Abstract
Background
Opioid overdoses are at epidemic levels in the United States. Emergency Medical Service (EMS) providers may administer naloxone to restore patient breathing and prevent respiratory arrest. There was a need for contemporary data to examine the number of naloxone administrations in an EMS encounter.
Methods
Using data from the National Emergency Medical Services Information System, we examined data from 2012–5 to determine trends in patients receiving multiple naloxone administrations (MNAs). Logis tic regression including demographic, clinical, and operational information was used to examine factors associated with MNA.
Results
Among all events where naloxone was administered only 16.7% of the 911 calls specifically identified the medical emergency as a drug ingestion or poisoning event. The percentage of patients receiving MNA increased from 14.5% in 2012 to 18.2% in 2015, which represents a 26% increase in MNA in 4 years. Patients aged 20–29 had the highest percentage of MNA (21.1%). Patients in the Northeast and the Midwest had the highest relative MNA (Chi Squared = 539.5, p < 0.01 and Chi Squared = 351.2, p < 0.01, respectively). The logistic regression model showed that the adjusted odds ratios (aOR) for MNA were greatest among people who live in the Northeast (aOR = 1.18, 95% CI = 1.13–1.22) and for men (aOR = 1.13, 95% CI = 1.10–1.16), but lower for suburban and rural areas (aOR = 0.76, 95% CI = 0.72–0.80 and aOR = 0.85, 95% CI = 0.80–0.89) and lowest for wilderness areas (aOR = 0.76, 95% CI = 0.68–0.84). Higher adjusted odds of MNA occurred when an advanced life support (ALS 2) level of service was provided compared to basic life support (BLS) ambulances (aOR = 2.15, 95% CI = 1.45–3.16) and when the dispatch complaint indicated there was a drug poisoning event (aOR = 1.12, 95% CI = 1.09–1.16). Reported layperson naloxone administration prior to EMS arrival was rare (1%).
Conclusion
This study shows that frequency of MNA is growing over time and is regionally dependent. MNA may be a barometer of the potency of the opioid involved in the overdose. The increase in MNAprovides support for a dosage review. Better identification of opioid related events in the dispatch system could lead to a better match of services with patient needs.
Keywords: Naloxone, opioid, EMS, overdose, heroin
Introduction
Opioid overdose deaths have risen since 1999,1 with the Centers for Disease Control and Prevention (CDC) first calling the rise in U.S. opioid-related deaths an epidemic in 2012.2 In 2015, 33,091 people experienced an overdose death involving opioids.1 In 2015, the mortality rate for synthetic opioids other than methadone (e.g., fentanyl) was 3.1 per 100,000 persons, which represents a 72% increase over 2014 (1.8 per 100,000 persons).1 While the drug overdose burden in the United States is growing, the recent rise in synthetic opioid overdoses, namely higher potency fentanyl, is likely to further affect future strategies to respond to this epidemic.
The over-prescribing of opioids is a major driver behind the epidemic.3 Primary prevention strategies for opioid overdose prevention include the implementation of “pill mill” laws (e.g., legislation designed to limit a doctor, clinic or pharmacy that is prescribing or dispensing powerful narcotics inappropriately or for non-medical reasons),4 insurance reimbursement strategies5 (e.g., drug utilization review, prior authorization) development or enhancement of prescription drug monitoring programs,6 and adherence to clinical prescribing guidelines.7 The main secondary prevention strategy is administering naloxone to reverse an opioid-related poisoning. The FDA originally approved naloxone in 1971 to reverse opioid related-overdoses and has approved two formulations suitable for community use more recently.
Although Law Enforcement usually arrives at a drug overdose scene first, Emergency Medical Service (EMS) providers are usually the first health care providers to arrive at the scene of an opioid overdose. EMS can administer naloxone via intranasal (IN), intramuscular (IM), or intravenous (IV) routes. Over the years, more EMS patients have been administered naloxone, as EMS providers treated the growing number of opioid overdoses.8 That growth has led to legal and regulatory efforts to increase the number of personnel who can administer naloxone.9–11 In an effort to address the epidemic, additional public safety personnel, such as firefighters and law enforcement, have been granted authority to administer naloxone.10 Subsequent evaluations of law enforcement shows safe naloxone administration.12 In recent years, IN naloxone has become a popular choice for EMS because of its ease of use in a prehospital setting, with successful reversal rates 66–83% of the time, similar to other routes of administration.13–17 Although the majority of the literature suggests that IN naloxone is effective, some research has shown that the clinical response time was slower and that more administrations were required to achieve the same effect as IV.16 It has also been noted that that the change in respiratory rate is slightly less rapid for IN.17 Dowling et al., found that a combination of IN and IM naloxone produced the best long-lasting reversal effect.18 Collectively, this information has raised questions regarding the overall effectiveness of current naloxone dosages, given the rise in synthetic opioids.
While more public health providers and safety professionals are now able to administer naloxone, along with laypersons who are helping friends and family members, there has been little attention to the naloxone dose in light of the overall trend of increasing potency of opioid-related drugs.19 Milligram for milligram, heroin is many more times more potent than some prescription opioids, and potency is even greater when combined with other opioids such as fentanyl. Moreover, during the period 2013 through 2014, the Drug Enforcement Agency found that drug submissions that tested positive for the synthetic opioid fentanyl rose by 426%; meanwhile, the Centers for Disease Control and Prevention revealed that deaths involving synthetic opioids (other than methadone) including fentanyl increased 80% for the same time period20 and those for heroin increased 26%.21 These deaths coincided with law enforcement reports of increased availability of fentanyl in certain geographic locations, with a concentration in the Northeast and Midwest of the United States.22 However, there is anecdotal evidence that IN naloxone is less effective in reversing longer-lasting, more potent synthetic opioids such as fentanyl,19 and that multiple doses of naloxone was used when law enforcement administered naloxone to patients who had fentanyl in their system.23 On October 5, 2016, the Food and Drug Administration held an advisory committee meeting to consider potential changes in naloxone dosing, in part, based on multiple naloxone administrations (MNA) and the increase of more potent illicit synthetic opioids, such as fentanyl.24
Naloxone use by EMS, as recorded in surveillance data, has been used to measure overdose incidence as well as to understand seasonal surges in opioid overdoses,25 and has been shown to correlate with drug overdose visits to the Emergency Department.26 EMS surveillance data can also identify circumstances where multiple doses of naloxone were needed, as well as the patterns of naloxone administration, and can provide specific patient and scene information from the original 9–1-1 emergency call.27 Other factors, such as the type of EMS vehicle dispatched, may also be important in determining naloxone use. Historically, Basic Life Support (BLS) vehicles, typically the first responders in rural communities,10 have been less likely to be equipped with naloxone than Advanced Life Support (ALS) vehicles, although this has been improving over time.
The purpose of this study is to determine if MNA were growing over time and to determine the circumstances where multiple doses occur. Changes in MNA in a geographic region may be associated with locations where opioid potency is increasing (such as in the Northeastern U.S.). Increases in MNA may also inform the public health community about a mismatch between typically used naloxone doses and changes in the potency of circulating opioids consumed by drug users. Insights into the patient, environmental, and situational factors that go into MNA could yield important information for the allocation of resources across first responders and response equipment. We were unable to identify any national or large study of MNA in the literature.
Methods
Data Source
This study used data from the National Emergency Medicine Service Information System (NEMSIS) for the years 2012 through 2015, and includes all years of publically available data. NEMSIS provides the framework for collecting, storing and sharing standardized EMS patient care, which ensures data collection consistency across the United States. During 2012 through 2015, the National EMS Database has collected records of EMS events from 42–45 states with most local agencies participating. These data were consolidated to create the NEMSIS data set and contain about the same number of weighted records as the nationally representative National Hospital Ambulatory Care Survey.28 NEM-SIS is not a weighted dataset, but is considered representative of US EMS activity.28 Additional information on how NEMSIS was constructed is available.28 This data set includes demographic data, basic 9–1-1 call information, details regarding the scene of injury or illness, and medications administered. For this study, a record was included for analysis only if naloxone was administered.
Variables and Analysis
The unit of analysis for this study is MNA, which may serve as an indirect measure of opioid potency, which helps us to understand more about the national opioid crisis. To evaluate trends in MNA over time, the total number of patients receiving MNA was divided by the total number of patients receiving at least one dose of naloxone. The result was a percentage of patients receiving more than one administration. Confidence intervals were calculated to determine if the rate changes were significant between consecutive years. To determine if frequencies of MNA were different by geographic region, a two way chi squared goodness of fit test was used to compare the observed and expected frequencies. An expected value for each cell in a two-way table was equal to (row total column∗total)/n, where n is the total number of observations. To examine predictors of MNA, we created a logistic regression model in which the binominal dependent variable was whether or not a person was administered naloxone more than once during 2015. The independent variables that were thought to influence MNA decisions included demographic (age, gender), clinical (dispatch complaint, primary symptom, oxygen administered (yes/no), previous administration of naloxone by a layperson (yes/no), and operational information (incident location, type of ambulance dis patched, urban/rural area, weekend vs. weekday and transport outcome). The results of the multivariate logistic regression were presented as adjusted odds ratios (aOR) with 95% confidence intervals (CI). All data were analyzed using SAS statistical software version 9.3.
Results
The National EMS data for 2012 show that 95,012 patients were administered naloxone, of whom 13,765 (14.49%, 95% CI = 14.26%–14.71%) received MNA. In 2013, the total number of patients receiving naloxone increased to 112,844, with 16,281 (14.91%, 95% CI = 14.71%–15.11%) patients receiving MNA. In 2014, the total number of patients receiving naloxone was 127,956 of whom 20,884 (16.32%, 95% CI = 16.12%–16.52%) patients received MNA and in 2015, 173,016 patients received naloxone and 31,554 (18.24%, 95% CI = 18.06%–18.42%) of them received MNA. MNA is increasing at a significant rate for years 2014 and 2015. Overall, MNA increased 25.8% from 2012 to 2015 (Figure 1).
FIGURE 1.
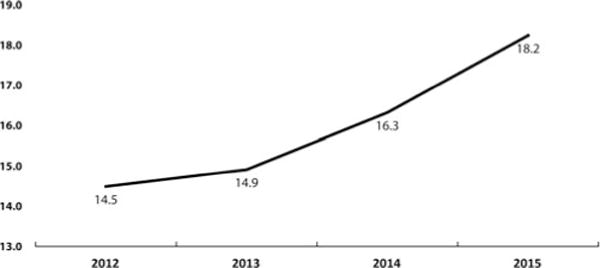
Percentage of patients receiving multiple naloxone administrations (MNA) in an EMS setting during 2012–15.
A comparison of expected MNA and observed MNA by US Census region shows that the South had a lower MNA (n = 9,954) than what would be expected (n = 13,991) (Chi Squared = 1,164.7, p<0.01; see Figure 2). The West, Northeast, and Midwest had significantly higher MNA than expected (Chi Squared = 106.46, p < 0.01, Chi Squared = 539.5, p < 0.01 and Chi Squared = 351.2, p < 0.01, respectively).
FIGURE 2.
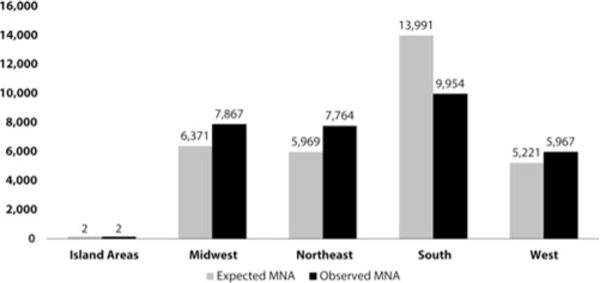
Multiple naloxone administrations (MNA) by U.S. census region in an EMS setting.
Table 1 demonstrates demographic differences between those administered only a single dose and those receiving MNA. Patients aged 20–29 had the highest percentage of MNA (21.1%) followed by patients aged 30–49 (20.1%), who had the largest percentage of total EMS events (n = 57,914, 33.5%) in this study. Patients from the South had the largest number of events receiving naloxone (76,713 or 44.3% of all EMS cases where naloxone was administered), but these patients had the lowest percentage of MNA (13.0%). The majority of naloxone administrations occurred in urban areas (80.9%) and, among those with known urbanicity, MNA was most common in urban areas (18.8%). The most frequent location for naloxone administrations by EMS providers was a home/residence (n = 105,758, 61.1%) and this was also the location with the highest rate of MNA (19.1%) among those with known, specific locations. The location with the lowest rates of MNA was a residential institution (nursing home, jail/prison, 14.0%). MNA was slightly higher for patients on the weekend (18.5%) versus during the week (18.0%). The reported use of naloxone among laypersons prior to EMS arrival was about 1% (n = 1,602).
Table 1.
Naloxone administration doses and population characteristics as reported by emergency medical service.
| Single Dose
|
Multiple Doses
|
Total within Category
|
||||
|---|---|---|---|---|---|---|
| N | % Received | N | % Received | N | Percent | |
| Age | ||||||
| 0-19 | 5,944 | 83.4 | 1,181 | 16.6 | 7,125 | 4.1 |
| 20-29 | 26,806 | 79.0 | 7,146 | 21.1 | 33,952 | 19.6 |
| 30-49 | 46,287 | 79.9 | 11,627 | 20.1 | 57,914 | 33.5 |
| 50-64 | 36,382 | 82.9 | 7,482 | 17.1 | 43,864 | 25.4 |
| 65 plus | 26,043 | 86.4 | 4,118 | 13.7 | 30,161 | 17.4 |
| Gender | ||||||
| Female | 59,459 | 83.1 | 12,113 | 16.9 | 71,572 | 41.4 |
| Male | 81,338 | 80.8 | 19,302 | 19.2 | 100,640 | 58.2 |
| Unknown | 665 | 82.7 | 139 | 17.3 | 804 | 0.5 |
| US Region | ||||||
| Island Areas | 6 | 75.0 | 2 | 25.0 | 8 | 0.0 |
| Midwest | 27,067 | 77.5 | 7,867 | 22.5 | 34,934 | 20.2 |
| Northeast | 24,967 | 76.3 | 7,764 | 23.7 | 32,731 | 18.9 |
| South | 66,759 | 87.0 | 9,954 | 13.0 | 76,713 | 44.3 |
| West | 22,663 | 79.2 | 5,967 | 20.8 | 28,630 | 16.5 |
| Urbanicity | ||||||
| Unknown | 4,820 | 79.5 | 1,240 | 20.5 | 6,060 | 3.5 |
| Urban | 113,747 | 81.2 | 26,284 | 18.8 | 140,031 | 80.9 |
| Suburban | 10,232 | 85.9 | 1,687 | 14.2 | 11,919 | 6.9 |
| Wilderness | 2,558 | 86.7 | 394 | 13.4 | 2,952 | 1.7 |
| Rural | 10,105 | 83.8 | 1,949 | 16.2 | 12,054 | 7.0 |
| Location | ||||||
| Home/Residence | 85,608 | 81.0 | 20,150 | 19.1 | 105,758 | 61.1 |
| Other Location | 11,413 | 81.0 | 2,676 | 19.0 | 14,089 | 8.1 |
| Residential Institution (Nursing Home, jail/prison) | 11,864 | 86.1 | 1,923 | 14.0 | 13,787 | 8.0 |
| Street or Highway | 16,890 | 84.0 | 3,208 | 16.0 | 20,098 | 11.6 |
| Trade or service (business, bars, restaurants, etc) | 8,690 | 82.2 | 1,886 | 17.8 | 10,576 | 6.1 |
| Unknown | 6,997 | 80.4 | 1,711 | 19.7 | 8,708 | 5.0 |
| Weekend | ||||||
| Monday-Thursday | 78,310 | 82.0 | 17,215 | 18.0 | 95,525 | 55.2 |
| Friday-Sunday | 63,152 | 81.5 | 14,339 | 18.5 | 77,491 | 44.8 |
| Layperson | ||||||
| No Previous Naloxone | 139,994 | 81.7 | 31,420 | 18.3 | 171,414 | 99.1 |
| Previous Naloxone | 1,468 | 91.6 | 134 | 8.4 | 1,602 | 0.9 |
| Ambulance Service | ||||||
| ALS, Level 1 | 18,135 | 81.1 | 4,215 | 18.9 | 22,350 | 12.9 |
| ALS, Level 1 Emergency | 40,624 | 83.9 | 7,783 | 16.1 | 48,407 | 28.0 |
| ALS, Level 2 | 11,401 | 77.0 | 3,415 | 23.1 | 14,816 | 8.6 |
| BLS | 223 | 88.1 | 30 | 11.9 | 253 | 0.1 |
| BLS, Emergency | 2,453 | 91.6 | 225 | 8.4 | 2,678 | 1.5 |
| Unknown/Other | 68,626 | 81.2 | 15,886 | 18.8 | 84,512 | 48.8 |
| Oxygen | ||||||
| Not Provided | 77,347 | 82.8 | 16,068 | 17.2 | 93,415 | 54.0 |
| Provided | 64,115 | 80.6 | 15,486 | 19.5 | 79,601 | 46.0 |
| Disposition | ||||||
| Dead at Scene | 4,529 | 88.6 | 581 | 11.4 | 5,110 | 3.0 |
| Treated and Released | 4,301 | 86.5 | 672 | 13.5 | 4,973 | 2.9 |
| Treated, Transferred Care | 4,957 | 81.7 | 1,114 | 18.4 | 6,071 | 3.5 |
| Treated, Transported by EMS | 127,583 | 81.4 | 29,177 | 18.6 | 156,760 | 90.6 |
| Treated, Transported by Law Enforcement | 57 | 90.5 | 6 | 9.5 | 63 | 0.0 |
| Treated, Transported by Private Vehicle | 35 | 89.7 | 4 | 10.3 | 39 | 0.0 |
Source: National EMS Information, 2015.
There was large variation in MNA by level of EMS service. BLS and BLS Emergency levels of service only provided MNA 11.9% and 8.4% of the time, respectively. The Advanced ALS Level 2 had the highest percentage of MNA (23.1%). EMS also administered oxygen in 46% of the events and, in those events, MNA was more common (19.5%). It was not common to for MNA to occur during the attempt to revive the patient if the patient was dead at the scene (11.4%). The vast majority of patients receiving naloxone were transported to the Emergency Department (90.6%).
Logistic regression was used to assess the factors that influenced MNA (Table 2). Although most of the independent variables in the logistic regression model were statistically significant predictors of MNA, the variables with the highest predictive values was U.S. Census Region, EMS level of Service and EMS primary symptom. The least predictive independent variable was whether naloxone was administered on a weekend.
Table 2.
Naloxone administration doses and population characteristics as reported by emergency.
| Odds Ratio Estimate | Lower CI | Upper CI | |
|---|---|---|---|
| Gender | |||
| Female | 1.00 | – | – |
| Male | 1.13 | 1.10 | 1.16 |
| Unknown | 1.13 | 0.94 | 1.37 |
| Age | |||
| ages 0–19 | 1.00 | – | – |
| ages 20–29 | 1.29 | 1.21 | 1.39 |
| ages 30–49 | 1.27 | 1.18 | 1.35 |
| ages 50–64 | 1.05 | 0.98 | 1.12 |
| ages 65 plus | 0.84 | 0.78 | 0.91 |
| Region | |||
| Midwest | 1.00 | – | – |
| Island Areas | 1.39 | 0.28 | 7.02 |
| Northeast | 1.18 | 1.13 | 1.22 |
| South | 0.53 | 0.51 | 0.55 |
| West | 0.99 | 0.95 | 1.03 |
| Urbanicity | |||
| Urban | 1.00 | ||
| Rural | 0.85 | 0.80 | 0.89 |
| Suburban | 0.76 | 0.72 | 0.80 |
| Wilderness | 0.76 | 0.68 | 0.84 |
| Unknown | 1.12 | 1.05 | 1.19 |
| Weekend | |||
| Monday-Thursday | 1.00 | – | – |
| Friday-Sunday | 1.02 | 0.99 | 1.04 |
| Layperson Administration | |||
| No Previous Naloxone | 1.00 | – | – |
| Previous Naloxone | 0.55 | 0.46 | 0.65 |
| Location | |||
| Street or Highway | 1.00 | – | – |
| Home/Residence | 1.42 | 1.36 | 1.48 |
| Other Location | 1.26 | 1.19 | 1.33 |
| Residential Institution (Nursing Home, jail/prison) | 1.12 | 1.05 | 1.19 |
| Trade or service (business, bars, restaurants, etc) | 1.22 | 1.14 | 1.30 |
| Unknown | 1.42 | 1.33 | 1.52 |
| Dispatch Complaint | |||
| Other | 1.00 | – | – |
| Ingestion/Poisoning | 1.12 | 1.09 | 1.16 |
| Unknown | 1.00 | 0.97 | 1.03 |
| Ambulance Service Level | |||
| BLS | 1.00 | – | – |
| BLS Emergency | 0.45 | 0.30 | 0.68 |
| ALS, Level 1 | 1.58 | 1.07 | 2.32 |
| ALS, Level 1, Emergency | 1.15 | 0.78 | 1.69 |
| ALS, Level 2 | 2.15 | 1.45 | 3.16 |
| Unknown\Other | 1.46 | 0.99 | 2.15 |
| Oxygen | |||
| Provided | 1.00 | – | – |
| Not Provided | 0.84 | 0.82 | 0.86 |
| Primary Symptom | |||
| None | 1.00 | – | – |
| Bleeding | 0.75 | 0.52 | 1.07 |
| Breathing Problem | 1.41 | 1.25 | 1.59 |
| Change in responsiveness | 1.28 | 1.15 | 1.43 |
| Choking | 0.97 | 0.56 | 1.68 |
| Death | 0.76 | 0.67 | 0.86 |
| Device/Equipment Problem | <0.001 | – | – |
| Diarrhea | 2.41 | 0.96 | 6.03 |
| Drainage/Discharge | 1.72 | 0.61 | 4.89 |
| Fever | 1.51 | 0.90 | 2.53 |
| Malaise | 0.70 | 0.55 | 0.88 |
| Mass/Lesion | <0.001 | – | – |
| Mental/Psych | 0.93 | 0.81 | 1.07 |
| Nausea/Vomiting | 0.59 | 0.46 | 0.78 |
| Pain | 0.87 | 0.74 | 1.02 |
| Palpitations | 0.83 | 0.52 | 1.33 |
| Rash/Itching | 0.28 | 0.04 | 2.13 |
| Swelling | 1.12 | 0.38 | 3.32 |
| Transport Only | 0.73 | 0.44 | 1.21 |
| Unknown | 1.06 | 0.95 | 1.19 |
| Weakness | 0.82 | 0.71 | 0.96 |
| Wound | 0.85 | 0.57 | 1.27 |
| Disposition | |||
| Dead at the Scene | 1.00 | – | – |
| Treated and Released | 1.09 | 0.96 | 1.23 |
| Treated, Transferred Care | 1.44 | 1.29 | 1.61 |
| Treated, Transported by EMS | 1.61 | 1.47 | 1.76 |
| Treated, Transported by Law Enforcement | 0.78 | 0.33 | 1.84 |
| Treated, Transported by Private Vehicle | 0.90 | 0.32 | 2.57 |
Source: National EMS Information, 2015.
Independent variables in the model revealed that the odds of MNA were higher if the patient was male (aOR = 1.13, 95%, CI = 1.10–1.16) and the odds of MNA increased with age for patients aged 20–29 and 30–49 (aOR = 1.29, 95%, CI = 1.21–1.39, aOR = 1.27, 95%, CI = 1.18–1.35, respectively). Compared to the Midwest, the Northeast had the highest odds of MNA administration (aOR = 1.18, 95%, CI = 1.13–1.22) and the South had the lowest odds (aOR = 0.53, 95%, CI = 0.51–0.55).
Layperson naloxone use, scene location, dispatch information, and primary symptom also affected MNA decisions. If a patient has previously received naloxone from a layperson, the odds of MNA were lower (aOR = 0.55, 95%, CI = 0.46–0.65). The odds of MNA also differed by urbanicity, with the suburban and wilderness areas having the lowest odds of MNA (aOR = 0.76, 95%, CI = 0.72–0.80 and aOR = 0.76, 95%, CI = 0.68–0.84, respectively) and urban areas having the highest (aOR = 1.0, reference group). The odds of MNA were also lower in rural areas compared to urban areas (aOR = 0.85, 95%, CI = 0.80–0.89). Compared to a “street or highway,” the odds of MNA were highest when EMS found the patient at a residence/home (aOR = 1.42, 95%, CI = 1.36–1.48). The dispatch complaint identified by the emergency medical dispatcher (EMD) from a 9–1-1 call may be unrelated to the primary symptom determined by EMS once they arrive on the scene. When the dispatch complaint was identified as an ingestion/poisoning, the odds of MNA were higher (aOR = 1.12, 95%, CI= 1.09–1.16). Similarly, when EMS professionals arrive on the scene, they make their own determinations about patient symptoms, and sometimes this does not match the original information in the dispatch complaint. MNA was highest when EMS determined that the patient’s primary symptom was a breathing problem (aOR = 1.41, 95%, CI = 1.25–1.59), followed by a change in responsiveness (aOR = 1.28, 95%, CI = 1.15–1.43). When oxygen was not provided, the odds of MNA were lower (aOR = 0.84, 95%, CI = 0.82–0.86). The type of ambulance dispatched was also associated with MNA. Using BLS as a reference, the odds of MNA were higher for both ALS 1 and ALS 2 levels of service (aOR = 1.58, 95%, CI = 1.07–2.32 and aOR = 2.15, 95%, CI = 1.45–3.16). Finally, patients who were treated and transported by EMS providers had the highest odds of MNA (aOR = 1.61, 95%, CI = 1.47–1.76).
Discussion
The central finding of this study is that MNA is increasing over time. In 2015, nearly one out of five patients received MNA in efforts to reverse a presumed opioid-related overdose compared to 14.5% in 2012, an increase of 26%. The odds of MNA were highest in the Northeastern part of the United States, which is consistent with where the DEA is finding higher number of fentanyl testing submissions.22 Perhaps, these higher potency opioids are related to the increase in MNA among EMS providers. Given that police officers, first response firefighters and other responders can now administer naloxone in some jurisdictions, and the fact that layperson naloxone is growing,29 these increases in MNA by EMS providers, are perhaps even more pronounced than what can be captured in EMS data.
Even though the database does not capture dosage forms, given the increase in use of IN naloxone among EMS providers,19 these results may provide some support for examining the dosage and concentration of IN naloxone. Drug users can have additional scarring in the nasal passages that may hamper the absorption of IN naloxone, but the likelihood of this explaining the results is low. Because the half-life of naloxone is 30–90 minutes,30 multiple doses of naloxone may be needed when trying to reverse drug overdoses due to long-lasting opioids.19 However, MNA in pre-hospital settings is usually undertaken because the patient’s breathing does not improve following the initial administration, rather than for a recrudescence of symptoms. Multiple doses related to half-life issues are rarely applicable in an EMS environment, where the priority for EMS is to manage the airway and immediately transport to definitive care, but may be pertinent in long rural transports. These results also confirm that MNA was most likely when there was a change in responsiveness and there were breathing problems at the injury scene.
Over 90% of the patients were transported to an emergency care facility after any naloxone administration and only 2.9% were treated and released by EMS. Some of these patients refused transport. While airway management and opioid reversal using naloxone is a priority, transport may not be. Notably, the concept of EMS releasing patients after reversal of opioid overdose is not universally accepted, although it is rather common in some jurisdictions and has been associated with low mortality.31–33
Two factors might explain lower MNA rates in non-urban compared to other settings. First, the transport and response times were, on average, longer in rural and wilderness areas than in urban areas.34 Because the inclusion criterion for this study was any event where naloxone was administered and because there is no diagnosis in EMS data, we could not capture on-scene deaths where no naloxone was administered by EMS at all. Because EMS responses in rural areas are slower compared to urban areas, MNA on an apparently dead person is less likely after the initial naloxone administration. Second, the level BLS was more common in rural and wilderness areas6 and was staffed differently and equipped differently than ALS. These differences in urbanicity are consistent with the study findings that ALS level 1 and level 2 patient encounters had higher MNA, even though naloxone administration among BLS response crews have been shown to be effective,35 when an opioid poisoning case is correctly identified.36 This discovery, coupled with the finding that the medical emergency was identified in the initial 911 call as a drug ingestion or a poisoning event in only 16.7% of the EMS events where naloxone was used, suggests that it would be helpful to obtain more detailed information. There were jurisdictions where the EMS provides additional information to the responding EMS personnel beyond dispatch complaint, such as the patient’s level of consciousness, breathing effort, and presence or absence of a pulse. Such jurisdictions are not solely dependent upon the dispatch complaint to ensure they respond with the appropriate level of service. Regardless, when EMS dispatch systems know more about the precise nature of the medical emergency, the dispatched EMS services could be more effective in treating a patient with a drug overdose. Also, this demonstrates the need for quality assurance programs that close the loop between public safety answering point for 9–1-1 calls and responders, such that the call-takers can improve their skills in getting callers to reports on-scene problems accurately.
Supplemental efforts to revive the patient were also assessed, such as layperson use of naloxone and EMS use of oxygen. In this study the reported use of layperson naloxone before EMS providers arrived on the scene was rare (<1%). In those cases, EMS administered MNA less often, suggesting that lay naloxone administration may reduce the need for EMS to administer a naloxone.
The odds of MNA were higher when EMS also administered oxygen to the patient. In this study, 46% of the patients who were administered naloxone received supplemental oxygen, and MNA was more common (19.5% vs. 17.2%) in those patients who received supplemental oxygen. The administration of supplemental oxygen for suspected narcotic overdose is a necessary and standard component of EMS response to and treatment protocols of a suspected narcotic overdose.37,38 Approximately half of all patients who received naloxone did not receive supplemental oxygen. This may be due to prompt administration of naloxone upon EMS arrival. Therefore, some patients may promptly receive naloxone, have a reversal of their respiratory depression, and not receive supplemental oxygen or ventilator assistance. It would be expected that those patients who do not have a rapid reversal of symptoms with a single dose of naloxone, and who may require MNA, would receive additional measures (i.e., supplemental oxygen, ventilation assistance, cardiac monitor) as EMS personnel continue to manage the overdose to prevent morbidity and mortality. We suspect that in cases where naloxone was administered, absent of oxygen, there was good patient recovery. Additional studies on this finding are needed.
The use of EMS data for trends and real-time surveillance at the local, state, and national levels can provide EMS agencies and policy makers with knowledge of sudden increases in MNA which can in turn inform the need for increasing the number of naloxone doses required to be carried by EMS personnel. Local-level public health officials have used EMS data to create hot-spot maps of opioid overdoses and those maps are shared with program officials managing opioid overdose prevention programs.39 Local, State, and Federal funding for EMS data systems has the potential to improve real-time surveillance for myriad public health emergencies, including the opioid epidemic. Integration of MNA data into the EMS response could improve emergency responses and potentially save more lives. Such data can be used to help with the targeting naloxone for layperson distribution programs. Future research directions include studies on IN naloxone and the frequency of MNA among patients who have used potent opioids, such as fentanyl and the even more potent carfentanyl, where the DEA has issued a warning that “Carfentanil is surfacing in more and more communities” on September 22, 2016.40
Limitations of this study include not knowing what route or dose of naloxone was used by the EMS provider and the exclusion of all calls in which no naloxone was administered. Nonetheless, it is uncommon for EMS providers to switch routes of administration unless the patient is unresponsive to IN route and the EMS provider switches to IV route.16 Thus, in interpreting MNA, there is likely stable routes of administration within each case. Although NEMSIS has been in development for over 10 years, the NEMSIS research dataset is relatively new and there are some missing aspects of EMS encounters, such as capturing all layperson administrations. Also, the national research dataset does not designate the state associated with the record, and, therefore, MNA associations with specific state opioid overdose burden is not possible.
Conclusion
This novel study uses EMS patient encounter data to describe the use of naloxone in the field. It demonstrates a possible method for monitoring real-time opioid potency on a national level. Although the national dataset does not include formulation and route of administration information, many states and localities do include such data, and they can analyze their own data and make specific and more accurate determinations about naloxone policy. However, these findings can inform examinations of the appropriate dosage levels for naloxone at a local level. The findings also underline the need for more accurate 9–1-1 call information from the public to ensure the best possible deployment of public safety equipment and personnel. Assuring that responding EMS providers are adequately equipped to handle the burden of injury and disease they face must be a key part of quality assurance programs. Recognizing the need for EMS to have adequate naloxone supplies to treat opioid overdose on a local or regional basis is a key to fighting this epidemic.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC), the Agency for Toxic Substances and Disease Registry or the Food and Drug Administration (FDA), and the National Highway Traffic and Safety Administration (NHTSA).
Footnotes
This article is not subject to US copyright law.
References
- 1.Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid overdose deaths-United States, 2000–2015. MMWR. 2016;65(50–51):1445–52. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses-a US epidemic. MMWR. 2012 Jan 13;61(1):10. [PubMed] [Google Scholar]
- 3.DuPont RL. Prescription drug abuse: an epidemic dilemma. J Psychoactive Drugs. 2010 Jun 1;42(2):127–32. doi: 10.1080/02791072.2010.10400685. [DOI] [PubMed] [Google Scholar]
- 4.Lyapustina T, Rutkow L, Chang HY, et al. Effect of a “pill mill” law on opioid prescribing and utilization: the case of Texas. Drug Alcohol Depend. 2016 Feb 1;159:190–7. doi: 10.1016/j.drugalcdep.2015.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faul M, Bohm M, Alexander GC. Methadone prescribing and overdose and the association with medicaid preferred drug list policies — United States, 2007–2014. MMWR. 2017;66(12):320–3. doi: 10.15585/mmwr.mm6612a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang HY, Lyapustina T, Rutkow L, et al. Impact of prescription drug monitoring programs and pill mill laws on high-risk opioid prescribers: a comparative interrupted time series analysis. Drug and alcohol dependence. 2016 Aug 1;165:1–8. doi: 10.1016/j.drugalcdep.2016.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMSA. 2016 Apr 19;315(15):1624–45. doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander JL, Burton JH, Bradshaw JR, Colin F. Suspected opioid-related emergency medical services encounters in a rural state, 1997-2002. Prehosp Emerg Care. 2004 Jan 1;8(4):427–30. doi: 10.1016/j.prehos.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Davis CS, Southwell JK, Niehaus VR, Walley AY, Dailey MW. Emergency medical services naloxone access: a national systematic legal review. Acad Emerg Med. 2014 Oct 1;21(10):1173–7. doi: 10.1111/acem.12485. [DOI] [PubMed] [Google Scholar]
- 10.Davis CS, Ruiz S, Glynn P, Picariello G, Walley AY. Expanded access to naloxone among firefighters, police officers, and emergency medical technicians in Massachusetts. Am J Public Health. 2014 Aug;104(8):e7–9. doi: 10.2105/AJPH.2014.302062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faul M, Dailey MW, Sugerman DE, Sasser SM, Levy B, Paulozzi LJ. Disparity in naloxone administration by emergency medical service providers and the burden of drug overdose in US rural communities. J Information. 2015 Jul;105(S3) doi: 10.2105/AJPH.2014.302520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher R, O’Donnell D, Ray B, Rusyniak D. Police officers can safely and effectively administer intranasal naloxone. Prehosp Emerg Care. 2016 Nov 1;20(6):675–80. doi: 10.1080/10903127.2016.1182605. [DOI] [PubMed] [Google Scholar]
- 13.Barton ED, Colwell CB, Wolfe T, et al. Efficacy of intranasal naloxone as a needleless alternative for treatment of opioid overdose in the prehospital setting. J Emerg Med. 2005 Oct 31;29(3):265–71. doi: 10.1016/j.jemermed.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Kelly AM, Kerr D, Dietze P, Patrick I, Walker T, Koutsogiannis Z. Randomised trial of intranasal versus intramuscular naloxone in prehospital treatment for suspected opioid overdose. Med J Aust. 2005 Jan 3;182(1):24–7. doi: 10.5694/j.1326-5377.2005.tb06550.x. [DOI] [PubMed] [Google Scholar]
- 15.Kerr D, Kelly AM, Dietze P, Jolley D, Barger B. Randomized controlled trial comparing the effectiveness and safety of intranasal and intramuscular naloxone for the treatment of suspected heroin overdose. Addiction. 2009 Dec 1;104(12):2067–74. doi: 10.1111/j.1360-0443.2009.02724.x. [DOI] [PubMed] [Google Scholar]
- 16.Robertson TM, Hendey GW, Stroh G, Shalit M. Intranasal naloxone is a viable alternative to intravenous naloxone for prehospital narcotic overdose. Prehosp Emerg Care. 2009 Jan 1;13(4):512–5. doi: 10.1080/10903120903144866. [DOI] [PubMed] [Google Scholar]
- 17.Merlin MA, Saybolt M, Kapitanyan R, et al. Intranasal naloxone delivery is an alternative to intravenous naloxone for opioid overdoses. Am J Emerg Med. 2010 Mar 31;28(3):296–303. doi: 10.1016/j.ajem.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 18.Dowling J, Isbister GK, Kirkpatrick CM, Naidoo D, Graudins A. Population pharmacokinetics of intravenous, intramuscular, and intranasal naloxone in human volunteers. Ther Drug Monitor. 2008 Aug 1;30(4):490–6. doi: 10.1097/FTD.0b013e3181816214. [DOI] [PubMed] [Google Scholar]
- 19.Zuckerman M, Weisberg SN, Boyer EW. Pitfalls of intranasal naloxone. Prehosp Emerg Care. 2014 Oct 2;18(4):550–4. doi: 10.3109/10903127.2014.896961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gladden RM. Fentanyl law enforcement submissions and increases in synthetic opioid–involved overdose deaths—27 states, 2013–2014. MMWR. 2016;65(33):837–43. doi: 10.15585/mmwr.mm6533a2. [DOI] [PubMed] [Google Scholar]
- 21.Rudd RA, Aleshire N, Zibbell JE, Matthew Gladden R. Increases in drug and opioid overdose deaths—United States, 2000–2014. MMWR. 2016;64:1378–82. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- 22.CDC. HAN Health Advisory. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. Increases in fentanyl drug confiscations and fentanylrelated overdose fatalities. Accessed December 21, 2016. Available at: http://emergency.cdc.gov/han/han00384.asp. [Google Scholar]
- 23.Kitch BB, Portela RC. Effective use of naloxone by law enforcement in response to multiple opioid overdoses. Prehosp Emerg Care. 2016 Mar 3;20(2):226–9. doi: 10.3109/10903127.2015.1076097. [DOI] [PubMed] [Google Scholar]
- 24.Food and Drug Administration. Joint Meeting of the Anesthetic and Analgesic Drug Products Advisory Committee and the Drug Safety and Risk Management Meeting Announcement. Beltsville Maryland: Oct 5, 2016. Accessed December 21, 2016. Retrieved from: https://www.fda.gov/AdvisoryCommittees/Calendar/ucm516000.htm. [Google Scholar]
- 25.Knowlton A, Weir BW, Hazzard F, et al. EMS runs for suspected opioid overdose: implications for surveillance and prevention. Prehosp Emerg Care. 2013 Jul 1;17(3):317–29. doi: 10.3109/10903127.2013.792888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lindstrom HA, Clemency BM, Snyder R, Consiglio JD, May PR, Moscati RM. Prehospital naloxone administration as a public health surveillance tool: a retrospective validation study. Prehosp Disaster Med. 2015 Aug 1;30(04):385–9. doi: 10.1017/S1049023X15004793. [DOI] [PubMed] [Google Scholar]
- 27.Merchant RC, Schwartzapfel BL, Wolf FA, Li W, Carlson L, Rich JD. Demographic, geographic, and temporal patterns of ambulance runs for suspected opiate overdose in Rhode Island, 1997-2002. Subst Use Misuse. 2006 Jan 1;41(9):1209–26. doi: 10.1080/10826080600751898. [DOI] [PubMed] [Google Scholar]
- 28.Mann NC, Kane L, Dai M, Jacobson K. Description of the 2012 NEMSIS public-release research dataset. Prehosp Emerg Care. 2015 Apr 3;19(2):232–40. doi: 10.3109/10903127.2014.959219. [DOI] [PubMed] [Google Scholar]
- 29.Wheeler E, Jones TS, Gilbert MK, Davidson PJ. Opioid overdose prevention programs providing naloxone to laypersons—United States, 2014. MMWR. 2015 Jun 19;64(23):631–5. [PMC free article] [PubMed] [Google Scholar]
- 30.Clarke SF, Dargan PI, Jones AL. Naloxone in opioid poisoning: walking the tightrope. Emerg Med J. 2005 Sep 1;22(9):612–6. doi: 10.1136/emj.2003.009613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wampler DA, Molina DK, McManus J, Laws P, Manifold CA. No deaths associated with patient refusal of transport after naloxone-reversed opioid overdose. Prehosp Emerg Care. 2011 Jun 8;15(3):320–4. doi: 10.3109/10903127.2011.569854. [DOI] [PubMed] [Google Scholar]
- 32.Levine M, Sanko S, Eckstein M. Assessing the risk of prehospital administration of naloxone with subsequent refusal of care. Prehosp Emerg Care. 2016 Mar;16:1–4. doi: 10.3109/10903127.2016.1142626. [DOI] [PubMed] [Google Scholar]
- 33.Willman MW, Liss DB, Schwarz ES, Mullins ME. Do heroin overdose patients require observation after receiving naloxone? Clin Toxicol. 2016 Nov;16:1–7. doi: 10.1080/15563650.2016.1253846. [DOI] [PubMed] [Google Scholar]
- 34.Carr BG, Caplan JM, Pryor JP, Branas CC. A meta-analysis of prehospital care times for trauma. Prehosp Emerg Care. 2006 Jan 1;10(2):198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 35.Weiner SG, Mitchell PM, Temin ES, Langlois BK, Dyer KS. Use of intranasal naloxone by basic life support providers. Prehosp Emerg Care. 2017 Feb;6:1–5. doi: 10.1080/10903127.2017.1282562. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 36.Sumner SA, Mercado-Crespo MC, Spelke MB, et al. Use of naloxone by emergency medical services during opioid drug overdose resuscitation efforts. Prehosp Emerg Care. 2016 Mar 3;20(2):220–5. doi: 10.3109/10903127.2015.1076096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boyer EW. Management of opioid analgesic overdose. NE J Med. 2012 Jul 12;367(2):146–55. doi: 10.1056/NEJMra1202561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burillo-Putze G, Miro O. Tintinalli’s Emergency medicine: a comprehensive study guide. 8th. McGraw Hill Education; 2015. (Opioids). Chapter 186. [Google Scholar]
- 39.Garza A, Dyer S. EMS data can help stop the opioid epidemic. J Emerg Med Serv. 2016 Nov 1; [Google Scholar]
- 40.Drug Enforcement Agency. DEAissues Carfentanil warning to police and public dangerous opioid 10,000 times more potent than morphine and 100 times more potent than fentanyl. DEA Public Affairs Office; Sep 22, 2016. Available at: https://www.dea.gov/divisions/hq/2016/hq092216.shtml. Accessed March 29, 2017. [Google Scholar]


