstriction, and asthma-like symptoms in elite women ice hockey players. Med Sci Sports Exerc. 2004;36(3):405–410. doi: 10.1249/01.mss.0000117118.77267.bf. [DOI] [PubMed] [Google Scholar]
- 39.Capao-Filipe M., Moreira A., Delgado L., Rodrigues J., Vaz M. Exercise-induced bronchoconstriction and respiratory symptoms in elite athletes. Allergy. 2003;58(11):1196. doi: 10.1046/j.0105-4538.2003.00309.x. [DOI] [PubMed] [Google Scholar]
- 40.Anderson S.D., Holzer K. Exercise-induced asthma: is it the right diagnosis in elite athletes? J Allergy Clin Immunol. 2000;106(3):419–428. doi: 10.1067/mai.2000.108914. [DOI] [PubMed] [Google Scholar]
- 41.Storms W.W. Exercise-induced asthma: diagnosis and treatment for the recreational or elite athlete. Med Sci Sports Exerc. 1999;31(1 suppl):S33–S38. doi: 10.1097/00005768-199901001-00006. [DOI] [PubMed] [Google Scholar]
- 42.Friemel F. Clinical and functional aspects of post exercise asthma in athletes. Sci Sports. 1992;7(3):147–150. [Google Scholar]
- 43.Simpson A.J., Romer L.M., Kippelen P. Self-reported symptoms after induced and inhibited bronchoconstriction in athletes. Med Sci Sports Exerc. 2015;47(10):2005–2013. doi: 10.1249/MSS.0000000000000646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schenk K., Faulhaber M., Gatterer H., Burtscher M., Ferrari M. Ski mountaineering competition: fit for it? Clin J Sport Med. 2011;21(2):114–118. doi: 10.1097/JSM.0b013e31820f903e. [DOI] [PubMed] [Google Scholar]
- 45.Seys S.F., Feyen L., Keirsbilck S., Adams E., Dupont L.J., Nemery B. An outbreak of swimming-pool related respiratory symptoms: an elusive source of trichloramine in a municipal indoor swimming pool. Int J Hyg Environ Health. 2015;218(4):386–391. doi: 10.1016/j.ijheh.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Yamauchi R., Shimizu K., Kimura F. Virus activation and immune function during intense training in rugby football players. Int J Sports Med. 2011;32(5):393–398. doi: 10.1055/s-0031-1271674. [DOI] [PubMed] [Google Scholar]
- 47.Schwellnus M.P., Lichaba M., Derman E.W. Respiratory tract symptoms in endurance athletes—a review of causes and consequences. Curr Allergy Clin Immunol. 2010;23(2):52–57. [Google Scholar]
- 48.Cox A.J., Gleeson M., Pyne D.B., Callister R., Hopkins W.G., Fricker P.A. Clinical and laboratory evaluation of upper respiratory symptoms in elite athletes. Clin J Sport Med. 2008;18(5):438–445. doi: 10.1097/JSM.0b013e318181e501. [DOI] [PubMed] [Google Scholar]
- 49.Hinkes E., Bhorade S.M., Wood L.D.H., Ndukwu I.M. Young adult with near-fatal pneumonia caused by adenovirus serotype 7. Respir Care. 1999;44(5):524–527. [Google Scholar]
- 50.Weidner T.G. Reporting behaviors and activity levels of intercollegiate athletes with an URI. Med Sci Sports Exerc. 1994;26(1):22–26. [PubMed] [Google Scholar]
- 51.Robson-Ansley P., Howatson G., Tallent J. Prevalence of allergy and upper respiratory tract symptoms in runners of the London marathon. Med Sci Sports Exerc. 2012;44(6):999–1004. doi: 10.1249/MSS.0b013e318243253d. [DOI] [PubMed] [Google Scholar]
- 52.Marcinow A.M., Thompson J., Chiang T., Forrest L.A., deSilva B.W. Paradoxical vocal fold motion disorder in the elite athlete: experience at a large division I university. Laryngoscope. 2014;124(6):1425–1430. doi: 10.1002/lary.24486. [DOI] [PubMed] [Google Scholar]
- 53.Panchasara B., Nelson C., Niven R., Ward S., Hull J.H. Lesson of the month: rowing-induced laryngeal obstruction: a novel cause of exertional dyspnoea: characterised by direct laryngoscopy. Thorax. 2015;70(1):95–97. doi: 10.1136/thoraxjnl-2014-205773. [DOI] [PubMed] [Google Scholar]
- 54.Yim E.S., Horn E.R., Hegedus A., Tibbles C.D. Cough and hemoptysis in athletes of an ice hockey team. J Emerg Med. 2012;43(1):107–110. doi: 10.1016/j.jemermed.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 55.Seccombe L.M., Rogers P.G., Jenkins C.R., Peters M.J. Maintenance of vital capacity during repetitive breath-hold in a spearfishing competition. Respirology. 2012;17(2):350–353. doi: 10.1111/j.1440-1843.2011.02090.x. [DOI] [PubMed] [Google Scholar]
- 56.Carter E.A., Koehle M.S. Immersion pulmonary edema in female triathletes. Pulm Med. 2011;2011:261404. doi: 10.1155/2011/261404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Koehle M.S., Lepawsky M., McKenzie D.C. Pulmonary oedema of immersion. Sports Med. 2005;35(3):183–190. doi: 10.2165/00007256-200535030-00001. [DOI] [PubMed] [Google Scholar]
- 58.Adir Y., Shupak A., Gil A. Swimming-induced pulmonary edema—clinical presentation and serial lung function. Chest. 2004;126(2):394–399. doi: 10.1378/chest.126.2.394. [DOI] [PubMed] [Google Scholar]
- 59.Lund K.L., Mahon R.T., Tanen D.A., Bakhda S. Swimming-induced pulmonary edema. Ann Emerg Med. 2003;41(2):251–256. doi: 10.1067/mem.2003.69. [DOI] [PubMed] [Google Scholar]
- 60.Hultgren H.N. High-altitude pulmonary edema: current concepts. Ann Rev Med. 1996;47:267–284. doi: 10.1146/annurev.med.47.1.267. [DOI] [PubMed] [Google Scholar]
- 61.Landesberg W.H. Pulmonary embolism in a female collegiate cross-country runner presenting as nonspecific back pain. J Chiropr. 2012;11(3):215–220. doi: 10.1016/j.jcm.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Edmonds C. A salt water aspiration syndrome. Mil Med. 1970;135(9):779–785. [PubMed] [Google Scholar]
- 63.Tsimoyianis G.V., Jacobson M.S., Feldman J.G. Reduction in pulmonary function and increased frequency of cough associated with passive smoking in teenage athletes. Pediatrics. 1987;80(1):32–36. [PubMed] [Google Scholar]
- 64.Bonini M., Braido F., Baiardini I. AQUA: Allergy Questionnaire for Athletes. Development and validation. Med Sci Sports Exerc. 2009;41(5):1034–1041. doi: 10.1249/MSS.0b013e318193c663. [DOI] [PubMed] [Google Scholar]
- 65.Teixeira R.N., Mendes F.A., Martins M.A., Mickleborough T.D., Carvalho C.R. AQUA© as predictor of allergy in elite marathon runners. World Allergy Org J. 2014;7:1. doi: 10.1186/1939-4551-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Turcotte H., Langdeau J.B., Bowie D.M., Boulet L.P. Are questionnaires on respiratory symptoms reliable predictors of airway hyperresponsiveness in athletes and sedentary subjects? J Asthma. 2003;40(1):71–80. doi: 10.1081/jas-120017209. [DOI] [PubMed] [Google Scholar]
- 67.Bordeleau M., Turmel J., Boulet L.P. Effects of ipratropium on exercise-induced cough in winter athletes: a hypothesis-generating study. Phys Sportsmed. 2014;42(4):7–13. doi: 10.3810/psm.2014.11.2086. [DOI] [PubMed] [Google Scholar]
- 68.Gong H., Jr., Bedi J.F., Horvath S.M. Inhaled albuterol does not protect against ozone toxicity in nonasthmatic athletes. Arch Environ Health. 1988;43(1):46–53. doi: 10.1080/00039896.1988.9934373. [DOI] [PubMed] [Google Scholar]
- 69.Koya T., Hasegawa T., Tanaka J. Effect of ciclesonide on bronchial asthma in athletes. J Asthma. 2009;46(10):1032–1036. doi: 10.3109/02770900903229693. [DOI] [PubMed] [Google Scholar]
- 70.Helenius I., Lumme A., Ounap J. No effect of montelukast on asthma-like symptoms in elite ice hockey players. Allergy. 2004;59(1):39–44. doi: 10.1046/j.1398-9995.2003.00353.x. [DOI] [PubMed] [Google Scholar]
- 71.Sue-Chu M., Karjalainen E.M., Laitinen A., Larsson L., Laitinen L.A., Bjermer L. Placebo-controlled study of inhaled budesonide on indices of airway inflammation in bronchoalveolar lavage fluid and bronchial biopsies in cross-country skiers. Respiration. 2000;67(4):417–425. doi: 10.1159/000029541. [DOI] [PubMed] [Google Scholar]
- 72.Peters E.M., Goetzsche J.M., Grobbelaar B., Noakes T.D. Vitamin C supplementation reduces the incidence of postrace symptoms of upper-respiratory-tract infection in ultramarathon runners. Am J Clin Nutr. 1993;57(2):170–174. doi: 10.1093/ajcn/57.2.170. [DOI] [PubMed] [Google Scholar]
- 73.ter Steege R.W., Van der Palen J., Kolkman J.J. Prevalence of gastrointestinal complaints in runners competing in a long-distance run: an internet-based observational study in 1281 subjects. Scand J Gastroenterol. 2008;43(12):1477–1482. doi: 10.1080/00365520802321170. [DOI] [PubMed] [Google Scholar]
- 74.Dimeo F.C., Peters J., Guderian H. Abdominal pain in long distance runners: case report and analysis of the literature. Br J Sports Med. 2004;38(5):E24. doi: 10.1136/bjsm.2003.007237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.de Oliveira E.P., Burini R.C. The impact of physical exercise on the gastrointestinal tract. Curr Opin Clin Nutr Metab Care. 2009;12(5):533–538. doi: 10.1097/MCO.0b013e32832e6776. [DOI] [PubMed] [Google Scholar]
- 76.Pratter M.R., Brightling C.E., Boulet L.P., Irwin R.S. An empiric integrative approach to the management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):222S–231S. doi: 10.1378/chest.129.1_suppl.222S. [DOI] [PubMed] [Google Scholar]