Abstract
Purpose
This study assessed the feasibility of near-infrared (NIR) imaging with indocyanine green (ICG) in investigating the completeness of laparoscopic lymph node (LN) dissection for gastric cancer.
Materials and Methods
Patients scheduled for laparoscopic gastrectomy for treating gastric cancer were enrolled in the study. After intraoperative submucosal ICG injection (0.05 mg/mL), LN dissection was performed under conventional laparoscopic light. After dissection, the LN stations of interest were examined under the NIR mode to locate any extra ICG-stained (E) tissues, which were excised and sent for pathologic confirmation. This technique was tested in 2 steps: infra-pyloric LN dissection (step 1) and review of all stations after proper radical node dissection (step 2).
Results
In step 1, 15 patients who underwent laparoscopic pylorus-preserving gastrectomy (LPPG) and 15 patients who underwent laparoscopic distal gastrectomy (LDG) were examined. Seven and 2 E-tissues were obtained during LPPG and LDG, respectively. From the retrieved E-tissues, 1 and 0 tissue obtained during LPPG and LDG, respectively, was confirmed as LN. In step 2, 20 patients were enrolled (13 D1+ dissection and 7 D2 dissection). Six E-tissues were retrieved from 5 patients, and 1 tissue was confirmed as LN in the pathologic review. Overall, 15 E-tissues were detected and removed, and 2 tissues were confirmed as LNs in the pathologic review. Both nodes were from LN station #6, with 1 case each in the LDG and LPPG groups.
Conclusions
NIR imaging may provide additional node detection during laparoscopic LN dissection for gastric cancer, especially in the infra-pyloric area.
Keywords: Indocyanine green, NIR, Diagnostic imaging, Lymph nodes, Gastric cancer
INTRODUCTION
Most cancer experts believe that adequate lymph node (LN) dissection provides a survival benefit in the treatment of gastric cancer [1]. However, multiple vasculatures with complex lymphatic channels within the stomach anatomy increase the difficulty in performing a radical gastrectomy without postoperative morbidity [2]. Because a high level of proficiency is required in performing radical LN dissection, additional identification of potentially involved LNs may improve surgical outcomes [3].
We previously reported that injecting diluted indocyanine green (ICG) followed by near-infrared (NIR) imaging was clinically applicable for identifying LNs adjacent to the injection site in a preclinical animal model [4]. ICG injection aided not only in the detection of LNs but also in the detection of lymphatic channels; thus, it is a method with low toxicity and hypersensitivity that could help identify the complex anatomy of the perigastric lymphatic structures [4]. Although ICG showed rapid and extensive dispersion with adequate titration and quantification, a NIR-facilitated view can be transmitted to the operating monitor to allow the identification of anatomical structures only where the dye is present.
The aim of this study was to assess the feasibility of NIR imaging with ICG injection in investigating the completeness of laparoscopic LN dissection for gastric cancer.
MATERIALS AND METHODS
Patients
Patients scheduled for laparoscopic gastrectomy as a primary treatment of gastric cancer at Seoul National University Hospital between January 2015 and March 2016 were considered eligible for the study. All surgical procedures were performed in accordance with the preoperative diagnosis regardless of the findings on the NIR view. This study was approved by the Institutional Review Board of Seoul National University Hospital, Seoul, Korea (approval No. 1410-142-622). Written consent was obtained from all patients before any procedure. All procedures were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration.
Study design
A prospective nonrandomized study was designed to investigate the additional role of NIR imaging with ICG in gastric surgery. With this novel technique, the completeness of LN dissection was assessed in 2 steps. First, it was applied in the assessment of the infra-pyloric LN station (#6 LN), as it is considered the most challenging step in node dissection in gastric cancer surgery [5]. In this step, the same number of patients undergoing laparoscopic pylorus-preserving gastrectomy (LPPG) and those undergoing laparoscopic distal gastrectomy (LDG) were enrolled, and the completeness of LN station #6 was reviewed. To focus on LN station #6, ICG was injected at 4 sites (anterior, posterior, lesser, and greater curvature) in the wall of the antrum through intraoperative endoscopy followed by laparoscopic dissection under white light. After the dissection, the infra-pyloric area was observed using NIR imaging. Additionally, ICG-stained tissues (6E) were resected and sent for pathologic review in the same manner.
In the second step, all stations involved in proper LN dissection (D1+ or D2) for distal gastrectomy (1, 3, 4sb, 4d, 5, 6, 7, 8, 9, and/or 11p, 12) were studied. ICG was injected at 3 sites (antrum, angle, and low body) along the lesser curvature and at 3 sites of the greater curvature that were contralateral to the injection sites of the lesser curvature. After performing LN dissections in all the intended stations, the resected stations were reviewed using NIR imaging. Additional residual soft tissues (E) with ICG uptake at the dissected stations were resected and sent for pathologic evaluation.
Preoperative workup
The diagnosis in all patients was based on pathologic confirmation from endoscopic biopsy of the primary tumor. Endoscopic ultrasound and computerized tomography with a stomach insufflation protocol was performed in all cases for preoperative staging. At 1 or 3 days before surgery, all patients underwent endoscopy for preoperative endoscopic clipping, performed by gastroenterologists, to mark the lesions of early gastric cancer. Endoscopic clipping is the conventional method to mark the location of the tumor in our practice, and it is performed for patient safety as a salvage procedure to facilitate intraoperative endoscopy and as a landmark to avoid while performing submucosal ICG injection.
ICG
The injection procedure used in this study was based on the results of a previous preclinical study [4]. In that study, the optimal setting for ICG preparation for LN biopsy was injecting 1 mL of a 0.05–0.1 mg/mL solution into 4–5 sites. In our study, 2.5 mg/mL ICG solution (Diagnogreen Inj; Daiichi Sankyo Propharma Co. Ltd., Osaka, Japan) was diluted with 0.9% normal saline and was prepared at a dose of 0.05 mg/mL. The solution (1 mL) was injected at each site 15 minutes before dissection.
Surgical procedure and NIR system
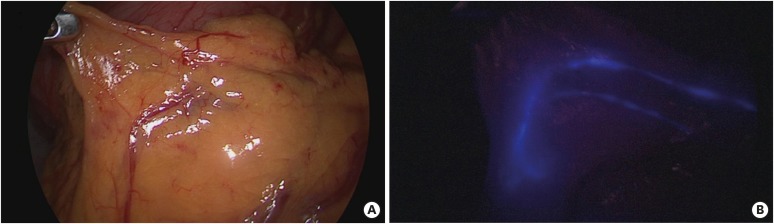
A laparoscopic system with NIR functionality (Karl Storz GmbH & Co. KG, Tuttlingen, Germany) was used in this study. The conversion from white light to the ICG mode was accomplished using a foot pedal. The images were generated using a full high-definition camera system (IMAGE1 S™ NIR-ICG system; Karl Storz GmbH & Co. KG) connected to a laparoscope with a 10-mm, 30° scope (Hopkins telescope; Karl Storz GmbH & Co. KG). After activating the NIR mode, white light was deactivated, and NIR vision was turned on, creating a NIR fluorescence imaging (NIR-ICG) mode (Figs. 1 and 2).
Fig. 1. View of the infra-pyloric area 5 minutes after endoscopic submucosal injection of (4 sites of the antrum): (A) under white light and (B) in NIR mode.
ICG = indocyanine green; NIR = near-infrared.
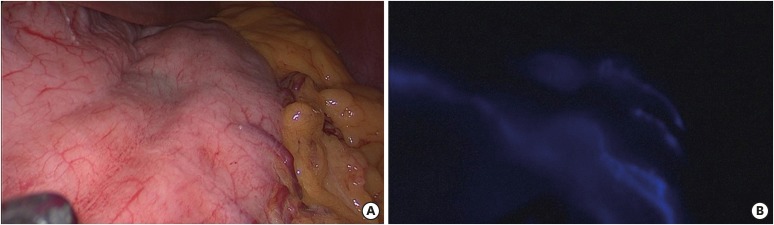
Fig. 2. Bidirectional dispersion of fluorescence after endoscopic submucosal injection of ICG on the anterior wall of the stomach: (A) under white light and (B) in NIR mode.
ICG = indocyanine green; NIR = near-infrared.
In all patients, 15 minutes after the gastroscopic submucosal injections, the NIR mode was activated to confirm the quality of the ICG injection and to identify the diffusion into the lymphatic channels.
The NIR mode was turned off during the laparoscopic dissection phase. After node dissections were completed, the NIR mode was activated, and each node station was closely reviewed. Every additional tissue with ICG uptake was collected and sent for histologic confirmation. The criterion for tissue collection was a brighter appearance of the tissue in the NIR mode during the laparoscopic view.
All surgical procedures were performed based on the Japanese Gastric Cancer Treatment Guidelines, and ex vivo LN dissections were performed according to the definition of gastric carcinoma based on the Japanese classification [6,7].
Data collection
Demographic, surgical, clinicopathologic, and clinical outcomes were recorded. The duration of intraoperative gastroscopy was recorded as the time from intubation to extubation of the gastroscope. All postoperative complications were recorded and graded using the Clavien-Dindo classification. Any findings that were considered an adverse event related to ICG injection were collected and recorded.
The chi-square was calculated, and Student's t-test was used for comparison of means. All tests were 2 sided, and P-values of <0.05 were considered significant. All statistical analyses were performed using IBM SPSS Statistics version 21 (IBM Inc., Chicago, IL, USA).
RESULTS
Demographics and clinical outcomes
Among the 52 patients who were enrolled for NIR imaging-assisted radical laparoscopic gastrectomy, 2 patients were excluded from the study owing to safety concerns. One patient underwent limited LN dissection because of severe perigastric variceal engorgement due to liver cirrhosis. Another patient was excluded from the study owing to extreme anatomical variation.
After excluding the above patients, the completeness of infra-pyloric LN dissection in 15 patients who underwent LPPG were compared with that of 15 patients who underwent LDG. The completeness of LN dissection in all dissected stations was reviewed in 20 patients (D1+ dissection in 13 patients and D2 dissection in 7 patients). All patients underwent scheduled treatment without conversion to the open method or total gastrectomy. No adverse events or additional morbidity due to ICG injection or the NIR camera system were reported.
Table 1 shows the demographic characteristics of the examined patients. The mean patient age was 58±11.5 years, most of the patients (72%) were men, and mean body mass index (BMI) was 24.2±2.5 kg/m2. Twenty patients who underwent LDG were reviewed for completeness of node dissection in all dissected stations.
Table 1. Demographics and clinical outcome.
| Variables | Mean±SD | No. (%) | |
|---|---|---|---|
| Demography | |||
| Age (yr) | 58.0±11.5 | ||
| Sex (M:F) | 36:14 | ||
| BMI (kg/m2) | 24.3±2.5 | ||
| Tumor location | |||
| Upper | 0 (0) | ||
| Middle | 13 (26) | ||
| Lower | 37 (74) | ||
| Preoperative clinical stage | |||
| Early gastric cancer (T1) | 43 (86) | ||
| Advanced gastric cancer (>T1) | 7 (14) | ||
| Mean postoperative stay (day) | 9.5±5.2 | ||
| Postoperative complication (Clavien-Dindo classification) | 3 (6) | ||
| II. Gastric stasis | 1 (2) | ||
| II. Postoperative ileus | 1 (2) | ||
| IIIa. Pyloric spasms (in LPPG) | 1 (6.7) | ||
| Adverse events related to ICG (late and early) | 0 | ||
SD = standard deviation; M = male; F = female; BMI = body mass index; LPPG = laparoscopic pylorus-preserving gastrectomy; ICG = indocyanine green.
A total of 3 complications were reported: 1 case of gastric stasis after distal gastrectomy, 1 case of postoperative ileus, and 1 case of pyloric spasm after LPPG. The patient with pyloric spasm required fluoroscopy-guided balloon dilatation, and the pyloric spasm resolved after a single session of the intervention.
Fluorescence-guided imaging
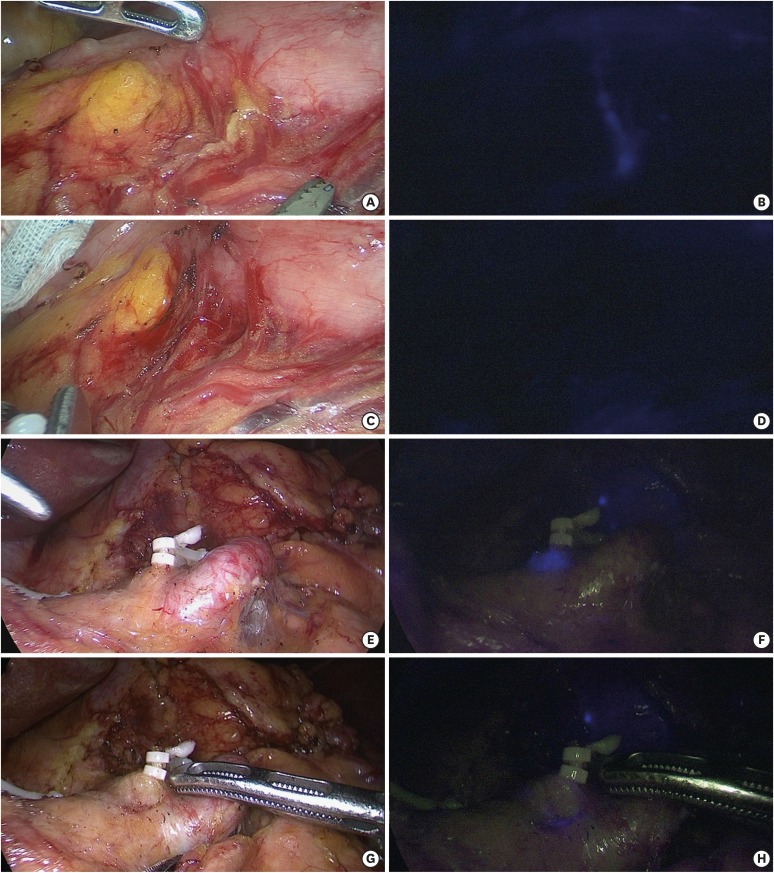
The mean time to the detection of the first node with ICG uptake by using the NIR camera was 178.8±86.1 seconds. In the laparoscopic NIR view, the injected sites were immediately identifiable as a blue area of fluorescence that extended into the thin lymphatic channels running along and inside the gastric viscera. The merging of lymphatic streams is shown in Fig. 1. ICG drained into the laminal flow within the visceral walls of the stomach before it reached the closest LNs and nearby lymphatic channels. When submucosal injection was performed on the anterior wall of the stomach, ICG drained in multiple directions (Fig. 2). Tissues with ICG uptake could be detected with good resolution by using the NIR system, and tissues with ICG uptake other than LNs were also detected and removed (Fig. 3).
Fig. 3. Comparison of additional tissue dissection guided with a NIR camera. Before dissection of the near infra-artery in a case of LPPG: (A) under white light view and (B) in NIR mode. After dissection: (C) under white light view and (D) confirmation with the NIR mode. After dissection, tissue with additional ICG uptake (E-tissue) in the left gastric artery in LDG: (E) under white light and (F) in NIR mode. After additional dissection of the E-tissue (G) under white light and (H) in NIR mode.
NIR = near-infrared; LPPG = laparoscopic pylorus-preserving gastrectomy; ICG = indocyanine green; LDG = laparoscopic distal gastrectomy.
Step 1. Completeness of infra-pyloric dissection
In this step, 15 patients who underwent LPPG and 15 patients who underwent LDG were enrolled. In these patients, the male-to-female ratio was 11:4 and the mean age was 58.7±10.3 (41–81) years. The mean operative time was 242.8±42.7 minutes for the LPPG cases and 233.9±50.2 minutes for the LDG cases (P=0.601). The mean postoperative hospital stay was 9.9±6.1 days for the LPPG cases and 9.5±6.0 days for the LDG cases (P=1.000).
Table 2 shows the comparative results of LN dissection in the LPPG and LDG groups. BMI showed no difference between the groups. The total numbers of retrieved LNs were 41.4±12.0 for LPPG and 36.6±14.5 for LDG (P=0.333). The numbers of retrieved infra-pyloric LNs were 6.7±3.0 for LPPG and 4.4±3.2 for LDG (P=0.058).
Table 2. Assessment of completeness of LN dissection confirmed using the near-infrared system: assessment of infra-pyloric LN dissection in LPPG and LDG.
| Variables | Mean±SD | No. (%) | P-value | |
|---|---|---|---|---|
| BMI (kg/m2) | 0.801 | |||
| LPPG | 24.2±2.4 | 15 | ||
| LDG | 24.4±2.6 | 15 | ||
| Retrieved LN numbers | 0.333 | |||
| LPPG | 41.4±12.0 | |||
| LDG | 36.6±14.5 | |||
| Retrieved LNs in station #6 | 0.058 | |||
| LPPG | 6.7±3.0 | |||
| LDG | 4.4±3.2 | |||
| E-tissues in LNs in station #6 | ||||
| LPPG | 7 (46.7) | |||
| LDG | 2 (13.3) | |||
| Pathology-confirmed LNs from E-tissues | ||||
| LPPG | 1 (6.7), NT | |||
| LDG | 0 | |||
| Operative time (min) | 0.601 | |||
| LPPG | 242.8±43.0 | |||
| LDG | 233.9±50.0 | |||
LN = lymph node; LPPG = laparoscopic pylorus-preserving gastrectomy; LDG = laparoscopic distal gastrectomy; SD = standard deviation; BMI = body mass index; NT = no tumor.
Concerning E-tissues, there were 7 E-tissues in the LPPG group and 2 in the LDG group (P=0.109). Among the additionally retrieved tissues, there was 1 LN in the LPPG group that contained no tumor, whereas no LN was found in the LDG group in pathologic review.
Step 2. Completeness of LN dissection in all dissected stations in LDG
In this step (n=20 patients), the mean operative time was 207.7±56.4 minutes for the D1+ group and 236.7±53.4 minutes for the D2 group (Table 3). The mean numbers of retrieved LNs were 37.2±12.6 for D1+ dissection and 39.1±11.1 for D2 dissection (P=0.686).
Table 3. Assessment of completeness of LN dissection confirmed using the near-infrared system: assessment of all stations in LDG.
| Variables | Mean±SD | No. (%) | P-value | |
|---|---|---|---|---|
| Extent of LN dissections | ||||
| D1+ | 13 (65) | |||
| D2 | 7 (35) | |||
| Retrieved LN numbers | 0.686 | |||
| D1+ | 37.2±12.6 | |||
| D2 | 39.1±11.1 | |||
| NIR system-detected E-tissues | 6 (30) | |||
| Station #1 | 1 (5) | |||
| Station #3 | 1 (5) | |||
| Station #4sb | 1 (5) | |||
| Station #6 | 2 (10) | |||
| Station #7 | 1 (5) | |||
| Pathology-confirmed LNs from E-tissues | ||||
| Station #6 | 1 (6.7), NT | |||
| Operative time, LDG (min) | 0.277 | |||
| D1+ | 207.7±56 | |||
| D2 | 236.8±53.4 | |||
LN = lymph node; NIR = near-infrared; LDG = laparoscopic distal gastrectomy; SD = standard deviation; NT = no tumor.
After conventional node dissection, a total of 6 E-tissues were collected from 5 patients. In the 20 patients (denominator), the numbers of E-tissues were 1 (5%), 1 (5%), 1 (5%), 2 (10%), and 1 (5%) for station numbers 1, 3, 4sb, 6, and 7, respectively. In the pathologic review, 1 LN (5%) was found among the extra harvested tissues that were retrieved from station #6.
Overall completeness of LN dissection
A total of 15 E-tissues were found in 14 of 50 patients (28%) after intended node dissection. From the 15 E-tissues, 2 tissues (4%) were histologically confirmed as LNs that showed no tumor involvement. Both nodes were retrieved from infra-pyloric LNs. E-tissues that were not LNs were mostly adipose tissues (n=13) or lymphatic duct tissue (n=1).
BMI and ICG
The mean intraoperative gastroscopy time was 11.5±3.7 minutes, and the mean time to the first ICG node uptake was 174 seconds. The mean time to the first ICG node uptake differed according to BMI, with the BMI ≥24 kg/m2 group showing a longer time than the BMI <24 kg/m2 group (198±51.6 vs. 150.1±183.3 seconds, P=0.018). Higher BMI also affected the operation time (250±47 minutes in the BMI ≥24 kg/m2 group and 210±46.7 minutes in the BMI <24 kg/m2 group). However, BMI did not affect the procedure time of submucosal injection under intraoperative gastroscopy (Table 4).
Table 4. Correlation of BMI with clinical outcomes.
| Variables | BMI <24 kg/m2 | BMI ≥24 kg/m2 | P-value |
|---|---|---|---|
| Time to first ICG uptake node (sec) | 150.1 (83.3) | 198.9 (51.6) | 0.018 |
| Intraoperative gastroscopy time (min) | 11.5 (3.6) | 10.5 (3.9) | 0.633 |
| Retrieved LN numbers | 36.3 (11.0) | 40.7 (13.0) | 0.562 |
| Operative time (min) | 210 (46.7) | 250 (47.0) | 0.004 |
BMI = body mass index; ICG = indocyanine green; LN = lymph node.
DISCUSSION
This study aimed to investigate the clinical application of a NIR camera system for radical laparoscopic gastrectomy performed by experienced surgeons at a high-volume center. The current study reports the experience of one the earliest and largest adaptation of the NIR-ICG technique in laparoscopic LN dissection for gastric cancer.
Complete dissection of the infra-pyloric area is technically challenging owing to anatomical variations in the vasculature and conjoining of embryologic planes, whereas nodal metastasis to the right gastroepiploic vessels is frequent in lower- and middle-third gastric cancer [5,8]. Pylorus-preserving gastrectomy has a higher likelihood of leaving behind soft tissues after dissection than distal gastrectomy and removing tissues from the small branches of the artery and vein while preserving them requires a higher level of surgical skill [9,10]. Recently, intraoperative vascular imaging with the ICG fluorescence technique has been introduced to overcome this hurdle [11]. With this background, we reported the completeness of LN dissection of the infra-pyloric area during LPPG in addition to that during LDG. Although tissues with ICG uptake were more frequent in LPPG than in LDG, it failed to show a statistical difference.
One of the limitations of our study was a high false-positive rate. Among 15 additional tissue specimens with ICG uptake, only 2 actual LNs and 13 visceral adipose specimens were obtained. The high temperature of the energy device or forceful handling of the LNs might have compromised the nodal structure, causing its deformity. Owing to false positivity under this setting and because unnecessary soft tissue dissection in patients with early gastric cancer may lead to additional injury, cautious application is required.
Moreover, compared with previous modalities, the NIR camera can detect even a very small fraction of ICG from the operation field, which might be confusing in the early application of this technique. To overcome this issue, additional quantification of the ICG signal could provide complementary information to distinguish tissues with different levels of fluorescence uptake. A quantification method can offset the false-positive ICG tissues and deliver precise information about the targeted tissues.
It was difficult to consider the sample size of this study for 2 reasons. First, this was an investigational study evaluating the feasibility of the NIR-ICG technique in various partial gastrectomy settings [12]. Second, although various methods have been proven safe and useful in gastric cancer mapping, there are no reports about the completeness of LN dissection with the NIR-ICG technique, which made it difficult to calculate the number of samples required for the anticipated events to develop [13,14,15]. Because the studied procedure was not performed or reported before the time of patient enrolment, it was difficult to follow the conventional sample size calculation. To compensate for this problem, we considered that this study should be categorized as an Innovation, Development, Exploration, Assessment, Long-term (IDEAL) phase 2a study, as introduced in previous publications about surgical [16,17].
Randomization could have provided stronger evidence for this study; however, the current protocol of the NIR-ICG technique still requires further revision, and a randomized clinical trial should be conducted after more background data are collected about this technique and after establishment of a more sophisticated protocol [18].
In our experience, the key factor for successful lymphatic mapping was the delivery of the tracer. The concentration and amount of injection are associated with the timing and degree of dispersion. The correct concentration and dosage should be calibrated according to the design and purpose of the study. We adopted the concentration at the lowest limit of our preclinical study (0.05 mg/mL) to obtain an optimal outcome from multiple (4–6) injections along the stomach. Second, the submucosal injection skill is important. Deep injection causes intravascular injection, which results in total blurriness of adjacent organs. In cases of extraluminal spillage, even small amounts can contaminate the operation field. Meanwhile, when ICG was injected only within the surface of the mucosa, a lag time in the perfusion of ICG into the laminal flow of the lymphatic system was noted, making it difficult to determine whether the procedure was successful.
In this study, we had to exclude 1 case. Initially, we proceeded with the operation; however, during dissection along the pancreas, we found a serious vascular anomaly: the portal vein was running through the anterior surface of the pancreas head and across the second part of the duodenum, and the common hepatic artery was totally replaced by an aberrant hepatic artery from the left gastric artery. For the safety of the patient, we decided to drop the patient from the study, and the NIR camera was turned on during the rest of the operation. With ICG-enhanced fluorescence until the end of the operation, we were able to perform a rather comfortable and safe surgery owing to a virtual lymphangiogram, which allowed the surgeon to differentiate the lymphatic structures from other anatomical structures and avoid injury of the unfamiliar vascular anatomy. In this case, the additional visual information provided a higher level of confirmation for the operator to avoid potential injury and bleeding when performing the D2 dissection, which could be helpful even for highly experienced gastric surgeons. This NIR technique can provide guidance in dissecting lymphatic tissues with safe visual confirmation and can improve intraoperative decision making during complex lymphatic dissections.
In summary, this report showed the feasibility and efficacy of an NIR camera system in laparoscopic gastrectomy for gastric cancer, which was facilitated by our experience in LN mapping. The quality of the images depends on the preparation of the tracer and the quality of its injection. In our experience, the benefit of this technique seemed limited to standardized laparoscopic radical partial gastrectomy cases with a normal anatomy.
The clinical implication of this study is that even for surgeons with a high level of experience in laparoscopic D2 dissections, the NIR system can serve as a complimentary tool to confirm complete LN dissection in patients with atypical anatomy. Meanwhile, for inexperienced surgeons, to perform function-preserving surgeries, such as LPPG, additional confirmation of complete dissection should benefit the surgical procedure to overcome the limitation of insufficient LN dissection.
Footnotes
Funding: This study was supported by Karl Storz® Inc. (grant No. 062015004, 062014318).
- Conceptualization: P.J.H.
- Data curation: S.Y.G.
- Formal analysis: H.Y.J.
- Funding acquisition: S.Y.S.
- Investigation: K.T.H.
- Methodology: L.H.J.
- Project administration: Y.H.K.
- Supervision: Y.H.K., L.H.J., K.S.H., S.Y.S.
- Validation: K.S.H.
- Visualization: S.Y.S.
- Writing - original draft: K.T.H.
- Writing - review & editing: Y.H.K., L.H.J., K.S.H., S.Y.S.
Conflict of Interest: This study was supported with instruments and partial financial support by Karl Storz.
References
- 1.Kim JP, Lee JH, Kim SJ, Yu HJ, Yang HK. Clinicopathologic characteristics and prognostic factors in 10 783 patients with gastric cancer. Gastric Cancer. 1998;1:125–133. doi: 10.1007/s101200050006. [DOI] [PubMed] [Google Scholar]
- 2.Degiuli M, Sasako M, Ponti A, Vendrame A, Tomatis M, Mazza C, et al. Randomized clinical trial comparing survival after D1 or D2 gastrectomy for gastric cancer. Br J Surg. 2014;101:23–31. doi: 10.1002/bjs.9345. [DOI] [PubMed] [Google Scholar]
- 3.Tokunaga M, Ohyama S, Hiki N, Fukunaga T, Yamada K, Sano T, et al. Investigation of the lymphatic stream of the stomach in gastric cancer with solitary lymph node metastasis. World J Surg. 2009;33:1235–1239. doi: 10.1007/s00268-009-9985-6. [DOI] [PubMed] [Google Scholar]
- 4.Kong SH, Noh YW, Suh YS, Park HS, Lee HJ, Kang KW, et al. Evaluation of the novel near-infrared fluorescence tracers pullulan polymer nanogel and indocyanine green/γ-glutamic acid complex for sentinel lymph node navigation surgery in large animal models. Gastric Cancer. 2015;18:55–64. doi: 10.1007/s10120-014-0345-3. [DOI] [PubMed] [Google Scholar]
- 5.Shinohara H, Kurahashi Y, Kanaya S, Haruta S, Ueno M, Udagawa H, et al. Topographic anatomy and laparoscopic technique for dissection of no. 6 infrapyloric lymph nodes in gastric cancer surgery. Gastric Cancer. 2013;16:615–620. doi: 10.1007/s10120-012-0229-3. [DOI] [PubMed] [Google Scholar]
- 6.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 7.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 8.Sasako M, McCulloch P, Kinoshita T, Maruyama K. New method to evaluate the therapeutic value of lymph node dissection for gastric cancer. Br J Surg. 1995;82:346–351. doi: 10.1002/bjs.1800820321. [DOI] [PubMed] [Google Scholar]
- 9.Suh YS, Han DS, Kong SH, Kwon S, Shin CI, Kim WH, et al. Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg. 2014;259:485–493. doi: 10.1097/SLA.0b013e318294d142. [DOI] [PubMed] [Google Scholar]
- 10.Sawai K, Takahashi T, Fujioka T, Minato H, Taniguchi H, Yamaguchi T. Pylorus-preserving gastrectomy with radical lymph node dissection based on anatomical variations of the infrapyloric artery. Am J Surg. 1995;170:285–288. doi: 10.1016/s0002-9610(05)80015-7. [DOI] [PubMed] [Google Scholar]
- 11.Kim M, Son SY, Cui LH, Shin HJ, Hur H, Han SU. Real-time vessel navigation using indocyanine green fluorescence during robotic or laparoscopic gastrectomy for gastric cancer. J Gastric Cancer. 2017;17:145–153. doi: 10.5230/jgc.2017.17.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45:626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miyashiro I, Hiratsuka M, Kishi K, Takachi K, Yano M, Takenaka A, et al. Intraoperative diagnosis using sentinel node biopsy with indocyanine green dye in gastric cancer surgery: an institutional trial by experienced surgeons. Ann Surg Oncol. 2013;20:542–546. doi: 10.1245/s10434-012-2608-8. [DOI] [PubMed] [Google Scholar]
- 14.Miyashiro I, Kishi K, Yano M, Tanaka K, Motoori M, Ohue M, et al. Laparoscopic detection of sentinel node in gastric cancer surgery by indocyanine green fluorescence imaging. Surg Endosc. 2011;25:1672–1676. doi: 10.1007/s00464-010-1405-3. [DOI] [PubMed] [Google Scholar]
- 15.Miwa K, Kinami S, Taniguchi K, Fushida S, Fujimura T, Nonomura A. Mapping sentinel nodes in patients with early-stage gastric carcinoma. Br J Surg. 2003;90:178–182. doi: 10.1002/bjs.4031. [DOI] [PubMed] [Google Scholar]
- 16.Ergina PL, Cook JA, Blazeby JM, Boutron I, Clavien PA, Reeves BC, et al. Challenges in evaluating surgical innovation. Lancet. 2009;374:1097–1104. doi: 10.1016/S0140-6736(09)61086-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet. 2009;374:1105–1112. doi: 10.1016/S0140-6736(09)61116-8. [DOI] [PubMed] [Google Scholar]
- 18.Barkun JS, Aronson JK, Feldman LS, Maddern GJ, Strasberg SM, Altman DG, et al. Evaluation and stages of surgical innovations. Lancet. 2009;374:1089–1096. doi: 10.1016/S0140-6736(09)61083-7. [DOI] [PubMed] [Google Scholar]