Abstract
From 2013 to 2017 the Centers for Medicare and Medicaid Services redacted Medicare claims that included diagnosis or procedure codes related to substance abuse. The redaction policy was in effect as the Affordable Care Act and the opioid epidemic changed the health care landscape. The policy substantially altered prevalence estimates of common chronic conditions that co-occur with substance abuse.
Introduction
In 2013 a reinterpretation of the federal regulation governing the confidentiality of drug and alcohol treatment and prevention records caused the Centers for Medicare and Medicaid Services (CMS) to redact any health care encounter that included a diagnosis or procedure code related to substance abuse from the Medicare and Medicaid research identifiable files.1 This created important and difficult-to-identify gaps in claims data, especially those related to use of inpatient services.2 The research community was relieved when in 2017 the Substance Abuse and Mental Health Services Administration announced changes to the Confidentiality of Substance Use Disorder Patient Records regulations3 restoring access to previously redacted Medicaid and Medicare claims.4,5 However, this relief does not acknowledge the legacy left by incomplete files already in use for analyses spanning the implementation of the Affordable Care Act (ACA), a time period characterized by new insurance coverage, payment, and delivery models in health care and falling US life expectancy.
The gap in data coincides with the accelerating epidemic of drug overdose and resulting deaths, which increased from 41,000 in 2012 to 64,000 in 2016, largely due to opioids.6 Our analysis of Medicare data for 2007–14 demonstrates a steep drop in the prevalence of treatment for nonfatal opioid overdose (Exhibit 1). We observed a 26.4 percent decline in such overdoses in beneficiaries ages sixty-five and older and a 41.7 percent decline in beneficiaries younger than age sixty-five between 2012 and 2013. Unfortunately, this decline is an artifact of redaction, since any overdose event with a diagnosis or procedure related to substance abuse is absent from the data. At a time when the opioid epidemic accelerated, Medicare claims suggest the opposite.
Exhibit 1: Prevalence of treatment for nonfatal opioid overdose (per 100,000 Medicare beneficiaries), by age, 2007-14.
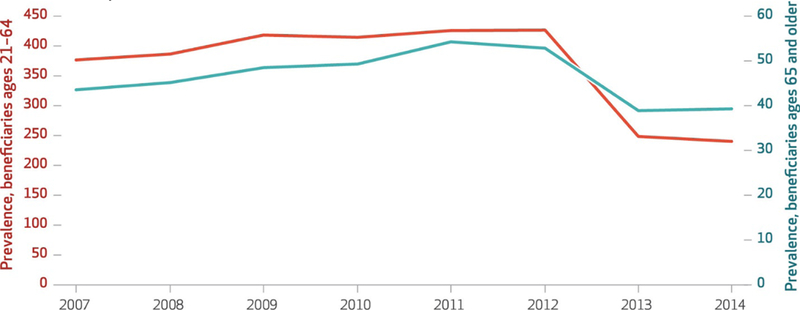
SOURCE Authors’ analysis of inpatient and outpatient claims for treatment in annual sample of 1.2 million fee-for-service Medicare beneficiaries aged 21 to 64 and 3.8 million beneficiaries aged 65 and older enrolled in parts A, B, and D (prescription drug plans) for full calendar year.
Despite laudable efforts by CMS to make “gap files” available, the months required to receive an amended data use agreement, high fees for gap files (the specific price depends on the agreement), and the time required to process files issued in a new format all create barriers to updating data. Researchers may be unwilling or unable to make the effort for studies that don’t specifically target addiction. But redaction can affect a wide range of studies. Prior analyses highlighting this issue were limited to Medicaid recipients2 or a subset of Medicare recipients with serious mental illness;7 the impact on the full Medicare population is unknown.
To more fully illustrate the impact of missing substance abuse claims in Medicare, we describe the effect of redaction on prevalence estimates of common chronic conditions and on inpatient use and spending overall, by age, and for selected inpatient diagnoses.
Study Data and Methods
We used complete fee-for-service Medicare claims for 2012, the last year of claims available before redaction was implemented. To estimate the impact of redaction, we created a new version of the 2012 cohort by removing any claim that included a substance abuse–related diagnosis or procedure code that was redacted in 2013, as specified by the Research Data Assistance Center (ResDAC).4 Our analysis used the full 2012 claims and the redacted version.
We estimated the prevalence of thirteen chronic conditions by age, comparing unredacted and redacted data (Exhibit 2). Following previously published work, we constructed chronic conditions based on International Classification of Diseases, Ninth Revision (ICD-9), codes corresponding to a subset of hierarchical classification categories used to risk adjust payments to Medicare Advantage health plans. We focused on a subset of conditions that are relatively common among Medicare beneficiaries or were likely to be affected by redaction.
Exhibit 2: Prevalence of chronic conditions among fee-for-service Medicare beneficiaries in 2012, with and without redaction.
| All (N = 31,808,792) | Younger than age 65 (n = 5,988,487) | Ages 65 and older (n = 25,820,305) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients missed | Patients missed | Patients missed | ||||||||||
| Condition | Unredacted | Redacted | No. | % | Unredacted | Redacted | No. | % | Unredacted | Redacted | No. | % |
| Hepatitis C | 0.52% | 0.46% | 19,350 | 11.7 | 1.94% | 1.66% | 16,768 | 14.5 | 0.19% | 0.18% | 2,582 | 5.2 |
| Other liver disease | 0.68 | 0.62 | 21,127 | 9.1 | 1.36 | 1.18 | 10,799 | 13.4 | 0.53 | 0.49 | 10,328 | 6.5 |
| Serious mental illness | 3.54 | 3.38 | 52,061 | 4.5 | 12.99 | 12.25 | 44,315 | 5.7 | 1.35 | 1.32 | 7,746 | 1.9 |
| Depression | 8.83 | 8.58 | 77,920 | 2.8 | 15.29 | 14.42 | 52,100 | 5.7 | 7.33 | 7.23 | 25,820 | 1.4 |
| Cerebral hemorrhage | 0.39 | 0.38 | 3,181 | 1.8 | 0.25 | 0.24 | 599 | 6.2 | 0.42 | 0.41 | 2,582 | 1.2 |
| Coronary artery disease | 4.32 | 4.24 | 24,288 | 1.9 | 3.20 | 3.01 | 11,378 | 6.0 | 4.58 | 4.53 | 12,910 | 1.2 |
| COPD | 9.63 | 9.49 | 41,429 | 1.4 | 9.46 | 9.07 | 23,355 | 4.2 | 9.66 | 9.59 | 18,074 | 0.8 |
| Dementia | 6.22 | 6.16 | 20,283 | 1.0 | 1.52 | 1.44 | 4,791 | 5.9 | 7.31 | 7.25 | 15,492 | 0.7 |
| CHF | 8.68 | 8.60 | 25,672 | 0.9 | 5.75 | 5.58 | 10,180 | 3.0 | 9.36 | 9.30 | 15,492 | 0.6 |
| Peripheral vascular disease | 8.93 | 8.87 | 17,514 | 0.7 | 5.33 | 5.21 | 7,186 | 2.2 | 9.76 | 9.72 | 10,328 | 0.5 |
| Cancer | 3.41 | 3.39 | 6,961 | 0.5 | 2.22 | 2.19 | 1,797 | 1.5 | 3.69 | 3.67 | 5,164 | 0.4 |
| Diabetes | 21.22 | 21.16 | 19,124 | 0.3 | 20.05 | 19.86 | 11,378 | 1.0 | 21.49 | 21.46 | 7,746 | 0.2 |
| HIV/AIDS | —a | —a | —a | —a | 1.28 | 1.25 | 1,797 | 2.2 | —a | —a | —a | —a |
SOURCE Authors’ analysis of fee-for-service Medicare claims for 2012. NOTES We used individual Hierarchical Condition Category codes to classify beneficiaries within conditions. We modified serious mental illness by removing International Classification of Diseases, Ninth Revision (ICD-9), codes for external causes (E*), and codes 296.2*, 296.3* (except for 296.24 and 296.34). Depression includes the following diagnoses: 300.4, 301.10–301.13, 309.1, 311, and 296.20–296.23, 296.25–296.33, 296.35, and 296.36. Hepatitis C includes the following diagnoses: 70.44, 70.41, 70.51, and 70.54. We classified a patient as having a condition if the patient had one inpatient claim or two physician visit claims at least seven days apart with a relevant diagnosis. COPD is chronic obstructive pulmonary disease. CHF is congestive heart failure.
Data not reported for beneficiaries ages sixty-five and older because of data suppression rules.
Next, we computed inpatient utilization in the redacted and unredacted data. We estimated inpatient admissions per 100 beneficiaries and inpatient spending per beneficiary, overall and by age (Exhibit 3). To characterize how redaction might affect studies that created diagnostic cohorts in inpatient settings, we calculated the population rates of admission per 100 beneficiaries (and, separately, psychiatric hospital admissions) for selected diagnoses likely to be affected (serious mental illness, depression, and hepatitis C) and less likely to be affected (diabetes) by redaction (Exhibit 4).
Exhibit 3: Inpatient admissions per 100 beneficiaries and average inpatient spending per beneficiary in 2012, with and without redaction.
| Inpatient admissions | Inpatient spending | ||||||
|---|---|---|---|---|---|---|---|
| Beneficiaries | Unredacted | Redacted | Difference | Unredacted | Redacted | Difference | Total underestimate |
| All | 42.0 | 39.8 | 5.2%**** | $4,417 | $4,203 | 4.8%** | $6.8 billion |
| Younger than age 65 | 44.8 | 37.5 | 16.3**** | 4,606 | 3,979 | 13.5** | 3.7 billion |
| Ages 65 and older | 41.3 | 40.3 | 2.4**** | 4,373 | 4,255 | 2.7** | 3.0 billion |
SOURCE Authors’ analysis of fee-for-service Medicare claims for 2012. NOTES Data are for inpatient stays at acute care hospitals, critical access hospitals, psychiatric hospitals, skilled nursing facilities, and long-term acute care hospitals, together with the very small number of stays in other inpatient settings captured in the Medicare Provider and Analysis Review file.
p < 0.05
p < 0.001
Exhibit 4: Inpatient admissions per 100 beneficiaries in 2012, with and without redaction, by type of facility and select inpatient diagnoses.
| Acute care hospital | Psychiatric hospital | |||||
|---|---|---|---|---|---|---|
| Co-occurring diagnosis | Unredacted | Redacted | Difference | Unredacted | Redacted | Difference |
| Serious mental illness | 0.703 | 0.573 | 18.5% | 0.494 | 0.349 | 29.3% |
| Depression | 6.226 | 5.663 | 9.0 | 0.489 | 0.310 | 36.6 |
| Hepatitis C | 0.637 | 0.430 | 32.4 | 0.055 | 0.013 | 76.3 |
| Diabetes | 15.208 | 14.609 | 3.9 | 0.309 | 0.241 | 22.1 |
SOURCE Authors’ analysis of fee-for-service Medicare claims for 2012. NOTE All differences in redacted and unredacted claims were significant (p < 0.001).
Study Results
Among all Medicare beneficiaries, the prevalence of chronic conditions related to substance abuse was lower with redaction (Exhibit 2). The prevalence of hepatitis C was understated by 11.7 percent, representing 19,085 patients. The prevalence of other liver disease was understated by 9.1 percent, with a similar number of missed patients. Redaction understated the prevalence of serious mental illness by 4.5 percent (50,894 patients) and depression by 2.8 percent (79,522 patients), but the prevalence of other conditions fell by less than 2 percent after redaction.
The underestimates of prevalence were greater for beneficiaries younger than age sixty-five. Redaction removed 14.5 percent of the hepatitis C population (16,768 patients) and 13.4 percent (10,799 patients) of the population with other liver disease. It also removed 5.7 percent (44,315 patients) of the population with serious mental illness and the same share (52,100 patients) of the population with depression.
Among the 6.3 million beneficiaries with inpatient claims (that is, inpatient admission), 7.1 percent had at least one inpatient claim redacted. As shown in Exhibit 3, inpatient admissions and inpatient spending were about 5 percent lower after redaction, resulting in a $6.8 billion underestimate of inpatient Medicare spending—a finding similar to ResDAC’s analyses.3 Compared with effects in older beneficiaries, effects were larger in the younger population, where admissions were reduced by 16.3 percent and spending was reported to be 13.5 percent ($3.7 billion) lower after redaction.
A sizable percentage of admissions were missing from redacted claims that included one of several diagnoses that commonly co-occur with substance abuse. There were 32.4 percent fewer admissions for hepatitis C after redaction, 18.5 percent fewer for serious mental illness, and 9.0 percent fewer for depression (Exhibit 4). For comparison, we also determined the percentage of admissions missing for hospitalizations related to diabetes, a common medical condition less likely to be comorbid with substance abuse. Only 3.9 percent of those admissions were missing after redaction.
In psychiatric hospitals, redaction removed 76.3 percent of admissions with a hepatitis C diagnosis and 36.6 percent of admissions with a depression diagnosis.
Discussion
Among Medicare beneficiaries, the redaction of substance abuse claims leads to underestimates of the prevalence of conditions that commonly occur with substance abuse and redaction leads to underestimates of overall inpatient use and spending.
The distortions caused by redaction were largest for Medicare beneficiaries younger than age sixty-five, who are primarily eligible for Medicare as a result of disability. In addition, admissions by comorbidity in inpatient settings were greatly underestimated, with even larger gaps between redacted and unredacted data for admissions to psychiatric hospitals.
Compared with one earlier study of Medicare beneficiaries with serious mental illness7 and compared with ResDAC’s analyses of redaction for all patients in Medicare,4 our study estimated how redaction affects the prevalence of conditions likely to be comorbid with substance abuse and the prevalence of inpatient admissions by diagnosis. Our study also quantified the concentrated effect of redaction among younger Medicare beneficiaries. Our results align with those of a related study that assessed redaction in a Medicaid population by comparing unredacted data for the period 2000–2006 and redacted data for 2007–10.2 However, our approach of comparing the same year of data with and without applying redaction eliminated the possibility that our findings stemmed from secular trends, coding practices, or true changes in prevalence.
Research files currently in use have a multiyear gap in the data for many high-cost, high-risk Medicare beneficiaries. The redacted Medicare claims are now available to qualified researchers, but the fees and time needed to obtain and process the files make it unclear whether researchers will backfill data for ongoing or future longitudinal studies that are likely to be biased by redaction.
Our analyses suggest important lessons for researchers, clinicians, health care administrators, and policy makers who rely on these data to understand how changing policies—such as those linked to the ACA—have influenced care. Researchers using CMS data purchased between 2013 and May 2017 should be aware of potential biases introduced by redaction. Audiences relying on research drawn from claims data should evaluate it with a critical eye toward potential biases, and policy makers must ask pointed questions about reports, peer-reviewed research, and analyses.
Our data suggest four important implications of the redaction of substance abuse claims for researchers using redacted Medicare claims. First, estimated comorbidity in the population age sixty-five and older will be minimally affected. Second, comorbidity in the population younger than age sixty-five will be understated, particularly for hepatitis C and mental illness. Third, redaction could distort evidence on the treatment and outcomes of two important patient groups: those with hepatitis C who are taking new drugs such as Sofosbuvir8 and those at risk of overdose related to opioid analgesic use.4 Fourth, research on inpatient use among Medicare beneficiaries younger than age sixty-five will be limited.
People analyzing claims, reading claims-based research, and making clinical or policy decisions using claims-based analyses may be unaware of gaps due to redaction, not only in data obtained from CMS but also in other data sets—such as state-run all-payer claims databases. The 2017 regulation making redacted data available gives unclear guidance about how such a database may receive substance-abuse related claims,5 so the databases may be incomplete. Furthermore, while ResDAC made the Medicare redaction approach public,4 commercial payers typically do not. Claims in an all-payer claims database may be redacted by some payers at the claim level, while other payers may drop all claims for enrollees for whom a substance abuse diagnosis or procedure is identified. Given that the methods of individual payers are opaque to people using the data, states could avoid costly mistakes by working with payers to make any gaps transparent.
To understand whether redaction may have influenced recent analyses using Medicare cohorts likely to be affected, we searched PubMed for articles published in peer-reviewed journals since 2016 using the term Medicare and one or more of the following additional terms: mental illness, opioid, substance abuse, depression, and hepatitis C. We identified at least nine studies that used Medicare data released during years when data were likely to be redacted (2012–14). Several authors noted that redaction had limited their ability to determine substance-abuse claims or comorbidity, but in other cases, as in our own analysis of opioid prescribing in Medicare, the 2012 data were complete.9–12 A recent economic analysis of opioid prescribing in Medicare acknowledged that redaction could affect estimates of nonfatal overdoses.13 Until now, even careful authors have had little information to help them estimate the magnitude of the potential bias. The lingering impact of redaction may continue to have significant policy implications beyond studies of addiction and the opioid epidemic because of the timing of the redacted claims, which coincided with two important events that are changing the face of health care and are under active study: implementation of the ACA and declining life expectancy in the United States.
References
- 1.Frakt AB, Bagley N. Protection or harm? Suppressing substance-use data. N Engl J Med. 2015;372(20):1879–81. [DOI] [PubMed] [Google Scholar]
- 2.Rough K, Bateman BT, Patorno E, Desai RJ, Park Y, Hernandez-Diaz S et al. Suppression of substance abuse claims in Medicaid data and rates of diagnoses for non–substance abuse conditions. JAMA. 2016;315(11):1164–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.42 CFR, Part 2.
- 4.Research Data Assistance Center. Redaction of substance abuse claims [Internet]. Minneapolis (MN): ResDAC; 2017. June 5 [cited 2018 Mar 9]. Available from: https://www.resdac.org/resconnect/articles/203 [Google Scholar]
- 5.Bagley N Good news for health-services research. Incidental Economist; [blog on the Internet]. 2017. March 31 [cited 2018 Mar 9]. Available from: http://theincidentaleconomist.com/wordpress/good-news-for-health-services-research/ [Google Scholar]
- 6.Ahmad FB, Rossen LM, Spencer MR, Warner M, Sutton P. Provisional drug overdose death counts [Internet]. Hyattsville (MD): [last updated 2018 Feb 9; cited 2018 Mar 9]. Available from: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- 7.Roberto P, Brandt N, Onukwugha E, Stuart B. Redaction of substance abuse claims in Medicare research files affects spending outcomes for nearly one in five beneficiaries with serious mental illness. Health Serv Res. 2017;52(3):1239–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neuman T, Hoadley J, Cubanski J. The cost of a cure: Medicare’s role in treating hepatitis C. Health Affairs Blog; [blog on the Internet]. 2014. June 5 [cited 2018 Mar 9]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20140605.039396/full/ [Google Scholar]
- 9.Meara E, Horwitz JR, Powell W, McClelland L, Zhou W, O’Malley AJ et al. State legal restrictions and prescription-opioid use among disabled adults. N Engl J Med. 2016;375(1):44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Busch AB, Huskamp HA, Kreider AR, McWilliams JM. Medicare accountable care organizations and antidepressant use by patients with depression. Psychiatr Serv. 2017;68(11):1193–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Busch AB, Huskamp HA, McWilliams JM. Early efforts by Medicare accountable care organizations have limited effect on mental illness care and management. Health Aff (Millwood). 2016;35(7):1247–56. [DOI] [PubMed] [Google Scholar]
- 12.Mehrotra A, Huskamp HA, Souza J, Uscher-Pines L, Rose S, Landon BE et al. Rapid growth in mental health telemedicine use among rural Medicare beneficiaries, wide variation across states. Health Aff (Millwood). 2017;36(5):909–17. [DOI] [PubMed] [Google Scholar]
- 13.Buchmueller TC, Carey C. The effect of prescription drug monitoring programs on opioid utilization in Medicare. Am Econ J: Econ Pol. 2018;10(1):77–112. [Google Scholar]


