Abstract
Background
Despite Food and Drug Administration approval of 2 new drugs for idiopathic pulmonary fibrosis (IPF), curative therapies remain elusive and mortality remains high. Preclinical and clinical data support the safety of human mesenchymal stem cells as a potential novel therapy for this fatal condition. The Allogeneic Human Cells (hMSC) in patients with Idiopathic Pulmonary Fibrosis via Intravenous Delivery (AETHER) trial was the first study designed to evaluate the safety of a single infusion of bone marrow–derived mesenchymal stem cells in patients with idiopathic pulmonary fibrosis.
Methods
Nine patients with mild to moderate IPF were sequentially assigned to 1 of 3 cohorts and dosed with a single IV infusion of 20, 100, or 200 × 106 human bone marrow–derived mesenchymal stem cells per infusion from young, unrelated, men. All baseline patient data were reviewed by a multidisciplinary study team to ensure accurate diagnosis. The primary end point was the incidence (at week 4 postinfusion) of treatment-emergent serious adverse events, defined as the composite of death, nonfatal pulmonary embolism, stroke, hospitalization for worsening dyspnea, and clinically significant laboratory test abnormalities. Safety was assessed until week 60 and additionally 28 days thereafter. Secondary efficacy end points were exploratory and measured disease progression.
Results
No treatment-emergent serious adverse events were reported. Two nontreatment-related deaths occurred because of progression of IPF (disease worsening and/or acute exacerbation). By 60 weeks postinfusion, there was a 3.0% mean decline in % predicted FVC and 5.4% mean decline in % predicted diffusing capacity of the lungs for carbon monoxide.
Conclusions
Data from this trial support the safety of a single infusion of human mesenchymal stem cells in patients with mild-moderate IPF.
Trial Registry
ClinicalTrials.gov; No.: NCT02013700; URL: www.clinicaltrials.gov.
Key Words: bone marrow, idiopathic pulmonary fibrosis, mesenchymal stem cells, safety trial
Abbreviations: 6-MWT, 6-min walk test; Dlco, diffusing capacity of the lungs for carbon monoxide; FDA, Food and Drug Administration; hMSCs, human mesenchymal stem cells; HRCT, high-resolution CT; IPF, idiopathic pulmonary fibrosis; MedDRA, Medical Dictionary for Regulatory Activities; MSCs, mesenchymal stem cells
FOR EDITORIAL COMMENT SEE PAGE 951
Idiopathic pulmonary fibrosis (IPF) is a progressive and debilitating lung disease characterized by interstitial fibrosis with decreasing lung volumes and pulmonary insufficiency, eventually resulting in death.1 Because of the insidious onset of symptoms, however, most patients receive a diagnosis at late stages of the disease after significant fibrosis has occurred. Diagnosis is established by the pathologic finding of usual interstitial pneumonia and/or by high-resolution CT (HRCT).2, 3, 4
The natural history of this disease is characterized by inexorable progressive decline interspersed with “exacerbations” or periods of accelerated disease, which are often fatal.1 Although 2 new drugs were recently approved by the Food and Drug Administration (FDA) for patients with IPF, neither is curative.5, 6
In preclinical studies, mesenchymal stem cells (MSCs) have shown promise as a potential novel treatment for lung disease.7, 8, 9 Studies of MSCs have shown that they contribute to tissue regeneration, home to sites of lung injury, contribute to tissue remodeling, decrease chronic airway inflammation, and restore alveolar fluid balance in acute lung injury.10, 11, 12, 13, 14, 15
In addition to safety data from preclinical studies, human trials have also demonstrated the safety and tolerability of IV allogeneic mesenchymal stem cells (hMSCs).16, 17, 18, 19, 20, 21, 22, 23 A single-center, open-label phase Ib study assessed the safety and tolerability of multiple IV doses of adipose-derived stromal cell-stromal vascular fraction (n = 14) for the treatment of IPF. Although short-term infusion toxicities and long-term ectopic tissue formation were reported, no adverse events related to the study treatment were observed.21 In another single-center phase I study, patients with IPF received IV placenta-derived hMSCs (n = 8). In this study, most adverse events were mild and self-limiting and no deaths were reported.19
Our study, the Allogeneic Human Cells in Patients With Idiopathic Pulmonary Fibrosis via Intravenous Delivery (AETHER) trial, was the first human trial designed to evaluate the safety of bone marrow–derived human allogeneic mesenchymal stem cells in patients with mild to moderate IPF.
Methods
Study Design and Participants
AETHER was a single-center, nonrandomized, non–placebo-controlled phase I study of 9 patients with mild to moderate IPF. The study was conducted at the University of Miami Miller School of Medicine (Miami, FL). Eligible patients were between the ages of 40 and 90, had a diagnosis of IPF according to American Thoracic Society guidelines, an FVC of at least 50% predicted, and a diffusing capacity of the lungs for carbon monoxide (Dlco) of at least 30% predicted.1 Patients received diagnoses by HRCT (lung biopsy was required in instances of inconclusive diagnosis). Patients with other infiltrative diseases, connective tissue disease, pulmonary hypertension, peripheral capillary oxygen saturation <93% at rest at sea level, life expectancy shorter than 1 year, and those actively listed for any organ transplant were excluded. Concomitant therapies, except oxygen supplementation and pulmonary rehabilitation, were prohibited.
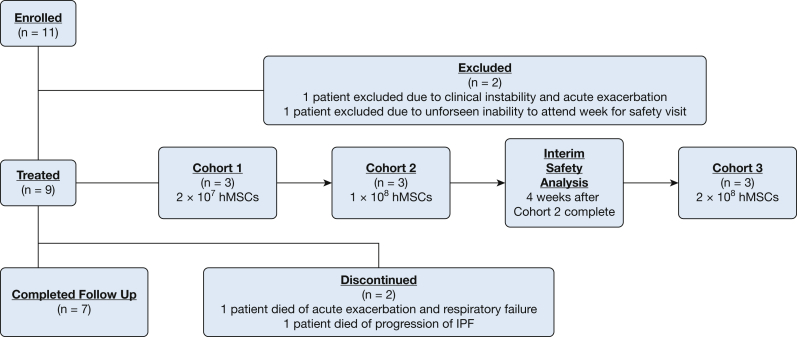
Eleven patients were enrolled between October 30, 2013, and September 9, 2014 (Fig 1). Two participants withdrew before treatment (1 from clinical instability and exacerbation of disease [patient 008] and another from an unforeseen inability to attend the week 4 safety visit [patient 009]). All patients provided written informed consent before enrollment and were treated according to the protocol approved by the University of Miami Institutional Review Board (protocol approval #20120924).
Figure 1.
Clinical trial participant flow chart.
The primary end point was the incidence (at week 4 postinfusion) of any treatment emergent serious adverse events, defined as the composite of death, nonfatal pulmonary embolism, stroke, hospitalization for worsening dyspnea, and clinically significant laboratory test abnormalities. This definition of treatment-emergent adverse events was made on the basis of single-dose IV MSC clinical trials in cardiovascular disease and aging. These trials used 30-day treatment-emergent adverse events as a primary safety end point.18, 24, 25 Secondary efficacy end points were exploratory and related to disease progression (rate of acute exacerbations as defined by consensus guidelines, and decline of lung function as measured by absolute FVC and Dlco).
Procedures
Patients were assigned to 1 of 3 cohorts and received treatment between November 21, 2013, and October 13, 2014. Allocation ratio to cohorts was 1:1:1 (n = 9), with enrolled patients sequentially assigned to the 3 cohorts. Dose escalation occurred between cohorts as shown in Table 1.
Table 1.
Dosing Schedule of AETHER Participants
| Cohort | Subject ID | Dosing Date |
|---|---|---|
| Cohort 1 | 001 | November 21, 2013 |
| 2 × 107 hMSCs/infusion | 002 | January 22, 2014 |
| (20 million) | 003 | February 26, 2014 |
| Cohort 2 | 004 | April 17, 2014 |
| 1 × 108 hMSCs/infusion | 005 | May 9, 2014 |
| (100 million) | 006 | May 15, 2104 |
| Cohort 3 | 007 | September 5, 2014 |
| 2 × 108 hMSCs/infusion | 010 | October 8, 2014 |
| (200 million) | 011 | October 13, 2014 |
AETHER = Allogeneic Human Mesenchymal Stem Cells in Patients With Idiopathic Pulmonary Fibrosis via Intravenous Delivery trial; hMSCs = human mesenchymal stem cells.
Patients in the study received a standard dose of hMSCs rather than weight-based doses made on the basis of results from previous studies in patients with cardiovascular disease.16 Detailed study procedures are listed in Table 2. At the initial screening visit, informed consent was obtained and medical history was reviewed. Baseline studies included physical examination, routine bloodwork, urinalysis, ECG, echocardiogram, HRCT, spirometry, Dlco, lung volumes, 6-min walk test (6-MWT), and quality of life questionnaires. Treatment infusion was considered day 1. Adverse events were reviewed at day 1, week 1, and at all visits thereafter. The primary end point was assessed starting at week 4 until week 60 and additionally 28 days thereafter. Secondary efficacy end points were measured at baseline and every 12 weeks until week 60.
Table 2.
AETHER Schedule of Assessments
| Visit | Screening ± 28 d | Baseline 2-4 wk | Day 1 Week 1 | Day 2 | Week 1 (Day 7) | Week 2 (Day 14) | Month 1 (Week 4) | Month 3 Week 12 (±3-5 d) | Month 6 Week 24 (±3-5 d) | Month 9 Week 36 (±3-5 d) | Month 12 Week 48 (±3-5 d) | Month 15 Week 60 (±3-5 d) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Informed consent | x | |||||||||||
| Full medical history | x | |||||||||||
| Physical examination | x | x | x | x | x | x | x | x | x | x | x | x |
| Chem7, LFTs, PT/INR | x | x | x | x | x | x | x | |||||
| Urinalysis, CBC, and metabolic profile | x | x | x | x | x | x | x | x | ||||
| Spirometry | x | x | x | x | x | x | ||||||
| Dlco | x | x | x | x | x | x | ||||||
| Echocardiogram | x | x | ||||||||||
| ECG | x | x | x | x | x | x | x | x | x | x | x | x |
| Treatment | x | |||||||||||
| Review adverse events | x | x | x | x | x | x | x | x | x | |||
| HRCT | x | x | x | |||||||||
| 6-MWT | x | x | x | x | x | x | ||||||
| Lung volumes | x | x | x | x | x | x | ||||||
| QOL questionnaires | x | x | x | x | x | x | x |
CBC = complete blood count; Chem7 = sodium, potassium, chloride, uric acid, glucose, blood urea nitrogen, creatinine; Dlco = diffusing capacity of the lungs for carbon monoxide; HRCT = high-resolution CT; LFTs = liver function tests (alanine transaminase, alkaline phosphatase, aspartate transaminase, bilirubin, albumin, total protein, gamma glutamyl transpeptidase); PT/INR = prothrombin time (PT) along with its derived measures of prothrombin ratio and international normalized ratio (INR); QOL = quality of life. See Table 1 legend for expansion of other abbreviations.
Isolation of hMSCs
Because of the potential for pregnancy-induced antibodies to men’s antigens, hMSCs were obtained only from men. Two men aged 24 and 25 years underwent bone marrow aspiration. Donors were neither related nor human leukocyte antigen–matched to recipients. Screening of allogeneic donors followed standard transplant practices and all allogeneic donors met allogeneic donor eligibility criteria as outlined in 21 CFR Part 1271. Donor eligibility screening included testing for antibodies against HIV-1/2, human T-lymphocyte virus I/II, hepatitis C virus, hepatitis B core (IgG and IgM), and cytomegalovirus; nucleic acid testing for HIV-1, hepatitis C virus, and West Nile virus; and testing for the surface antigen of the hepatitis B virus, Trypanosoma cruzi enzyme-linked immunosorbent assay, and rapid plasma reagin.
For each donor, a total of 60 mL of bone marrow was aspirated from the posterior iliac crest. The mononuclear cell fraction was isolated using a density gradient with lymphocyte separation media (specific gravity, 1.077). Low-density cells were collected and washed with Plasma-Lyte A containing 1% human serum albumin. Washed cells were sampled and viable cell numbers determined. The bone marrow mononuclear cells were seeded into 225 cm2 tissue culture flasks in alpha Minimal Essential Medium containing 20% fetal bovine serum. After 14 days of culture, passage zero (P0) cells were harvested by trypsin treatment and expanded into 60 individual flasks. These flasks were incubated for a further 7 to 10 days before harvesting of MSCs by trypsin treatment (P1 cells). All procedures used in the preparation of the investigational product followed protocols previously published by the sponsor (Joshua M. Hare).26
Safety and Monitoring
After administration of hMSCs, patients were observed overnight in the ICU for any clinically significant changes in respiratory or cardiovascular parameters. Vital signs were assessed 2 hours before infusion, at the start of the infusion, and every 15 minutes after infusion.
The incidence and nature of all serious adverse events were reviewed and independently evaluated by the data safety monitoring board to determine whether they could be related to MSC administration. The data safety monitoring board was responsible for reviewing data for each cohort before dose escalation and for making recommendations regarding the continuation of the trial on the basis of the interim safety analysis performed 4 weeks after treatment of the last patient in cohort 2.
A nonsafety-related temporary hold was placed on the study on June 30, 2015, by the FDA. All 9 participants were dosed before the hold; therefore, the dosing schedule was not affected. Adverse events were graded according to the Medical Dictionary for Regulatory Activities (MedDRA) scale.
Statistical Analysis
No formal statistical justification was performed to determine sample size. Cohort size was determined on the basis of expected requirements for safety analyses and projected enrollment rates. A 2-tailed Student t test was used to evaluate differences in secondary end points from baseline. A P value < .05 was considered statistically significant.
Results
Table 3 summarizes the baseline characteristics of the 9 patients receiving treatment. Mean age of patients was 71.6 (±6.13) years, and all patients were white men of Hispanic/Latino or Caucasian descent. Mean time from diagnosis was 22 months. On the basis of baseline total lung capacity, FVC, Dlco, 6-MWT results, and the use of supplemental oxygen, patients in cohort 3 appear to have had more advanced disease than patients in cohorts 1 and 2. Eight patients received a diagnosis by HRCT; 1 required a lung biopsy because of a lack of honeycombing on the baseline HRCT.
Table 3.
Baseline Characteristics of Treated Patients
| Characteristic | Cohort 1 2 × 107 hMSCs/Infusion |
Cohort 2 1 × 108 hMSCs/Infusion |
Cohort 3 2 × 108 hMSCs/Infusion |
All Cohorts |
|---|---|---|---|---|
| Age, y, mean (SD) | 71.00 (7.21) | 73.33 (4.04) | 70.33 (8.62) | 71.6 (6.13) |
| Men, No. (%) | 3 (100) | 3 (100) | 3 (100) | 9 (100) |
| Race, white, No. (%) | 3 (100) | 3 (100) | 3 (100) | 9 (100) |
| Ethnicity, Caucasian, No. (%) | 1 (33.3) | 2 (66.7) | 3 (100) | 6 (67) |
| Ethnicity, Hispanic/Latino, No. (%) | 2 (66.7) | 1 (33.3) | 0 (0) | 3 (33) |
| Time from diagnosis ≤1 y, No. (%) | 2 (66.7) | 0 (0) | 1 (33.3) | 3 (33) |
| Time from diagnosis ≥1 y, No. (%) | 1 (33.3) | 3 (100) | 2 (66.7) | 6 (67) |
| HRCT diagnosis, No. (%) | 2 (66.7) | 3 (100) | 3 (100) | 8 (88.9) |
| HRCT + biopsy diagnosis, No. (%) | 1 (33.3) | 0 (0) | 0 (0) | 1 (11.1) |
| TLC, L, mean (SD) | 4.15 (0.59) | 4.39 (1.22) | 3.93 (0.21) | 4.16 (0.71) |
| FVC, % predicted, mean (SD) | 76.00 (18.73) | 69.67 (21.55) | 56.33 (8.39) | 67.33 (17.23) |
| FVC, mL, mean (SD) | 2.88 (0.45) | 2.77 (0.82) | 2.49 (0.23) | 2.75 (0.52) |
| Dlco, % predicted, mean (SD) | 69.67 (21.78) | 44.33 (4.62) | 45.33 (11.24) | 53.11 (17.60) |
| 6-MWT, meters, mean (SD) | 415 (58.66) | 493 (48.77) | 340 (186.35) | 416 (120.52) |
| Baseline supplemental O2, No. (%) | 0 (0) | 1 (33.3) | 2 (66.7) | 3 (33.3) |
Eleven patients were enrolled in the study, but 2 patients withdrew before treatment. A total of 9 patients (3 per cohort) received treatment, and 7 patients completed the study (Fig 1). Two patients in cohort 3 died before study completion, 1 at 10 weeks and 3 days postinfusion and the other died at 29 weeks and 6 days postinfusion (Table 4). Reported results are made on the basis of the modified intention-to-treat set, which includes all 9 patients that received treatment.
Table 4.
Modified Intention-to-Treat Set
| Subject Status | Cohort 1 2 × 107 hMSCs/Infusion |
Cohort 2 1 × 108 hMSCs/Infusion |
Cohort 3 2 × 108 hMSCs/Infusion |
Total, No. (%) |
|---|---|---|---|---|
| Started, No. (%) | 3 (100) | 3 (100) | 3 (100) | 9 (100) |
| Completed, No. (%) | 3 (100) | 3 (100) | 1 (33.3) | 7 (78) |
| Not completed, No. (%) | 0 (0) | 0 (0) | 2 (66.7) | 2 (22) |
Data are No. of participants (%). Modified intention-to-treat set = participants treated with hMSCs, regardless of study completion. See Table 1 legend for expansion of abbreviations.
Table 5 summarizes patients’ respiratory and hemodynamic parameters at baseline, during treatment, and at 2 hours postinfusion. None of the participants experienced clinically significant changes in any of these parameters and all patients received the full treatment dose.
Table 5.
Respiratory and Hemodynamic Parameters at Baseline and After hMSC Infusion
| Subject ID | 2 h Before Infusion (Baseline) |
Start/During Infusion |
2 h After Infusion |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR (beats/min) | MAP (mm Hg) | SpO2 (%) | HR (beats/min) | MAP (mm Hg) | SpO2 (%) | HR (beats/min) | MAP (mm Hg) | SpO2 (%) | |
| 001 | 69 | 120/73 | 95 | 76 | 121/70 | 96 | 79 | 115/74 | 96 |
| 002 | 67 | 116/71 | 97 | 75 | 108/63 | 95 | 74 | 115/60 | 97 |
| 003 | 65 | 158/68 | 99 | 63 | 150/49 | 99 | 68 | 134/55 | 98 |
| 004 | 54 | 132/61 | 98 | 56 | 120/68 | 100 | 62 | 129/72 | 99 |
| 005 | 54 | 153/83 | 97 | 58 | 162/77 | 98 | 56 | 154/76 | 94 |
| 006 | 70 | 152/72 | 99 | 65 | 148/82 | 100 | 67 | 130/80 | 99 |
| 007 | 61 | 127/63 | 94 | 58 | 137/58 | 94 | 58 | 140/55 | 95 |
| 010 | 61 | 158/76 | 97 | 60 | 165/74 | 98 | 66 | 155/74 | 96 |
| 011 | 56 | 139/78 | 98 | 57 | 126/71 | 98 | 61 | 97/49 | 95 |
HR = heart rate; MAP = mean arterial pressure; SpO2 = peripheral capillary oxygen saturation.
A total of 21 adverse events occurred in 7 patients in the modified intention-to-treat set (Table 6). The most frequently recorded adverse events included bronchitis (3 patients) and common cold (2 patients). Of the 21 adverse events recorded, only 1 (generalized anxiety disorder in patient 007 that began at 8 weeks postinfusion) was classified as possibly related to the study intervention (grade 3; MedDRA). No probable (grade 4; MedDRA) or definite (grade 5; MedDRA) adverse events were reported.
Table 6.
Adverse Events: Pooled Data From the AETHER Trial
| Adverse Events | Cohort 1 (n = 3) 2 × 107 hMSCs/Infusion |
Cohort 2 (n = 3) 1 × 108 hMSCs/Infusion |
Cohort 3 (n = 3) 2 × 108 hMSCs/Infusion |
Total, No. (%) |
|---|---|---|---|---|
| Treatment-emergent adverse events | 0 | 0 | 0 | 0 |
| Any adverse events | 3 | 1 | 3 | 7 (78) |
| Most frequent adverse eventsa | ||||
| Bronchitis | 3 | 0 | 0 | 3 (33) |
| Common cold | 1 | 0 | 1 | 2 (22) |
| Less frequent adverse events | ||||
| Sinusitis | 1 | 0 | 0 | 1 (11) |
| Squamous cell carcinoma | 1 | 0 | 0 | 1 (11) |
| Worsening hypoxia | 0 | 0 | 1 | 1 (11) |
| Dyspnea | 0 | 0 | 1 | 1 (11) |
| Increased cough | 0 | 0 | 1 | 1 (11) |
| Mild sore throat | 1 | 0 | 0 | 1 (11) |
| Rhinitis | 0 | 0 | 1 | 1 (11) |
| Body aches | 0 | 0 | 1 | 1 (11) |
| Leg swelling | 1 | 0 | 0 | 1 (11) |
| Prostatitis | 0 | 0 | 1 | 1 (11) |
| Generalized anxiety disorderb | 0 | 0 | 1 | 1 (11) |
| Serious adverse event(s) | ||||
| Respiratory failure | 0 | 0 | 1 | 1 (11) |
| Progression of idiopathic pulmonary fibrosisc | 0 | 0 | 2 | 1 (22) |
| Fatal adverse event(s) | 0 | 0 | 2 | 2 (22) |
See Table 1 legend for expansion of abbreviations.
Adverse events reported by more than one patient in the study.
Adverse event possibly related to the study.
Corresponds to MedDRA term “IPF,” which includes disease worsening and exacerbations of IPF.
There were no instances of treatment-emergent adverse events. No events of worsened dyspnea or acute exacerbation were reported within 30 days of treatment. One patient experienced worsened dyspnea at 4 weeks and 5 days postinfusion (patient 007), and the same patient experienced an acute exacerbation at 7 weeks and 3 days postinfusion.
Three serious adverse events (2 instances of death [patients 007 and 010] and 1 instance of respiratory failure [patient 007]) occurred in cohort 3. Patient 007 experienced an acute exacerbation and subsequent respiratory failure resulting in death at 10 weeks and 3 days postinfusion. Patient 010 experienced progression of IPF (defined as disease worsening according to MedDRA), resulting in death at 29 weeks and 6 days postinfusion. None of these serious adverse events was determined to be treatment-related.
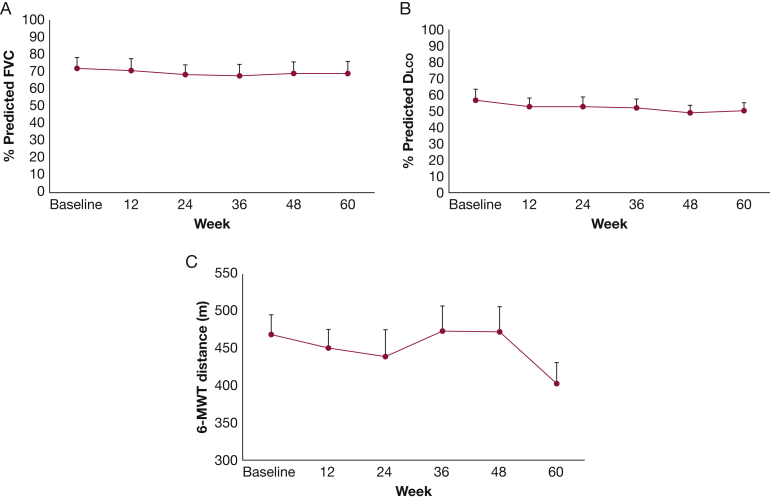
Table 7 shows the progression of lung function parameters over the course of the study. Data for participants 007 and 010 are not available beyond week 4. Figure 2 shows progression of select respiratory parameters up to 60 weeks postinfusion. Data combined for all cohorts (n = 7) demonstrated a mean absolute decline in % predicted FVC of 3.0% and a 5.4% decline in % predicted Dlco. Overall, 6-MWT improved by 36 weeks postinfusion (+1% improvement from baseline), and declined to -4.4% from baseline by week 60 (Fig 2). These data are considered exploratory because the study was not powered for efficacy analyses and lacked a placebo-control arm.
Table 7.
Progression of Lung Function Parameters
| Subject ID |
Baseline |
Week 12 |
Week 24 |
Week 36 |
Week 48 |
Week 60 |
|---|---|---|---|---|---|---|
| TLC, L, Mean | ||||||
| 001 | 3.60 | 3.21 | 3.90 | 3.12 | 3.16 | 3.12 |
| 002 | 4.08 | 4.59 | 4.04 | 4.63 | 4.76 | 4.80 |
| 003 | 4.78 | 5.08 | 4.07 | 4.39 | 4.39 | 3.34 |
| 004 | 5.79 | 4.39 | 4.97 | 4.50 | 5.81 | 5.62 |
| 005 | 3.85 | 3.66 | 3.53 | 4.45 | 4.17 | 4.39 |
| 006 | 3.54 | 3.47 | 3.31 | 3.62 | 4.29 | 4.52 |
| 007 | 3.73 | N/A | N/A | N/A | N/A | N/A |
| 010 | 4.14 | N/A | N/A | N/A | N/A | N/A |
| 011 | 3.91 | 4.09 | 4.25 | 4.18 | 4.67 | 4.85 |
| FVC, L, Mean | ||||||
|---|---|---|---|---|---|---|
| 001 | 2.48 | 2.14 | 2.56 | 2.20 | 2.26 | 1.95 |
| 002 | 3.38 | 3.64 | 2.98 | 3.39 | 3.34 | 3.34 |
| 003 | 2.91 | 2.85 | 2.92 | 2.65 | 2.69 | 2.83 |
| 004 | 3.76 | 3.50 | 3.67 | 3.62 | 3.75 | 3.61 |
| 005 | 2.18 | 2.20 | 2.17 | 2.05 | 2.07 | 2.03 |
| 006 | 2.58 | 2.62 | 2.4 | 2.54 | 2.42 | 2.48 |
| 007 | 2.25 | N/A | N/A | N/A | N/A | N/A |
| 010 | 2.51 | N/A | N/A | N/A | N/A | N/A |
| 011 | 2.70 | 2.76 | 2.50 | 2.47 | 2.75 | 2.94 |
| Dlco, % Predicted, Mean | ||||||
|---|---|---|---|---|---|---|
| 001 | 63 | 50 | 50 | 52 | 46 | 45 |
| 002 | 52 | 50 | 44 | 46 | 40 | 43 |
| 003 | 94 | 79 | 84 | 80 | 72 | 79 |
| 004 | 47 | 42 | 49 | 50 | 47 | 46 |
| 005 | 47 | 44 | 51 | 44 | 39 | 45 |
| 006 | 39 | 41 | 33 | 33 | 41 | 43 |
| 007 | 48 | N/A | N/A | N/A | N/A | N/A |
| 010 | 33 | N/A | N/A | N/A | N/A | N/A |
| 011 | 55 | 63 | 58 | 58 | 58 | 51 |
| 6-MWT, meters, Mean | ||||||
|---|---|---|---|---|---|---|
| 001 | 471 | 460 | 417 | 540 | 450 | 360 |
| 002 | 420 | 402 | 270 | 315 | 381 | 300 |
| 003 | 354 | 393 | 405 | 465 | 420 | 366 |
| 004 | 531 | 423 | 495 | 540 | 560 | 486 |
| 005 | 510 | 540 | 540 | 525 | 432 | 393 |
| 006 | 438 | 396 | 405 | 390 | 432 | 405 |
| 007 | 225 | N/A | N/A | N/A | N/A | N/A |
| 010 | 240 | N/A | N/A | N/A | N/A | N/A |
| 011 | 555 | 540 | 540 | 537 | 630 | 510 |
N/A = not applicable. See Table 2 legend for expansion of other abbreviations.
Figure 2.
Secondary efficacy outcomes during the 60-week study period. A, Changes in mean % predicted FVC for overall study period. B, Changes in % predicted diffusing capacity of the lungs for carbon monoxide (Dlco). C, Changes in 6-min walk test (6-MWT) distance. N = 7 for all data.
Discussion
AETHER was the first clinical trial conducted over 60 weeks to support the safety of a single IV infusion of bone marrow–derived hMSCs in patients with IPF. All study objectives followed the recommendations of the FDA and the American Thoracic Society.1
AETHER trial met its primary end point of safety, showing that the administration of hMSCs is safe in patients with IPF up to 2 × 108 cells/infusion. The intervention was well-tolerated in all patients and there were no treatment-emergent serious adverse events reported. A majority of patients (78%) experienced treatment unrelated adverse events including, but not limited to, bronchitis, common cold, and sinusitis (Table 7), which one might expect given the long duration of the study and the characteristics of the population being studied.
There were 2 events of nonstudy-related death from disease progression and acute exacerbation of IPF. As expected in IPF, those enrolled in the AETHER trial had variable rates of disease progression. Although the clinical course of this disease is unpredictable, the natural history is typically one of steady decline of lung function punctuated by acute exacerbations. Baseline lung function parameters suggest that patients in cohort 3 had significantly more advanced disease than patients in cohorts 1 and 2. The 2 subjects who died were both in cohort 3 and had the lowest baseline FVC values and 6-MWT distances. One of the 2 patients also had the lowest baseline Dlco overall. In light of a presumed 1-year mortality risk of approximately 20% in patients with moderately advanced disease,27 the observed death of 2 of 9 subjects was not unexpected. Prior trials using intravenously delivered MSCs, primarily in the cardiovascular literature, have not shown increased mortality related to MSC treatment.16, 24 Additionally, although concerns that MSCs may contribute to lung fibrosis have been raised in the past,28, 29, 30, 31 there are no preclinical or human studies that have demonstrated this relationship.
Secondary end points were exploratory and related to disease progression. On the basis of Consensus Statement guidelines for patients with IPF, a decline in the absolute FVC ≥10% or ≥15% in the absolute Dlco over 3 to 6 months represents progression of disease.1, 32 As with other phase 1 trials of cell-based therapies for IPF, we noted substantial inter- and intra-subject variability in the direction and magnitude of change of lung function parameters.19, 21 The average absolute decline in % predicted FVC and Dlco by the end of this study were below the previously mentioned thresholds for IPF disease progression. However, this small phase I study was designed to evaluate safety and was not powered to detect significant changes in lung function. Although encouraging, these data are preliminary and should not be interpreted as proof of efficacy of hMSCs in IPF disease progression.
Results from the ASCEND (A Randomized, Double-Blind, Placebo Controlled, Phase 3 Study of the Efficacy and Safety of Pirfenidone in Patients With Idiopathic Pulmonary Fibrosis) trial of pirfenidone for the treatment of IPF suggest that the use of supplemental oxygen and FVC at baseline significantly correlates with rate of disease progression.5 In the ASCEND trial, subjects who required supplemental oxygen experienced a higher rate of disease progression, whereas those with a higher baseline FVC experienced a lower rate of disease progression. In line with these findings, 3 subjects in the AETHER trial used supplemental oxygen at baseline and 2 died during the course of the study.
Results from the ASCEND trial also suggest that baseline body weight is correlated with a decreased rate of disease progression in treated subjects weighing up to approximately 85 kg (187.5 lb). For patients with body weights greater than 85 kg, disease progression was found to be similar in both the treatment and placebo groups. The average body weight of subjects in the AETHER study was 86.36 (±8.34) kg; only 4 of 9 subjects weighed less than 85 kg at baseline. Both patients who died during the study weighed more than 85 kg. AETHER did not analyze disease progression in relation to body weight; however, future trials could aim to enroll subjects with similar baseline body mass index to ensure a uniform weight-based dose of hMSCs. An alternative approach could be to dose patients by body weight as in previous hMSC trials.16, 17, 18, 19, 20, 23
In agreement with other studies of IPF patients treated with cell therapies, the data support the safety of a single IV administration of hMSCs up to 2 × 108 cells/infusion for the treatment of IPF.19, 21 Limitations of the current study include its small sample size, lack of randomization, and lack of a placebo arm. Current safety findings support the role of more extensive studies of the safety and efficacy of hMSCs in the treatment of IPF. Before larger randomized placebo-controlled studies are done to evaluate efficacy, further safety studies should be conducted with larger numbers of patients as well as patients with more advanced IPF. One challenge will be to establish the optimal number of infusions and the appropriate dosing interval. Another challenge will be to identify early stage patients most likely to benefit from the intervention. Ultimately, well-designed and meticulously conducted phase II/III clinical trials of hMSCs for the treatment of IPF will be required to evaluate their efficacy as a potential therapeutic modality for this devastating disease.
Acknowledgments
Author contributions: Study conception: M. K. G., R. L. T., and J. M. H. Study design and coordination: D. D., A. K., M. V. P., S. S., V. F. L., L. H. L., G. D. R., J. F., E. S. S., A. M., and Y. N. M. Data analysis and reporting: M. K. G., R. L. T., and J. M. Manuscript preparation: M. K. G., J. M., R. L. T., and G. A. R. Critical revision of manuscript for important intellectual content: all authors read and approved final manuscript. M. K. G. had full access to all of the data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: M. K. G. is participating in a role of an investigator at industry-sponsored clinical trials for Genentech, Boehringer Ingelheim, Bayer, and Biogen and serves as a consultant expert for Genentech and Boehringer Ingelheim. L. H. L. served as an investigator for Boehringer Ingelheim, Genentech, Global Blood Therapeutics, Celgene, Roche, and Veracyte and has served on advisory boards for Genentech and Boehringer Ingelheim. Y. N. M. has served on the speakers bureau for Boehringer Ingelheim. None declared (J. M., R. L. T., E. S. S., G. A. R., D. D.; S. S., A. K., M. V. P., V. F. L., G. D. R., J. F., A. M., J. M. H.).
Role of sponsor: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: We thank the Lester and Sue Smith Foundation for funding the AETHER trial and ongoing support; Kevin Anstrom, PhD, for reviewing the data; Jose Da Silva, PhD, for providing input for the conduction of the trial; and study coordinators Julio Sierra, MD, and Cindy Delgado, MA, who coordinated subject visits.
Footnotes
FUNDING/SUPPORT: Financial support for the AETHER trial came from the Lester and Sue Smith Foundation.
References
- 1.Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Resp Crit Care Med.183(6):788-824. [DOI] [PMC free article] [PubMed]
- 2.Travis W.D., Hunninghake G., King T.E., Jr. Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project. Am J Resp Crit Care Med. 2008;177(12):1338–1347. doi: 10.1164/rccm.200611-1685OC. [DOI] [PubMed] [Google Scholar]
- 3.Nishimura K., Kitaichi M., Izumi T., Nagai S., Kanaoka M., Itoh H. Usual interstitial pneumonia: histologic correlation with high-resolution CT. Radiology. 1992;182(2):337–342. doi: 10.1148/radiology.182.2.1732946. [DOI] [PubMed] [Google Scholar]
- 4.Johkoh T., Muller N.L., Cartier Y. Idiopathic interstitial pneumonias: diagnostic accuracy of thin-section CT in 129 patients. Radiology. 1999;211(2):555–560. doi: 10.1148/radiology.211.2.r99ma01555. [DOI] [PubMed] [Google Scholar]
- 5.King T.E., Jr., Bradford W.Z., Castro-Bernardini S. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2083–2092. doi: 10.1056/NEJMoa1402582. [DOI] [PubMed] [Google Scholar]
- 6.Richeldi L., Cottin V., du Bois R.M. Nintedanib in patients with idiopathic pulmonary fibrosis: Combined evidence from the TOMORROW and INPULSIS((R)) trials. Res Med. 2016;113:74–79. doi: 10.1016/j.rmed.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Moodley Y., Atienza D., Manuelpillai U. Human umbilical cord mesenchymal stem cells reduce fibrosis of bleomycin-induced lung injury. Am J Pathol. 2009;175(1):303–313. doi: 10.2353/ajpath.2009.080629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rojas M., Xu J., Woods C.R. Bone marrow-derived mesenchymal stem cells in repair of the injured lung. Am J Resp Cell Mol Bio. 2005;33(2):145–152. doi: 10.1165/rcmb.2004-0330OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tashiro J., Elliot S.J., Gerth D.J. Therapeutic benefits of young, but not old, adipose-derived mesenchymal stem cells in a chronic mouse model of bleomycin-induced pulmonary fibrosis. Transl Res. 2015;166(6):554–567. doi: 10.1016/j.trsl.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ortiz L.A., Gambelli F., McBride C. Mesenchymal stem cell engraftment in lung is enhanced in response to bleomycin exposure and ameliorates its fibrotic effects. Proc Natl Acad Sci U S A. 2003;100(14):8407–8411. doi: 10.1073/pnas.1432929100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ishizawa K., Kubo H., Yamada M. Bone marrow-derived cells contribute to lung regeneration after elastase-induced pulmonary emphysema. FEBS Lett. 2004;556(1-3):249–252. doi: 10.1016/s0014-5793(03)01399-1. [DOI] [PubMed] [Google Scholar]
- 12.Spees J.L., Pociask D.A., Sullivan D.E. Engraftment of bone marrow progenitor cells in a rat model of asbestos-induced pulmonary fibrosis. Am J Resp Crit Care Med. 2007;176(4):385–394. doi: 10.1164/rccm.200607-1004OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spees J.L., Whitney M.J., Sullivan D.E. Bone marrow progenitor cells contribute to repair and remodeling of the lung and heart in a rat model of progressive pulmonary hypertension. FASEB J. 2008;22(4):1226–1236. doi: 10.1096/fj.07-8076com. [DOI] [PubMed] [Google Scholar]
- 14.Bonfield T.L., Koloze M., Lennon D.P., Zuchowski B., Yang S.E., Caplan A.I. Human mesenchymal stem cells suppress chronic airway inflammation in the murine ovalbumin asthma model. Am J Physiol. 2010;299(6):L760–L770. doi: 10.1152/ajplung.00182.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee J.W., Fang X., Gupta N., Serikov V., Matthay M.A. Allogeneic human mesenchymal stem cells for treatment of E. coli endotoxin-induced acute lung injury in the ex vivo perfused human lung. Proc Natl Acad Sci U S A. 2009;106(38):16357–16362. doi: 10.1073/pnas.0907996106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hare J.M., Traverse J.H., Henry T.D. A randomized, double-blind, placebo-controlled, dose-escalation study of intravenous adult human mesenchymal stem cells (prochymal) after acute myocardial infarction. J Am Coll Cardiol. 2009;54(24):2277–2286. doi: 10.1016/j.jacc.2009.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liang J., Zhang H., Hua B. Allogenic mesenchymal stem cells transplantation in refractory systemic lupus erythematosus: a pilot clinical study. Ann Rheum Dis. 2010;69(8):1423–1429. doi: 10.1136/ard.2009.123463. [DOI] [PubMed] [Google Scholar]
- 18.Hare J.M., Fishman J.E., Gerstenblith G. Comparison of allogeneic vs autologous bone marrow-derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. JAMA. 2012;308(22):2369–2379. doi: 10.1001/jama.2012.25321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chambers D.C., Enever D., Ilic N. A phase 1b study of placenta-derived mesenchymal stromal cells in patients with idiopathic pulmonary fibrosis. Respirology. 2014;19(7):1013–1018. doi: 10.1111/resp.12343. [DOI] [PubMed] [Google Scholar]
- 20.Le Blanc K., Frassoni F., Ball L. Mesenchymal stem cells for treatment of steroid-resistant, severe, acute graft-versus-host disease: a phase II study. Lancet. 2008;371(9624):1579–1586. doi: 10.1016/S0140-6736(08)60690-X. [DOI] [PubMed] [Google Scholar]
- 21.Tzouvelekis A., Paspaliaris V., Koliakos G. A prospective, non-randomized, no placebo-controlled, phase Ib clinical trial to study the safety of the adipose derived stromal cells-stromal vascular fraction in idiopathic pulmonary fibrosis. J Transl Med. 2013;11:171. doi: 10.1186/1479-5876-11-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weiss D.J., Casaburi R., Flannery R., LeRoux-Williams M., Tashkin D.P. A placebo-controlled, randomized trial of mesenchymal stem cells in COPD. Chest. 2013;143(6):1590–1598. doi: 10.1378/chest.12-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilson J.G., Liu K.D., Zhuo H. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet. 2015;3(1):24–32. doi: 10.1016/S2213-2600(14)70291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heldman A.W., DiFede D.L., Fishman J.E. Transendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy: the TAC-HFT randomized trial. JAMA. 2014;311(1):62–73. doi: 10.1001/jama.2013.282909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Golpanian S., DiFede D.L., Pujol M.V. Rationale and design of the allogeneiC human mesenchymal stem cells (hMSC) in patients with aging fRAilTy via intravenoUS delivery (CRATUS) study: a phase I/II, randomized, blinded and placebo controlled trial to evaluate the safety and potential efficacy of allogeneic human mesenchymal stem cell infusion in patients with aging frailty. Oncotarget. 2016;7(11):11899–11912. doi: 10.18632/oncotarget.7727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trachtenberg B., Velazquez D.L., Williams A.R. Rationale and design of the Transendocardial Injection of Autologous Human Cells (bone marrow or mesenchymal) in Chronic Ischemic Left Ventricular Dysfunction and Heart Failure Secondary to Myocardial Infarction (TAC-HFT) trial: a randomized, double-blind, placebo-controlled study of safety and efficacy. Am Heart J. 2011;161(3):487–493. doi: 10.1016/j.ahj.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 27.Ley B., Bradford W.Z., Weycker D., Vittinghoff E., du Bois R.M., Collard H.R. Unified baseline and longitudinal mortality prediction in idiopathic pulmonary fibrosis. Eur Resp J. 2015;45(5):1374–1381. doi: 10.1183/09031936.00146314. [DOI] [PubMed] [Google Scholar]
- 28.Lama V.N., Phan S.H. The extrapulmonary origin of fibroblasts: stem/progenitor cells and beyond. Proc Am Thorac Soc. 2006;3(4):373–376. doi: 10.1513/pats.200512-133TK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phillips R.J., Burdick M.D., Hong K. Circulating fibrocytes traffic to the lungs in response to CXCL12 and mediate fibrosis. J Clin Invest. 2004;114(3):438–446. doi: 10.1172/JCI20997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salazar K.D., Lankford S.M., Brody A.R. Mesenchymal stem cells produce Wnt isoforms and TGF-beta1 that mediate proliferation and procollagen expression by lung fibroblasts. Am J Physiol. 2009;297(5):L1002–L1011. doi: 10.1152/ajplung.90347.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hashimoto N., Jin H., Liu T., Chensue S.W., Phan S.H. Bone marrow-derived progenitor cells in pulmonary fibrosis. J Clin Invest. 2004;113(2):243–252. doi: 10.1172/JCI18847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raghu G., Collard H.R., Anstrom K.J. Idiopathic pulmonary fibrosis: clinically meaningful primary endpoints in phase 3 clinical trials. Am J Resp Crit Care Med. 2012;185(10):1044–1048. doi: 10.1164/rccm.201201-0006PP. [DOI] [PMC free article] [PubMed] [Google Scholar]