Abstract
It was quoted recently in the literature that “The risk of death associated with childbirth is approximately 14 times higher than with abortion.” This statement is unsupported by the literature and there is no credible scientific basis to support it. A reasonable woman would find any discussion about the risk of dying from a procedure as material, i.e., important and significant. In order for the physician–patient informed consent dialogue to address this critical issue, the physician must rely upon objective and accurate information concerning abortion. There are numerous and complicated methodological factors that make a valid scientific assessment of abortion mortality extremely difficult. Among the many factors responsible are incomplete reporting, definitional incompatibilities, voluntary data collection, research bias, reliance upon estimations, political correctness, inaccurate and/or incomplete death certificate completion, incomparability with maternal mortality statistics, and failing to include other causes of death such as suicides. Given the importance of this disclosure about abortion mortality, the lack of credible and reliable scientific evidence supporting this representation requires substantial discussion.
Keywords: Maternal mortality, Childbirth, Elective abortion
Abortion Mortality: Mythology and Methodology
It was quoted recently in the literature that “The risk of death associated with childbirth is approximately 14 times higher than with abortion” (Raymond and Grimes 2012). This statement is unsupported by the literature and there is no credible scientific basis to support it.
A reasonable woman would find any discussion about the risk of dying from a procedure as material, i.e. important and significant. In order for the physician–patient informed consent dialogue to address this critical issue, the physician must rely upon objective and accurate information concerning abortion. There are numerous and complicated methodological factors that make a valid scientific assessment of abortion mortality extremely difficult. Among the many factors responsible are incomplete reporting, definitional incompatibilities, voluntary data collection, research bias, reliance upon estimations, political correctness, inaccurate and/or incomplete death certificate completion, incomparability with maternal mortality statistics, and failing to include other causes of death such as suicides.
Given the importance of this disclosure about abortion mortality, the lack of credible and reliable scientific evidence supporting this representation requires substantial discussion.
Abortion data are unreliable
For any assessment of the health risks of abortion, it is necessary to obtain complete statistics on the incidence and prevalence of abortion as well as its mortality and morbidity in the USA. But, there is no federal reporting requirement and thus, only estimates are available (see, for example, Grimes 2006; Raymond and Grimes 2012). Only 26 states require providers to report abortion complications to the Centers for Disease Control (CDC) (Saul 1998; Guttmacher Institute 2009). States that do report incidence data are plagued by incomplete and inconsistent reporting, underreporting, and the lack of a national legal mandate to report.1 Abortion data are simply not complete and those provided are merely estimates with huge variance, and are subject to considerable error. Current incidence estimates by the CDC exclude abortions in California, District of Columbia, New Hampshire, and New Jersey. The CDC data are unreliable because they base their estimates on voluntary submissions by state health departments, whose accuracy is widely acknowledged to be inconsistent and unreliable. “Many state health departments are able to obtain only incomplete data from abortion providers, and in some states, only 40–50 percent of abortions are reported” (Jones et al. 2008). Furthermore, CDC data regarding maternal mortality are collected by two different agencies using two different definitions and data sources: the National Vital Statistics System (NVSS) and the Pregnancy Mortality Surveillance System (PMSS). For the years 1995–1997, the NVSS reported 898 maternal deaths and the PMSS system reported 1,387 pregnancy related deaths. Therefore the total number of pregnancy related deaths for the time period was the 1,387 documented in the PMSS system. However, only 54 percent of pregnancy related deaths were reported in both systems (MacKay et al. 2005). This disparity in reporting demonstrates that even within the CDC, there is lack of comparability of data regarding pregnancy related deaths. It is from this inaccurate data that abortion mortality data is derived, and, as a result, the CDC has cautioned medical professionals to not make comparative statements based upon CDC data.
The only other institution which collects abortion data is the Guttmacher Institute (GI).
The abortion reporting by GI is based on voluntary submissions in their periodic polling of abortion providers who are simply asked to guesstimate the number of procedures performed, by trimester, proximity to provider, etc. The scientific validity and utility of this unconventional data gathering method is minimal since it does not capture all providers, who in turn are simply estimating annual data. It cannot be relied upon in identifying national incidence. Despite this, in this case, GI submitted a sworn affidavit that the only data they rely upon is that provided by the CDC, which is inherently unreliable. GI is a special affiliate of Planned Parenthood Federation of America, the largest single provider of abortions in this country. GI is an advocacy center whose expressed purpose is to broadly support abortion rights and to limit abortion regulation: “The Institute works to protect, expand and equalize access to information, services and rights that will enable women and men to…exercise the right to choose abortion…” (http://www.guttmacher.org/about/mission.html). Because GI seeks to protect abortion rights, it would be disinclined to provide data which could interfere with unrestricted abortion. Also, in GI's periodic survey of abortion providers, physicians performing abortions face an obvious conflict of interest: disclosure of abortion complications may fuel state laws restricting access if GI publishes all data gathered. In short, GI data are not credible as it is incomplete and inherently biased. Even GI's own publications confirm this: “Without question, reputable published science should tell readers about potential conflicts of interest” (Sonfield 2005), which it obviously does not do.
There are other methodological problems with abortion data that make it largely unreliable:
-
a.
It is widely acknowledged that abortion is underreported in the U.S. with less than half of all abortions reported by women in face-to-face interviews (Jones and Kost 2007). The most likely effect of this systematic underreporting across studies is an overly favorable assessment of health risks due to abortion since women often do no report their abortion history (Jones and Kost 2007).
-
b.
There are no fetal death certificates issued when an abortion occurs. Abortions are often underreported by women and thus do not appear in their medical records. As a result, disease state or complications are not linked to abortion since it is largely not reported and thus, invisible in epidemiological research. When the patient's medical records are incomplete, any aggregated abortion mortality or morbidity reporting and analyses reflect this systematic bias.
-
c.
Most women do not return to the abortion clinic for follow-up care and assessment. Many abortion providers do not have after hours contact numbers or merely send patients with problems post-abortion to local emergency rooms to be seen by other healthcare providers. It has been estimated that more than two out of three women do not return for follow-up appointments at the abortion clinic (Picker Institute 1999).
Definitional issues regarding maternal mortality are problematic and not comparable
The numbers of women who die from abortion are largely unknown due to poor quality reporting and definitional issues. Abortion-related deaths are captured in some standardized definitions but not in others where they are undifferentiated from spontaneous abortions (Chang et al. 2003; Harrison 2009). The World Health Organization (WHO) has acknowledged: “…all existing estimates of maternal mortality are subject to greater or lesser degrees of uncertainty” (World Health Organization 2004). Because the data are so incomplete, the WHO has used seven different methods to estimate maternal death (World Health Organization 2004, 2007). Maternal mortality is difficult to measure precisely because routine recording of deaths tend not to be complete within civil registration systems. Even if such deaths were recorded, the woman's pregnancy status may not have been known and the death would therefore not have been reported as a maternal death even if the woman had been pregnant. Horon (2005) estimated that physicians completing death certificates after a maternal death fail to report that the woman was pregnant or had a recent pregnancy in 50 percent or more of the cases. In most developing-country settings where medical certification of cause of death does not exist, accurate attribution of female deaths as maternal death is difficult to impossible. Even in developed countries where routine registration of deaths is in place, maternal deaths may be considerably underreported (World Health Organization 2007). Additionally, reliance upon death certificates in maternal mortality assessments has been shown to be considerably unreliable and underestimates abortion related mortality (Reardon et al. 2004a).
Abortion-related deaths are not easily or accurately identified. Among the definitions used to capture abortion mortality are:
- Maternal deaths are defined by the WHO as the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. Suicide, unintentional injuries, or homicide are not included as causes of death in this definition (Deneux-Tharaux et al. 2005). In WHO's International Classification of Diseases, coding criteria obfuscated deaths by requiring only complications be reported versus the treatment itself. According to the WHO (2004, 4) “all existing estimates of maternal mortality are subject to greater or lesser degrees of uncertainty.”
- Late maternal deaths are defined as “the deaths of a woman from direct or indirect obstetric causes more than 42 days but less than one year after termination of pregnancy.”
- Pregnancy-related deaths, including from direct and indirect obstetric causes, are defined as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the cause of death.” Direct obstetric deaths: “those resulting from obstetric complications of the pregnant state (pregnancy, labor, and puerperium), from interventions, omissions, incorrect treatment, or from a chain of events resulting from any of the above.” Indirect obstetric deaths: “…those resulting from previous existing disease or disease that developed during pregnancy and which was not due to direct obstetric causes, but which was aggravated by physiologic effects of pregnancy” (Hoyert 2007). In the U.S. Abortion Mortality Surveillance System, Elam-Evans et al. (2003) concluded that existing methods and systems for capturing abortion related deaths are inadequate and underreported.
- Pregnancy-associated deaths, developed by the Centers for Disease Control and Prevention, and with the Maternal Mortality Special Interest Group of the American College of Obstetricians and Gynecologists, define a death from any cause during pregnancy or within 1 calendar year of delivery or pregnancy termination, regardless of the duration or anatomical site of the pregnancy (Wilcox and Marks 1995). Pregnancy-associated deaths include not only deaths commonly associated with pregnancy such as hemorrhage, pregnancy-induced hypertension, and embolism—which are captured in the WHO definition—but also deaths not traditionally considered to be related to pregnancy such as accidents, homicide, and suicide. Pregnancy associated death also includes deaths occurring 43–365 days following termination of pregnancy. Because cause-of-death information on death certificates cannot identify deaths from non-maternal causes or deaths occurring 43 or more days following termination of pregnancy as associated with pregnancy, additional sources of data must be used for complete assessment of all pregnancy-associated deaths (Horon and Cheng 2001). Even with pregnancy-associated deaths there is considerable differentiation between states as to case definition and comparability to CDC estimates of pregnancy associated maternal mortality ratios (Mascola et al. 2004; Horon 2005).
Yet another way of examining abortion related mortality is calculating a national case-fatality rate: the number of known legal induced abortion-related deaths per 100,000 reported legal induced abortions. This would assume that all abortion deaths are identified from direct and indirect causes, as well as immediate and delayed causes up to 1 year after termination of pregnancy. Even if this were possible, which it is not at this time, this rate could not be calculated because a substantial number of abortions occur in non-reporting states. Thus, the denominator (total number of abortions in the United States) is unknown.
The above definitions indicate that there are only two criteria used in indentifying maternal deaths: (1) medical causes of death and (2) timing of pregnancy-related death. By excluding all other categories that are not due to physical complications, other deaths are simply not captured, including suicide and other indirect deaths which result from physical, psychological, interpersonal, or behavioral problems linked to abortion as the marker event. Causes of deaths resulting directly from abortion are identified. However, abortion may also worsen or initiate physical, psychological, interpersonal, and maladaptive behavioral pathways which can lead to diminished mental or physical health and eventuate in death. These cumulative risk factors which can substantially contribute to abortion mortality are identified. Research by Gissler et al. (2005), Reardon et al. (2004a), Christiansen et al. (2006), and Kavanaugh et al. (2009) support such a broadened assessment of pregnancy associated deaths. The impact of substance abuse, depression, anxiety, and suicide resulting from abortion is considerable. As a result, indirect abortion-associated deaths are likely to be many times higher than those deaths directly caused by obstetric complications.
Measurement issues of maternal mortality are problematic
The computation of maternal mortality is most commonly a ratio of the number of maternal deaths during a given period per 100,000 live births during the same period. But other measures are also in use: maternal mortality rate (number of maternal deaths in a given period per 100,000 women of reproductive age during the same time period) and lifetime risk of maternal death (risk of death once a woman has become pregnant). The difficulty and complexity of measuring maternal mortality are evident in the following areas:
-
a.
There are gross difficulties inherent in measuring maternal mortality and definitions regarding precisely what constitutes a death due to pregnancy/birth are evolving.
-
b.
There is a lack of consensus regarding how long after pregnancy resolution a death is appropriately linked with the pregnancy.
-
c.
The two national sources of abortion statistics (CDC and the Guttmacher Institute) are plagued by significant levels of underreporting. Further, discrepancies exist between the two national sources, a minimum 12 percent discrepancy was reported (Strauss et al. 2007).
-
d.
For various reasons (incomplete medical records, lack of fetal death records), deaths due to abortion are often not recorded as resulting from the procedure, with only the immediate cause of death (e.g., embolism, sepsis, and hemorrhage) provided.
-
e.
Women, who experience serious, life-threatening health complications as a result of abortion usually go to a hospital emergency room and are not seen by their abortion providers. Their deaths will therefore not be counted.
-
f.
Abortion-related deaths (from physical complications of the procedure) are reported as maternal deaths.
-
g.
The death statistics tabulated for abortion focus on “uncomplicated abortion”; whereas the statistics for childbirth incorporate complicated delivery (e.g., caesarian delivery). If “uncomplicated delivery” is compared to “uncomplicated abortion,” the risk of dying from abortion is twice as high. Maternal mortality caused by abortion is twice as high compared to women with vaginal deliveries, when caesarean deliveries are excluded (Lanska et al. 1983). Further, analyses do not control for co-morbidities in relation to abortion and pregnancy.
-
h.
The available statistics do not address long-term and less direct causes of death associated with abortion and childbirth. Over time the risk of death associated with abortion increases due to enhanced likelihood of substance abuse, cancer, future pregnancy complications, and suicide ideation, whereas with the risk of dying from these causes are lessened dramatically after completion of a term pregnancy without abortion.
The contemporary definition of pregnancy-related deaths that restricts inclusion of a maternal death to within 42 days of delivery is likely to capture the majority of deaths associated with a full-term pregnancy (see Figure 1 adopted from Chang et al. 2003). However, many of the most serious health risks associated with abortion noted above are more insidious and occur over a much less compressed time period.
Figure 1.
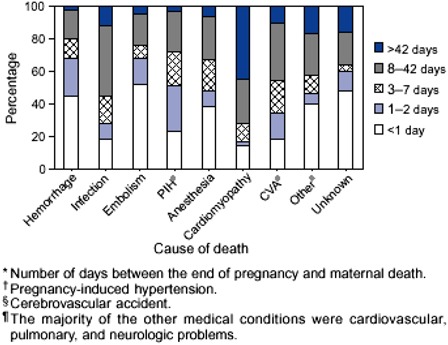
Distribution of pregnancy-related deaths, by cause of death and time interval—United States, 1991–1999.
National data compare deaths associated with term pregnancies to deaths associated with abortion at any point in pregnancy. This is a flawed technique that has produced an over-estimation of maternal mortality and an under-estimation of abortion mortality. The two central issues are detailed below:
-
a.
Maternal mortality is determined by dividing maternal deaths by live births as opposed to pregnancies. Deaths due to ectopic pregnancies (the leading cause of death in the first trimester), molar pregnancies, miscarriage, and stillbirth are represented in the numerator, but not in the denominator. According to the CDC only 60 percent of pregnancy-related deaths occur in conjunction with a live birth. This means that 40 percent of the deaths are never represented in the denominator, resulting in a dramatically over-inflated maternal mortality rate. Moreover, the majority of women who survive ectopic pregnancies, molar pregnancies, miscarriage, and stillbirth will not be in the data at all since their pregnancies do not result in live births.
-
b.
Maternal mortality and abortion mortality statistics are not analogous because maternal mortality statistics do not take into consideration the stage of gestation, whereas abortion mortality statistics are predominantly based on first trimester losses. Appropriate comparisons would be prospective in nature with same gestational point comparisons related to the risk of death associated with the two reproductive outcomes. Existing statistics compare maternal deaths at any point in pregnancy and the post-partum period to abortion deaths, which primarily occur in the second and third months of pregnancy since most abortions are in the first trimester. Bartlett et al. (2004) examined national U.S. data from 1988 to 1997 and found: the relative risk of abortion-related mortality increased dramatically with gestational age of the procedure increasing from 14.7/100,000 procedures at 13–15 weeks gestation, to 29.5/100,000 procedures at 16–20 weeks gestation, and to an astounding 76.6/100,000 procedures at/or after 21 weeks gestation.
Comparisons conducted with no regard for the gestational stage in which the death occurs are flawed for several reasons:
-
a.
Deaths occurring during the first 6 weeks of pregnancy (when maternal morbidity and mortality are highest) are classified as maternal deaths and are lumped together with deaths associated with birth and delivery. This is inappropriate in that the intended outcome of these early pregnancies is unknown.
-
b.
Women who reach the common point of awareness that they are pregnant and make the decision to abort (2 weeks late on the menstrual period or 6 weeks pregnant) have already survived beyond the period of the pregnancy's greatest risk.
-
c.
Abortions do not typically occur very early and are impossible beyond 9 months of gestation when most maternal deaths comprising the maternal mortality statistics occur. Therefore, valid gestational period comparisons can only logically be made in the latter half of the first trimester through the end of the third trimester. During the second and third trimesters, abortion-related mortality is equal to and then exceeds that of childbirth (Bartlett et al. 2004).
Gestational period comparisons would only be valid with sophisticated controls for a variety of socio-demographic factors (age, income, education, marital status) based on sound evidence that women belonging to particular socio-demographic groups (e.g., very young and older women) are more at risk for adverse pregnancy events occurring during pregnancy and the post-partum period.
As indicated earlier in this report, maternal mortality and morbidity are largely based on incomplete data and estimates. In the case of WHO and maternal mortality, definitional issues together with rampant statistical manipulation generate even more inaccurate estimates. In an attempt to identify abortion-related mortality, WHO researchers advocated combining the incidence of spontaneous and induced abortion together, and then correcting for the incidence of spontaneous abortion. According to Harrison (2009), one of the WHO researchers acknowledged: “We make huge adjustments to make the numbers turn out right. More than fifty percent of some numbers are ‘adjusted’ ” (Harrison 2009, 4).
There are powerful financial, socio-political, and interpersonal forces potentially driving the concealment of abortion-related deaths. The same facilities that report the data run the risk of being more closely scrutinized or even closed if there are deaths at their facilities. Deaths associated with abortion are likely to become highly publicized and could result in legal restrictions. Finally, abortion-related deaths may be concealed, because the family is unaware there was a termination or if the family is privy to the information there is likely to be a strong motivation to hide it in order to protect the family from further grief or shame.
Abortion Mortality Compared to Childbirth: Rresearch Evidence
According to Kaunitz (1985), induced abortion is the fifth leading cause of maternal mortality in the U.S. Even so, this finding is likely to be an underestimation as most abortion-related deaths are either not reported, or not captured in the existing definitions and national data collection from state health departments. Other deaths resulting from abortion remain excluded: suicide, avoidable deaths due to injuries, accidents, substance abuse, and cumulative and contributory disease states.
A number of factors enter into the relative risks of dying from abortion compared to childbirth, in addition to the methodological issues identified above. These include patient age, operator skill and experience, race, gestational age, type of procedure employed, pre-existing physical and mental health, etc.
In a growing body of literature, childbirth is protective against death from non-obstetric causes, including breast cancer and suicide in both the immediate and long term (Gissler et al. 1996, 2005; Marzuk et al. 1997; Thorp et al. 2003; Carroll 2007). In a large, health record-linked U.S. study spanning 8 years, women who aborted compared to those who delivered, were 62 percent more likely to die from any cause. Suicide carried a 154 percent increased risk (Reardon et al. 2002). In Finland, using a comprehensive health data linkage system, Gissler et al. (1997) examined death rates up to 1 year after abortion and found a 4 times higher risk among women who aborted versus those who carried to term. Similar adverse findings were reported in subsequent studies: mortality was lower after a birth (28.2/100,000) than after an induced abortion (83.1/100,000)—a 3 times higher mortality risk for abortion compared to childbirth (Gissler et al. 2004b); abortion was associated with a 6 times higher risk for suicide compared to birth (Gissler et al. 2005). Without such record-linkage, 73 percent of all pregnancy-associated deaths would have been missed if they were based only upon death certificates. The percentage of deaths due to abortion would have been even higher (Gissler et al. 2004a). In the U.K., Morgan et al. (1997) reported a similar increased risk of suicide for women electing abortion versus delivery: 8.1 suicide attempts per thousand among those who had abortions compared to only 1.9 suicide attempts per thousand among those who had given birth. Both Hoyer and Lund (1993) and Appleby (1991) found childbirth overall to be risk protective against suicide.
Most striking are the findings by Gissler et al. (2005) that the age group from 15 to 24 years is significantly prone to suicide in the context of an abortion with an increase of almost 50 percent in the suicide rate compared to non-pregnant women (Christiansen et al. 2006). For U.S. women aged 15–19 years, suicide is the third leading cause of death corresponding to 7.5 percent of deaths.
According to Chang et al. (2003), the literature commonly reports three main causes of abortion-related death: infection (33.9%), hemorrhage (21.8%), and embolism (13.9%); additional abortion-related causes of death include ectopic pregnancy, perforation or rupture of the uterus, and anesthesia complications among others. Hemorrhage and infection deaths from abortion are nearly 8 times and 9 times greater when compared to the percentage of maternal deaths attributed to these causes in live-birth.
Gissler et al. (2004a) compared the pregnancy-associated mortality ratio for the different pregnancy outcomes (live births and stillbirths, spontaneous abortions and ectopic pregnancies, and induced abortions) for all childbearing Finnish women. They reported: “The pregnancy associated mortality ratio per 100,000 pregnancies increased only slightly for live births and stillbirths, but became sevenfold for spontaneous abortions and ectopic pregnancies, and 5.5-fold for induced abortions. The outcome-specific denominator also revealed that the crude risk of a pregnancy-associated death was more than twice as high after a spontaneous abortion or an ectopic pregnancy and more than three times as high after an induced abortion than after a live birth or stillbirth” (Gissler et al. 2004a, 453). Pregnancy-associated deaths have usually been calculated using the number of live births as the denominator. Gissler et al. (2004a) demonstrated that calculating pregnancy-associated deaths per 100,000 pregnancies with a specific pregnancy outcome gives a very different and improved picture (Gissler et al. 2004a).
Reardon et al. (2004b) estimated that there were between 2,132 and 7,036 excess deaths per year among women who abort and 766 to 4,021 deaths due to violent causes. These researchers further reported that abortion-related increases in smoking are likely to result in 3,740 more lung cancer deaths in the lifetimes of the 1.4 million women who abort each year in the U.S. (Reardon et al. 2004b). Available evidence points to numerous unexamined pathways where abortion can increase a woman's chance of dying from either direct and immediate complications or after prolonged exposure to adverse disease and dysfunctional coping in the future.
The true number of deaths related to pregnancy might increase from 30 to 150 percent with active surveillance (Chang et al. 2003; Deneux-Tharaux et al. 2005). Until more robust research is undertaken accounting for multiple confounders in national prospective studies, statements about abortion being many times safer than childbirth are unreliable and false. Existing research does not support this allegedly factual assertion. A reasonable patient would want to be informed of the risks of death related to abortion from all causes.
Abortion Mortality: Most Recent Research Evidence
In a carefully done study using 42 years of United Kingdom National Health data comparing England, Wales, and Scotland with Northern Ireland and parallel national data from the Republic of Ireland found that countries with legal abortion actually had a higher maternal mortality rate per 100,000 live births (Ireland's Gain 2011). In fact, Carroll's maternal mortality rates of 8/100,000 and 10/100,000 live births in England, Wales, and Scotland are eerily familiar to the maternal mortality rate of 8.8/100,000 quoted for the U.S. in Raymond and Grimes (2012). The Raymond and Grimes (2012) mortality rate of 0.6/100,000 for abortion is simply not supported by good data (i.e., real data from a national database not estimates) and the present literature. In fact such assertions about abortion mortality seem to represent a biased misuse of statistics and maternal mortality calculations.
Koch et al. (2012a, b) demonstrated in their study of Mexico and abortion the problem of significant overestimation of maternal mortality when not utilizing actual data from a national database (Coleman et al. 2012). Koch et al. (2012a, b) accessed the national database to compare the Federal District of Mexico (Mexico City) with the remainder of Mexico and found a 10-fold overestimation of abortion mortality in the Federal District of Mexico. Previously, maternal mortality in Mexico had been thought to be linked to lack of access to legal abortion. However, maternal deaths fell 30 percent in Mexico in spite of the lack of access to legal abortion. Koch et al. (2012a, b) noted that abortion legalization in the Federal District of Mexico did nothing to lower maternal mortality in the Federal District of Mexico City. In fact, the maternal mortality ratio of maternal deaths compared to abortion deaths per 100,000 live-births decreased from 1.48 to 1.14 in Mexico during the interval from 2007 to 2012 (Koch et al. 2012a, b). Koch's conclusion was that maternal health in Mexico would be better served with better access to emergency and specialized obstetrical care not abortion (Koch et al. 2012a, b).
Coleman et al. (2012) review mortality rates in Denmark's linked data base for the 25-year interval from 1962 to 1993, which included over 1 million women with complete reproductive outcomes including abortions, live births, and spontaneous miscarriages. They found that the risk of death was 6 times greater among women who had never been pregnant compared to women who delivered. There was increased risk of death was 45, 114, and 191 percent for 1, 2, and 3 abortions, respectively, compared to women who had ever given birth during the same time period (Coleman et al. 2012). Maternal death rates compared to abortions were reduced by 108 percent for 2 births and reduced by 63 percent for 3 or more births (Coleman et al. 2012). This significant study with linked, database data overturns previous assertions based on limited and incomplete data demonstrating increased death rates with abortion compared to live births. Further, it shows the dose-related effects of multiple abortions on increasing maternal death rates compared to giving birth.
Abortion laws have been liberalized in countries where there have been large numbers of deaths attributable to clandestine abortions. Those who favor liberalizing abortion laws assume that the health of women is better served by providing abortion. Koch et al. (2012a, b) challenged this assertion recently in their paper covering 50 years of maternal deaths in Chile. Koch et al. (2012a, b) found by utilizing national birth registry statistics over two separate epochs: one with legal abortion covering 1957–1988 and one with prohibition of abortion covering 1989–2007. They found by careful analysis that the legal status of abortion had no relationship to the reduction in maternal mortality. Rather, the reduction in maternal deaths during pregnancy was related to the better education and obstetrical care for women available in the different time periods (Koch et al. 2012a, b).
Certainly critically important issue of maternal mortality in women's health requires the use of accurate data that is only available with the collection of data at a national level in a comprehensive national health database that includes all of women's reproductive outcomes linked to abortion and all other health variables. Such a database must also provide open access to all researchers to evaluate this critical women's health issue. We urge the establishment and financial support of a national healthcare database for the United States with the inclusion of all reproductive outcome variables and associations: including elective abortions.
Endnote
See, for example, the Guttmacher Institute's critique of CDC incidence data: “The estimates presented in this report are subject to some limitations and should be considered provisional. First, not all states are included; the estimates assume that changes in abortion incidence in the excluded states are similar to the overall trend seen in the reporting states. Second, the completeness of abortion reporting to state health departments can vary from year to year. We attempted to exclude all states that had inconsistent reporting, but if (for example) reporting improved in some states we included, it would mean that earlier state reports were too low and that the percentage decline we calculated was too small. In such cases, our new estimates of the number of abortions would be too high” (Finer and Henshaw 2006, 3).
References
- Appleby L. 1991. Suicide after pregnancy and the first postnatal year. British Medical Journal 302: 137–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett L.A., Berg C.J., Shulman H.B., Zane S.B., Green C.A., Whitehead S., Atrash H.K. 2004. Risk factors for legal induced abortion-related mortality in the United States. Obstetrics & Gynecology 103: 729–37 [DOI] [PubMed] [Google Scholar]
- Carroll P.S. 2007. The breast cancer epidemic: modeling and forecasts based on abortion and other risk factors. Journal of American Physicians and Surgeons 12(3): 72–8. [Google Scholar]
- Chang J., Elam-Evans L.D., Berg C.J., Herndon J., Flowers L., Seed K.A., Syverson C.J. 2003. Pregnancy-related mortality surveillance-United States, 1991–1999. MMWR 52: 1–8. [PubMed] [Google Scholar]
- Christiansen L.R., Collins K.A. 2006. Pregnancy-associated deaths: A 15-year retrospective study and overall review of maternal pathophysiology. American Journal of Forensic Medicine and Pathology 27: 11–9. [DOI] [PubMed] [Google Scholar]
- Coleman P.K., Reardon D.C., Calhoun B.C. 2012. Reproductive history patterns and long-term mortality rates: A Danish, population-based record linkage study. European Journal of Public Health 1–6 doi:10.1093/eurpub/cks107http://eurpub.oxfordjournal.org. [DOI] [PubMed] [Google Scholar]
- Deneux-Tharaux C., Berg C., Bouvier-Colle M.H., Gissler M., Harper M., Nannini A., Alexander S., Wildman K., Breart G., Buekens P. 2005. Underreporting of pregnancy-related mortality in the U.S. and Europe. Obstetrics & Gynecology 106: 684–92. [DOI] [PubMed] [Google Scholar]
- Elam-Evans L.D., Strauss L.T., Herndon J., Parker W.Y., Bowens S.V., Zane S., Berg C.J. 2003. Abortion surveillance-United States, 2000. Atlanta, GA: Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Finer L., Henshaw S. 2006. Estimates of U.S. abortion incidence, 2001–2003. Guttmacher Institute, August 3, 1–3. http://www.guttmacher.org/pubs/2006/08/03/ab_incidence.pdf.
- Gissler M., Berg C., Bouvier-Colle M., Buekins P. 2004. a. Methods for identifying pregnancy-associated deaths: Population-based data from Finland 1987–2000. Paediatric & Perinatal Epidemiology 18: 448–55. [DOI] [PubMed] [Google Scholar]
- Gissler M., Berg C., Bouvier-Colle M., Buekins P. 2004. b. Pregnancy-associated mortality after birth, spontaneous abortion, or induced abortion in Finland, 1987–2000. American Journal of Obstetrics and Gynecology 190: 422–7. [DOI] [PubMed] [Google Scholar]
- Gissler M., Hemminki E., Lonnqvist J. 1996. Suicides after pregnancy in Finland, 1987–94: Register linkage study. British Medical Journal 313: 1431–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gissler M., Kauppila R., Merilainen J., Toukomaa H., Hemminki E. 1997. Pregnancy associated deaths in Finland 1987–1994: Definition problems and benefits of record linkage. Acta Obstetricia et Gynecologica Scandinavica 76: 651–7. [DOI] [PubMed] [Google Scholar]
- Gissler M., Berg C., Bouvier-Colle M.H., Buekens P. 2005. Injury deaths, suicides and homicides associated with pregnancy, Finland 1987–2000. European Journal of Public Health 15: 459–63. [DOI] [PubMed] [Google Scholar]
- Grimes D. 2006. Estimation of pregnancy-related mortality risk by pregnancy outcome, United States, 1991–1999. American Journal of Obstetrics and Gynecology 194: 92–3. [DOI] [PubMed] [Google Scholar]
- Guttmacher Institute. 2009. Abortion reporting requirements. State Policies in Brief 12 September 1, http://www.guttmacher.org/statecenter/spibs/spib_OAL.pdf.
- Harrison D. 2009. Removing the roadblocks from achieving MDG 5 by improving the data on maternal mortality. Briefing paper No. 5, New York: International Organizations Research Group. [Google Scholar]
- Horon I. 2005. Underreoporting of maternal deaths on death certificates and the magnitude of the problem of maternal mortality. American Journal of Public Health 95: 479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horon I.L., Cheng D. 2001. Enhanced surveillance for pregnancy-associated mortality: Maryland, 1993–1998. JAMA 285: 1455–9. [DOI] [PubMed] [Google Scholar]
- Hoyer G., Lund E. 1993. Suicide among women related to number of children in marriage. Archives of General Psychiatry 50: 134–7. [DOI] [PubMed] [Google Scholar]
- Hoyert D. 2007. Maternal mortality and related concepts. National Center for Health Statistics. Vital Health Statistics 3(33): 1–20. [PubMed] [Google Scholar]
- Ireland's Gain. 2011. The demographic impact and consequences for the health of women of the abortion laws in the Republic of Ireland and Northern Ireland since 1968 London: PAPRI. [Google Scholar]
- Jones R.K., Kost K. 2007. Underreporting of induced and spontaneous abortion in the United States: An analysis of the 2002 National Survey of Family Growth. Studies in Family Planning 38: 187–97. [DOI] [PubMed] [Google Scholar]
- Jones R.K., Zolna M.R.S., Henshaw S.K., Finer L.B. 2008. Abortion in the United States: Incidence and access to services, 2005. Perspectives on Sexual and Reproductive Health 40(1): 6–16. [DOI] [PubMed] [Google Scholar]
- Kaunitz A.M. 1985. Causes of maternal mortality in the United States. Obstetrics and Gynecology 65: 605–12. [PubMed] [Google Scholar]
- Kavanaugh V., Fierro M.F., Suttle D.E., Heyl P.S., Bendheim S.H., Powell V. 2009. Psychosocial risk factors as contributors to pregnancy-associated death in Virginia, 1999–2001. Journal of Women's Health 18: 1041–8. [DOI] [PubMed] [Google Scholar]
- Koch E., Aracena P., Gatica S., Bravo M., Huerta-Zepeda A., Calhoun B.C. 2012. a. Fundamental discrepancies in abortion estimates and abortion-related mortality: A reevaluation of recent studies in Mexico with special reference to the International Classification of Diseases. International Journal of Women's Health 4: 613–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch E., Thorp J., Bravo M., Gatica S., Romero C.X., Aguilera H., Ahlers I. 2012. b. Women's educational level, maternal health facilities, abortion legislation, and maternal deaths: A natural experiment in Chile from 1957–2007. PLoSONE 7(5): 1–16, e36613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanska J., Lanska A., Rimm A. 1983. Mortality from abortion & childbirth. Journal of the American Medical Association 250: 361, Cited in P. Cunningham & C. Forsythe, Is abortion the “First Right” for women?: Some consequences of legal abortion. In Butler, J. and Walbert, D. 1992. Abortion, Medicine & the Law. New York. [Google Scholar]
- MacKay A., Berg C.J., Duran C., Chang J., Rosenberg H. 2005. An assessment of pregnancy-related mortality in the U.S. Pediatric & Perinatal Epidemiology 19: 206–14. [DOI] [PubMed] [Google Scholar]
- Marzuk P.M., Tardiff K., Leon A.C. 1997. Lower risk of suicide during pregnancy. American Journal of Psychiatry 154: 122–3. [DOI] [PubMed] [Google Scholar]
- Mascola M., Schellpfeffer M.S., Kruse T.K., Conway A.E., Kvale K.M., Katcher M.L. 2004. Pregnancy-associated deaths and pregnancy-related deaths in Wisconsin, 1998–2001. Wisconsin Medical Journal 103: 61–6. [PubMed] [Google Scholar]
- Morgan C., Evans M., Peters J.R. 1997. Suicides after pregnancy: Mental health may deteriorate as a direct effect of induced abortion. British Medical Journal 314: 902. [PMC free article] [PubMed] [Google Scholar]
- Picker Institute. 1999. From the patient's perspective – quality of abortion care. Boston, MA. [Google Scholar]
- Raymond E.G., Grimes D.A. 2012. The comparative safety of legal induced abortion and childbirth in the United States. Obstetrics & Gynecology 119: 215–9. [DOI] [PubMed] [Google Scholar]
- Reardon D.C., Coleman P.K., Cougle J. 2004. a. Substance use associated with prior history of abortion and unintended birth: A national cross sectional cohort study. American Journal of Drug and Alcohol Abuse 26: 369–83. [DOI] [PubMed] [Google Scholar]
- Reardon D.C., Cougle J., Ney P.G., Scheuren F., Coleman P.K., Strahan T. 2002. Deaths associated with delivery and abortion among California Medicaid patients: A record linkage study. Southern Medical Journal 95: 834–41. [PubMed] [Google Scholar]
- Reardon D.C., Strahan T.W., Thorp J.M., Shuping M.W. 2004. b. Deaths associated with abortion compared to childbirth: A review of new and old data and the medical and legal implications. The Journal of Contemporary Health Law and Policy 20: 279–327. [PubMed] [Google Scholar]
- Saul R. 1998. Abortion reporting in the United States. Family Planning Perspective 30: 244–7. [PubMed] [Google Scholar]
- Sonfield A. 2005. The uses and abuses of science in sexual and reproductive health policy debates. Guttmacher Report, November, 1–3.
- Strauss L., Gamble S., Parker W., Cook D., Zane S., Hamdan S. 2007. Abortion surveillance–United States, 2004. Centers for Disease Control and Prevention. MMWR Surveillance Summary 56(9): 1–33. Division of Reproductive Health. [PubMed] [Google Scholar]
- Thorp J., Hartmann K., Shadigan E. 2003. Long-term physical and psychological health consequences of induced abortion: Review of the evidence. Obstetrical and Gynecological Survey 58: 67–79. [DOI] [PubMed] [Google Scholar]
- Wilcox L., Marks J. 1995. From data to action. CDC's Public Health Surveillance for Women, Infants and Children. US Department of Health and Human Services. Public Health Service, Centers for Disease Control and Prevention, National Center for Health Statistics, Hyattsville, MD, May, 1996. 1–118. [Google Scholar]
- World Health Organization. 2004. Maternal mortality in 2000-estimates by UNICEF, WHO, & UNFPA. Geneva, Switzerland: Department of Reproductive Health & Research, WHO. [Google Scholar]
- World Health Organization. 2007. Maternal mortality in 2005 – estimates developed by WHO, UNICEF, UNFPA, and The World Bank.


