Abstract
Objectives
This study assessed influences on vaccination decisions among parents of young children and examined common vaccination information and advice sources.
Methods
Using panel samples of parents of children under 7 years, web-based surveys were conducted in 2012 (n = 2603) and 2014 (n = 2518). A vaccine decision-making typology (non-hesitant acceptors, hesitant acceptors, delayers, and refusers) was established and weighted population estimates of potential factors influencing parental vaccination decision (e.g., provider influence, source of information and advice) were computed by year and decision type.
Results
Delayers and refusers were more likely than acceptors to know someone whose child experienced a severe reaction to a vaccine or delayed/refused vaccine(s). High proportions of delayers (2012: 33.4%, 2014: 33.9%) and refusers (2012: 49.6%, 2014: 58.6%) reported selecting their healthcare provider based on whether the provider would allow them to delay/refuse vaccines. Providers were the most frequently reported trusted vaccine information source among all parents, though more often by acceptors than refusers (2012, 2014: p < 0.01). We found differing patterns of provider advice-seeking and internet as a reliable vaccine information source by group. Among those who had considered delay/refusal, trust in their healthcare provider’s advice was the most common reason cited for their decision reversal.
Conclusions for Practice
Provider trust and communication along with varying degrees of personal-network influences likely contribute to immunization decisions of parents. Vaccine hesitant parents often seek providers amenable to accommodating their vaccine beliefs. Providers may benefit from vaccine communication training as their recommendations may influence hesitant parents to immunize their children.
Keywords: Vaccine acceptability, Vaccine delay, Vaccine hesitancy, Vaccine refusal, Pediatric populations, Parental decision-making
Introduction
National childhood vaccination rates have remained consistently high over the past decade in the United States (US) (Hill et al. 2015), with intentional vaccine delay estimated at 7.7–21.8% (McCauley et al. 2012; Smith et al. 2010) and refusal of one or more vaccines at 4.0–16% (Association of State and Territorial Health Officials 2010; Frew et al. 2016; McCauley et al. 2012). Yet, recent high profile outbreaks of measles (Zipprich et al. 2015) and pertussis (Cherry 2012) have brought the repercussions of under-immunization to national attention, sparking sometimes polarized debates on decisional freedom and the potential public risk posed by following personal health philosophy (Omer et al. 2013). As a result, some states have reduced or eliminated philosophical exemptions to childhood vaccines required for school entry (Jones and Buttenheim 2014; Oregon Health Authority 2013). Meanwhile, less attention has been paid to the equally critical issue of how parents’ vaccination decision-making is shaped by social values and community norms within networks (Frew et al. 2014; Kennedy and Gust 2005; Sobo 2015).
Some factors associated with vaccine decisions have been identified in prior studies. Healthcare providers (HCP) are the most consistently reported trusted vaccine information source among parents holding varying vaccination attitudes (Brunson 2013; Hill et al. 2015; Smith et al. 2006). Studies have also shown that trust in providers was influenced by provision of balanced risk/benefit information (Glanz et al. 2013) and by parent-provider communication behaviors (Opel et al. 2015). Many also report obtaining vaccine information from spouses/partners, friends, and online sources (Brunson 2013; Sobo 2015). This study examines key factors associated with attitudes and reported immunization decisions of parents with varying vaccination attitudes. Specifically, this study explores the influences on vaccine decisions among parents of young children, describes provider selection and personal-network characteristics, and determines vaccination information and advice sources. The goal was to identify opportunity points for targeted and tailored interventions to improve vaccine coverage by understanding these factors among subgroups of parents with varying vaccination decisions (Smith et al. 2011).
Methods
Study Design and Sample
In 2012 and 2014, national surveys of US parents and guardians of young children were conducted to measure the knowledge, beliefs and attitudes towards childhood immunization, as well as self-reported vaccination decisions for their youngest child. Participants were sampled from KnowledgePanel, a web-based research panel maintained by GfK Group, using probability-proportional-to-size sampling (GfK 2013). Panel members had been recruited using random digit dialing (1999–2008) and address-based sampling (2008-present), and selected to provide representative sampling frames for the US population on age and gender, race/Hispanic ethnicity, education, household income, census region, and metropolitan residence. Participants were 18 years and older who were parents or guardians of children under 7 years old, an age group for which the “Immunization Schedule for Infants and Children” is recommended (Centers for Disease Control and Prevention 2017). Participants were offered $5 compensation for their time.
Surveys were independently administered online from January to March 2012 and June to July 2014. Post-stratification weights were constructed using raking, allowing adjustment for differences between characteristics of the sample and US population, sampling strategy, and non-response. The 2012 and 2014, surveys were approved by the FHI360 and Westat Institutional Review Boards (IRBs), with subsequent review and determination issued by the Emory University IRB. Centers for Disease Control and Prevention (CDC) was determined to be non-engaged in the study for purposes of IRB approval.
Measurement
Childhood Vaccination Decisions
Parents were classified as “non-hesitant acceptors,” “hesitant acceptors,” “delayers,” or “refusers” based on a series of initial questions assessing their vaccination decision (discounting non-vaccination due to sickness or shortage of vaccines) for their youngest child on recommended non-influenza vaccines. “Non-hesitant acceptors” reported receiving all vaccines at the recommended time or that they were actively working to catch up on all vaccines, and further reported that they had not thought about delaying/refusing any vaccine. “Hesitant acceptors” reported receiving or working to catch up on all vaccines, but had considered delaying/refusing. “Delayers” indicated delay of some or all recommended vaccines, but did not refuse any, while “refusers” reported refusal of one or more vaccines.
“Delayers” and “refusers” were asked to report the specific vaccines delayed/refused, which was used for final decision category determination. Parents who reported delay/refusal of vaccines, but subsequently reported acceptance of all non-influenza vaccines were treated as missing in this analysis because information on hesitancy was unavailable (2012: n = 11, 2014: n = 21). Parents who indicated delay but were not certain of delay of specific vaccines were considered “delayers” so long as they did not report acceptance of all non-influenza vaccines. Parents indicating refusal were coded in the same fashion. One 2014 participant with missing outcome was accounted for by casewise deletion.
Vaccine Information Source and Decision Influences
To determine vaccine information sources, participants were asked to mark their top-three trusted vaccine information sources. Ten options were given in 2012: (1) baby’s doctor/HCP, (2) family, (3) friends, (4–7) internet choices (search engine, health information site, news site, blog/social media), (8) magazines, newspapers, radio, or television, (9) celebrity/public figure, and (10) other. In 2014, internet choices were collapsed into a single option and book was added, resulting in eight options. Participants who selected internet were asked to specify which internet source they used.
Parents were also asked to mark their top-three sources of advice on which vaccines were recommended for their youngest child. Answer choices included, (1) spouse/significant other/domestic partner (2012) and child’s other parent (2014), (2) participant’s parents/guardians, (3) other family members, (4) friends, (5) neighbors, (6) co-workers, (7) social/civic group members, (8) doctors, (9) nurses, (10) other HCP, (11, 12) other parents (young/older children), (13) none, and (14) other.
To determine provider influence, parents were asked whether a doctor, a nurse, and/or another HCP influenced their vaccination decision, and whether tolerance of vaccine delay/refusal was a consideration when selecting a doctor for their youngest child. “Hesitant acceptors” were also asked to select the reason for vaccinating as recommended despite having considered delay/refusal.
To determine potential personal-network influences, parents’ personal-networks were characterized. Participants were asked if they knew someone who had delayed/refused vaccine(s) and to indicate the relationship of these parent(s) to them. Possible responses included family, friend, neighbor, co-worker, community/religious group member, fellow parent, celebrity, and other. Parents were also asked if they knew someone (including themselves) whose child had experienced a serious reaction to a vaccine, which required medical attention. Participants were then asked to specify who these parents were in relation to them from the aforementioned list.
Statistical Analysis
Post-stratification survey weights were used to construct US population estimates for vaccine decision groups (GfK 2013). Survey weights were also used to estimate population rates for trusted sources of information and advice, provider selection and influence, and personal-network factors. Survey-appropriate adjusted chi-squared test of Rao and Scott was used to test for overall changes between 2012 and 2014 in these factors, as well as in parents’ vaccine decisions (Rao and Scott 1984).
To explore relationships between vaccination decisions and the information and influence factors, rate estimates were further stratified by vaccination decision category. Pair-wise rate differences between categories and between years were tested using adjusted chi-squared tests in contrasts of saturated multinomial logit models. All analyses were conducted using SPSS version 21.0, with the SPSS Complex Sample Module (IBM SPSS Inc., Chicago, IL, USA). Statistical significance was determined using α = 0.05 significance levels, and 95% confidence intervals (CI) constructed for point estimates.
Results
In 2012, 2603 participants qualified for and completed the survey, out of 4933 panelists contacted and 2792 who initiated the survey (response rate 56.6%, completion rate 93.2%). The 2014 sample included 2518 parents, from 4803 panelists contacted and 2618 who initiated the survey (response rate 54.5%, completion rate 96.2%).
Selected sociodemographic characteristics of participants are presented in Table 1. There were no significant differences between years in variables other than education and income. Overall, parents were accepting of all recommended non-influenza childhood vaccines and there was no significant change among the overall proportions of parents by vaccine decision group between 2012 and 2014 (p = 0.16).
Table 1.
Sociodemographic characteristics of survey respondents
| 2012 (n = 2603) | 2014 (n = 2518)
|
||
|---|---|---|---|
| Frequency (% | Frequency (% | p Value | |
| Gender | 0.91 | ||
| Male | 719 (27.6%) | 699 (27.8%) | |
| Female | 1884 (72.4%) | 1819 (72.2%) | |
| Age | 0.48 | ||
| 18–29 | 812 (31.2%) | 776 (30.8%) | |
| 30–44 | 1599 (61.4%) | 1563 (62.1%) | |
| 45–59 | 184 (7.1%) | 165 (6.6%) | |
| 60 and over | 8 (0.3%) | 14 (0.6%) | |
| Ethnicity | 0.56 | ||
| Hispanic/Latino | 363 (13.9%) | 337 (13.4%) | |
| Not Hispanic/Latino | 2224 (85.4%) | 2165 (86.0%) | |
| Missing or refused | 16 (0.6%) | 16 (0.6%) | |
| Racea | 0.12 | ||
| White only | 2059 (79.1%) | 1989 (79.0%) | |
| Black or African American only | 260 (10.0%) | 238 (9.5%) | |
| American Indian or Alaska native only | 20 (0.8%) | 17 (0.7%) | |
| Asian only | 91 (3.5%) | 85 (3.4%) | |
| Native Hawaiian or Pacific Islander only | 17 (0.7%) | 9 (0.4%) | |
| Other single race | 65 (2.5%) | 57 (2.3%) | |
| Multiple race | 55 (2.1%) | 84 (3.3%) | |
| Missing or refused | 36 (1.4%) | 39 (1.5%) | |
| Educational attainment | 0.01 | ||
| High school degree or less | 468 (18.0%) | 385 (15.3%) | |
| Some college | 916 (35.2%) | 871 (34.6%) | |
| Bachelor’s degree or more | 1219 (46.8%) | 1262 (50.1%) | |
| Annual household income | <0.001 | ||
| <$20,000 | 410 (15.8%) | 305 (12.1%) | |
| $20,000–$39,999 | 561 (21.6%) | 505 (20.1%) | |
| $40,000–$59,999 | 463 (17.8%) | 450 (17.9%) | |
| $60,000–$99,999 | 714 (27.4%) | 757 (30.1%) | |
| $100,000 or more | 455 (17.5%) | 501 (19.9%) | |
| Residence in metropolitan statistical area | 0.43 | ||
| Metropolitan | 2218 (85.2%) | 2165 (86.0%) | |
| Non-metropolitan | 385 (14.8%) | 353 (14.0%) | |
| Geographic region of residence | 0.69 | ||
| Northeast | 357 (13.7%) | 351 (13.9%) | |
| Midwest | 730 (28.0%) | 673 (26.7%) | |
| South | 869 (33.4%) | 840 (33.4%) | |
| West | 647 (24.9%) | 654 (26.0%) | |
| Vaccination decision | 0.18 | ||
| Non-hesitant acceptorb | 1761 (67.7%) | 1748 (69.4%) | |
| Hesitant acceptorc | 493 (18.9%) | 465 (18.5%) | |
| Delayerd | 191 (7.3%) | 171 (6.8%) | |
| Refusere | 147 (5.6%) | 112 (4.4%) | |
| Missing | 11 (0.4%) | 22 (0.9%) | |
Race was assessed separately from Hispanic ethnicity; persons reporting Hispanic ethnicity may be of any race
Parents who accepted all recommended non-influenza vaccines and those actively working to catch up who reported not thinking about delaying/refusing any vaccine
Parents who specified as having thought about delaying/refusing any vaccine but accepted all recommended non-influenza vaccines or are actively working to catch up
Parents who indicated delay, or possible delay, but unsure, of at least one non-influenza vaccine, but did not refuse any
Parents who indicated refusal, or possible refusal, but unsure, of at least one non-influenza vaccine
The largest proportion of “refusers” reported selecting a provider based on non-vaccination tolerance (Fig. 1). The proportion of “non-hesitant acceptors” who reported selecting a provider based on a vaccine opt-out permissiveness decreased significantly from 2012 to 2014 (p = 0.02). For all other decision groups, the proportions remained stable.
Fig. 1.
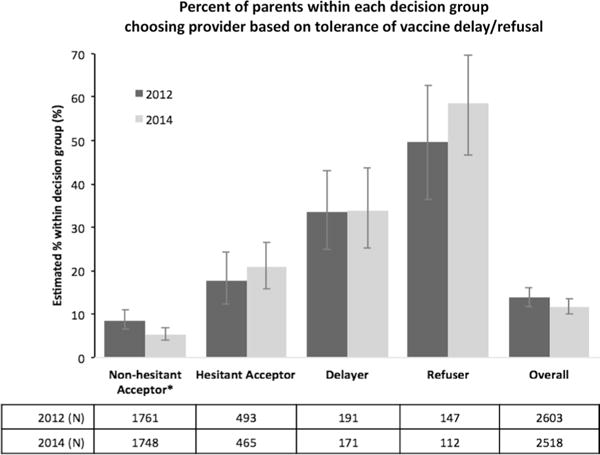
Healthcare provider selection based on provider’s willingness to allow delay/refusal of vaccine(s) by non-influenza vaccine decision and by survey year. Error bars indicate 95% CI of the point estimate for each decision group. *Rate is significantly different by survey year with p < 0.05
Provider Influence
The largest proportion of “hesitant acceptors” reported that a doctor influenced their vaccine decision for their child in both years (Fig. 2a). The proportion of parents reporting that a doctor influenced their decision remained stable for all decision groups. The proportion of parents reporting that a nurse influenced their decision declined among “non-hesitant acceptors” (p = 0.008) and “delayers” (p = 0.03) from 2012 to 2014 (Fig. 2b). The proportion of parents reporting that another HCP (e.g., pharmacist, physician assistant) influenced their decision decreased significantly among “non-hesitant acceptors” (p = 0.002) (Fig. 2c).
Fig. 2.
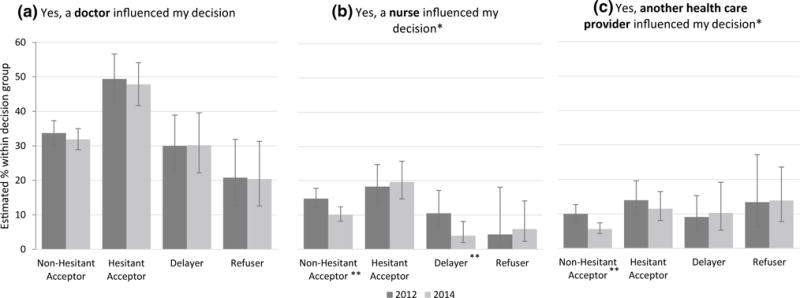
Healthcare provider influence on decision about vaccination by non-influenza vaccine decision and by survey year. Participants were asked the following questions: Did a a doctor, b a nurse, c another healthcare provider influence your decision about vaccinating your youngest child? Error bars indicate 95% CI of the point estimate for each decision group. Non-hesitant acceptor (2012: N = 1761, 2014: N = 1748), hesitant acceptor (2012: N = 493, 2014: N = 465), delayer (2012: N = 191, 2014: N = 171), refuser (2012: N = 147, 2014: N = 112). *Overall distribution of rates among vaccine decision groups is significantly different between survey years with p < 0.05.
**Rate within this vaccine decision group is significantly different between survey years with p < 0.01
In 2014, respondents who reported that a doctor, a nurse, and/or another HCP influenced their vaccination decision were asked if the provider made them more or less likely to vaccinate. Most “non-hesitant acceptors,” “hesitant acceptors,” and “delayers” reported that a doctor/nurse made them more likely to vaccinate, whereas most “refusers” reported that a doctor/nurse made them less likely to vaccinate (Table 2). When asked about another HCP influence, most “non-hesitant acceptors” and “hesitant acceptors” reported that another HCP made them more likely to vaccinate, while most “delayers” and “refusers” reported that another HCP made them less likely to vaccinate.
Table 2.
Population estimates of positive/negative healthcare provider influence among parents indicating provider influence, by non-influenza vaccine decision for youngest child in 2014
| Non-hesitant acceptor Est. (95% CI) |
Hesitant acceptor Est. (95% CI) |
Delayer Est. (95% CI) |
Refuser Est. (95% CI) |
Overall Est. (95% CI) |
|
|---|---|---|---|---|---|
| A doctor made me ________ to vaccinate | (n = 487)a | (n = 215)a | (n = 57)a | (n = 23)a | (n = 782)a |
| More likely | 97.4% (94.7, 98.7%) | 91.6% (83.0, 96.1%) | 92.5% (84.0, 96.7%) | 25.4% (11.0, 48.5%)d | 94.1% (91.4, 96.0%) |
| Less likely | 2.6% (1.3, 5.3%) | 8.4% (3.9, 17.0%) | 7.5% (3.3, 16.0%) | 74.6% (51.5, 89.0%)d | 5.9% (4.0, 8.6%) |
| A nurse made me ________ to vaccinate | (n = 144)b | (n = 74)b | (n = 10)b | (n = 6)b | (n = 234)b |
| More likely | 89.4% (81.2, 94.3%) | 88.4% (78.7, 94.1%) | 67.2% (33.6, 89.3%) | 13.8% (2.7, 48.3%)d,e | 87.3% (81.3, 91.5%) |
| Less likely | 10.6% (5.7, 18.8%) | 11.6% (5.9, 21.3%) | 32.8% (10.7, 66.4%) | 86.2% (51.7, 97.3%)d,e | 12.7% (8.5, 18.7%) |
| Another HCP made me ________ to vaccinate | (n = 89)c | (n = 54)c | (n = 18)c | (n = 15)c | (n = 176)c |
| More likely | 94.4% (88.5, 97.3%) | 83.5% (70.3, 91.5%) | 16.5% (5.6, 39.8%)d | 2.1% (0.3, 14.8%)d | 78.6% (70.3, 85.0%) |
| Less likely | 5.6% (2.7, 11.5%) | 16.5% (8.5, 29.7%) | 83.5% (60.2, 94.4%)d | 97.9% (85.2, 99.7%)d | 21.4% (15.0, 29.7%) |
Est. weighted US population estimate, HCP healthcare provider, CI confidence interval
Estimates are percentage of parents indicating the response from among parents who indicated that a doctor influenced their vaccination decision
Estimates are percentage of parents indicating the response from among parents who indicated that a nurse influenced their vaccination decision
Estimates are percentage of parents indicating the response from among parents who indicated that another healthcare provider influenced their vaccination decision
Estimates of this decision group differ significantly from “non-hesitant acceptors” and “hesitant acceptors” (p < 0.001)
Estimates of this decision group differ significantly from “delayers” (p < 0.05)
Also highlighting this positive influence, we found that among “hesitant acceptors,” trust in doctor/HCP advice was most the commonly cited reason to change their mind and accept all recommended vaccine(s) [2012: 43.6% (36.5–51.0%); 2014: 41.5% (35.4–47.9%)], which was followed by “I just thought more about it” [2012: 37.4% (30.5–44.9%); 2014: 37.9% (31.8–44.3%)] and “day care/school/travel requirement” [2012: 15.0% (10.7–20.7%); 2014: 18.2% (13.6–24.0%)].
Personal-Network Characteristics
In both years, the largest proportion of “refusers” reported knowing someone whose child had experienced a severe vaccine reaction (Table 3). “Delayers” and “refusers” were more likely to report knowing someone, compared to “non-hesitant acceptors” or “hesitant acceptors.” Overall, of the parents who reported knowing someone, most cited knowing a “friend” [2012: 42.9% (34.6–51.6%); 2014: 45.1% (37.7–52.6%)], followed by “my child” [2012: 29.0% (21.5–37.9%); 2014: 18.2% (12.2–26.1%)], and “family member” [2012: 13.9% (10.1–19.0%); 2014: 23.0% (17.5–29.8%)].
Table 3.
Population estimates of parents’ personal network characteristics by survey year and by non-influenza vaccination decision
| Non-hesitant acceptor Est (95% CI) |
Hesitant acceptor Est (95% CI) |
Delayer Est (95% CI) |
Refuser Est (95% CI) |
|
|---|---|---|---|---|
| Know someone whose child has experienced a severe reaction † to a vaccine | ||||
| 2012 | 8.4% (6.4–11.0%)* | 14.4% (10.5–19.3%) | 31.1% (22.4–41.4%)a | 53.7% (40.4–66.4%)a,b |
| 2014 | 5.2% (4.1–6.5%)* | 17.4% (13.0–23.0%) | 35.1% (26.4–44.9%)a | 46.0% (34.3–58.1%)a |
| Know someone who chose to delay their child’s vaccination(s) | ||||
| 2012 | 32.1% (28.9–35.6%) | 52.9% (45.5–60.1%) | 80.6% (72.1–86.9%)a | 90.0% (83.1–94.3%)a,c |
| 2014 | 33.1% (30.3–36.0%) | 54.2% (47.9–60.4%) | 87.4% (80.2–92.2%)a | 85.5% (75.9–91.7%)a |
| Know someone who chose to refuse their child’s vaccination(s) | ||||
| 2012 | 23.2% (20.4–26.2%) | 38.6% (32.0–45.7%) | 58.4% (48.4–67.8%)d,e | 87.6% (77.3–93.6%)a,f |
| 2014 | 24.1% (21.7–26.7%) | 44.1% (38.2–50.3%) | 60.3% (49.7–70.0%)d,g | 85.8% (76.5–91.8%)a,f |
Est. weighted US population estimate, CI confidence interval
Severe reaction was defined as reactions that required medical attention and could not be treated at home
Rate is significantly different between survey years with p < 0.01
Estimates of this decision group differ significantly from “non-hesitant acceptors” and “hesitant acceptors” (p ≤ 0.001)
Estimates of this decision group differ significantly from “delayers” (p < 0.01)
Estimates of this decision group differs significantly from “delayers” (p < 0.05)
Estimates of this decision group differ significantly from “non-hesitant acceptors” (p ≤ 0.001)
Estimates of this decision group differ significantly from “hesitant acceptors” (p < 0.01)
Estimates of this decision group differ significantly from “delayers” (p < 0.001)
Estimates of this decision group differ significantly from “hesitant acceptors” (p < 0.05)
The largest proportion of “delayers” and “refusers” reported knowing someone who chose to delay/refuse vaccine(s); conversely, “non-hesitant acceptors” comprised the smallest proportion (Table 3). “Delayers” and “refusers” were more likely to report knowing someone, compared to “non-hesitant acceptors” and/or “hesitant acceptors.” Overall, of the parents who reported knowing someone who delayed vaccine(s), most cited knowing a “friend” [2012: 62.9% (58.5–67.1%); 2014: 60.8% (57.0–64.5%)], followed by a “family member” [2012: 29.2% (25.1–33.7%); 2014: 26.7% (23.4–30.3%)]. Similarly, of the parents who reported knowing someone who refused vaccine(s), most cited knowing a “friend” [2012: 58.3% (53.2–63.2%); 2014: 58.3% (53.9–62.5%)], followed by “family member” [2012: 27.7% (23.3–32.5%); 2014: 26.8% (23.0–31.1%)].
Trusted Sources of Information and Advice
Most respondents, regardless of decision group, cited HCP among their top-three trusted sources for vaccine information. The second and third most commonly cited sources varied slightly by decision group. In 2012 and 2014 “family members” and “internet” were the second and third most commonly cited sources for “non-hesitant acceptors” and “hesitant acceptors.” In 2012, “internet” and “family members” were the second and third most commonly cited sources for “delayers” and “refusers.” However in 2014, the second and third most commonly reported sources were “family members” and “internet” for “delayers,” and “internet” and “books” for “refusers.” The majority of parents who reported using the internet indicated that they referred to health information sites (e.g. CDC, AAP, WebMD) [76.6% (66.5–75.1%)], followed by search engines (e.g. Google, Yahoo!) [46.3% (43.2–49.4%)].
The most commonly cited source of advice for understanding recommended vaccines for youngest child was “doctors” regardless of decision group. In 2012, we also found that across groups, parents turned to their “spouse/significant other/domestic partner” for advisement. In 2014, this shifted for “non-hesitant acceptors,” when the second most commonly cited source became “nurses.” We found some variation between years and among groups on the third most commonly cited source as they cited “nurses,” “participant’s parents/guardians,” “other family members,” “other HCPs,” “friends,” and “other.”
Discussion
This study offers interesting insight on clinical and social dynamics related to various levels of vaccine hesitancy beyond those found in other settings such as schools (Kennedy and Gust 2005; Sobo 2015). To our knowledge, this is one of the first studies that have looked closely at various self-reported influences by subgroups of acceptors (i.e. hesitant and non-hesitant) along with parents who delayed or refused vaccines. Characterization of the “hesitant acceptors” was of particular interest, as these parents, at one point, could have delayed or refused vaccines.
Provider selectivity increased with increasing levels of hesitancy, with parents who reported refusing vaccine(s) being the most purposive in their selection of providers perceived as sympathetic to their vaccination decision. Providers may find that even when they spend the time to discuss vaccines with concerned parents, their interventions can still be ineffective in increasing timely vaccination (Kempe et al. 2015). The implementation of practice-based dismissal policies requiring parents who refuse to follow the recommended schedule to look for another provider may result in fewer options for parents who want to refuse/delay vaccines (Omer et al. 2009; Schwartz 2013). Consistent rates of increased provider selectivity with increased vaccine hesitancy observed in this study reflect this situation of parents potentially clustering into practices with providers that allow non-vaccination. This provider selectivity of vaccine hesitant parents highlights potential epidemiologic implications, particularly if community and clinical interventions are not implemented to reduce vaccine hesitancy in specific geographic settings where there may be greater vaccine delay/refusal and lower coverage (Dube et al. 2015; Lieu et al. 2015). Thus, the findings point to the need to develop communication interventions for providers, which may increase effective patient-provider discussions, reduce the need for patient dismissal, decrease provider selectivity, and minimize clustering of vaccine hesitant families within specific practices (Dube et al. 2015; Sadaf et al. 2013).
Study results indicated that across vaccine decision groups, HCPs are a consistent, trusted and influential source of vaccine-related information, which also opens up great potential for improved patient-provider communication strategies (Smith et al. 2006). In particular, it was encouraging to learn that “hesitant acceptors” trusted their physician’s advice. Parents who reported delaying or refusing vaccines also reported physicians as a vital vaccine information source but at lower rates, indicating the need to learn more about the information needs of these parents. By learning what information is effective in leading to vaccine acceptance, new strategies may be formulated using varying content and delivery formats tailored to each group (Opel et al. 2015).
In contrast to physician influence, much lower rates of reported nurses’ influence on vaccine decision-making were observed. This may be due to nurses, with the exception of nurse practitioners, typically being the ones to administer rather than discuss vaccines following physician orders (Scott and Batty 2016). Nonetheless, the need for interventions for pediatric nurses who administer vaccines or have conversations with parents about vaccine concerns are in line with these findings (Stinchfield 2001).
Among all participants, parents who reported refusing vaccine(s) were the least likely to report that providers influenced their decision. These parents most often cited doctor/HCP as a trusted source of vaccine information and advice, however, at lower rates compared to other decision groups. Parents who refused vaccine(s) also reported using the internet and books for vaccine information and turning to their spouse/partner for vaccine advice at higher rates compared to other participants. These findings suggest that for some vaccine hesitant parents, decisions may occur outside of the clinical encounter, based on information gathered from these various sources other than a HCP (Dube et al. 2015; Sobo 2015). Thus, it may be important for HCPs to draw out parents’ vaccination positions so that tailored strategies such as non-adversarial discussions may be used for vaccine hesitant parents (Leask et al. 2012). To address vaccine hesitancy and refusal, content analysis of the key sources of vaccine information (e.g., internet sites and books) and personal-network analyses may yield further insight on message development and dissemination approaches within personal networks. In 2014, most parents who reported refusing vaccine(s) reported that HCPs made them less likely, rather than more likely to vaccinate. This may have been a result of poor patient-provider communication, reemphasizing the need for vaccine communication interventions.
Finally, significant effects among personal networks were identified. Parents who delayed or refused vaccine(s) were more likely than acceptors to report knowing someone who refused, delayed, or had a child who experienced a severe vaccine reaction, most of whom were friends, family members, and themselves. It is possible that for some parents their networks helped shape immunization decisions, while for others they may have chosen networks with individuals holding similar values (Nickerson 1998). Although causal inferences cannot be made due to the cross-sectional nature of the study, these findings highlight the important role past experiences (e.g. parents’ own or their networks’) may play in shaping or confirming parents’ immunization decisions. Parents also often cited family as a trusted information source for immunization decision-making. As demonstrated in other studies, families have a strong impact on decision-making due to strong interpersonal dynamics and shared histories of illness and prevention options (Bronfenbrenner 1994; Frew et al. 2013, 2014). Thus, it is important that any vaccine messages and interventions also target information to families, as the potential for dissemination is highly likely to inform future immunization decisions (Frew et al. 2014).
Limitations
Limitations of self-reported vaccination decision estimates include the possibility of recall bias and social desirability bias. Although the survey was designed to be representative of the US population, vaccine attitudes and experiences of the surveyed parents may not be fully generalizable. A few of the survey questions’ answer choices changed slightly between 2012 and 2014 and may have influenced survey responses (e.g., response options for top-three trusted source of information were collapsed and “book” was added as a choice in 2014; directionality was introduced on doctor/nurse/another provider influence items). However, most variation was observed within less commonly reported answer choices and findings of this study are congruent with previous studies.
Conclusions
Across vaccine decision groups, provider trust and communication along with varying degree of personal network influence likely contributes to parents’ immunization decisions for their young children. Thus interventions targeted to parents addressing normative values and opinions may increase vaccine uptake. Additionally, HCP may benefit from vaccine communication training for addressing parents’ concerns as their recommendations may influence otherwise reluctant parents to immunize their children.
Significance.
What’s known on this subject
Previous studies have suggested that healthcare providers serve an important role for parents as trusted sources of vaccine information and advice.
What this study adds
This study examines the various potential influencers of parental vaccination decision by vaccine decision category between 2012 and 2014 to determine if different approaches and channels need to be considered to reach parents who intentionally delay or refuse vaccines.
Acknowledgments
The authors would like to acknowledge all the poll participants of this study. This research was supported in part by a grant from the Centers for Disease Control and Prevention (CDC) and an appointment to the Research Participation Program at the CDC administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC. The findings and conclusions in this report are those of the authors, and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Association of State and Territorial Health Officials. Communicating effectively about vaccines: Summary of a survey of US parents and guardians Arlington, VA. 2010 Retrieved from http://www.astho.org/Programs/Immunization/Communicating-Effectively-About-Vaccines-Summary-of-a-Survey-of-U-S-Parents-and-Guardians/.
- Bronfenbrenner U. International encyclopedia of education. 2nd. Vol. 3. Oxford: Elsevier; 1994. Ecological models of human development. [Google Scholar]
- Brunson EK. The impact of social networks on parents’ vaccination decisions. Pediatrics. 2013;131(5):e1397–e1404. doi: 10.1542/peds.2012-2452. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Immunization Schedules for Infants and Children. 2017 February 6, 2017. Retrieved from https://www.cdc.gov/vaccines/schedules/easy-to-read/child.html.
- Cherry JD. Epidemic pertussis in 2012—The resurgence of a vaccine-preventable disease. New England Journal of Medicine. 2012;367(9):785–787. doi: 10.1056/NEJMp1209051. [DOI] [PubMed] [Google Scholar]
- Dube E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Review of Vaccines. 2015;14(1):99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- Frew PM, Fisher AK, Basket MM, Chung Y, Schamel J, Weiner JL, Orenstein WA. Changes in childhood immunization decisions in the United States: Results from 2012 & 2014 National Parental Surveys. Vaccine. 2016;34(46):5689–5696. doi: 10.1016/j.vaccine.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frew PM, Saint-Victor DS, Owens LE, Omer SB. Socioecological and message framing factors influencing maternal influenza immunization among minority women. Vaccine. 2014;32(15):1736–1744. doi: 10.1016/j.vaccine.2014.01.030. [DOI] [PubMed] [Google Scholar]
- Frew PM, Zhang S, Saint-Victor DS, Schade AC, Benedict S, Banan M, Omer SB. Influenza vaccination acceptance among diverse pregnant women and its impact on infant immunization. Human Vaccines Immunotherapeutics. 2013;9(12):2591–2602. doi: 10.4161/hv.26993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GfK. KnowledgePanel Design Summary. 2013 Retrieved from http://www.knowledgenetworks.com/knpanel/docs/knowledgepanel(R)-design-summary-description.pdf.
- Glanz JM, Wagner NM, Narwaney KJ, Shoup JA, McClure DL, McCormick EV, Daley MF. A mixed methods study of parental vaccine decision making and parent-provider trust. Academic Pediatrics. 2013;13(5):481–488. doi: 10.1016/j.acap.2013.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill HA, Elam-Evans LD, Yankey D, Singleton JA, Kolasa M. National, State, and selected local area vaccination coverage among children aged 19–35 months—United States, 2014. MMWR Morbidity and Mortality Weekly Report. 2015;64(33):889–896. doi: 10.15585/mmwr.mm6433a1. [DOI] [PubMed] [Google Scholar]
- Jones M, Buttenheim A. Potential effects of California’s new vaccine exemption law on the prevalence and clustering of exemptions. American Journal of Public Health. 2014;104(9):e3–e6. doi: 10.2105/AJPH.2014.302065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempe A, O’Leary ST, Kennedy A, Crane LA, Allison MA, Beaty BL, Stokley S. Physician response to parental requests to spread out the recommended vaccine schedule. Pediatrics. 2015 doi: 10.1542/peds.2014-3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy AM, Gust DA. Parental vaccine beliefs and child’s school type. Journal of School Health. 2005;75(7):276–280. doi: 10.1111/j.1746-1561.2005.00037.x. [DOI] [PubMed] [Google Scholar]
- Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: A framework for health professionals. BMC Pediatrics. 2012;12:154. doi: 10.1186/1471-2431-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieu TA, Ray GT, Klein NP, Chung C, Kulldorff M. Geographic clusters in underimmunization and vaccine refusal. Pediatrics. 2015;135(2):280–289. doi: 10.1542/peds.2014-2715. [DOI] [PubMed] [Google Scholar]
- McCauley MM, Kennedy A, Basket M, Sheedy K. Exploring the choice to refuse or delay vaccines: A national survey of parents of 6-through 23-month-olds. Academic Pediatrics. 2012;12(5):375–383. doi: 10.1016/j.acap.2012.06.007. [DOI] [PubMed] [Google Scholar]
- Nickerson RS. Confirmation bias: A ubiquitous phenomenon in many guises. Review of General Psychology. 1998;2(2):175. [Google Scholar]
- Omer SB, Orenstein WA, Koplan JP. Go big and go fast–vaccine refusal and disease eradication. New England Journal of Medicine. 2013;368(15):1374–1376. doi: 10.1056/NEJMp1300765. [DOI] [PubMed] [Google Scholar]
- Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. New England Journal of Medicine. 2009;360(19):1981–1988. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- Opel DJ, Mangione-Smith R, Robinson JD, Heritage J, DeVere V, Salas HS, Taylor JA. The influence of provider communication behaviors on parental vaccine acceptance and visit experience. American Journal of Public Health. 2015;105(10):1998–2004. doi: 10.2105/ajph.2014.302425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oregon Health Authority. New process for claiming non-medical exemptions to school immunization requirements begins March. 2013;1:2014. [Google Scholar]
- Rao JNK, Scott AJ. On chi-squared tests for multiway contingency tables with cell proporitions estimated from survey data. Annals of Statistics. 1984;12(1):46–60. [Google Scholar]
- Sadaf A, Richards JL, Glanz J, Salmon DA, Omer SB. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine. 2013;31(40):4293–4304. doi: 10.1016/j.vaccine.2013.07.013. [DOI] [PubMed] [Google Scholar]
- Schwartz JL. “Model” patients and the consequences of provider responses to vaccine hesitancy. Human Vaccines & Immunotherapeutics. 2013;9(12):2663–2665. doi: 10.4161/hv.26371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott K, Batty ML. HPV vaccine uptake among canadian youth and the role of the nurse practitioner. Journal of Community Health. 2016;41(1):197–205. doi: 10.1007/s10900-015-0069-2. [DOI] [PubMed] [Google Scholar]
- Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, Hibbs B. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Reports. 2011;126(Suppl 2):135–146. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PJ, Humiston SG, Parnell T, Vannice KS, Salmon DA. The association between intentional delay of vaccine administration and timely childhood vaccination coverage. Public Health Reports (Washington, D C: 1974) 2010;125(4):534–541. doi: 10.1177/003335491012500408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics. 2006;118(5):e1287–e1292. doi: 10.1542/peds.2006-0923. [DOI] [PubMed] [Google Scholar]
- Sobo EJ. Social cultivation of vaccine refusal and delay among Waldorf (Steiner) school parents. Medical Anthropology Quarterly. 2015 doi: 10.1111/maq.12214. [DOI] [PubMed] [Google Scholar]
- Stinchfield PK. Ask the expert: Vaccine safety communication: The role of the pediatric nurse. Journal for Specialists in Pediatric Nursing. 2001;6(3):143–146. doi: 10.1111/j.1744-6155.2001.tb00136.x. [DOI] [PubMed] [Google Scholar]
- Zipprich J, Winter K, Hacker J, Xia D, Watt J, Harriman K, Centers for Disease Control and Prevention Measles outbreak—California, December 2014-February 2015. MMWR Morbidity and Mortality Weekly Report. 2015;64(6):153–154. [PMC free article] [PubMed] [Google Scholar]


