Abstract
The current approach to infertility of assisted reproductive technology (ART) completely misses and then bypasses the evaluation and treatment of cervical factor infertility. In contrast, the Creighton Model Fertility Care System (CrMS), a method of fertility awareness that has the unique ability to quantify cervical mucus observations, and natural procreative technology (NaProTECHNOLOGY or NPT) directly evaluate and treat cervical factor infertility. The ART treatment of choice for cervical factor infertility–-intrauterine insemination (IUI)–-is also morally disparate from the NPT treatment protocol: while the latter genuinely assists the infertile couple's act of sexual union to achieve its natural end of pregnancy, IUI replaces the natural act, depriving human conception of the one context worthy of the dignity of human life and procreation, a reciprocal self-gifting act of love between husband and wife. A renewed interest and focus on the direct evaluation and treatment of cervical factor infertility is needed.
Introduction
The respective protocols of NaProTECHNOLOGY (natural procreative technology or NPT) and assisted reproductive technology (ART) for the treatment of cervical factor infertility are clinically distinct. In part I, we compare and contrast these two approaches in reference to an actual clinical case; and in part II, we evaluate the moral dynamic of each of these reproductive technologies when judged against natural law norms that are confirmed and enriched by faith.
I. The NaProTECHNOLOGY and Assisted Reproductive Technology Approaches to Cervical Factor Infertility
Case
A twenty-nine-year-old, Gravida zero woman presents with complaints of inability to conceive a pregnancy after five years of unprotected intercourse. For six months, she charted her cycles using the Creighton Model FertilityCare System (CrMS) and used fertility-focused intercourse to achieve a pregnancy. On review of her charts, her cycles were categorized as limited mucus cycles with an average score of 4.5, which normalized to a score of 8 with mucus enhancers (regular mucus cycle score 7.6–16 and limited mucus cycle score 0.1–7.5).
Background
The causes of infertility are traditionally categorized according to several categories or factors. These are male, ovarian, cervical, uterine, tubal, peritoneal, and unexplained.1 Cervical mucus is a necessary component of human fertility and plays at least two critically important physiologic roles in fertility. First, cervical mucus is essential to sperm survival and transport. The duration of the fertile window is six days in couples of normal fertility: the five days that the sperm can survive in fertile-type mucus plus the day of ovulation. Without fertile mucus sperm would last only hours in the vagina with little chance of meeting and fertilizing the egg (ovum).2 Second, cervical mucus has been described as a “biological valve,” admitting sperm to the uterus at certain times of the cycle while inhibiting their entrance at other times. During the preovulatory phase of the cycle and under the influence of estrogen, cervical mucus (when viewed under a microscope) forms parallel channels that allow sperm to traverse the cervix and then to swim up to the fallopian tubes: the biological valve–-cervical mucus–-is literally “open.” In the postovulatory phase and under the influence of progesterone, cervical mucus is thick (with a “cobblestone” appearance under the microscope) and blocks the passage of sperm into the uterus: the biological valve of cervical mucus is “closed.”3
Diagnosis
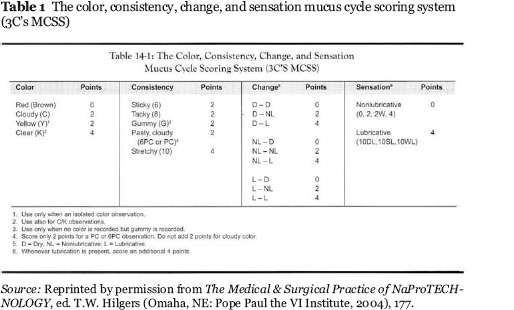
With the CrMS, a woman tracks her ovulatory and menstrual cycles by means of a standardized recording system of her cervical mucus observations. CrMS addresses the diagnosis of cervical factor infertility in a very unique way, by standardizing and classifying mucus observations. Other methods of fertility awareness simply detect the presence or absence of cervical mucus, or allow it to be described in a subjective, nonstandardized way. The CrMS is standardized in the way it is taught and in the way the mucus observations are made in a quantifiable and reproducible manner.4 The mucus cycle score is calculated from the standardized CrMS vaginal discharge recording system (VDRS), based on the stretch, color, and sensation of the mucus (see table 1).5 This recording system is converted to a daily numerical score ranging from zero to sixteen. An average of the daily score from the peak day and the five days preceding the peak day yields a summary mucus cycle score for each menstrual cycle. Cycle scores have been categorized in the following: 1) dry cycles, with a score of 0; 2) limited mucus cycles, with scores ranging from 0.1 to 7.5; and 3) regular mucus cycles, with scores above 7.6.6 A study by J.B. Stanford, J.R. Smith, and D.B. Dunson evaluated 1,681 menstrual cycles charted with the CrMS and demonstrated a positive correlation of the mucus score categories to pregnancy probability.7 The CrMS allows providers a unique way not only to diagnose cervical factor infertility, but also to effectively follow and monitor treatments. The patient in our case charted her cycles with the CrMS, was diagnosed with limited mucus cycles, and was treated according to NPT protocols (see “Treatment” section below).
Table 1.
The color, consistency, change, and sensation mucus cycle scoring system (3C's MCSS)
An ART infertility evaluation of this patient would be unable to identify the woman's limited mucus cycles, since it lacks the means to evaluate or measure cervical mucus. Until recently, the recommended ART method for diagnosing cervical factor infertility was the postcoital test8: the post-intercourse collection of mucus shortly before the time of ovulation and a few to several hours after intercourse. The mucus specimen is evaluated for pH, clarity, cellularity, viscosity (the length to which a column of mucus can be stretched in centimeters also known as spinnbarkeit), salinity (evaluated according to the number of channels formed by the crystallization of the mucus when dried on a glass slide also know as “ferning”), and the number and motility of surviving sperm. Abnormal test results were common due to poor timing. This is directly due to the fact that standard ART evaluation of infertility lacks a simple, accurate way of timing tests. It is recommended that the postcoital test be performed two days before the luteinizing hormone (LH) surge, and while LH predictor kits are available, they are also costly and do not allow for a proper prospective determination of the timing for the test. Transvaginal ultrasound can also be used to identify a mature follicle, but it, too, is time-intensive and costly. The CrMS, in contrast, is a simple, reliable, and cost-effective method of identifying the fertile window and impending ovulation through the woman's standardized observations of fertile mucus.
Given these limitations, the postcoital test for the diagnosis of cervical factor is no longer recommended by ART experts.9 While M.A. Fritz and L. Speroff gives several reasons, the most definitive is this: “The postcoital test results seldom change clinical management, because contemporary treatments for unexplained infertility include IUI (usually with ovarian stimulation) or IVF, both of which negate any contributing cervical factor.” In short, the ART approach to infertility is not to assess the patient for cervical factor but to circumvent evaluation and to proceed directly to treatment with IUI or IVF. In direct contrast, the CrMS is a simple, standardized way to evaluate and monitor treatment for cervical factor infertility.
Treatment
In our case scenario, the patient's limited mucus cycles were treated with an NPT protocol. To improve her cervical mucus, the patient was given vitamin B6 500 mg sustained release taken every day by mouth. After eight weeks on this mucus enhancer, her mucus cycle score went from an average of 4.5 to 8, and her mucus cycle score improved from a limited mucus cycle to a regular mucus cycle score. After two cycles of the cervical mucus enhancer and fertility-focused intercourse, the patient achieved pregnancy.
Mucus enhancer treatments for limited cervical mucus include vitamin B6, guaifenesin, antibiotics such as amoxicillin, and FertileCM.10
Vitamin B6 and antibiotics (during the fertile window) are theorized to enhance the utilization of estrogen at the target organ, the cervix.11 It has been shown that guaifenesin, a respiratory expectorant that increases the volume and decreases viscosity of respiratory tract secretions, has similar effects on cervical mucus.12 It is postulated that FertileCM enhances cervical mucus because it contains L-arginine–-a precursor to nitric oxide–-a molecule responsible for the autonomic cholinergic nervous modulation of cervical mucus secretion.13 Data generated by T. Hilgers shows that mucus enhancers improve mucus cycle scores.14 For example, in a group of eleven patients taking amoxicillin during the fertile window, mucus cycles scores went from an average of 4.0 to an average score of 9 (p = 0.003). In another group of sixteen patients taking vitamin B6 500 mg SR every day, the mucus cycle scores improved from an average of 4.1 to an average of 6.4 after treatment (p = 0.05).
The patient in our case also used fertility-focused intercourse in conjunction with mucus enhancers. But in some infertility cases, fertility-focused intercourse proves to be the only treatment necessary to achieve a pregnancy. A study by Stanford, Smith, and Dunson found that subfertile couples with a three-day fertile window had a 26 percent rate of conception with using fertility-focused intercourse only.15 These results underscore the highly effective way the CrMS 1) identifies the fertile window, and 2) uses fertility-focused intercourse to achieve pregnancy with infertile couples.
The ART treatment for a woman suspected of cervical factor infertility would be intrauterine insemination (IUI) usually with ovulation induction or controlled ovarian hyperstimulation. IUI, with or without ovulation induction or controlled ovarian hyperstimulation, is recommended so that the sperm bypass potentially hostile cervical factors and an enhanced number of them gain access to the uterine cavity, giving rise to a slight increase of pregnancy rates (see “Outcomes” section below).
Outcomes
Dr. Hilgers studied outcomes of patients treated using fertility-focused intercourse alone or fertility-focused intercourse and mucus enhancers.16 Forty patients with limited mucus cycles and an average of 3.2 years of trying to achieve a pregnancy before starting CrMS had a 40 percent pregnancy rate using fertility-focused intercourse only or in conjunction with vitamin B6. The length of time to pregnancy was a mean of 5.4 months. Ten patients with dry cycles who had an average length of trying to achieve pregnancy of 3.6 years before starting CrMS had a 20 percent pregnancy rate over an average period of twelve months.
The ART community has studied IUI in natural cycles. One trial compared expectant management to IUI.17 The trial included 191 couples receiving IUI over six months and compared them to 193 couples managed expectantly. Both groups had an average age of thirty-two years and an average duration of infertility of 2.5 years. The pregnancy rates for each group were 23 percent and 17 percent, respectively. This difference of 6 percent was not found to be significant. Fritz and Speroff, citing this and other studies, conclude, “The best available evidence suggests that treatment with IUI in natural cycles has no clinically important effects.”18
Treatment using IUI with ovulation induction using clomiphene citrate has been studied. A large study of 1,738 infertility patients treated with clomiphene citrate and IUI revealed cumulative pregnancy rates over four cycles of 20.6 percent.19 Another study compared clomiphene citrate and IUI treatment to timed intercourse.20 The infertile participants were an average age of thirty-three and experienced an average time of infertility of 3.5 years. Human chorionic gonadotropin (hCG) was used to trigger ovulation in the treatment group. The couples in the timed intercourse group were instructed to have intercourse during the periovulatory period, based on basal body temperature graphs and/or LH predictor kits. There was a statistically significant difference of fecundities in the treatment group as compared to the control group; the cumulative pregnancy rate in the treatment group was 35 percent over four cycles as compared to 14 percent in the control group. Fritz and Speroff summarize,
In sum, evidence for the effectiveness of combined treatment with clomiphene and IUI is not compelling. However, considering its relatively modest cost and complexity … treatment with clomiphene and IUI seems justified because the cycle fecundability observed in large prospective and retrospective studies is significantly higher than can be expected in couples with unexplained infertility receiving no treatment.21
Treatment using IUI with controlled ovarian hyperstimulation has also been studied. A Dutch study compared IUI with controlled ovarian hyperstimulation to expectant management and found no significant difference in pregnancy outcomes.22 Patients were an average age of thirty-three and had infertility problems for an average time of two years. The pregnancy rate in the couples managed with IUI and controlled ovarian hyperstimulation was 23 percent over six months versus 27 percent in the expectant group. A U.S. trial showed a greater benefit in patients with a longer time of infertility, with a 33 percent pregnancy rate in patients treated with IUI and controlled ovarian hyperstimulation over four cycles.23 Fritz and Speroff conclude,
In summary, treatment with gonadotropins and IUI is modestly effective treatment for couples with longer duration of unexplained fertility (more than three years). Treatment with gonadotropins and IUI is reasonable to consider for couples who fail to conceive during treatment with clomiphene and IUI and when clomiphene treatment fails to stimulate multiple follicular development, especially when IVF is not a viable option.24
While more robust comparative studies and more research are needed, NPT appears to offer a more cost-efficient and more effective treatment over ART (IUI). NPT is a restorative approach, which directly evaluates and treats cervical factor infertility; ART is a circumventive approach that bypasses, and therefore fails to directly treat, the cervical factor.
II. Ethical Analysis of the Respective NPT and ART Approach to Cervical Factor Infertility Moral Norms: Their Source and Scope
The moral norms that help evaluate the morality of the respective ART and NPT treatments for cervical factor infertility have not developed in a vacuum. They follow directly from the Roman Catholic Church's comprehensive vision of the human person, a vision rooted in reason and confirmed, as well as enriched, by faith.25
God's fatherly love, expressed in the Divine acts of Creation and Redemption, is the paradigm of, and therefore the moral measure for, married love.26 God's love is the template; married love is its icon. As the template of love and life, God's creative and redemptive acts of love always manifest their perfection in giving life–-plant life, animal life, human life, angelic life, the life of Jesus, His Holy Spirit, and His Church. From the perspective of the human icon of married love, then, the acts of sexual union between husband and wife ought also to manifest their perfection by being–-just like God's love–-inseparably life-giving.
Accordingly, the first norm to help us evaluate the ethics of infertility treatment requires that: just as God's love indivisibly manifests its perfection in being life-giving, so must married love.
A natural law perspective of a couple's fertile act of love highlights the interconnectivity between its inherent love- and life-giving meanings.27 The procreative meaning–-the couple's ability to generate a new human life from two complementary reproductive cells (one female, one male) through coitus, is indivisibly linked to its unitive meaning–-the capacity of marital sexual love to unite husband and wife into “one flesh.” Love-making and baby-making capacities are not two disparate coins, but the two sides of the single coin of marital sexual love. Love's dimensions are ineluctably coupled, precisely the way married couples experience their fertile acts of sex: one meaning engraved within the other, love-making inextricably linked to baby-making, a procreative act that demands, activates, and defines union, and a unitive act that demands, activates, and defines openness to life. This inextricable linkage explains why, when contemporary reproductive technology effectively sunders the natural connection between sex and procreation–-as contraception and sterilization disassociate sex from pregnancy, and “assisted” reproductive technologies divorce procreation from sex, it is never without demoralizing consequences for the husband, the wife, and their marriage. Just as defacing one side of a rare coin devalues the whole so, too, contraception, sterilization, and IVF, in sundering one meaning of sexual love from the other, erode the integrity of conjugal love and can, over time, attenuate the whole of married love.
Given the nature of marital sexual love and the natural nexus between its inherent meanings, we arrive at the second norm that guides our assessment of infertility treatment: The only context worthy of conceiving a new human being is within the couple's loving acts of sexual union.28
But, you object, what is an infertile or subfertile couple to do when they are unable to achieve a pregnancy within their own intimate acts of love? The answer is seek out a fertility treatment (like the CrMS/NPT approach discussed previously) that facilitates, rather than replaces, the conjugal act; find protocols that diagnose and treat the pathology underlying the infertility so the couple can achieve a pregnancy within their own acts of life-giving sexual union.29
Accordingly, then, the third and “bottom-line” principle deciding the morality of infertility treatment follows logically from the first two: any treatment that assists the couple's act of sex to achieve its natural end of conception is moral, that is, conducive to the couple's fulfillment; any infertility treatment that replaces the couple's conjugal act–-that is, achieves a pregnancy outside an act of their sexual union–-is immoral, that is, antagonistic toward the couple's fulfillment.30
Refection on this third norm from the perspective of the nature and dignity of the child to be conceived evokes a correlate standard: Every child has the right: to be conceived within an act of his parents’ reciprocal self-giving sexual love, to be the “fruit” of a loving act of sexual union between his mother and father.31
Application of Pertinent Moral Norms to the NPT Approach to Cervical Factor Infertility
The diagnostic and treatment aspects of the NPT approach to the couple who presented with cervical factor infertility is morally sound, i.e., whether analyzed step-by-step or taken collectively, the protocol enhanced the couple's physical, psychological, and moral well-being as it aligned their procreative plans with God's plan for responsible parenthood. Putting a fine point on this conclusion, each diagnostic/treatment step assisted the couple's act of intercourse to achieve its natural end: a) After direction from their CrMS practitioner,32 the couple cyclically tracked the quality of cervical mucus, especially its color, consistency, and the presence or absence of lubrication; b) the NPT physician scored (i.e., quantified) the couple's cervical mucus cycle and categorized it as a limited mucus cycle; c) the physician treated the woman's mucus deficiency with vitamin B6, a mucus enhancer, and then scored the mucus cycle again; d) the physician compared the respective baseline score (an average of 4.5) and post-treatment mucus cycle score (an average of 8) and, based on the enhanced post-treatment score, advised the couple to engage in fertility-focused intercourse33; and e) after two cycles of fertility-focused intercourse (and in the presence of enhanced cervical mucus), the couple conceived.
In sum, the aim of the NPT approach in the case showcased here was to diagnose and treat the pathology underlying the infertility–-a cervical mucus deficiency, so as to increase the couple's chances of conceiving their child within their intimate acts of love. Both the intention (the “why” of the NPT treatment) and the moral object of the protocol (what was actually done) respected the principal norms governing the morality of treatment for infertility: a) the treatment unambiguously and directly assisted the couple's act of sex to achieve its natural end; b) the couple achieved a pregnancy within the one context worthy of human conception, a loving act of sexual intercourse where their baby-making arose from within their love-making; c) the child the couple conceived, with the assistance of the treatment, was the fruit of a loving act of sex or, alternately, the child's right to be conceived within and, therefore, to be connected to the protection, security and, yes, intimacy of his parents’ bodily union was respected; and d) the marital love of the couple manifested its perfection, just as God's love does, in being, at once, life-giving.
Application of Pertinent Moral Norms to the ART Approach to Cervical Factor Infertility
Background
As we have seen in part I, the ART treatment approach for couples who present with what could be cervical factor infertility is IUI. The prerequisite for a sound moral evaluation of the procedure–-whether it assists or replaces the act of sex between the couple attempting to achieve a pregnancy–-is a clear grasp of 1) IUI's preparation of the sperm, and 2) the insemination process itself.34
Sperm Processing and Insemination
A semen specimen is collected by the male patient by means of masturbation in the morning and after two to three days of abstinence. Ejaculate is collected into a sterile cup and then prepared prior to insemination: 1) Sperm are separated from prostaglandin-rich prostatic secretions or seminal fluid that can cause uterine cramping in the woman or anaphylaxis when placed directly into the uterine cavity, and 2) sperm specimen is concentrated, that is, the number of sperm are maximized; number of motile sperm are increased, and cellular debris is removed either through a “swim up” process or through gradient density centrifugation.
Intrauterine Insemination Process
The female patient undresses from the waist down and lies on an examination table in dorsal lithotomy position with her feet in stirrups. The processed sperm and its suspension media are aspirated into the syringe, and the syringe is then connected to an insemination catheter. A speculum is inserted into the cervix for adequate visualization, and the catheter is inserted through the cervical os, then the endocervical canal, and into the uterus to a depth of approximately 6 to 6.5 cm. The sperm are injected into the uterus and then the catheter is slowly withdrawn. The patient rests in supine or in the Trendelenburg position for ten minutes after sperm injection
Moral Analysis of Conventional IUI (IUI Performed with Sperm Collected through Masturbation)
Understanding the phases of the process of IUI as it is conventionally performed reveals one important fact: there is no act of intercourse. For that reason, conventional IUI (cIUI) is immoral because it replaces the act of sexual union and, as a result, 1) requires that the male partner collect a semen specimen by means of masturbation (an immoral act subversive of both the unitive and procreative meanings of marital sexual love); thus 2) divorcing the child's conception from the couple's sexual act of union, the only context worthy of the dignity of the conception of a new human being; therefore 3) depriving the child of his right to be the fruit of his parents’ loving act of sexual love; 4) his right to be connected to the protection, security and, yes, intimacy of his parents’ bodily union; 5) failing to imitate God's creative and redemptive acts of love which are, at once, life-giving; and 6) displacing God's cocreative wisdom for human procreation with the technological production of human life.
Moral Analysis of “Modified” IUI (Moral Analysis of IUI Performed with Sperm Collected by a Perforated Seminal Fluid Collection Device during a Natural Act of Intercourse)
Background
Donum vitae includes the following principle within its discussion of the morality of artificial insemination: “If the technical means [insemination using husband's sperm] facilitates the conjugal act or helps it to reach its natural objectives, it can be morally acceptable.”35 This statement prompted theologians trying to understand the document to ask: How could artificial insemination assist the marital act when the technique, conventionally performed, does not involve the infertile couple's act of sex? Since Donum vitae failed to provide an example of insemination techniques that would constitute assistance,36 some of these theologians proposed their own. They reasoned that the insemination process could be moral, if it were modified by the introduction of a precedent act of sex during which the husband wears a perforated condom assuring that some sperm are deposited in the woman's vagina (constituting an integral act of sex) and the rest are collected at the base of the sheath.37 Since 1987, theological evaluation of modified IUI (mIUI) has been divided between those who contend the technique assists the conjugal act to achieve its natural end of pregnancy and those who argue it replaces rather than assists, the couple's act of sexual union. The Church has never definitively approved or disapproved of mIUI nor agreed or disagreed with the respective arguments that claim the technique assists or replaces the conjugal act.
In a case like that of mIUI, where the Church does not provide a definitive moral evaluation and faithful theologians come to diverse moral opinions regarding its morality, the onus of making an informed conscientious decision falls squarely on the shoulders of 1) the infertile couple considering use of the procedure to build their family and/or 2) the fertility specialist contemplating clinical provision of the treatment. Both parties should form their consciences according to the argumentation and moral counsel they think most cogently respect relevant norms that promote human fulfillment as outlined in official Catholic documents.
Some argue that mIUI assists the conjugal act to attain its natural end of pregnancy due to the alleged moral unity or continuity that exists between its various steps38: 1) Use of a perforated condom is a morally acceptable means for semen collection. 2) The sperm collected at the base of the sheath is a part of the integral act of sex since it is a portion of the husband's ejaculate. 3) The conjugal act remains the essential step in fertilization of the egg and sperm, while the technique simply “repositions” the sperm from the sex act into the woman's uterus. 4) The insemination process is separated from the act of intercourse by only a few hours. And 5) if conception occurs, it does so within the woman's body.
The principal weakness of the preceding argument is its circular reasoning: It assumes what it needs to prove. How does the morality of the individual phases of mIUI evince moral unity between those steps? Why do sperm collected at the base of the sheath, rather than deposited in the woman's vagina, count as part of the integral act of sex? How, precisely, does the conjugal act in the context of mIUI maintain its place of primacy?
Moral Analysis
Moral assessment of mIUI must go beyond gross appearances. The nub of the question is whether what happens during the act of intercourse–-the distinction between sperm deposited in the woman's vagina and that collected at the base of the sheath, and what occurs after the act of intercourse: washing and centrifuging the sperm, transferring sperm into the uterus–-constitutes assistance or replacement of the marital act. To speak in philosophical terms: Does mIUI assist the couple's act of sex by virtue of maintaining moral continuity between the act of intercourse and the technological processes? That is, does the capital effect of mIUI guarantee the centrality and integrity of the marital act by ensuring that any child conceived as a result will truly be the fruit of an act of sexual union between his parents, the personal embodiment of his parents’ self-gifting love? Or, does mIUI, by reducing the act of sexual intercourse to a method of sperm collection, replace the sex act so that, rather than the technique assisting the marital act, the marital act assists–-by being a mere subsidiary of–-the reproductive technique?
One way of resolving the critical questions of assistance and moral continuity that has proved helpful for infertile couples or clinicians seeking moral counsel regarding mIUI depends on a Socratic dialogue of sorts. The following exchange summarizes the questions posed (Q) and the typical answers they elicited from the client (C-A):
(Q) Let's say a couple struggling with infertility for at least twelve months conceive after mIUI. Which sperm do you think, in all likelihood, was responsible for the fertilization of the woman's egg: the sperm that was part of the ejaculate that penetrated the woman's body, or the sperm that was part of the semen deposited at the base of the sheath, taken to the lab, made rich, and subsequently injected into the woman's uterus?
(C-A): The sperm that was part of the semen specimen was most likely responsible for fertilizing the woman's egg since it was washed, spun down, and made rich. If it were the sperm deposited in the woman's vagina, the couple would have been pregnant a year or more ago.
(Q) Was the sperm collected at the base of the sheath part of the act of sexual union between the prospective parents?
(C-A): Well, not really, since the collected sperm were not deposited in the woman's vagina.
(Q) Given your answers to the first two questions, can we legitimately conclude, then, that the infertility treatment facilitated the child's conception as the “fruit” of his parents’ loving act of intercourse or honored the child's right to be conceived within his parents’ act of sexual love?
(C-A): Not really, since the sperm that in all probability contributed to the conception of the child was not part of the couple's act of sex.
After working through this exercise, most couples conclude that modified IUI replaces, rather than assists, the act of intercourse. They agree with the assessment that, while there may be material continuity between the technique and the act of sex, there is no formal, and therefore no moral, continuity between the two. Since the reproductive technique of IUI highjacks the center-stage position, it replaces the act of sex by reducing it to the ancillary role of a semen collection method that avoids the evil of masturbation.39
In short, we contend that mIUI is immoral. It replaces the act of sexual love between the couple (reduces the sex act to an ancillary act of sperm collection while, at the same time, enshrining the reproductive technique as the primordial event leading to fertilization) and, in the event of conception, leads to a pregnancy outside the marital act, outside the one context worthy of human conception: the couple's act of self-giving love. Correspondingly, use, or clinical provision, of mIUI deprives the couple, the child, and the clinical provider of full human flourishing.
Conclusion
First, the CrMS/NPT approach to cervical factor infertility, a protocol that is both medically effective and ethically sound, is inherently moral. It respects the dignity of human procreation by allowing parents and providers to cooperate responsibly with the fruitful love of God. Second, IUI (conventional or modified) is an inherently immoral reproductive technique. It profanes the true meaning of human procreation and prevents couples and clinical providers from cooperating responsibly with God's plan for human procreation. Finally, in the interests of promoting reproductive medicine that is medically and morally effective, a renewed interest and focus on the direct evaluation and treatment of cervical factor infertility is needed.
Notes
M.A. Fritz and L. Speroff, Clinical Gynecologic Endocrinology and Infertility (Philadelphia: Lippincott Williams & Wilkins, 2011), 1157.
D.B. Dunson et al., “Day-Specific Probabilities of Clinical Pregnancy Based on Two Studies with Imperfect Measures of Ovulation,” Human Reproduction 14 (1999): 1835–1839; D. Fordney-Settlage, “A Review of Cervical Mucus and Sperm Interactions in Humans,” International Journal of Fertility 26 (1981): 161–169.
T.W. Hilgers and A.M. Prebil, “The Ovulation Method–-Vulvar Observations as an Index of Fertility/Infertility,” Obstetrics & Gynecology 53 (1979): 12–22.
J.B. Stanford, “Fecundity and the Mucus Cycle Score in Couples Using the CrMS,” in The Medical & Surgical Practice of NaProTECHNOLOGY, ed. T.W. Hilgers (Omaha, NE: Pope Paul the VI Institute, 2004), 643.
Hilgers, The Medical & Surgical Practice of NaProTECHNOLOGY, 177.
Ibid., 179.
J.B. Stanford, K.R. Smith, and D.B. Dunson, “Vulvar Mucus Observations and the Probability of Pregnancy,” Obstetrics & Gynecology 101 (2003): 1285–1293.
Fritz and Speroff, Clinical Gynecologic Endocrinology and Infertility, 1168.
Ibid., 1169.
Hilgers, The Medical & Surgical Practice of NaProTECHNOLOGY, 610; Fairhaven Health, “FertileCM: A Dietary Supplement for Women,” http://www.fertilecm.com.
T.W. Hilgers et al., The Creighton Model FertilityCareSystem: A Standardized Case Management Approach to Teaching Book II: Advanced Teaching Skills (Omaha, NE: Pope Paul the VI, 2003), 287; Hilgers, The Medical & Surgical Practice of NaProTECHNOLOGY, 621.
J.H. Check, H.G. Adelson, and W. Chung-Hsiu, “Improvement of Cervical Factor with Guaifenesin,” Fertility and Sterility 37 (1982): 707–708.
B. Morlin and M. Hammarstrom, “Nitric Oxide Increases Cervical Secretion at the Ovulatory Phase in the Female,” Acta Obstetricia et Gynecologica Scandinavica 84 (2005): 883–886; G.I. Gorodeski, “NO Increases Permeability of Cultured Human Cervical Epithelia by cGMP-Mediated Increase in G-actin,” American Journal of Physiology–-Cell Physiology 278 (2000): C942–C952.
Hilgers, The Medical & Surgical Practice of NaProTECHNOLOGY, 621.
Stanford, Smith, and Dunson, “Vulvar Mucus Observations and the Probability of Pregnancy.”
Hilgers, The Medical & Surgical Practice of NaProTECHNOLOGY, 681.
S. Bhattacharya et al., “Clomifene Citrate or Unstimulated Intrauterine Insemination Compared with Expectant Management for Unexplained Infertility: Pragmatic Randomised Controlled Trial,” British Medical Journal 337 (2008): 716.
Fritz and Speroff, Clinical Gynecologic Endocrinology and Infertility, 1187.
S.D. Dovey, R.M. Sneeringer, and A.S. Penzias, “Clomiphene Citrate and Intrauterine Insemination: Analysis of More than 4,100 Cycles,” Fertility and Sterility 90 (2008): 2281–2286.
J.L. Deaton et al., “A Randomized, Controlled Trial of Clomiphene Citrate and Intrauterine Insemination in Couples with Unexplained Infertility or Surgically Corrected Endometriosis,” Fertility and Sterility 54 (1990): 1083–1088.
Fritz and Speroff, Clinical Gynecologic Endocrinology and Infertility, 1188.
P. Steures et al. “Intrauterine Insemination with Controlled Ovarian Hyper-stimulation Versus Expectant Management for Couples with Unexplained Sub-fertility and an Intermediate Prognosis: A Randomized Clinical Trial,” Lancet 368 (2006): 216–221.
D.S. Guzick et al., “Efficacy of Superovulation and Intrauterine Insemination in the Treatment of Infertility,” New England Journal of Medicine 40 (1999): 177–183.
Fritz and Speroff, Clinical Gynecologic Endocrinology and Infertility, 1189.
Pope Paul VI, in Humanae vitae, insists that only a Christian anthropological view of the human person provides an adequate moral compass to investigate the meaning of human procreation, responsible parenthood, and reproductive technologies: “The question of human procreation, like every other question which touches human life, involves more than the limited aspects specific to such disciplines as biology, psychology, demography or sociology. It is the whole man and the whole mission to which he is called that must be considered: both its natural, earthly aspects and its supernatural, eternal aspects” (n. 7: AAS 60 [1968], 488–499). Congregation for the Doctrine of the Faith, Donum vitae, quotes John Paul II's address to the World Medical Association, which underscores the Church anthropological vision when considering the ethics of reproductive interventions: “Each human person in his absolutely unique singularity is constituted not only by his spirit, but by his body as well. Thus, in the body and through the body, one touches the person himself in his concrete reality. To respect the dignity of man consequently amounts to safeguarding this identity of the man corpore et anima unus.” The personal nature of the human being and the specific goods and values of marriage and procreation “determine from the moral point of view the meaning and limits of artificial interventions regarding procreation and the origin of human life.” These interventions are not to be rejected on the grounds that they are artificial… . But they must be given a moral evaluation in reference to the dignity of the human person, who is called to realize his vocation from God to the gift of love and the gift of life” (nn. 3.4 and 3.6: AAS 80 [1988], 74–75). Congregation for the Doctrine of the Faith, Dignitas personae outlines the three fundamental goods of the human person that reproductive technologies must respect “a) the right to life and to physical integrity of every human being from conception to natural death; b) the unity of marriage, which means reciprocal respect for the right within marriage to become a father or mother only together with the other spouse; c) the specifically human values of sexuality,” which require “the procreation of a human person be brought about as the fruit of the conjugal act specific to the love between the spouses” (n. 12: AAS 100.2 [2008], 865). Since the life and physical integrity of the child to be conceived are not threatened by either the NPT or IUI protocols, I omit the first moral norm listed in Dignitas personae–-reproductive technologies must respect “the right to life and physical integrity of the human being from conception to natural death.” However, see Renee Mirkes, “The Ethics of Infertility Treatment” for an analysis of IVF, a reproductive technology whose underlying philosophy “simply tortures logic beyond all comprehension. Prior to any fertilization in the laboratory, the IVF specialist arrogates to himself the right to instruct the couple which of their embryos will be transferred, which will be surrealistically suspended through cryopreservation, which will be donated to destructive embryonic research, and which will be discarded because of developmental abnormalities. Keep in mind that all of this anti-life violence is directed toward embryos who fall outside the most popular justification for abortion, namely, ‘unwanted’ babies resulting from so-called unplanned pregnancies.” (in Live the Truth, Proceedings of the Twentieth Workshop for Bishops, ed. Edward J. Furton [Philadelphia: National Conference of Catholic Bishops, 2006], 203–231.)
Paul VI, Humanae vitae, n. 8.1: “Married love particularly reveals its true nature and nobility when we realize that it takes its origin from God, who ‘is love,’ (see 1 Jn 4:8) the Father ‘from whom every family in heaven and on earth is named’ (Eph. 3:15).”
Paul VI, Humanae vitae, nn. 12.1, 12.2; Congregation for the Doctrine of the Faith, Donum vitae, II, B, n. 4.1.
Paul VI, Humanae vitae, nn. 9.5, 11; Congregation for the Doctrine of the Faith, Donum vitae, II, B, n. 4; Congregation for the Doctrine of the Faith, Dignitas personae, n. 12.1.
As Congregation for the Doctrine of the Faith, Dignitas personae, states, “Certainly, techniques aimed at removing obstacles to natural fertilization, as for example, hormonal treatments for infertility, surgery for endometriosis, unblocking of fallopian tubes or their surgical repair, are licit. All these techniques may be considered authentic treatment because, once the problem causing the infertility has beenresolved, the married couple is able to engage in conjugal acts resulting in procreation, without the physician's action directly interfering in that act itself” (II, n. 13.1).
Congregation for the Doctrine of the Faith, Donum vitae, II, B, n. 6; Congregation for the Doctrine of the Faith, Dignitas personae, n. 12.2, quoting Congregation for the Doctrine of the Faith, Donum vitae.
Congregation for the Doctrine of the Faith, Donum vitae, II, A, nn. 1.3 and 1.4; idem, Dignitas personae, n. 12.1.
The hub of the woman's health science of NPT is its method of tracking the natural procreating system: the Creighton Model FertilityCare System. An instructor, the FertilityCare practitioner, helps single women or married couples to chart their menstrual and ovulatory cycles according to biomarkers of fertility and infertility. Married couples can use the reproductive information generated by the charts to effectively achieve or avoid a pregnancy according to the current demands of their marriage and to ensure that the woman's reproductive system is functioning optimally. Single women can use the system of NaProTracking to maintain and monitor their reproductive health.
Treating the mucus insufficiency made sense to this couple in the context of their charting instruction for the Creighton Model FertilityCare System. In the introductory session and throughout the eight follow-up sessions, they learned that there are three requirements for optimizing natural conception: good sperm, good egg, and good mucus. Given their cervical factor infertility, they clearly understood the rationale behind the NPT physician's goal to facilitate natural conception by improving the quality and quantity of cervical mucus and intelligently cooperated.
This is a summary of material presented in Elizabeth S. Ginsburg, “Procedure for Intrauterine Insemination,” UpToDate (2012), http://www.uptodate.com/contents/procedure-for-intrauterine-insemination.
Congregation for the Doctrine of the Faith, Donum vitae, II, B, n. 6.
Congregation for the Doctrine of the Faith, Donum vitae‘s sequel, Dignitas personae, suffers from a similar omission, merely quoting the working principle from Congregation for the Doctrine of the Faith, Donum vitae, II, B, n. 6: “Homologous artificial insemination within marriage cannot be admitted except for those cases in which the technical means is not a substitute for the conjugal act, but serves to facilitate and to help so that the act attains its natural purpose” (n. 12.2).
Postcoitus, the semen specimen collected at the base of the condom is placed in a sterile receptacle, taken to the lab, centrifuged, made rich, and then injected into the woman's uterus.
Cf. “GIFT? No!” and “GIFT? Yes!” Ethics & Medics 18.9 (September 1993), for Father McCarthy's analysis of mGIFT (which also applies to mIUI) and his conclusion that mGIFT assists, not replaces, the couple's conjugal act (which is equally pertinent to the morality of mIUI).
See William E. May, “Homologous Intrauterine Insemination: Does It Replace the Marriage Act?” Zenit, September 22, 2010, http://www.zenit.org/article-30451?l=english: “It is important to note that the procedure [GIFT] was originally developed by Dr. Ricardo Asch and his associates at the University of Health Science Center in Houston, Texas, as an offshoot of IVF; and the husband's sperm was collected by masturbation. Informed that the Catholic Church condemns masturbation, even as a way of obtaining a husband's sperm, Asch and other doctors who used the method suggested that sperm be obtained by using a perforated condom during the marital act,” quoted in Chipi Buenafe, “Homologous Intrauterine Insemination: Does It Replace the Marriage Act?” Catholic Metanarrative Blog, September 23, 2010, http://4nov80.blogspot.com/2010/09/article-homologous-intrauterine.html. On this, see Rev. Donald G. McCarthy, “Catholic Medical Teaching and TOT/GIFT: Response: A Response to Donald DeMarco,” in Reproductive Technologies, Marriage and the Church, ed. Donald G. McCarthy (St. Louis: Pope John XXIII Medical Moral Center, 1988), 144.


