Abstract
Background
Increased depression, hearing loss, dementia, alcoholism, and mortality in essential tremor patients remain unexplained. We investigated whether conditions associated with tremor are linked to chronic stress.
Methods
The FY2013 Veterans Affairs database was queried for 38 selected dual diagnosis combinations in 5,854,223 veterans aged 21–95 years.
Results
Post-traumatic stress disorder, anxiety, and depression were the most common psychiatric diagnoses in tremor patients, with the odds ratio exceeding 2 in all 15-year cohorts. Depending on age, patients with essential tremor were more likely than those without to have obsessive–compulsive disorder, bipolar illness, schizophrenia, use tobacco and abuse alcohol, have hypertension, obesity, hyperlipidemia, diabetes, vitamin D deficiency, coronary and cerebrovascular diseases, congestive heart failure, stroke, asthma, hypothyroidism, irritable bowel syndrome, renal insufficiency, alcoholic liver disease, hearing loss, glaucoma, macular degeneration, migraine, epilepsy, idiopathic polyneuropathy, history of head trauma, and ‘Alzheimer’s dementia. In contrast, lung and colorectal cancer, amyotrophic lateral sclerosis, psychostimulant abuse, and rheumatoid arthritis were not more common.
Discussion
Post-traumatic stress disorder, anxiety, and depression, strongly associated with essential tremor, are known risk factors for poor health habits, tobacco use and alcohol abuse; collectively these are risk factors for vascular disease, with further negative health consequences for multiple organ systems. As essential tremor is associated with all these conditions, we propose that chronic stress is not only responsible for the conditions associated with tremor but in some cases itself directly and indirectly induces essential tremor, so that tremor and poor health share a common cause.
Keywords: Essential tremor, affective disorders, epidemiology, personality disorder, drug abuse
Introduction
The cause(s) of essential tremor (ET) remains poorly understood. Observers agree that persons with ET are prone to anxiety and depression; however, the reason for this is not clear.1 Furthermore, the greater rate of hearing loss,2 dementia,3 and mortality in ET remains unexplained.4
We have noted an association of ET not only with depression and anxiety but also with post-traumatic stress disorder (PTSD), all of which are causes of chronic stress. We thus asked whether conditions known to be associated with chronic stress are also more common in persons with ET. If so, poor health features of ET may be interpreted as constituting part of a larger pattern that arises ultimately from stress/distress. To address this notion, we queried the United States Veterans Affairs (VA) database to ascertain whether the frequency of various conditions was altered in ET veteran patients compared to those without ET.
Methods
The Veterans Health Administration has utilized an electronic medical record system since the 1990s. Providers entered diagnostic International Classification of Diseases (ICD)-9 codes at the time of each outpatient encounter. For inpatient encounters, trained coders reviewed electronic records and assigned diagnostic codes. All encounter information from VA medical centers and clinics across the United States was relayed regularly to a central database in Austin, TX.
The Austin National Inpatient and Outpatient Workload files were queried for patients with selected dual diagnoses combinations seen during fiscal year 2013 (FY13): from October 1, 2012, to September 30, 2013. The presence of specific conditions in patients with or without the diagnostic code for ET, 333.1, was assessed. Over 108 million outpatient encounters for 5,870,023 unique outpatients were queried. Another file was created for 508,939 unique inpatients, and merged with the outpatient file.
We examined 38 clinical conditions. Data were generated in 15-year age cohorts, and represent both men and women except for prostate cancer. Conditions of chronic stress (PTSD, depression, and anxiety), along with common psychiatric disorders were initially examined. With the finding of strong associations of ET with chronic stress conditions, we then examined substance abuse disorders and components of the metabolic syndrome and poor diet for association with ET, as these are known to be more common in chronic stress disorders. As vascular disease is more common in persons with chronic stress, smoking and alcohol use, and with components of the metabolic syndrome, we then examined whether cardiovascular and cerebrovascular disease is more common in persons with ET. Next, we examined various medical and neurological diseases based on known associations with chronic stress, substance abuse, metabolic syndrome, vascular risk factors, or based on prior literature suggesting an association with ET.
To assess the accuracy of the diagnostic code 333.1 for ET, we examined the medical records of all 355 patients who were diagnosed with 333.1 in FY13 in the VA Greater Los Angeles Healthcare System who were aged 21–95 years at that time. Records were examined not only for FY13 but for prior and subsequent years.
Statistical analysis
Very small numbers of veterans below the age of 21 and over the age of 95 years were available and therefore were excluded from analyses, so that data from 5,854,223 were analyzed. Calculation of p values utilized a two-tailed chi-square test. Any statement that the odds ratio (OR) for a specific condition is higher or lower in tremor patients than in non-tremor cases is made only if the corresponding chi-square test has shown significance, with p < 0.00026, after a Bonferroni correction that takes into account 190 tests (38 conditions × five age cohorts). In the figures, only statistically significant ORs are displayed.
Results
VA Greater Los Angeles FY13 case review
The VA Greater Los Angeles Healthcare System serves veterans living in urban and rural areas within southern California. Electronic medical records spanned over 20 years, making it possible, for example, to ascertain from early records whether tremor onset antedated the use of a tremor-inducing medication, while more recent records permitted determination whether the FY13 diagnosis was retrospectively incorrect. Five charts were rejected for having no information on the patient’s tremor. Of the remaining 350 diagnosed with 333.1 in FY13, the diagnosis of ET was incorrect due to Parkinson’s in 22 (6.3%), drug-induced tremor in nine (2.6%), atypical tremor, usually head or writing tremor, in eight (2.3%), physiological tremor in five (1.3%), and other, such as dystonia, psychogenic, or due to alcohol or trauma, in 14 (4.0%). Of 292 judged on chart review to have classic ET (83.4%), 12 had recent-onset parkinsonism preceded by ET.
National VA database
The percentage of veteran patients diagnosed with ET in the nationwide survey at ages 21–35, 36–50, 51–65, 66–80, and 81–95 years was 0.07% (437/586,169), 0.17% (1,348/783,127), 0.49% (9,523/1,961,836), 0.77% (13,425/1,751,046), and 0.75% (5,792/772,045), respectively.
Psychiatric disorders
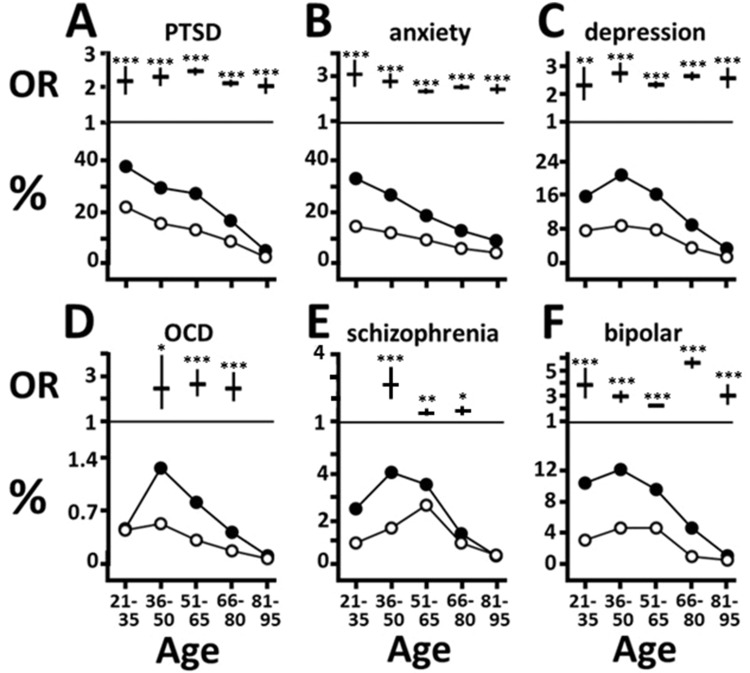
PTSD and anxiety were the two most common psychiatric disorders among veterans with tremor. The PTSD OR was doubled at all ages, being present in 38% of 21–35-year-olds, falling to 27% at 51–65, and <10% above age 80 (Figure 1A). At all ages ET patients had at least doubled OR for anxiety, as high as 33% at ages 21–35, and falling to <10% at ages 81–95 years (Figure 1B). The OR for depression was also doubled in ET patients, with a peak of 20.8% at ages 36–50 and falling to <10% above age 65 (Figure 1C). The high association of ET with anxiety and depression confirms literature reports,1,5 to which PTSD can now be added.
Figure 1. Frequency of Psychiatric Disorders in Veterans with and without Essential Tremor. In this and the next four figures, the lower part of each panel displays the percentages of veteran patients with (closed circles) or without (open circles) tremor who have the comorbid condition within 15-year cohorts from age 21 to 95. The upper part of each panel displays the age-corresponding odds ration with 95% confidence intervals, shown only if statistically significant (two-tailed chi-square test). *p < 0.00026; **p < 1 × 10−7; ***p < 1 × 10−10.
Because PTSD has been associated with obsessive–compulsive disorder (OCD)6,7 and bipolar disorder,8,9 and stress with schizophrenia,10 we examined these. ET veterans did not have OCD more often than non-ET cases at ages 21–35 or 81–95, but did at ages in between, with OR above 2.4. OCD was uncommon, present in 1.3% of ET cases at 36–50 years, falling to 0.4% at ages 66–80 (Figure 1D). Schizophrenia was increased in ET patients, especially at ages 36–50, with OR = 2.6, falling to 1.4 at ages 51–80; the prevalence was 4.2% at ages 36–50 (Figure 1E). ET patients were more likely to have bipolar disorder across all ages, with the OR ranging between 2.2 and 5.6, and a prevalence of 12% at 36–50 years, falling to <5% after age 65 (Figure 1F).
Substance dependency/abuse
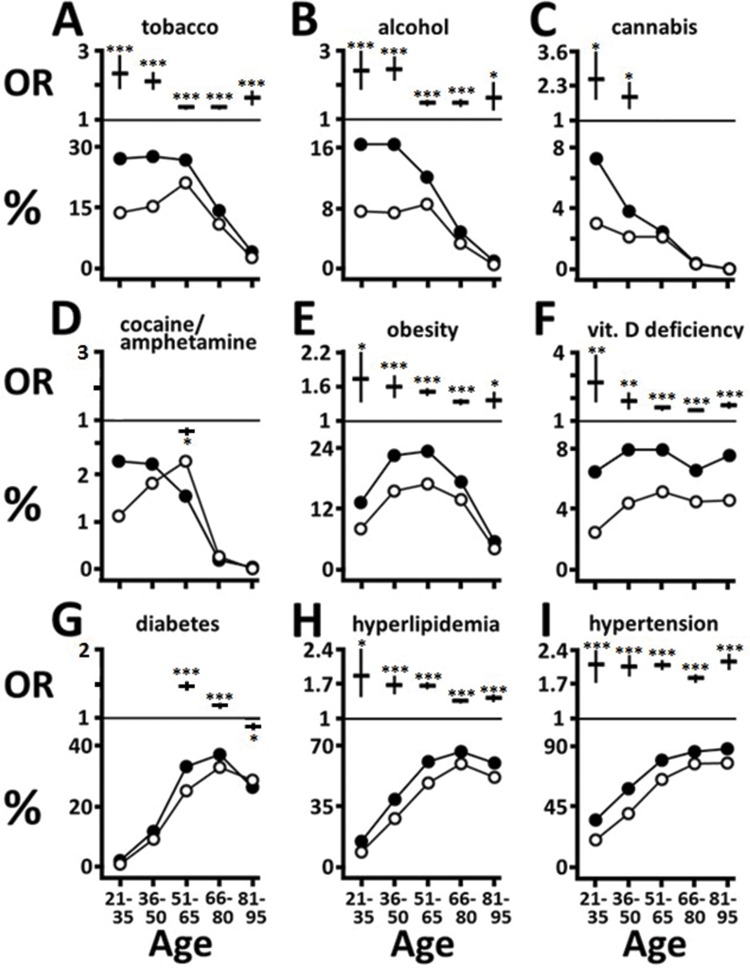
As chronic stress is a well-established risk factor for substance abuse,11–14 we examined this feature next. The OR for tobacco abuse among ET patients was elevated at all ages, especially for 21–50-year-olds at 2.1–2.3, falling to 1.4 at ages 51–80 (Figure 2A). Across ages 21 to 65, 27-28% of ET cases smoked. Alcohol dependency/abuse in tremor patients was increased at all ages, with OR of 2.4–2.5 at ages 21–50, falling to 1.5 at 51–80, with a prevalence of 16% at ages 21–50, falling below 10% only after age 65 (Figure 2B). Cannabis use/abuse in ET was most marked at ages 21–35 (OR = 2.5), but fell thereafter, and was not increased after age 50 (Figure 2C). In contrast, the abuse of psychostimulant drugs (cocaine, amphetamine) differed only at ages 51–65, when it was below non-ET rates (OR = 0.67, confidence interval [CI] 0.57–0.79, p = 0.000002), when only 1.6% of ET patients used them (Figure 2D). These results indicate that among the substance abuse disorders, tobacco and alcohol abuse are especially more common in ET cases.
Figure 2. Substance Abuse (A–D) and Components of the Metabolic Syndrome and Diet (E–I). See Figure 1 for description of veterans with and without tremor.
Components of the metabolic syndrome and diet
PTSD, anxiety, and depression are known risk factors for the metabolic syndrome,15–19 thus we examined whether ET is associated with components of this syndrome. Obesity was more common in ET, with OR ranging from 1.7 at ages 21–35 to 1.3 at ages 81–95, and prevalence ranging from 13% at ages 21–35 to 23% at ages 36-65 (Figure 2E). Vitamin D deficiency, as a marker of poor diet/exercise, was more common in tremor patients at all ages, with OR of 2.7 at ages 21–35, then between 1.9 and 1.5 at subsequent ages, and with a prevalence ranging between 6.6% and 8.1% (Figure 2F). At ages 51–65 and 66–80, the OR for diabetes was modestly increased (OR = 1.5, 1.2 respectively), with a prevalence of 37% at ages 66–80. At ages 81–95, ET veterans were less likely than non-ET cases to have diabetes (OR = 0.88, CI 0.83-0.94, p = 0.00004, Figure 2G).
Hyperlipidemia was more common in ET patients at all ages, with OR ranging from 1.9 at ages 21–35 to 1.4 at ages 66–95. Over 60% of 51–95-year-olds with ET had hyperlipidemia (Figure 2H). Hypertension was increased in ET with an OR of 2 across ages 21–95, with a percentage of 36% at ages 21–35 and over 85% among those over 65 (Figure 2I). In summary, ET patients were more likely to be obese, have hypertension, hyperlipidemia, and low vitamin D levels at all ages, whereas the association with diabetes was modest and age-limited.
Vascular and respiratory disease
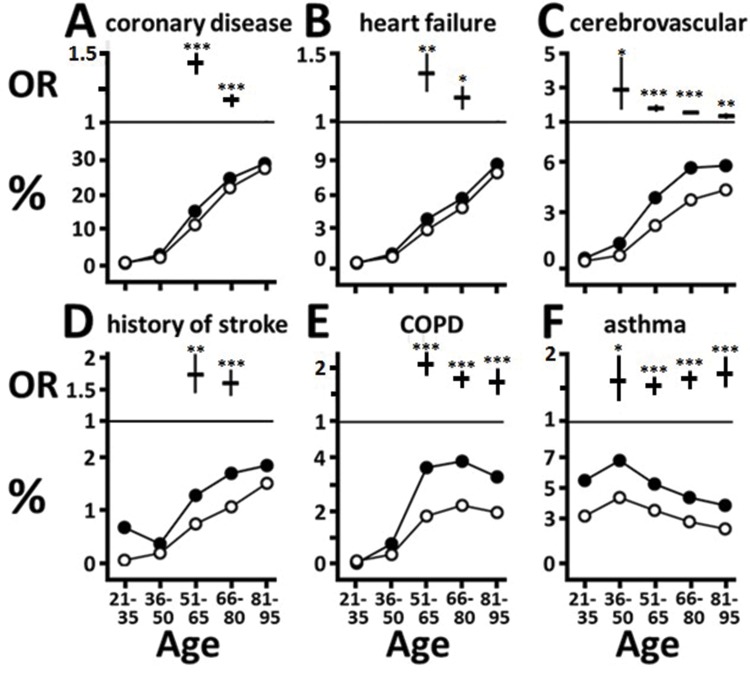
Tobacco and alcohol use, hypertension, and metabolic syndrome components are well known risk factors for vascular disease, while smoking and poor diet are linked to respiratory disease. In addition, persons with chronic stress are more likely to have coronary artery disease (CAD),16,20–22 and are prone to stroke.23 Given these risk factors in ET patients, we examined the prevalence of vascular and respiratory diseases. CAD was modestly more likely in tremor patients only at ages 51–65 and 66–80 (OR = 1.4, 1.2 respectively, Figure 3A). At these ages, tremor patients were modestly more likely to have congestive heart failure (OR = 1.4, 1.2 respectively). Compared with cardiovascular disease, cerebrovascular disease was more markedly increased in tremor patients. It was more common above age 35, with OR = 2.9 at ages 36–50, falling to 1.4 by ages 81–95 (Figure 3C). Residual deficit from prior stroke was more likely at ages 51–65 and 66–80 (OR = 1.7, 1.6 respectively, Figure 3D). At ages 66–80, 5.6% of tremor cases had cerebrovascular disease, 1.7% had residual from stroke, 5.7% had heart failure, and 25% had CAD.
Figure 3. Vascular (A–D) and Respiratory (E–F) Diseases. See Figure 1 for description of veterans with and without tremor.
Above age 50, chronic obstructive pulmonary disease (COPD) was more common in ET, with OR of 2.1 at ages 51–65 (CI 1.85–2.30), falling to 1.7 at ages 81–95 (CI 1.49–1.99), the prevalence ranging between 3.3% and 3.8% at ages 51 to 95 (Figure 3E). Asthma was more common in ET after age 35, with OR ranging from 1.5 to 1.7, and the prevalence between 4% and 7% (Figure 3F).
Numerous facets of health may be affected by chronic stress, tobacco/alcohol abuse, and vascular risk factors, thus we sampled various organ diseases, cancer, and neurological disorders to examine their relative prevalence in ET.
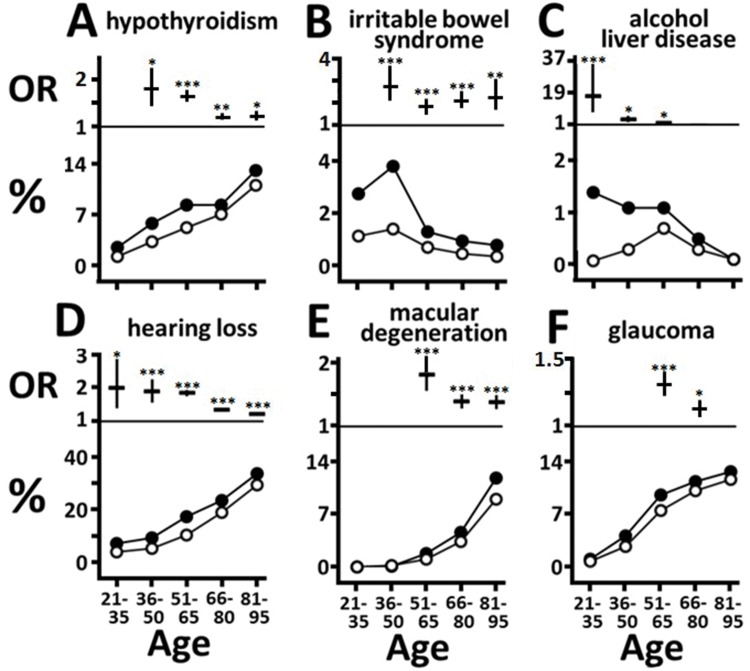
Other medical conditions
Hypothyroidism, linked to smoking,24 was moderately increased in tremor patients at ages 36–65 (OR 1.8–1.6), and modestly over age 65 (OR = 1.2), with the prevalence rising from 5.8% at ages 36–50 to 13% at ages 81–95 (Figure 4A). Although smoking is a risk factor for rheumatoid arthritis,25 this disease was not more common in ET cases (not shown). The OR for irritable bowel syndrome (IBS), a condition strongly linked to chronic stress,26,27 was increased twofold above age 35 in ET, with the prevalence peaking at 3.8% at ages 36–50, and falling to about 1% thereafter (Figure 4B). Renal insufficiency, associated with vascular risk factors,28 was modestly more common among tremor patients aged 51–65 (OR = 1.4, CI 1.29–1.55, p < 1 × 10–10) and 66–80 (OR = 1.2, CI 1.12–1.27, p < 1 × 10–8), with a prevalence of 5.1% to 8.7% at these ages (not shown). Alcoholic liver disease was more common in ET below age 66, with an OR of 16.7 at ages 21–35, falling to 3.4 at ages 36–50 and to 1.5 at 51–65, with the prevalence falling from 1.4% to 1.1% across these ages (Figure 4C).
Figure 4. Other Medical Conditions (A–C) and Diseases of the Ear and Eye (D–F). See Figure 1 for description of veterans with and without tremor.
As cancer rates are influenced by lifestyle factors, we examined three common cancers. Despite higher tobacco use in tremor patients, their rate of lung cancer did not differ from that of non-tremor cases at any age (not shown). Similarly, colorectal cancer rates did not differ (not shown). Prostate cancer was modestly more common among men with tremor only at ages 51–65 (OR = 1.2, CI 1.11–1.39, p = 0.00023), with the condition diagnosed in 3.5% (not shown).
Vascular risk factors are associated with higher rates of hearing loss,29 macular degeneration,30,31 and glaucoma,32 thus the frequency of these conditions was examined in ET cases. Tremor patients were more likely to have sensorineural hearing loss, with OR = 2.0 at ages 21–35 (CI 1.38–2.84, p = 0.00015), falling below 1.8 after age 65, with 7.3% of 21–35, 17% of 51–65, and 34% of 81–95-year-olds having hearing loss (Figure 4D). Macular degeneration was more common in ET after age 50, with OR = 1.8 at ages 51–65 (CI 1.55–2.10), falling to 1.4 at ages 81–95 (CI 1.26–1.48), with a prevalence of 1.8% at 51–65, rising to 12% at ages 81–95 (Figure 4E). At ages 51–65 and 66–80, glaucoma was modestly more common in ET, with OR = 1.3 (CI 1.22–1.40, p < 1 × 10–10) and 1.1 (CI 1.07–1.19, p = 0.00001), with a prevalence of 7.4% and 10% at these ages respectively (Figure 4F).
Neurological disorders
We examined traumatic brain injury (TBI) as it is strongly associated with PTSD,33,34 migraine due to associations with TBI, chronic stress, and smoking,35–38 epilepsy in view of associations with TBI, substance abuse and vascular risk factors,39,40 idiopathic polyneuropathy as it is associated with smoking and vascular risk factors,41,42 and dementia in view of associations with depression and vascular risk factors,43,44 all these risk factors being more common in tremor cases. Amyotrophic lateral sclerosis (ALS) was examined as its prevalence has been inversely correlated with that of multiple chronic conditions.45
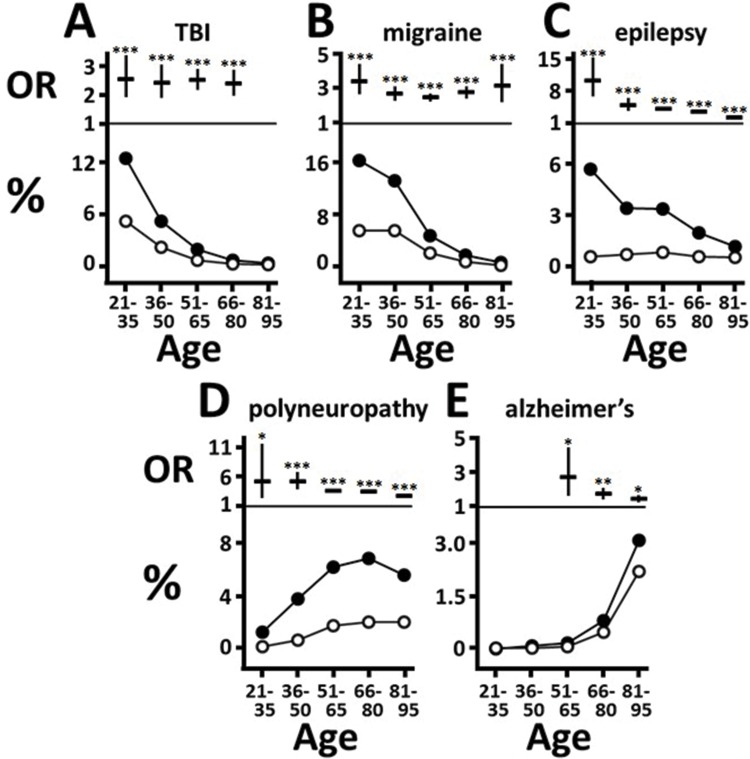
TBI was more common in tremor patients aged 21–80, with an OR of 2.4–2.6; the prevalence was 13% among 21–35-year-olds, falling to 5.3% at 36–50, and to 0.8% at 66–80 (Figure 5A). Migraine was more common at all ages in ET, with the maximal OR (3.3) at ages 21–35 and the minimum (2.4) at 51–65. Migraine was present in 16% of ET 21–35-year-olds, and in 1.7% at ages 66–80 (Figure 5B). Epilepsy was increased at all ages in ET, and markedly so at ages 21–35 (OR = 10.2), among whom 5.7% had epilepsy. The OR fell to 4.9 at ages 36–50 and to 2.2 at 81–95 (Figure 5C). The diagnosis of idiopathic polyneuropathy was also much more common in tremor patients, with an OR of 5.1–5.2 below age 51, and approximately 3 in those over age 50, with a prevalence of 1.4% of 21–35-year-olds, rising to 6.9% at ages 66–80 (Figure 5D). The diagnosis of Alzheimer’s dementia was more common in tremor patients above age 50, with OR = 2.7 at ages 51-65, falling to 1.4 at 81–95, with a prevalence of 0.2% at ages 51–65, rising to 3.1% at ages 81–95 (Figure 5E). The frequency of ALS did not differ significantly (not shown), although there was a trend to a lower rate from ages 21 to 95 in ET, with OR = 0.16 (p = 0.00034).
Figure 5. Neurological Conditions. See Figure 1 for description of veterans with and without tremor.
Discussion
Limitations of this survey include the fact that “other specified forms of tremor,” as well as ET, qualified for the ICD-9 code 333.1, so that a population study based on this code cannot be 100% accurate for ET. In addition, inaccurate diagnoses may be made by non-specialists, including general neurologists. In a study by Louis et al.,46 chart review of patients identified with 333.1 in billing records indicated that the diagnosis was correct in only 49%.
The results of the current study form a coherent pattern in which the altered prevalence of numerous comorbidities in cases diagnosed with 333.1 can be linked to chronic stress or, with some conditions, to TBI, which is highly correlated with PTSD. Compared to the disease profile of Parkinson’s disease, the main diagnostic consideration in persons with tremor, that of ET in this study shares some overlap, but also significant differences. The present study shares findings with those described for Parkinson’s disease of increased rates of anxiety, depression, PTSD,47 schizophrenia, bipolar disorder,48 vitamin D insufficiency,49 congestive heart failure,50 IBS,51 hearing loss,52 history of head trauma,53 dementia, polyneuropathy,54 and high or normal rates of diabetes.55–57 However, in contrast to the study population, Parkinson’s is characterized by unchanged rates of OCD,58 less smoking and alcohol abuse,56,57,59,60 a lower rate of hyperlipidemia,61 normal or low rates of hypertension, CAD, and stroke,56,57,62,63 normal rate of hypothyroidism,64 low rates of lung and colorectal cancer,65 decreased migraine,66 less epilepsy,67 and an association with ALS68 compared to control populations. These numerous differences indicate that ET-diagnosed cases of the present study did not represent misdiagnosed Parkinson’s disease.
On review of all 350 evaluable charts of veterans in VA Greater Los Angeles Healthcare System diagnosed with 333.1 in FY13, we found that 83.4% had clinical descriptions consistent with ET, or 80%, if cases with associated recent-onset parkinsonism are excluded. This figure suggests that, with extrapolation to national data, the findings of the overall survey are likely to be valid, but should be confirmed in other large databases using the ICD-10 code, which excludes other forms of tremor, and potentially using additional criteria. Reasons why our figure is higher than that of Louis et al.46 may include differences in the provider and patient populations. VA providers may have been more likely to use the code 781.0 Tremor Unspecified when the diagnosis was not clear, and veterans, due to exposure to stress, may be more likely to have ET compared to other forms of tremor.
Strengths include a large database and a health status portrayal more comprehensive than most studies. Despite limitations, this study replicated previous findings, including increased anxiety, depression, hearing loss, migraine, dementia in ET, and associations with alcohol, head trauma, and likely poor diet, supporting the validity of the overall findings.
Chronic stress and the ET patient
At all ages the OR for PTSD, anxiety and depression among ET veterans was at least doubled, resulting in high prevalence rates. Combat veterans with PTSD are prone to develop co-morbid anxiety and depression that persist even 20 years later.8,69 IBS, strongly associated with stress, anxiety, depression, and major life trauma,26,27 was also doubled after age 35 in ET veterans. TBI, previously reported to increase ET risk,70 is strongly associated with PTSD,33,34 accounting for the doubled rate of TBI below age 81 in ET veterans.
Much research indicates that emotional experience is dominated by two dimensions: negative (NA) and positive affect. NA includes fearfulness, tension, sadness, guilt, anxiety, and depression. The high-NA trait may be related to early life circumstances or occur after a traumatic life event, and forms the basis of two personality constructs, one characterized by exaggerated negative reactions, and the other, known as type D (distressed) personality, in which NA is combined with social inhibition of emotional expression.26 The type D personality is stable over time and, along with its subcomponents NA and social inhibition, is influenced by both environmental and heritable factors.71,72 ET subjects score high on personality scales for fearfulness, anxiety, anticipatory worry, and pessimism,73,74 NA trait features. The high tendency for social withdrawal, shyness, and social phobia75 suggests that at least some ET subjects possess the type D personality. The burden of chronic stress associated with PTSD, anxiety, depression, NA, and type D personality promotes multiple poor health outcomes, as explored below.
Chronic stress, tremor, mental illness, and substance abuse
OCD may commence 10 years after a traumatic life event,6,7 thus the doubled rate of OCD among ET veterans between age 36 and 80 is consistent with combat experiences at ages 21–35. The greater rate of schizophrenia can be related to higher rates in tremor cases of risk factors: cannabis use, alcohol abuse, anxiety, bipolar disorder,10 and TBI.76 Chronic social stress and social isolation, likely present in stressed ET patients, are also risks for schizophrenia.77 PTSD is associated with later bipolar disorder,8,9 which was increased in ET cases.
Although smoking is reported to reduce the risk of ET,78,79 the tremor patients of this survey had higher tobacco use, attributable to known risk factors for smoking: depression, anxiety, PTSD, bipolar disease, and schizophrenia.12,80,81 Persons with type D personality are more likely to smoke.82 Alcohol abuse and alcoholic liver disease were more common in tremor patients. Alcohol use is a risk factor for developing ET,83 conceivably due to chronic stress, a well-known precipitant of alcohol use disorder.11 ET veterans had higher rates of risk factors for alcohol dependency: anxiety, depression, and PTSD.11,13 Type D personality is also associated with alcoholism.84
Increased cannabis usage below age 51 by tremor veterans may be due to anxiety and depression, as anxiety disorders have a high association with cannabis use.14,85 In contrast, psychostimulant abuse was one-third less frequent than in non-ET patients at ages 51–65, possibly due to the elevated harm avoidance trait,73 which is also believed to underlie reduced abuse by OCD patients.13
Chronic stress, tremor, hypertension, and components of the metabolic syndrome
Especially striking was the strong association of ET with hypertension, with OR doubled at most ages. Chronic stress, which causes excess cortisol secretion and sympathetic nervous system activation, is a well-established cause of hypertension.12 Hypertension and evidence of sympathetic overarousal have been found in PTSD,16,86 anxiety disorders,20,87 depression,88,89 and type D personality.22,82 A Mediterranean diet is associated with a lower risk for developing ET.90 In contrast, the tremor patients of this study had risk factors for poor diet. Chronic stress, including depression, PTSD, type D personality, and social isolation are generally associated with a high-fat, low-fruit diet, obesity, and physical inactivity.12,15,16,21,82,91–94 ET veterans had increased obesity rates at all ages, consistent with these risk factors. Vitamin D deficiency in ET patients reinforces the impression that they had poor diet and lack of outdoor activity. Tremor patients had slightly more diabetes at ages 51–80, likely related to poor diet, obesity, physical inactivity,95 depression, PTSD, smoking, and alcohol use,17,89,96 all increased in tremor patients. The reduction of diabetes at ages 81–95 might have resulted from a reduced lifespan in ET patients with diabetes. At all ages the OR for hyperlipidemia was increased in ET patients, again likely related to poor diet and lack of exercise; PTSD is also a risk factor.17,86
Tremor, medical illnesses, and cancer
Tremor patients were more likely to have cerebrovascular disease above age 35, and CAD, congestive heart failure, and stroke above age 50. The well-known CAD risk factors hypertension, smoking, hyperlipidemia, diabetes, and alcoholism were more common in tremor patients. In addition, chronic stress, depression, PTSD, generalized anxiety, type D personality, and lack of social support promote CAD, mediated by excess activation of the hypothalamic–pituitary–adrenal (HPA) axis.12,16,20–22,82,93 The elevated rate of congestive heart failure in middle-aged and older tremor patients may be related to the presence of known risk factors: CAD, diabetes, hypertension, obesity, smoking,97 potentially physical inactivity,98 and PTSD,16 Of risk factors for stroke, many were increased in tremor patients: depression, anxiety, chronic stress,23 hypertension, smoking, obesity, diabetes, excessive alcohol consumption, abnormal lipid profile, and possibly poor diet and physical inactivity. Renal insufficiency was more common in tremor patients aged 51–80, likely due to the enhanced presence of the main risk factors hypertension, diabetes, obesity, and vascular disease.28
The increased prevalence of COPD among tremor patients above age 50 is likely related to the main risk factor, smoking.99 Similarly, increased asthma above age 35 may be related to smoking100 and potentially to diet.101 Autoimmune hypothyroidism is elevated sixfold after smoking cessation,24 thus hypothyroidism, more frequent after age 35 in tremor patients, might be related to attempts to cease smoking.
Despite higher tobacco use by tremor patients, lung cancer rates were not increased. Similarly, despite the increased presence of risk factors for colorectal cancer: smoking, alcohol abuse, obesity, low vitamin D, and potentially poor diet and physical inactivity,102–104 colorectal cancer rates were not increased, in contrast to a prior finding of an increase in ET.105 Prostate cancer was also generally not increased, except for a slight increase at age 51–65, despite risk factors of smoking, obesity, vitamin D deficiency, and potentially poor dietary and exercise habits.102,106,107 It is possible that, due to higher vascular risk factors, more tremor veterans may have taken aspirin, which is protective against lung108 and colorectal cancers,109 or were exposed to another protective factor.
Tremor, hearing, sight, and neurological disorders
In confirmation of prior studies,2,110 we found increased sensorineural hearing loss at all ages in tremor patients. Some ET veterans may have had hearing loss from TBI, which was more common among them, or from combat experiences. Risk factors for hearing impairment were more prevalent in tremor cases, including hypertension, smoking, diabetes, and hyperlipidemia.29 The increased macular degeneration seen in tremor patients after age 50 is attributable to the higher rates of known risk factors: smoking, hypertension, obesity, vascular disease,30,31 and potentially poor diet.111,112 Diabetes and hypertension, more common in tremor patients, are risk factors for glaucoma,32 more common at ages 51–70.
The increased rate of migraine at all ages in tremor cases is consistent with a prior study.113 Risk factors for migraine present in tremor cases include TBI, PTSD, depression, OCD, anxiety disorders, COPD, asthma, stressful life events, obesity,35–37 hyperlipidemia, and smoking.35–38 In addition to TBI, risk factors for epilepsy that were more common in tremor patients include depression,114,115 smoking,116 alcohol dependency,39 hypertension,40 diabetes,117 history of stroke,118 and Alzheimer’s disease.119 Idiopathic polyneuropathy was found more often at all ages in tremor patients, who had the known risk factors hypertension, obesity, metabolic syndrome, vascular disease, and smoking.41,42,120 In some patients the “idiopathic” polyneuropathy may have been secondary to alcoholism or early diabetes, both more common in tremor patients. The present study found increased rates of ‘Alzheimer’s diagnosis in tremor patients over age 50, confirming previous reports.4,121 Risk factors for dementia more common in tremor patients include depression, mid-life hypertension, diabetes, mid-life obesity, mid-life hyperlipidemia, smoking, probably physical inactivity,43,44 COPD,122 and TBI.123 Moreover, PTSD carries a 1.8-fold increase of dementia in veterans.124
Chronic stress as a common cause of tremor and associated conditions
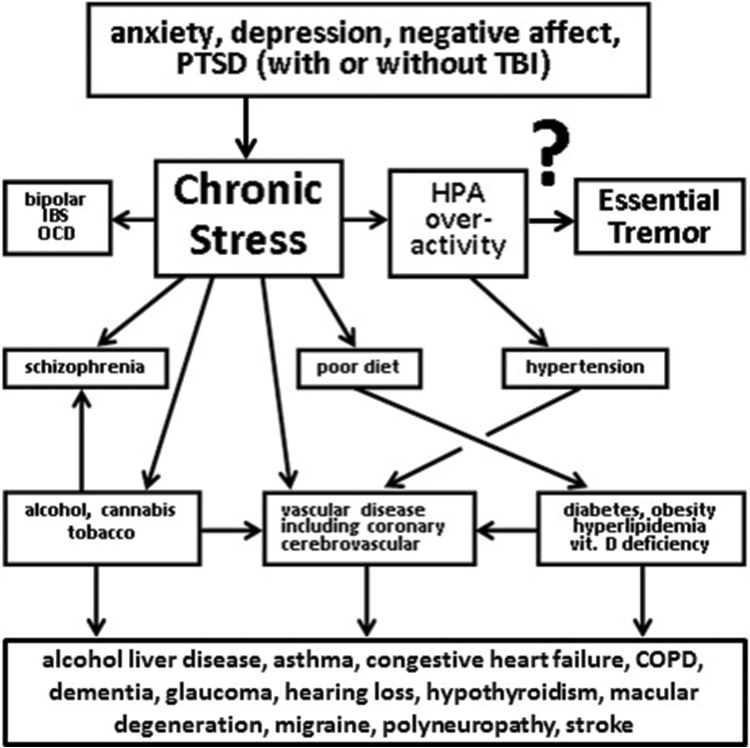
Chronic stress among tremor veterans, as associated with PTSD, anxiety, and depression, provides a basis for a heightened disease burden (Figure 6). Insofar as PTSD, anxiety, depression, chronic stress, and type D personality are common in the general population, the associations with tremor noted in veterans are likely present in non-veterans as well, providing explanations for higher mortality in ET,4 and for previously noted associations of ET with dementia, alcoholism, and hearing loss.
Figure 6. Model of Relationship of Essential Tremor to Comorbid Conditions. Chronic stress, as occurs with post-traumatic stress disorder (PTSD), anxiety, depression, or negative affect/Type D personality trait increases the risk of psychiatric conditions, substance abuse, vascular disease, hypertension, components of the metabolic syndrome, and poor diet. These together in turn increase the risk of diseases affecting multiple organs, eyesight and hearing, and neurological conditions. Traumatic brain injury , present in many PTSD patients, also contributes to certain neurologic conditions, such as migraine and epilepsy. It is proposed that chronic stress, in addition to increasing the risk of multiple diseases, promotes essential tremor (ET), so that the conditions associated with chronic stress are more common in ET.
A key question is why ET may be associated with chronic stress. Two potential explanations may apply. In one, chronic stress induces poor health outcomes; these in turn promoting nervous system injury that may underlie tremor, as well as dementia and polyneuropathy. Another explanation, one that we suggest applies to some ET cases, is that chronic stress directly causes ET. This notion is supported by the finding that depressed persons are more likely than non-depressed persons to have developed ET when evaluated just three years later.1 A recurring theme among conditions associated with tremor is excess activation of the HPA axis, involved in chronic stress, PTSD, depression, anxiety, hypertension, obesity, diabetes, IBS, and the type D personality. Stress/distress/HPA overactivity might ensue from discrete traumatic life events (causing PTSD or depression), early life events, epigenetic or genetic factors that affect temperament or resilience, or from variations in HPA functioning.
Chronic stress might induce tremor through affecting receptors and ion channels, or by affecting brain microstructure. Depression reduces 5-hydroxytryptamine (HT)1a receptors in frontal and limbic cortex;125 stress also reduces Purkinje neuron 5-HT1a receptor levels in mice.126 Stress affects dendritic morphology and spine numbers in hippocampus, medial prefrontal cortex, bed nucleus of stria terminalis, and basolateral amygdala as the best-studied nuclei. Dendritic changes in the amygdala are long-lasting, and thought to underlie enhanced fear and anxiety responses.127 By analogy, chronic stress and/or HPA hyperactivation might cause long-lasting microstructural changes in cerebellar or related circuitry so that ET ensues. After 1 hour of restraint stress, rats not only show more anxiety, but increased Purkinje spine numbers, indicating that stress can affect Purkinje cell morphology.128 Abnormal climbing fiber–Purkinje cell connections have been described in ET cerebellar cortex.129 Further research is needed to explore whether these or other changes may be engendered by stress and lead to tremor.
Acknowledgments
We thank Hovsep Kosoyan, PhD, and David I. Smith, MS, for assistance in data analysis and the preparation of figures.
Footnotes
Funding: The authors were supported by Veterans Affairs.
Financial Disclosures: None.
Conflict of Interests: The authors report no conflict of interest.
Ethics Statement: This study was reviewed and approved by the authors' institutional ethics committee and was performed in accordance with the ethical standards detailed in the Declaration of Helsinki, with waived consent and authorization for review of medical records.
References
- 1.Louis ED, Benito-León J, Bermejo-Pareja F. Neurological disorders in central Spain (NEDICES) Study Group. Self-reported depression and anti-depressant medication use in essential tremor: cross-sectional and prospective analyses in a population-based study. Eur J Neurol. 2007;14:1138–1146. doi: 10.1111/j.1468-1331.2007.01923.x. doi: 10.1111/j.1468-1331.2007.01923.x. [DOI] [PubMed] [Google Scholar]
- 2.Ondo WG, Sutton L, Dat Vuong K, Lai D, Jankovic J. Hearing impairment in essential tremor. Neurology. 2003;61:1093–1097. doi: 10.1212/01.wnl.0000086376.40750.af. doi: 10.1212/01.WNL.0000086376.40750.AF. [DOI] [PubMed] [Google Scholar]
- 3.Bermejo-Pareja F, Louis ED, Benito-León J. Neurological Disorders in Central Spain (NEDICES) Study Group. Risk of incident dementia in essential tremor: a population-based study. Mov Disord. 2007;22:1573–1580. doi: 10.1002/mds.21553. doi: 10.1002/mds.21553. [DOI] [PubMed] [Google Scholar]
- 4.Louis ED, Benito-León J, Ottman R, Bermejo-Pareja F, Neurological Disorders in Central Spain (NEDICES) Study Group A population-based study of mortality in essential tremor. Neurology. 2007;69:1982–1989. doi: 10.1212/01.wnl.0000279339.87987.d7. doi: 10.1212/01.wnl.0000279339.87987.d7. [DOI] [PubMed] [Google Scholar]
- 5.Lorenz D, Poremba C, Papengut F, Schreiber S, Deuschl G. The psychosocial burden of essential tremor in an outpatient- and a community-based cohort. Eur J Neurol. 2011;18:972–979. doi: 10.1111/j.1468-1331.2010.03295.x. doi: 10.1111/j.1468-1331.2010.03295.x. [DOI] [PubMed] [Google Scholar]
- 6.Fontenelle LF, Cocchi L, Harrison BJ, Shavitt RG, do Rosário MC, Ferrãof YA, et al. Towards a post-traumatic subtype of obsessive-compulsive disorder. J Anxiety Disord. 2012;26:377–383. doi: 10.1016/j.janxdis.2011.12.001. doi: 10.1016/j.janxdis.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Dykshoorn KL. Trauma-related obsessive-compulsive disorder: a review. Health Psychol Behav Med. 2014;2:517–528. doi: 10.1080/21642850.2014.905207. doi: 10.1080/21642850.2014.905207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chou KL, Mackenzie CS, Liang K, Sareen J. Three-year incidence and predictors of first-onset of DSM-IV mood, anxiety, and substance use disorders in older adults: results from Wave 2 of the National Epidemiologic Survey on alcohol and related conditions. J Clin Psychiatry. 2011;72:144–155. doi: 10.4088/JCP.09m05618gry. doi: 10.4088/JCP.09m05618gry. [DOI] [PubMed] [Google Scholar]
- 9.Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on alcohol and related conditions. Mol Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harper S, Towers-Evans H, MacCabe J. The aetiology of schizophrenia: what have the Swedish medical registers taught us? Soc Psychiatry Psychiatr Epidemiol. 2015;50:1471–1479. doi: 10.1007/s00127-015-1081-7. doi: 10.1007/s00127-015-1081-7. [DOI] [PubMed] [Google Scholar]
- 11.Anthenelli RM. Focus on: comorbid mental health disorders. Alcohol Res Health. 2010;33:109–117. [PMC free article] [PubMed] [Google Scholar]
- 12.Strike PC, Steptoe A. Psychosocial factors in the development of coronary artery disease. Prog Cardiovasc Dis. 2004;46:337–347. doi: 10.1016/j.pcad.2003.09.001. doi: 10.1016/j.pcad.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Brady KT, Haynes LF, Hartwell KJ, Killeen TK. Substance use disorders and anxiety: a treatment challenge for social workers. Soc Work Public Health. 2013;28:407–423. doi: 10.1080/19371918.2013.774675. doi: 10.1080/19371918.2013.774675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crippa JA, Zuardi AW, Martín-Santos R, Bhattacharyya S, Atakan Z, McGuire P, et al. Cannabis and anxiety: a critical review of the evidence. Hum Psychopharmacol. 2009;24:515–523. doi: 10.1002/hup.1048. doi: 10.1002/hup.1048. [DOI] [PubMed] [Google Scholar]
- 15.Godfrey KM, Lindamer LA, Mostoufi S, Afari N. Posttraumatic stress disorder and health: a preliminary study of group differences in health and health behaviors. Ann Gen Psychiatry. 2013;12:30. doi: 10.1186/1744-859X-12-30. doi: 10.1186/1744-859X-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brudey C, Park J, Wiaderkiewicz J, Kobayashi I, Mellman TA, Marvar PJ. Autonomic and inflammatory consequences of posttraumatic stress disorder and the link to cardiovascular disease. Am J Physiol Regul Integr Comp Physiol. 2015;309:R315–321. doi: 10.1152/ajpregu.00343.2014. doi: 10.1152/ajpregu.00343.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levine AB, Levine LM, Levine TB. Posttraumatic stress disorder and cardiometabolic disease. Cardiology. 2014;127:1–19. doi: 10.1159/000354910. doi: 10.1159/000354910. [DOI] [PubMed] [Google Scholar]
- 18.Heppner PS, Crawford EF, Haji UA, Afari N, Hauger RL, Dashevsky BA, et al. The association of posttraumatic stress disorder and metabolic syndrome: a study of increased health risk in veterans. BMC Med. 2009;7:1. doi: 10.1186/1741-7015-7-1. doi: 10.1186/1741-7015-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kahl KG, Schweiger U, Correll C, Müller C, Busch ML, Bauer M, et al. Depression, anxiety disorders, and metabolic syndrome in a population at risk for type 2 diabetes mellitus. Brain Behav. 2015;5:e00306. doi: 10.1002/brb3.306. doi: 10.1002/brb3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tully PJ, Cosh SM, Baune BT. A review of the affects of worry and generalized anxiety disorder upon cardiovascular health and coronary heart disease. Psychol Health Med. 2013;18:627–644. doi: 10.1080/13548506.2012.749355. doi: 10.1080/13548506.2012.749355. [DOI] [PubMed] [Google Scholar]
- 21.Bhatt H, Safford M, Glasser S. Coronary heart disease risk factors and outcomes in the twenty-first century: findings from the REasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Curr Hypertens Rep. 2015;17:541. doi: 10.1007/s11906-015-0541-5. doi: 10.1007/s11906-015-0541-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Molloy GJ, Perkins-Porras L, Strike PC, Steptoe A. Type-D personality and cortisol in survivors of acute coronary syndrome. Psychosom Med. 2008;70:863–868. doi: 10.1097/PSY.0b013e3181842e0c. doi: 10.1097/PSY.0b013e3181842e0c. [DOI] [PubMed] [Google Scholar]
- 23.Kuklina EV, Tong X, George MG, Bansil P. Epidemiology and prevention of stroke: a worldwide perspective. Expert Rev Neurother. 2012;12:199–208. doi: 10.1586/ern.11.99. doi: 10.1586/ern.11.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carlé A, Bülow Pedersen I, Knudsen N, Perrild H, Ovesen L, Rasmussen LB, et al. Smoking cessation is followed by a sharp but transient rise in the incidence of overt autoimmune hypothyroidism – a population-based, case-control study. Clin Endocrinol (Oxf) 2012;77:764–772. doi: 10.1111/j.1365-2265.2012.04455.x. doi: 10.1111/j.1365-2265.2012.04455.x. [DOI] [PubMed] [Google Scholar]
- 25.Sugiyama D, Nishimura K, Tamaki K, Tsuji G, Nakazawa T, Morinobu A, et al. Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. 2010;69:70–81. doi: 10.1136/ard.2008.096487. doi: 10.1136/ard.2008.096487. [DOI] [PubMed] [Google Scholar]
- 26.Muscatello MR, Bruno A, Scimeca G, Pandolfo G, Zoccali RA. Role of negative affects in pathophysiology and clinical expression of irritable bowel syndrome. World J Gastroenterol. 2014;20:7570–7586. doi: 10.3748/wjg.v20.i24.7570. doi: 10.3748/wjg.v20.i24.7570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. 2014;20:14126–14131. doi: 10.3748/wjg.v20.i39.14126. doi: 10.3748/wjg.v20.i39.14126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kiefer MM, Ryan MJ. Primary care of the patient with chronic kidney disease. Med Clin North Am. 2015;99:935–952. doi: 10.1016/j.mcna.2015.05.003. doi: 10.1016/j.mcna.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Oron Y, Elgart K, Marom T, Roth Y. Cardiovascular risk factors as causes for hearing impairment. Audiol Neurootol. 2014;19:256–260. doi: 10.1159/000363215. doi: 10.1159/000363215. [DOI] [PubMed] [Google Scholar]
- 30.Chakravarthy U, Wong TY, Fletcher A, Piault E, Evans C, Zlateva G, et al. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol. 2010;10:31. doi: 10.1186/1471-2415-10-31. doi: 10.1186/1471-2415-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Velilla S, García-Medina JJ, García-Layana A, Dolz-Marco R, Pons-Vázquez S, Pinazo-Durán MD, et al. Smoking and age-related macular degeneration: review and update. J Ophthalmol. 2013;2013:895147. doi: 10.1155/2013/895147. doi: 10.1155/2013/895147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Newman-Casey PA, Talwar N, Nan B, Musch DC, Stein JD. The relationship between components of metabolic syndrome and open-angle glaucoma. Ophthalmology. 2011;118:1318–1326. doi: 10.1016/j.ophtha.2010.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. Am J Psychiatry. 2009;166:768–776. doi: 10.1176/appi.ajp.2009.08101604. doi: 10.1176/appi.ajp.2009.08101604. [DOI] [PubMed] [Google Scholar]
- 34.Yurgil KA, Barkauskas DA, Vasterling JJ, Nievergelt CM, Larson GE, Schork NJ, et al. Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty Marines. JAMA Psychiatry. 2014;71:149–157. doi: 10.1001/jamapsychiatry.2013.3080. doi: 10.1001/jamapsychiatry.2013.3080. [DOI] [PubMed] [Google Scholar]
- 35.Buse DC, Silberstein SD, Manack AN, Papapetropoulos S, Lipton RB. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260:1960–1969. doi: 10.1007/s00415-012-6725-x. doi: 10.1007/s00415-012-6725-x. [DOI] [PubMed] [Google Scholar]
- 36.Carod-Artal FJ. Tackling chronic migraine: current perspectives. J Pain Res. 2014;7:185–194. doi: 10.2147/JPR.S61819. doi: 10.2147/JPR.S61819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Defrin R. Chronic post-traumatic headache: clinical findings and possible mechanisms. J Man Manip Ther. 2014;22:36–44. doi: 10.1179/2042618613Y.0000000053. doi: 10.1179/2042618613Y.0000000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sacco S, Pistoia F, Degan D, Carolei A. Conventional vascular risk factors: their role in the association between migraine and cardiovascular diseases. Cephalalgia. 2015;35:146–164. doi: 10.1177/0333102414559551. doi: 10.1177/0333102414559551. [DOI] [PubMed] [Google Scholar]
- 39.Samokhvalov AV, Irving H, Mohapatra S, Rehm J. Alcohol consumption, unprovoked seizures, and epilepsy: a systematic review and meta-analysis. Epilepsia. 2010;51:1177–1184. doi: 10.1111/j.1528-1167.2009.02426.x. doi: 10.1111/j.1528-1167.2009.02426.x. [DOI] [PubMed] [Google Scholar]
- 40.Ng SK, Hauser WA, Brust JC, Susser M. Hypertension and the risk of new-onset unprovoked seizures. Neurology. 1993;43:425–428. doi: 10.1212/wnl.43.2.425. doi: 10.1212/WNL.43.2.425. [DOI] [PubMed] [Google Scholar]
- 41.Baldereschi M, Inzitari M, Di Carlo A, Bovis F, Maggi S, Capurso A, et al. Vascular factors predict polyneuropathy in a non-diabetic elderly population. Neurol Sci. 2013;34:955–962. doi: 10.1007/s10072-012-1167-x. doi: 10.1007/s10072-012-1167-x. [DOI] [PubMed] [Google Scholar]
- 42.Visser NA, Vrancken AF, van der Schouw YT, van den Berg LH, Notermans NC. Chronic idiopathic axonal polyneuropathy is associated with the metabolic syndrome. Diabetes Care. 2013;36:817–822. doi: 10.2337/dc12-0469. doi: 10.2337/dc12-0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de Bruijn RF, Ikram MA. Cardiovascular risk factors and future risk of Alzheimer’s disease. BMC Med. 2014;12:130. doi: 10.1186/s12916-014-0130-5. doi: 10.1186/s12916-014-0130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Deckers K, van Boxtel MP, Schiepers OJ, de Vugt M, Muñoz Sánchez JL, Anstey KJ, et al. Target risk factors for dementia prevention: a systematic review and Delphi consensus study on the evidence from observational studies. Int J Geriatr Psychiatry. 2015;30:234–246. doi: 10.1002/gps.4245. doi: 10.1002/gps.4245. [DOI] [PubMed] [Google Scholar]
- 45.Mitchell CS, Hollinger SK, Goswami SD, Polak MA, Lee RH, Glass JD. Antecedent disease is less prevalent in amyotrophic lateral sclerosis. Neurodegener Dis. 2015;15:109–113. doi: 10.1159/000369812. doi: 10.1159/000369812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Louis ED, Applegate LM, Rios E. ICD-9 CM code 333.1 as an identifier of patients with essential tremor: a study of the positive predictive value of this code. Neuroepidemiology. 2007;28:181–185. doi: 10.1159/000104096. doi: 10.1159/000104096. [DOI] [PubMed] [Google Scholar]
- 47.Chan YE, Bai YM, Hsu JW. Post-traumatic stress disorder and risk of Parkinson Disease: a nationwide longitudinal study. Am J Geriatr Psychiatry. 2017;25:917–923. doi: 10.1016/j.jagp.2017.03.012. doi: 10.1016/j.jagp.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 48.Lin HL, Lin HC, Chen YH. Psychiatric diseases predated the occurrence of Parkinson disease: a retrospective cohort study. Ann Epidemiol. 2014;24:206–213. doi: 10.1016/j.annepidem.2013.12.010. doi: 10.1016/j.annepidem.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 49.Zhao Y, Sun Y, Ji HF, Shen L. Vitamin D levels in Alzheimer’s and Parkinson’s diseases: a meta-analysis. Nutrition. 2013;29:828–832. doi: 10.1016/j.nut.2012.11.018. doi: 10.1016/j.nut.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 50.Zesiewicz TA, Strom JA, Borenstein AR, Hauser RA, Cimino CR, Fontanet HL, et al. Heart failure in ‘Parkinson’s disease: analysis of the United States Medicare current beneficiary survey. Parkinsonism Relat Disord. 2004;10:417–420. doi: 10.1016/j.parkreldis.2004.04.001. doi: 10.1016/j.parkreldis.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 51.Mishima T, Fukae J, Fujioka S, Inoue K, Tsuboi Y. The prevalence of constipation and irritable bowel syndrome in Parkinson’s disease patients according to Rome III diagnostic criteria. J Parkinsons Dis. 2017;7:353–357. doi: 10.3233/JPD-160982. doi: 10.3233/JPD-160982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vitale C, Marcelli V, Allocca R, Santangelo G, Riccardi P, Erro R, et al. Hearing impairment in Parkinson’s disease: expanding the nonmotor phenotype. Mov Disord. 2012;27:1530–1535. doi: 10.1002/mds.25149. doi: 10.1002/mds.25149. [DOI] [PubMed] [Google Scholar]
- 53.Jafari S, Etminan M, Aminzadeh F, Samii A. Head injury and risk of Parkinson disease: a systematic review and meta-analysis. Mov Disord. 2013;28:1222–1229. doi: 10.1002/mds.25458. doi: 10.1002/mds.25458. [DOI] [PubMed] [Google Scholar]
- 54.Zis P, Grünewald RA, Chaudhuri RK, Hadjivassiliou M. Peripheral neuropathy in idiopathic Parkinson’s disease: a systematic review. J Neurol Sci. 2017;378:204–209. doi: 10.1016/j.jns.2017.05.023. doi: 10.1016/j.jns.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 55.Klimek P, Kautzky-Willer A, Chmiel A, Schiller-Frühwirth I, Thurner S. Quantification of diabetes comorbidity risks across life using nation-wide big claims data. PLoS Comput Biol. 2015;11:e1004125. doi: 10.1371/journal.pcbi.1004125. doi: 10.1371/journal.pcbi.1004125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nataraj A, Rajput AH. ’Parkinson’s disease, stroke, and related epidemiology. Mov Disord. 2005;20:1476–1480. doi: 10.1002/mds.20608. doi: 10.1002/mds.20608. [DOI] [PubMed] [Google Scholar]
- 57.Levine RL, Jones JC, Bee N. Stroke and Parkinson’s disease. Stroke. 1992;23:839–842. doi: 10.1161/01.str.23.6.839. doi: 10.1161/01.STR.23.6.839. [DOI] [PubMed] [Google Scholar]
- 58.Harbishettar V, Pal PK, Janardhan Reddy YC, Thennarasu K. Is there a relationship between Parkinson’s disease and obsessive-compulsive disorder? Parkinsonism Relat Disord. 2005;11:85–88. doi: 10.1016/j.parkreldis.2004.07.006. doi: 10.1016/j.parkreldis.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 59.Nicoletti A, Pugliese P, Nicoletti G, Arabia G, Annesi G, De Mari M, et al. Voluptuary habits and clinical subtypes of ‘Parkinson’s disease: the FRAGAMP case-control study. Mov Disord. 2010;25:2387–2394. doi: 10.1002/mds.23297. doi: 10.1002/mds.23297. [DOI] [PubMed] [Google Scholar]
- 60.Evans AH, Lawrence AD, Potts J, MacGregor L, Katzenschlager R, Shaw K, et al. Relationship between impulsive sensation seeking traits, smoking, alcohol and caffeine intake, and ‘Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2006;77:317–321. doi: 10.1136/jnnp.2005.065417. doi: 10.1136/jnnp.2005.065417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cereda E, Cassani E, Barichella M, Spadafranca A, Caccialanza R, Bertoli S, et al. Low cardiometabolic risk in Parkinson’s disease is independent of nutritional status, body composition and fat distribution. Clin Nutr. 2012;31:699–704. doi: 10.1016/j.clnu.2012.02.004. doi: 10.1016/j.clnu.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 62.Konitsiotis S, Bostantjopoulou S, Chondrogiorgi M, Katsarou Z, Tagaris G, Mavromatis I, et al. Clinical characteristics of Parkinson’s disease patients in Greece: a multicenter, nation-wide, cross-sectional study. J Neurol Sci. 2014;343:36–40. doi: 10.1016/j.jns.2014.05.003. doi: 10.1016/j.jns.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 63.Struck LK, Rodnitzky RL, Dobson JK. Stroke and its modification in ‘Parkinson’s disease. Stroke. 1990;20:1395–1399. doi: 10.1161/01.str.21.10.1395. doi: 10.1161/01.STR.21.10.1395. [DOI] [PubMed] [Google Scholar]
- 64.Munhoz RP, Teive HA, Troiano AR. Parkinson’s disease and thyroid dysfunction. Parkinsonism Relat Disord. 2004;10:381–383. doi: 10.1016/j.parkreldis.2004.03.008. doi: 10.1016/j.parkreldis.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 65.Catalá-López F, Suárez-Pinilla M, Suárez-Pinilla P, Valderas JM, Gómez-Beneyto M, Martinez S, et al. Inverse and direct cancer comorbidity in people with central nervous system disorders: a meta-analysis of cancer incidence in 577,013 participants of 50 observational studies. Psychother Psychosom. 2014;83:89–105. doi: 10.1159/000356498. doi: 10.1159/000356498. [DOI] [PubMed] [Google Scholar]
- 66.Nunes JC, Costa Bergamaschi EN, Freitas FC. Prevalence of headache in patients with Parkinson’s disease and its association with the side of motor symptom onset. Neurol Sci. 2014;35:595–600. doi: 10.1007/s10072-013-1571-x. doi: 10.1007/s10072-013-1571-x. [DOI] [PubMed] [Google Scholar]
- 67.Feddersen B, Rémi J, Einhellig M, Stoyke C, Krauss P, Noachtar S. ’Parkinson’s disease: less epileptic seizures, more status epilepticus. Epilepsy Res. 2014;108:349–354. doi: 10.1016/j.eplepsyres.2013.11.013. doi: 10.1016/j.eplepsyres.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 68.Longinetti E, Mariosa D, Larsson H, Ye W, Ingre C, Almqvist C, et al. Neurodegenerative and psychiatric diseases among families with amyotrophic lateral sclerosis. Neurology. 2017;89:578–585. doi: 10.1212/WNL.0000000000004179. doi: 10.1212/WNL.0000000000004179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. J Affect Disord. 2010;123:249–257. doi: 10.1016/j.jad.2009.08.006. doi: 10.1016/j.jad.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 70.Benito-León J, Louis ED, Labiano-Fontcuberta A, Bermejo-Pareja F. Serious head trauma preceding essential tremor: a population-based study (NEDICES) J Neurol Sci. 2015;353:116–121. doi: 10.1016/j.jns.2015.04.030. doi: 10.1016/j.jns.2015.04.030. [DOI] [PubMed] [Google Scholar]
- 71.Kupper N, Denollet J, de Geus EJ, Boomsma DI, Willemsen G. Heritability of type-D personality. Psychosom Med. 2007;69:675–681. doi: 10.1097/PSY.0b013e318149f4a7. doi: 10.1097/PSY.0b013e318149f4a7. [DOI] [PubMed] [Google Scholar]
- 72.Kupper N, Boomsma DI, de Geus EJ, Denollet J, Willemsen G. Nine-year stability of type D personality: contributions of genes and environment. Psychosom Med. 2011;73:75–82. doi: 10.1097/PSY.0b013e3181fdce54. doi: 10.1097/PSY.0b013e3181fdce54. [DOI] [PubMed] [Google Scholar]
- 73.Chatterjee A, Jurewicz EC, Applegate LM, Louis ED. Personality in essential tremor: further evidence of non-motor manifestations of the disease. J Neurol Neurosurg Psychiatry. 2004;75:958–961. doi: 10.1136/jnnp.2004.037176. doi: 10.1136/jnnp.2004.037176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Thenganatt MA, Louis ED. Personality profile in essential tremor: a case-control study. Parkinsonism Relat Disord. 2012;18:1042–1044. doi: 10.1016/j.parkreldis.2012.05.015. doi: 10.1016/j.parkreldis.2012.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Woods SP, Scott JC, Fields JA, Poquette A, Tröster AI. Executive dysfunction and neuropsychiatric symptoms predict lower health status in essential tremor. Cogn Behav Neurol. 2008;21:28–33. doi: 10.1097/WNN.0b013e3181684414. doi: 10.1097/WNN.0b013e3181684414. [DOI] [PubMed] [Google Scholar]
- 76.Molloy C, Conroy RM, Cotter DR, Cannon M. Is traumatic brain injury a risk factor for schizophrenia? A meta-analysis of case-controlled population-based studies. Schizophr Bull. 2011;37:1104–1110. doi: 10.1093/schbul/sbr091. doi: 10.1093/schbul/sbr091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Akdeniz C, Tost H, Meyer-Lindenberg A. The neurobiology of social environmental risk for schizophrenia: an evolving research field. Soc Psychiatry Psychiatr Epidemiol. 2014;49:507–517. doi: 10.1007/s00127-014-0858-4. doi: 10.1007/s00127-014-0858-4. [DOI] [PubMed] [Google Scholar]
- 78.Louis ED, Benito-León J, Bermejo-Pareja F. Neurological Disorders in Central Spain (NEDICES) Study Group. Population-based prospective study of cigarette smoking and risk of incident essential tremor. Neurology. 2008;70:1682–1687. doi: 10.1212/01.wnl.0000311271.42596.32. doi: 10.1212/01.wnl.0000311271.42596.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Benito-León J, Louis ED, Bermejo-Pareja F. Neurological Disorders in Central Spain (NEDICES) Study Group. Population-based case-control study of cigarette smoking and essential tremor. Mov Disord. 2008;23:246–252. doi: 10.1002/mds.21810. doi: 10.1002/mds.21810. [DOI] [PubMed] [Google Scholar]
- 80.Moylan S, Jacka FN, Pasco JA, Berk M. Cigarette smoking, nicotine dependence and anxiety disorders: a systematic review of population-based, epidemiological studies. BMC Med. 2012;10:123. doi: 10.1186/1741-7015-10-123. doi: 10.1186/1741-7015-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Minichino A, Bersani FS, Calò WK, Spagnoli F, Francesconi M, Vicinanza R, et al. Smoking behaviour and mental health disorders—mutual influences and implications for therapy. Int J Environ Res Public Health. 2013;10:4790–4811. doi: 10.3390/ijerph10104790. doi: 10.3390/ijerph10104790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Svansdottir E, Denollet J, Thorsson B, Gudnason T, Halldorsdottir S, Gudnason V, et al. Association of type D personality with unhealthy lifestyle, and estimated risk of coronary events in the general Icelandic population. Eur J Prev Cardiol. 2013;20:322–330. doi: 10.1177/2047487312441723. doi: 10.1177/2047487312441723. [DOI] [PubMed] [Google Scholar]
- 83.Louis ED, Benito-León J, Bermejo-Pareja F. Population-based study of baseline ethanol consumption and risk of incident essential tremor. J Neurol Neurosurg Psychiatry. 2009;80:494–497. doi: 10.1136/jnnp.2008.162701. doi: 10.1136/jnnp.2008.162701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bruce G, Curren C, Williams L. Type D personality, alcohol dependence, and drinking motives in the general population. J Stud Alcohol Drugs. 2013;74:120–124. doi: 10.15288/jsad.2013.74.120. doi: 10.15288/jsad.2013.74.120. [DOI] [PubMed] [Google Scholar]
- 85.Bohnert KM, Perron BE, Ashrafioun L, Kleinberg F, Jannausch M, Ilgen MA. Positive posttraumatic stress disorder screens among first-time medical cannabis patients: prevalence and association with other substance use. Addict Behav. 2014;39:1414–1417. doi: 10.1016/j.addbeh.2014.05.022. doi: 10.1016/j.addbeh.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cohen BE, Marmar C, Ren L, Bertenthal D, Seal KH. Association of cardiovascular risk factors with mental health diagnoses in Iraq and Afghanistan war veterans using VA health care. JAMA. 2009;302:489–492. doi: 10.1001/jama.2009.1084. doi: 10.1001/jama.2009.1084. [DOI] [PubMed] [Google Scholar]
- 87.Player MS, Peterson LE. Anxiety disorders, hypertension, and cardiovascular risk: a review. Int J Psychiatry Med. 2011;41:365–377. doi: 10.2190/PM.41.4.f. doi: 10.2190/PM.41.4.f. [DOI] [PubMed] [Google Scholar]
- 88.Cuffee Y, Ogedegbe C, Williams NJ, Ogedegbe G, Schoenthaler A. Psychosocial risk factors for hypertension: an update of the literature. Curr Hypertens Rep. 2014;16:483. doi: 10.1007/s11906-014-0483-3. doi: 10.1007/s11906-014-0483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gragnoli C. Hypothesis of the neuroendocrine cortisol pathway gene role in the comorbidity of depression, type 2 diabetes, and metabolic syndrome. Appl Clin Genet. 2014;7:43–53. doi: 10.2147/TACG.S39993. doi: 10.2147/TACG.S39993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Scarmeas N, Louis ED. Mediterranean diet and essential tremor. A case-control study. Neuroepidemiology. 2007;29:170–177. doi: 10.1159/000111579. doi: 10.1159/000111579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Blaine B. Does depression cause obesity? a meta-analysis of longitudinal studies of depression and weight control. J Health Psychol. 2008;13:1190–1197. doi: 10.1177/1359105308095977. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- 92.Bartoli F, Crocamo C, Alamia A, Amidani F, Paggi E, Pini E, et al. Posttraumatic stress disorder and risk of obesity: systematic review and meta-analysis. J Clin Psychiatry. 2015;76:e1253–261. doi: 10.4088/JCP.14r09199. doi: 10.4088/JCP.14r09199. [DOI] [PubMed] [Google Scholar]
- 93.Wiltink J, Beutel ME, Till Y, Ojeda FM, Wild PS, Münzel T, et al. Prevalence of distress, comorbid conditions and well being in the general population. J Affect Disord. 2011;130:429–437. doi: 10.1016/j.jad.2010.10.041. doi: 10.1016/j.jad.2010.10.041. [DOI] [PubMed] [Google Scholar]
- 94.Booth L, Williams L. Type D personality and dietary intake: the mediating effects of coping style. J Health Psychol. 2015;20:921–927. doi: 10.1177/1359105315573433. doi: 10.1177/1359105315573433. [DOI] [PubMed] [Google Scholar]
- 95.Wu Y, Ding Y, Tanaka Y, Zhang W. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci. 2014;11:1185–1200. doi: 10.7150/ijms.10001. doi: 10.7150/ijms.10001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lidfeldt J, Nerbrand C, Samsioe G, Agardh CD. Women living alone have an increased risk to develop diabetes, which is explained mainly by lifestyle factors. Diabetes Care. 2005;28:2531–2536. doi: 10.2337/diacare.28.10.2531. doi: 10.2337/diacare.28.10.2531. [DOI] [PubMed] [Google Scholar]
- 97.Yang H, Negishi K, Otahal P, Marwick TH. Clinical prediction of incident heart failure risk: a systematic review and meta-analysis. Open Heart. 2015;2:e000222. doi: 10.1136/openhrt-2014-000222. doi: 10.1136/openhrt-2014-000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nayor M, Vasan RS. Preventing heart failure: the role of physical activity. Curr Opin Cardiol. 2015;30:543–550. doi: 10.1097/HCO.0000000000000206. doi: 10.1097/HCO.0000000000000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Postma DS, Bush A, van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet. 2015;385:899–909. doi: 10.1016/S0140-6736(14)60446-3. doi: 10.1016/S0140-6736(14)60446-3. [DOI] [PubMed] [Google Scholar]
- 100.Tan DJ, Walters EH, Perret JL, Lodge CJ, Lowe AJ, Matheson MC, et al. Age-of-asthma onset as a determinant of different asthma phenotypes in adults: a systematic review and meta-analysis of the literature. Expert Rev Respir Med. 2015;9:109–123. doi: 10.1586/17476348.2015.1000311. doi: 10.1586/17476348.2015.1000311. [DOI] [PubMed] [Google Scholar]
- 101.Berthon BS, Wood LG. Nutrition and respiratory health—feature review. Nutrients. 2015;7:1618–1643. doi: 10.3390/nu7031618. doi: 10.3390/nu7031618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wranicz J, Szostak-Węgierek D. Health outcomes of vitamin D. Part II. Role in prevention of diseases. Rocz Panstw Zakl Hig. 2014;65:273–279. [PubMed] [Google Scholar]
- 103.Baena R, Salinas P. Diet and colorectal cancer. Maturitas. 2015;80:258–264. doi: 10.1016/j.maturitas.2014.12.017. doi: 10.1016/j.maturitas.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 104.Cuzick J, Thorat MA, Andriole G. Diet and colorectal cancer. Maturitas. 2015;80:258–264. doi: 10.1016/j.maturitas.2014.12.017. doi: 10.1016/j.maturitas.2014.12.017. [DOI] [PubMed] [Google Scholar]
- 105.Louis ED, Pellegrino KM, Factor-Litvak P, Rios E, Jiang W, Henchcliffe C, et al. Cancer and blood concentrations of the comutagen harmane in essential tremor. Mov Disord. 2008;23:1747–1751. doi: 10.1002/mds.22084. doi: 10.1002/mds.22084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cuzick J, Thorat MA, Andriole G. Prevention and early detection of prostate cancer. Lancet Oncol. 2014;15:e484–492. doi: 10.1016/S1470-2045(14)70211-6. doi: 10.1016/S1470-2045(14)70211-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lin PH, Aronson W, Freedland SJ. Nutrition, dietary interventions and prostate cancer: the latest evidence. BMC Med. 2015;13:3. doi: 10.1186/s12916-014-0234-y. doi: 10.1186/s12916-014-0234-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hochmuth F, Jochem M, Schlattmann P. Meta-analysis of aspirin use and risk of lung cancer shows notable results. Eur J Cancer Prev. 2016;25:259–268. doi: 10.1097/CEJ.0000000000000176. doi: 10.1097/CEJ.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 109.Cea Soriano L, Soriano-Gabarró M, García Rodríguez LA. The protective effect of low-dose aspirin against colorectal cancer is unlikely explained by selection bias: results from three different study designs in clinical practice. PLoS One. 2016;11:e0159179. doi: 10.1371/journal.pone.0159179. doi: 10.1371/journal.pone.0159179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Benito-León J, Louis ED, Bermejo-Pareja F. Neurological Disorders in Central Spain (NEDICES) Study Group. Reported hearing impairment in essential tremor: a population-based case-control study. Neuroepidemiology. 2007;29:213–217. doi: 10.1159/000112463. doi: 10.1159/000112463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ersoy L, Ristau T, Lechanteur YT. Nutritional risk factors for age-related macular degeneration. Biomed Res Int. 2014;2014:413150. doi: 10.1155/2014/413150. doi: 10.1155/2014/413150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Querques G, Souied EH. The role of omega-3 and micronutrients in age-related macular degeneration. Surv Ophthalmol. 2014;59:532–539. doi: 10.1016/j.survophthal.2014.01.001. doi: 10.1016/j.survophthal.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 113.Hu Y, Tang W, Liu R, Dong Z, Chen X, Pan M, et al. Higher prevalence of migraine in essential tremor: a case-control study. Cephalalgia. 2014;34:1142–1149. doi: 10.1177/0333102414531153. doi: 10.1177/0333102414531153. [DOI] [PubMed] [Google Scholar]
- 114.Hesdorffer DC, Hauser WA, Annegers JF, Cascino G. Major depression is a risk factor for seizures in older adults. Ann Neurol 2000; 47: 246–249. [PubMed] [Google Scholar]
- 115.Hesdorffer DC, Hauser WA, Olafsson E, Ludvigsson P, Kjartansson O. Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006;59:35–41. doi: 10.1002/ana.20685. doi: 10.1002/ana.20685. [DOI] [PubMed] [Google Scholar]
- 116.Dworetzky BA, Bromfield EB, Townsend MK, Kang JH. A prospective study of smoking, caffeine, and alcohol as risk factors for seizures or epilepsy in young adult women: data from the ‘Nurses’ Health Study II. Epilepsia. 2010;51:198–205. doi: 10.1111/j.1528-1167.2009.02268.x. doi: 10.1111/j.1528-1167.2009.02268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yun C, Xuefeng W. Association between seizures and diabetes mellitus: a comprehensive review of literature. Curr Diabetes Rev. 2013;9:350–354. doi: 10.2174/15733998113099990060. doi: 10.2174/15733998113099990060. [DOI] [PubMed] [Google Scholar]
- 118.So EL, Annegers JF, Hauser WA, O’Brien PC, Whisnant JP. Population-based study of seizure disorders after cerebral infarction. Neurology. 1996;46:350–355. doi: 10.1212/wnl.46.2.350. doi: 10.1212/WNL.46.2.350. [DOI] [PubMed] [Google Scholar]
- 119.Hesdorffer DC, Hauser WA, Annegers JF, Kokmen E, Rocca WA. Dementia and adult-onset unprovoked seizures. Neurology. 1996;46:727–730. doi: 10.1212/wnl.46.3.727. doi: 10.1212/WNL.46.3.727. [DOI] [PubMed] [Google Scholar]
- 120.Teunissen LL, Franssen H, Wokke JH, van der Graaf Y, Linssen WH, Banga JD, et al. Is cardiovascular disease a risk factor in the development of axonal polyneuropathy? J Neurol Neurosurg Psychiatry. 2002;72:590–595. doi: 10.1136/jnnp.72.5.590. doi: 10.1136/jnnp.72.5.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Thawani SP, Schupf N, Louis ED. Essential tremor is associated with dementia: prospective population-based study in New York. Neurology. 2009;73:621–625. doi: 10.1212/WNL.0b013e3181b389f1. doi: 10.1212/WNL.0b013e3181b389f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dodd JW. Lung disease as a determinant of cognitive decline and dementia. Alzheimers Res Ther. 2015;7:32. doi: 10.1186/s13195-015-0116-3. doi: 10.1186/s13195-015-0116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.McKee AC, Robinson ME. Military-related traumatic brain injury and neurodegeneration. Alzheimers Dement. 2014;10(Suppl.):S242–253. doi: 10.1016/j.jalz.2014.04.003. doi: 10.1016/j.jalz.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Yaffe K, Vittinghoff E, Lindquist K, Barnes D, Covinsky KE, Neylan T, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry. 2010;67:608–613. doi: 10.1001/archgenpsychiatry.2010.61. doi: 10.1001/archgenpsychiatry.2010.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sargent PA, Kjaer KH, Bench CJ, Rabiner EA, Messa C, Meyer J, et al. Brain serotonin1A receptor binding measured by positron emission tomography with [11C]WAY-100635: effects of depression and antidepressant treatment. Arch Gen Psychiatry. 2000;57:174–180. doi: 10.1001/archpsyc.57.2.174. doi: 10.1001/archpsyc.57.2.174. [DOI] [PubMed] [Google Scholar]
- 126.Rasul A, Johansson B, Lonne-Rahm SB, Nordlind K, Theodorsson E, El-Nour H. Chronic mild stress modulates 5-HT1A and 5-HT2A receptor expression in the cerebellar cortex of NC/Nga atopic-like mice. Arch Dermatol Res. 2013;305:407–413. doi: 10.1007/s00403-013-1325-x. doi: 10.1007/s00403-013-1325-x. [DOI] [PubMed] [Google Scholar]
- 127.Leuner B, Shors TJ. Stress, anxiety, and dendritic spines: what are the connections? Neuroscience. 2013;251:108–119. doi: 10.1016/j.neuroscience.2012.04.021. doi: 10.1016/j.neuroscience.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 128.Gounko NV, Swinny JD, Kalicharan D, Jafari S, Corteen N, Seifi M, et al. Corticotropin-releasing factor and urocortin regulate spine and synapse formation: structural basis for stress-induced neuronal remodeling and pathology. Mol Psychiatry. 2013;18:86–92. doi: 10.1038/mp.2012.43. doi: 10.1038/mp.2012.43. [DOI] [PubMed] [Google Scholar]
- 129.Lin CY, Louis ED, Faust PL, Koeppen AH, Vonsattel JP, Kuo SH. Abnormal climbing fibre-Purkinje cell synaptic connections in the essential tremor cerebellum. Brain. 2014;137:3149–3159. doi: 10.1093/brain/awu281. doi: 10.1093/brain/awu281. [DOI] [PMC free article] [PubMed] [Google Scholar]