Introduction
Primary cutaneous lymphomas are a heterogeneous group of lymphoid malignancies and are the second most common group of extranodal non-Hodgkin lymphoma (NHL) following gastrointestinal lymphomas.1 NHL involving the female genitalia is unusual, posing diagnostic and therapeutic challenges.2–4 Rare cases of vulvar NHL presenting as a vulvar mass were mostly diagnosed as diffuse large B-cell lymphoma and had an aggressive course.3,5 Cases of cutaneous T-cell lymphoma (CTCL) involving the vulva have been rarely reported. We herein describe three patients with mycosis fungoides (MF) tumors involving the labia majora and discuss our therapeutic approach.
Report of cases
Three consecutive female patients with MF and vulvar involvement by tumors were recently diagnosed and treated in our institution. The first case was a 30-year-old female with a 10-year history of MF stage IIA who had been previously treated with topical steroids, phototherapy, interferon and local radiation. Partial response was achieved with oral bexarotene 450 mg daily until she presented with worsening of plaque disease on her skin and a rapidly growing tumor involving the external genitalia. Physical examination revealed pink to violaceous plaques with overlying scale on the extremities, buttocks and vulva and a 2 centimeters tumor on her right labia majora (Figure 1-A). A biopsy of the tumor showed histopathological findings consistent with tumor stage MF with monoclonal T-cell receptor (TCR) gene rearrangements identical to those identified in a forearm MF lesion. The patient was staged as IIB. CD30 staining of the tumor tissue highlighted larger lymphocytes and therefore brentuximab vedotin (BV) treatment was initiated; however, only partial response was achieved and a new ulcerated tumor developed on the left labia. The patient was referred for palliative electron beam radiotherapy (RT) to the left labia (14 Gy given in 7 fractions given 2 fractions per week) with complete response, followed by total skin electron beam (TSEB) radiotherapy to the rest of her skin.
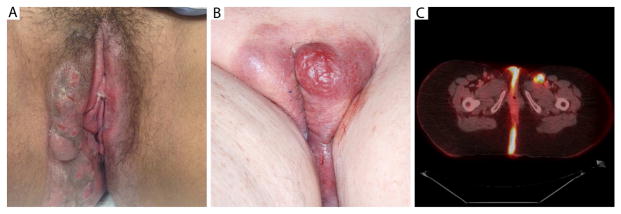
Figure 1. Clinical presentation and Positron Emission Tomography–Computed Tomography (PET-CT) scan of vulvar mycosis fungoides tumors.
A, Erythematous 4–5 cm tumor with focal erosions involving the right labia majora and erythematous eroded plaques on the inner right thigh and perineal area in patient 1.
B, A bright red, 3 cm tumor on the left labia majora and red-violet colored plaques involving labia and perineal area bilaterally in patient 2.
C, Marked Fluoro-deoxy-glucose (FDG)-avid right labial and bilateral gluteal cutaneous/subcutaneous infiltration and left inguinal lymph node as shown on positron emission tomography (PET-CT) scan in patient 3.
The second case was an 85-year-old female patient with a 5-year history of stage IIB MF and large cell transformation, who was in near-complete remission with maintenance therapy of oral bexarotene (150 mg daily) after being treated with TSEB therapy and additional radiation doses to the perineum and the gluteal folds. The patient developed recurrent patches and plaques on her trunk and extremities and bexarotene dose was increased (300 mg daily). Two months later the patient returned to our clinic complaining of a rapidly growing labial mass. Physical examination revealed erythematous plaques on her trunk and red-purple tumors involving the vulva (Figure 1-B). A biopsy was preformed from the labial mass confirming the diagnosis of MF. The patient received photon radiotherapy to the vulvar area (25 Gy in 10 fractions given every other day) with an almost complete response and significant alleviation of symptoms. Shortly after the treatment was completed, the patient developed pneumonia and expired.
The third case was a 52-year-old woman who was diagnosed three years earlier with MF stage IIB, and was treated with romidepsin, local radiation, chemotherapy (gemcitabine/doxorubicin), oral bexarotene, BV, and TSEB with additional RT doses to the groin area. While on maintenance bexarotene (300 mg daily), the patient complained of a new painful tumor on her labia. On physical examination, hyperpigmented and erythematous patches and plaques were seen on the trunk, extremities, inguinal and intergluteal folds. On the right labia majora a red tumor was present. Based on the clinical appearance, the patient was referred for localized RT.
Prior to treatment a PET scan was performed showing increased cutaneous FDG-avid lesions in the gluteal and perineal areas (Figure 1-C). The patient was treated with electron beam radiotherapy, 20 Gy in 10 fractions given every other day to the right labia and intergluteal fold with significant local improvement. The patient was enrolled to a clinical trial of an experimental targeted therapy, with initial improvement but eventual progression of generalized skin disease, but not in the genitalia.
Discussion
MF is an indolent NHL and is the most common type of CTCL. It typically presents on sun-protected body areas, involving the chest, inner arms, buttocks, lower trunk and groin,6 and involvement of the genitalia by MF has not been well characterized. The labia majora can be potentially involved by CTCL; however, there are only rare reports in the literature of such cases.
All three cases reported herein had a long history of MF before presenting with a vulvar MF tumor, and cases 2 and 3 had developed other tumors previously. Bakar et al described a woman in her 30s with a 7-year history of MF stage IA who presented with a new mass involving the left labia majora that was diagnosed as an MF tumor. The tumor appeared during the postpartum period, and was successfully treated with low-dose intermittent local RT.7 In another report, MF was initially diagnosed in a female in her 50s with solitary labial swelling and no prior history of MF. The vulvar lesion was excised with no evidence of recurrence.8 Two cases had non-tumorous MF vulvar lesions, presenting as a chronic fissure9 and vulvar pruritus and dyspareunia.3 Primary cutaneous anaplastic large cell lymphoma presenting as an ulcerated mass on the labia majora has also been reported. This patient was treated with a short chemotherapy course and local RT to achieve complete response.10
Because of its rarity, lymphoma in general and CTCL in particular are not usually considered in the differential diagnosis of vulvar tumors, and inflammatory processes and other malignancies present more commonly on the external female genitalia.3,11 In a patient with CTCL with a history of a rapidly growing genital mass, vulvar involvement by cutaneous lymphoma should be considered and histological confirmation obtained.
CTCLs are highly radiosensitive, and localized RT is a very effective treatment approach for localized or large plaques and tumor nodules in both early- and advanced-stage MF.12 For local palliation, doses between 8–30 Gy are recommended in order to achieve complete response, and tumor stage and large cell transformation require the higher doses. The dose can be divided to fraction sizes of 3 to 5 Gy that are generally very well tolerated.13 16 Gy in eight fractions was given to a previously reported patient with vulvar MF tumor to achieve complete remission.7 Male patients may also develop genital involvement by MF: in one case, a penile ulcerated MF lesion was treated with excision, local RT (27 Gy in 15 fractions) and systemic therapies with complete response.14 In our case-series excellent results were achieved with localized RT to the vulva area (14–25 Gy doses given in 7–10 fractions).
In our cases, the vulvar tumors accompanied flare of diffuse extragenital plaque disease. Despite the excellent local response to RT of the genital area, in two patients the extragenital disease was resistant to therapies and progressed, and the third patient died from pneumonia shortly after RT. Although our case-series is small, our findings support prior reports on aggressive disease in NHL involving the vulva3; however larger series are needed to confirm this association.
Conclusions
MF patients should be routinely questioned about genital involvement, appropriate physical examination of the genital areas should be performed, and suspicious new lesions should be biopsied. Excellent local control can be achieved with low dose RT.
CLINICAL PRACTICE POINTS.
Involvement of the female external genitalia by cutaneous T-cell lymphoma (CTCL) and mycosis fungoides (MF) is rare and difficult to diagnose and treat.
Here we report three consecutive female patients with a history of MF who presented with new tumors involving the labia majora. In all cases, a painful genital tumor accompanied an exacerbation of extra-genital diffuse plaque disease with an aggressive course.
All three patients were treated with localized electron or photon radiotherapy (RT) to the vulvar area (14–25 Gy given in 7–10 fractions) with an excellent local response.
A vulvar tumor in a patient with known history of MF should raise a high suspicion for genital involvement by disease and skin biopsy should be considered.
Acknowledgments
Funding sources: This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748. The above funders were not involved in the study design, data collection, data analysis, manuscript preparation or publication decisions.
Footnotes
Conflict of interest disclosures: Dr Horwitz has consulting and/or research relationships with Celgene, Millenium Pharmaceuticals/Takeda, Kyowa-Hakka-Kirin, Forty-Seven, Seattle Genetics, Infinity Pharmaceuticals, HUYA, Spectrum Pharmaceuticals, ADCT therapeutics, and Aileron Therapeutics. Dr Moskowitz has research, speaking, and advisory board relationships with Bristol-Myers Squibb, Takeda, and Seattle Genetics. Drs Geller, Pitter, Yahalom and Myskowski have no conflicts of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Willemze R, Kerl H, Sterry W, et al. EORTC classification for primary cutaneous lymphomas: a proposal from the Cutaneous Lymphoma Study Group of the European Organization for Research and Treatment of Cancer. Blood. 1997;90(1):354–371. [PubMed] [Google Scholar]
- 2.Cheng MH, Chao HT, Wang PH. Vulvar metastasis as the initial presentation of non-Hodgkin’s lymphoma: a case report. J Reprod Med. 2007;52(11):1065–1066. [PubMed] [Google Scholar]
- 3.Vang R, Medeiros LJ, Malpica A, Levenback C, Deavers M. Non-Hodgkin’s lymphoma involving the vulva. Int J Gynecol Pathol. 2000;19(3):236–242. doi: 10.1097/00004347-200007000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Kosari F, Daneshbod Y, Parwaresch R, Krams M, Wacker HH. Lymphomas of the female genital tract: a study of 186 cases and review of the literature. Am J Surg Pathol. 2005;29(11):1512–1520. doi: 10.1097/01.pas.0000178089.77018.a9. [DOI] [PubMed] [Google Scholar]
- 5.Tjalma WA, Van de Velde AL, Schroyens WA. Primary non-Hodgkin’s lymphoma in Bartholin’s gland. Gynecol Oncol. 2002;87(3):308–309. doi: 10.1006/gyno.2002.6828. [DOI] [PubMed] [Google Scholar]
- 6.Jawed SI, Myskowski PL, Horwitz S, Moskowitz A, Querfeld C. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sezary syndrome): part I. Diagnosis: clinical and histopathologic features and new molecular and biologic markers. J Am Acad Dermatol. 2014;70(2):205e201–216. doi: 10.1016/j.jaad.2013.07.049. quiz 221-202. [DOI] [PubMed] [Google Scholar]
- 7.Bakar O, Sahin S, Cetinozman F, Willemze R, Tezcanli E, Cetin ED. Tumor-stage mycosis fungoides of the vulva successfully treated with local low-dose radiotherapy. Dermatol Ther. 2015;28(1):36–39. doi: 10.1111/dth.12181. [DOI] [PubMed] [Google Scholar]
- 8.Buras AL, McSwain AN, Qin Y, Meunier JK. Primary mycosis fungoides of the vulva: The first reported case. Gynecol Oncol Rep. 2015;12:7–8. doi: 10.1016/j.gore.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reichman O, Sobel JD, Bentley G. Chronic vulvar fissure--a rare manifestation of mycosis fungoides. J Low Genit Tract Dis. 2010;14(1):65–67. doi: 10.1097/LGT.0b013e31819d09ad. [DOI] [PubMed] [Google Scholar]
- 10.Koh LP, Wong LC, Ng SB, Poon ML, Low JJ. Primary cutaneous anaplastic large cell lymphoma of the vulva: a typical cutaneous lesion with an ‘atypical’ presenting site. Int J Hematol. 2009;90(3):388–391. doi: 10.1007/s12185-009-0395-1. [DOI] [PubMed] [Google Scholar]
- 11.Lagoo AS, Robboy SJ. Lymphoma of the female genital tract: current status. Int J Gynecol Pathol. 2006;25(1):1–21. doi: 10.1097/01.pgp.0000183049.30212.f9. [DOI] [PubMed] [Google Scholar]
- 12.Whittaker S, Hoppe R, Prince HM. How I treat mycosis fungoides and Sezary syndrome. Blood. 2016;127(25):3142–3153. doi: 10.1182/blood-2015-12-611830. [DOI] [PubMed] [Google Scholar]
- 13.Specht L, Dabaja B, Illidge T, Wilson LD, Hoppe RT. Modern radiation therapy for primary cutaneous lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2015;92(1):32–39. doi: 10.1016/j.ijrobp.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 14.O’Brien JS, Manning T, Perera M, Prince HM, Lawrentschuk N. Blueprint unknown: a case for multidisciplinary management of advanced penile mycosis fungoides. Can J Urol. 2017;24(6):9139–9144. [PubMed] [Google Scholar]