Abstract
Photobiomodulation therapy (PBMT) has been investigated because of its intimate relationship with tissue recovery processes, such as on peripheral nerve damage. Based on the wide range of benefits that the PBMT has shown and its clinical relevance, the aim of this research was to carry out a systematic review of the last 10 years, ascertaining the influence of the PBMT in the regeneration of injured peripheral nerves. The search was performed in the PubMed/MEDLINE database with the combination of the keywords: low-level laser therapy AND nerve regeneration. Initially, 54 articles were obtained, 26 articles of which were chosen for the study according to the inclusion criteria. In the qualitative aspect, it was observed that PBMT was able to accelerate the process of nerve regeneration, presenting an increase in the number of myelinated fibers and a better lamellar organization of myelin sheath, besides improvement of electrophysiological function, immunoreactivity, high functionality rate, decrease of inflammation, pain, and the facilitation of neural regeneration, release of growth factors, increase of vascular network and collagen. It was concluded that PBMT has beneficial effects on the recovery of nerve lesions, especially when related to a faster regeneration and functional improvement, despite the variety of parameters.
Keywords: low-level laser therapy, nerve regeneration, peripheral nerve repair, photobiomodulation therapy, tissue regeneration
1. Introduction
Low-level laser therapy (LLLT), now commonly referred to as photobiomodulation therapy (PBMT), using low-level infrared light spectrum lasers is considered a therapeutic advance. Its effects are related to tissue biostimulation, presenting therapeutic responses from photoelectric, photoenergetic, and photochemical reactions [1]. Scientific research has shown the application of PBMT in bone tissue and peripheral nerves with good results whether or not it is associated with other supporting methods in tissue repair [2,3,4,5,6,7].
Laser photobiomodulation presents itself as an electromagnetic technology that is being inserted into clinical practice due to its characteristics that differ from other conventional thermal sources [8,9]. It was observed that there are several features of PBMT that are related to the reduction of tissue repair time and its capacity to increase cell proliferation [10].
In rehabilitative health, PBMT was inserted to promote the repair and recovery of tissues. For example, in physical therapy, the use of PBMT is applied in postoperative phases as an aid in the muscular, nervous, joint, and other functional recovery processes, and in dentistry it is applied in the processes of dental extraction, grafting, osteonecrosis, and periodontal lesions [11,12,13].
The wavelength of infrared irradiation is easily absorbed by tissues and the loss of intensity is minimal, affecting metabolic modifications, DNA activity, adenosine triphosphate (ATP) formation, and the mitochondrial chain. The effect of photobiomodulation is due to the absorption of the photons by cytochrome C oxidase in the mitochondrial respiratory chain, consequently increasing the cytochrome C oxidase activity and therefore ATP formation. ATP from injured or regions of impaired blood perfusion can reactivate injured cells and metabolic disorders [10]. PBMT is also related to pain and inflammation relief and prevention of tissue death to avoid neurological degeneration [14,15].
The wavelength is the key point that regulates the depth and penetration of the laser irradiance in the tissue, noting that the absorption and dispersion coefficients are larger at the lower wavelengths. Regarding the type of wave, whether continuous or pulsed, there are still divergences in which is the best and for which factors are the pulse parameters to be chosen [16]. PBMT presents difficulties in selecting the most suitable parameters for its application due to the lack of standardization, since wavelength, power density, irradiation time, and light polarization have repercussions on the biological effects [9].
Due to the photochemical and photobiological effects of PBMT at the cellular level, there is a relationship between the improvement of trophic conditions and the reduction of inflammatory processes, closely related to a more efficient nervous regeneration and, also, promoting the secretion of neural factors [16,17]. Thus, photobiomodulation therapy in the neurological area acts as an adjuvant in the treatment of traumatic brain degeneration/injury, spinal cord trauma, and in the process of peripheral nerve regeneration.
Peripheral nerve lesions are a reality today, but there is a deficit in relating effective treatments for recovery of the nerves, resulting in considerable functional changes in the daily life of the individual. When injured, the nerve can lose its function, causing motor or sensitive deficits. There is retrograde axonal degeneration to the area of the lesion, so regeneration occurs slowly and sometimes incompletely [18,19].
At the end of the 80’s, the scientific interest in the therapeutic approach of rehabilitation for neural lesions was initiated [20], due to the good results with the use of PBMT in the recovery of injured peripheral nerves but, until the present day, there are still difficulties related to the application parameters [19,20]. Its beneficial effects are independent of the repair technique, neurorrhaphy techniques, and the use of fibrin sealants [3,6,7,21].
PBMT leads to changes in important vascular levels such as elevation of the secretion of antiapoptotic factors in ischemic organs, providing a better wound healing [22,23]; the presence of angiogenesis when ischemic organs were injured [24,25]; a decrease in the site of infarction in rats; as well as elevation in neurological scores following embolic stroke in rats [26,27].
Due to the high range of benefits that PBMT has shown and its clinical relevance of application, the aim of this research was to carry out a systematic review of the scientific papers published in the last 10 years verifying the relation of PBMT with the regeneration of injured peripheral nerves.
2. Materials and Methods
A search was performed in the PubMed/MEDLINE database, combining low-level laser therapy AND nerve regeneration keywords, over the last 10 years and restricted to the English language. The next step was to restrict the verification and consultation of articles that used animals as a study object (non-human species).
We verified those articles that presented titles and summaries that approached the subject of this research, as well as methodology, results, and relevance for its practical application.
The articles included should necessarily be presented with full access to the text. The acquired texts were analyzed and synthesized in a reflexive way in order to obtain consistent information on the subject.
3. Results
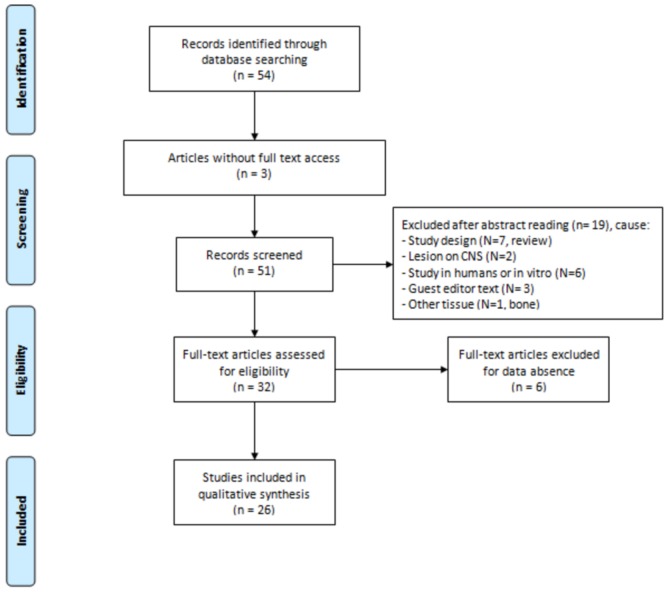
Initially, 54 articles were obtained from the PubMed/MEDLINE database, of which 28 were excluded because they were not included in the search criteria (in English, study in animals, and full access to content). At the end, 26 articles related to the subject were included. Figure 1 schematizes the search system, according to PRISMA Flow Diagram [28].
Figure 1.
Design used to select the articles.
Table 1 summarizes the data presented in the 26 articles selected for this research.
Table 1.
Data of selected articles.
| Authors | Type of Laser (Manufacturer) | Wavelength (nm)/Spot Beam | Energy (mW) | Energy Density (J/cm2) | Radiation Amount | Variables | Irradiation Site | Evaluation Time | Main Results |
|---|---|---|---|---|---|---|---|---|---|
| Buchaim et al. [2] | GaAlAs (Laserpulse IBRAMED, Brazil) | 660/0.116 | 30 | 4 | 16 s per point; 3 points | Sural nerve graft was coapted to the vagus nerve using the fibrin glue. | Right side of the neck. | Application on the 1st day post-operatory, 5 weeks, 3 times a week. Evaluation 30 days after irradiation. | LLLT improved the nerve regeneration. |
| Buchaim et al. [3] | GaAlAs (Laserpulse IBRAMED, Brazil) | 830/0.116 | 30 | 6 | 24 s per point; 3 points | Neurotmeses of buccal branch of facial nerve, followed by end-to-end suture or coaptation with heterologous fibrin sealant derived from snake venom | On the surgical site, on both sides of the face | Application 1st day post-operatory, 3 times/week for 5 weeks. Evaluation 5 and 10 weeks after the surgery. | LLLT showed satisfactory results on facial nerve regeneration. |
| Buchaim et al. [6] | GaAlAs (Laserpulse IBRAMED®, Brazil) | 830/0.116 | 30 | 6.2 | 24 s per point; 3 points | Neurotmeses of buccal branch of facial nerve, end-to-end anastomosis. Use of epineural suture or coaptation with heterologous fibrin sealant derived from snake venom. | On the surgical site, on both sides of the face | Application on the 1st day post-operatory, 3 times a week, for 5 weeks. | Laser stimulated axonal regeneration accelerated the process of functional recovery of whisker, and the two techniques used allowed the growth of axons. |
| Rosso et al. [7] | GaAlAs (Laserpulse IBRAMED®, Brazil) | 830/0.116 | 30 | 6.2 | 24 s per point; 3 points | Neurotmeses in buccal branch of facial nerve, end-lateral anastomosis in the zygomatic branch of the facial nerve with epineural suture or heterologous sealant of fibrin derived from snake venom. | On the surgical site, on both sides of the face | Application on the 1st day post- operatory, 3 times a week, for 10 weeks. | Laser groups presented faster functional recovery, similar results to the control group. It was observed that PBMT provided accelerated morphological and functional repair in the two techniques used. |
| Ziago et al. [19] | GaAlAs (Twin Laser, MMO, São Carlos, SP, Brazil) | 780/0.04 | 40 | 4 10 50 |
4, 10 e 50 s per point; 3 points | Crushing of the left sciatic nerve. | On the surgical site | Application during 6 sessions on alternate days. | Best morphological quantitative and morphometric results on L10 group after 15 days of nerve lesion. |
| Alessi Pissulin et al. [29] | GaAs (Endophoton, KLD Biosystems, Amparo, Brazil) | 904/0.035 | 50 | 69 | 48 s per point | 0.5% bupivacaine injection to the right and 0.9% sodium chloride injection to the left on sternocleidomastoid muscle and accessory nerve exposed in surgery. | Ventral side of the neck | Application 1st day post-operatory, during 5 successive days. | LLLT reduced the aggressive effects of bupivacaine on the nerve and the muscle, of muscular degeneration, of myonecrosis and fibrosis, kept the morphology of the axon and the myelin sheath. |
| Takhtfooladi; Sharifi [30] | GaAlAs (pulsed) LED (red and blue) (-----) |
680/0.04 650/1.5 red 450/1.5 blue |
10 | 10 | 200 s per point; 3 points | Neurotmeses of right sciatic nerve followed by epineural neurorrhaphy. | On the surgical site, sciatic nerve | Application 1st day post-operatory, during 14 successive days | LLLT increased Schwann cells on the great myelinic axons and on neurons, sped up and potentialized nerve regeneration. |
| Takhtfooladi et al. [31] | InGaAlP (Teralaser; DMC® São Carlos, SP, Brazil) | 685/0.028 | 15 | 3 | 10 s per point | Crushing of the left sciatic nerve. | On the surgery site on sciatic nerve. | Application on the 1st day post-operatory, during 21 successive days. | LLLT accelerated and improved the nerve function after crushing lesion. |
| Wang et al. [32] | GaAlAs (Transverse IND. CO., LTD., Taipei, Taiwan) | 808/3.8 | 170 | 3 8 15 |
67.2 s 179 s 335.6 s |
Crushing of the right sciatic nerve. | On lesion on sciatic nerve. | Application during 20 successive days. | LLLT (3 and 8 J/cm2) accelerated functional and morphologic recovery of the nerve, increased the expression of the marker GAP43. |
| Shen; Yang; Liu [33] | AlGaInP (Megalas1-AM-800, Konftec Co., Taipei, Taiwan, ROC) | 660/----- | 0.0032 | 3.84 | 5 min per day | Neurotmeses of the left sciatic nerve, 10 mm gap and use of biodegradable tube containing genipin-cross-linked gelatin annexed with β-tricalcium phosphate ceramic particles (genipin-gelatin-tricalcium phosphate, GGT) | Applied to the surgical site. | Application 1st day post-operatory, during 20 successive days. Euthanasia after 8 weeks. | LLLT obtained better functional, electrophysiological and histomorphometric results and assisted on neural repair. |
| Shen; Yang; Liu [34] | AlGaInP (MegalasVR -AM-800; Konftec, Taipei, Taiwan) | 660/---- | 50 | Immediate post-surgery (5.76) 9 following days (0.96) |
Immediate post-surgery (30 min) 9 successive consecutive (5 min) |
Neurotmeses of the left sciatic nerve, 15 mm gap and the use of 1-ethyl-3-(3-dimethylaminopro-pyl) carbodiimide (EDC) cross-linked gelatin, annexed with β-tricalcium phosphate (TCP) ceramic particles (EDC-Gelatin-TCP, EGT). | On the surgery site. | Application immediately after the lesion, during 9 successive days. Euthanasia after 12 weeks. | LLLT showed better results on the functional index, on development, on electrophysiology, on nerve regeneration, larger neural tissue area, larger axon, and myelin sheath diameter. |
| Medalha et al. [35] | GaAlAs (Teralaser, DMC São Carlos, São Paulo, Brazil) | 660/0.028 808/0.028 |
30 30 |
10 e 50 10 e 50 |
9 s and 47 s; 3 points 9 s and 47 s; 3 points |
Neurotmeses of the sciatic nerve, approximately 3 mm distal to the tendon of the internal obturator. Anastomosis with 3 sutures using nylon monofilament 10-0. | Applied to the surgical site. | Application 1st day post-operatory during 5 successive days and 2 days interval until completing 15 days. | LLLT 808 nm on 50 J/cm2 obtained higher fiber density. LLLT 660 nm on 50 J/cm2 presented larger diameters of axons and of fibers of gait functional recovery. |
| Shen et al. [36] | GaAlAsP (Aculas-AM-100A, Konftec Co., Taipei, Taiwan) | 660/0.1 | 50 | 2 | 2 min per day; 2 points at the same time | A biodegradable nerve conduit containing genipin-cross-linked gelatin was annexed using beta-tricalcium phosphate (TCP) ceramic particles (genipin-gelatin-TCP, GGT) with a 15 mm sciatic nerve transection gap. | On the sciatic nerve. | Application 1st day post-operatory during 10 successive days. | LLLT accelerated the nerve regeneration due to the larger neural tissue, larger diameter and thicker myelin sheath, motor function, electrophysiology and muscular innervation. |
| Chen et al. [37] | GaAlAs (Transverse IND. CO., LTD., Taipei, Taiwan) | 808 ± 5/≤0.5 | 190 | 8 | 207 s | Chronic compression on dorsal root ganglion. A thin L shaped needle (0,6 mm of diameter) was inserted 4 mm in the L4 and L5 intervertebral foramen. | On the dorsal root of L4 and L5. | Application 1st day post-operatory, per 8 successive days. Euthanasia 4 e 8 days. | LLLT decreased the levels of inflammatory cytokines and of pain, facilitating the nerve regeneration, demonstrated by levels of TNF-a, IL-1b e GAP-43. |
| Belchior et al. [38] | GaAlAs (KLD® Endophoton model) | 660/0.63 | 26.3 | 4 | 96.7 s; 3 points | Crushing of the right sciatic nerve. | On the surgical site. | Application 1st day post-operatory, during 20 successive days. | LLLT was positive on the functional index after the 21st day. |
| Barbosa et al. [39] | GaAlAs (Ibramed® Equipamentos Médicos) | 660/0.06 830/0.116 |
30 | 10 10 |
20 s 38.66 s |
Crushing of the right sciatic nerve. | On the surgical site. | Application 1st day post-operatory, during 20 successive days. | LLLT 660 nm promoted functional recovery in a faster manner. |
| Marcolino et al. [40] | AlGaAs (Laser Diode, Ibramed) | 830/0.116 | 30 | 10 40 80 |
38.66 s 154.66 s 309.33 s |
Crushing of the right fibular nerve. | On the right sciatic nerve. | Application immediately after surgery and during the 21 successive days. | 40 J/cm2 and 80 J/cm2 LLLT influenced the functional recovery of the nerve. |
| Akgul; Gulsoy; Gulcur [41] | Laser diode (model: DH650-24-3(5), Huanic, China) | 650/≈0.14 | 25 | 10 | 57 s on 3 points | Crushing of the sciatic nerve. | On the sciatic nerve. | Early group: Application after surgery, up to the 14th day. Delayed group: Application on the 7th day post-operatory and up to the 21st day. | LLLT accelerated nervous recovery. The group with delayed application showed better functional results. |
| Gigo-Benato et al. [42] | GaAlAs (TWIN LASER; MM Optics, São Carlos, SP, Brazil) | 660/0.04 780/0.04 |
40 40 |
10, 60 and 120 10, 60 and 120 |
0.3 s, 1 min and 2 min 0.3 s, 1 min and 2 min; 2 points |
Crushing of the left sciatic nerve. | Applied to the surgical site. | Application 1st day post-operatory, during 10 successive days. | LLLT (660 nm, 10 J/cm2 or 60 J/cm2) accelerated the neuromuscular recuperation. |
| dos Reis et al. [43] | AlGaAs (KLD®; Endophoton model) | 660/0.63 | 26.3 | 4 | 96.7 s per point; 3 points | Neurotmeses and epineural anastomosis on the right sciatic nerve. | On the surgical site. | Application 1st day post-operatory, 20 successive days. | LLLT significantly changed the morphometry (myelin sheath), but did not interfere on functionality. |
| Yang et al. [44] | GaAlAs (Aculas-Am series, Multi-channel LLLT System, Konftec Corp., Taipei, Taiwan) | 660/≈0.2 | 30 | 9 | 60 s per point; 4 points | Use of Mesenchymal stem cells (MSC) on the lesion by crushing of sciatic nerve. | On the sciatic nerve | 7 successive days. | LLLT+MSC improved the electrophysiologic function, S100 immunoreactivity, less inflammatory cells and less vacuole formation. |
| de Oliveira Martins et al. [45] | GaAs (Laserpulse-Laser, Ibramed Brazil) pulsado | 904/0.1 | 70 Wpk | 6 | 18 s on 5 points | Pulsed LLLT. Lesion on alveolar nerve, by a hemostatic Crile clamp. |
On the sciatic nerve. | 10 sessions every 10 days. | LLLT obtained better nociception, higher expression of neural growth factor (NGF) 53% and of expression of neurotrophic factor (BDNF) 40%. |
| Gomes; Dalmarco; André [46] | HeNe (----) | 632.8/0.1 | 5 | 10 | 20 s on 10 points | Crushing of the right sciatic nerve. | On the sciatic nerve. | 1st Application 24 h after surgery; 7, 14 and 21 successive days. | LLLT increased the expression of mRNA and the factors BDNF and NGF after 14 days and maximum expression was observed on the 21st day. |
| Hsieh et al. [47] | GaAlAs (Aculas-Am series, Multi-channel laser system; Konftec, Taipei, Taiwan) | 660/≈0.2 | 30 | 9 | 60 s per point; 4 points | Lesion on the sciatic nerve with 4 ligatures, using chromic suture 4-0. | On the surgery site. | Application 7th post-operatory, during 7 successive days. | LLLT improved functional index, decreased HIF-1a, TNF-a, and IL-1b, increased VEGF, NGF, and S100, reduced tissue ischemia and inflammation, helped the nerve recovery. |
| Sene et al. [48] | GaAsAl (Physiolux Dual, BIOSET, Rio Claro, Brazil) | 830/0.02 | 30 | 5 10 20 |
Maximum time of application was 40 s | Crushing of the right fibular nerve. | Application fibular nerve region. | Application immediately after the lesion, during 21 successive days. | LLLT simulation group obtained a larger nerve transverse area; group 10 J/cm2 obtained higher density of the fiber. LLLT did not speed up nerve recovery. |
| Dias et al. [49] | GaAlAs (Mm Twin Laser Optics, São Carlos, Brazil) | 780/0.4 | 30 | 15 | 20 s per point; 3 points | Latex protein (F1) on lesion per crushing of sciatic nerve. | On the surgery site, sciatic nerve. | Application per 6 sessions on alternate days. | LLLT associated to the F1 protein did not present positive results and did not potentialize the effects of this protein. |
4. Discussion
With the evolution of the technology in the health field and the evolution of the adjunct methods for rehabilitation and functional restoration of injured nerves [3,6,7,8,9], the PBMT has shown a wide range of benefits with clinical relevance. Thus, the aim of this research was to carry out a review of the scientific papers published in the last 10 years in order to verify the relation of PBMT in the regeneration of injured peripheral nerves. Regarding the varied benefits of PBMT, the highlight is the reduction of regeneration time and the aid in nerve function.
Among the effects of PBMT on nerve injury, it was verified that the laser minimized the side effects of bupivacaine on the nerve and on the muscle [29], potentiated the process of nerve regeneration observed by morpho-quantitative analysis of the axons and of the nerve fibers [2,3,19,30,31,32,33,34,35], in addition to assisting muscular reinnervation [36].
Photobiomodulation in the nerve injury was also related to a decrease in inflammatory cytokine levels, in pain, and to the facilitation of neural regeneration, demonstrated by the levels of TNF-a, IL-1b, and GAP-43 [32,37].
The functional analysis evidenced the evolution of functional recovery associated with PBMT [6,7,34,38,39]. Marcolino et al. [40] found a functional recovery with both 40 J/cm2 and 80 J/cm2 (830 nm), Akgul; Gulsoy; Gulcur [41] also scored improvement in functionality with late application PBMT (650 nm) (7 days after injury), as well as Medalha et al. [35] at 660 nm at 50 J/cm2. PBMT 660 nm, 10 J/cm2, or 60 J/cm2 accelerated neuromuscular recovery when compared to 780 nm and 830 nm PBMT [42]. Differently, dos Reis et al. [43] observed that PBMT significantly altered morphometry (myelin sheath thickness values) but did not interfere with the functionality.
Yang et al. [44], when associating PBMT with MSC, demonstrated a better electrophysiological function, immunoreactivity of S100, and fewer inflammatory cells. de Oliveira Martins et al. [45] demonstrated that PBMT (904 nm) had better nociception, greater expression of neural growth factor (NGF) 53% and neurotrophic factor expression (BDNF) 40%. As seen, Gomes; Dalmarco; André [46] evidenced that PBMT (632.8 nm) increased mRNA expression, BDNF and NGF factors after 14 days and maximum expression was observed on day 21. PBMT (660 nm) improved functional index, reduced HIF-1a, TNF-a, and IL-1b, elevated VEGF, NGF, and S100, and decreased tissue ischemia and inflammation [47]. Sene et al. [48] (830 nm) observed that PBMT did not accelerate nerve recovery and the study by Dias et al. [49] when associating PBMT (780 nm) with latex protein also did not find positive results.
The effects of PBMT on nerve damage were verified in the sciatic nerve in 17 articles [19,30,31,32,33,34,35,36,38,39,41,42,43,44,46,47,49], facial nerve in 3 [3,6,7], fibular nerve in 2 articles [40,48], and vagus nerve [2], accessory nerve [29], alveolar nerve [45], and dorsal root [37] in one article each. Of the 26 articles inserted in this review, it was observed that 14 [19,31,32,37,38,39,40,41,42,44,45,46,48,49] presented compression as nerve damage (crushing) and 11 [2,3,6,7,30,33,34,35,36,43,47] articles evaluated the effects of PBMT on neurotmeses, which is the worst type of nerve injury.
It has been observed that the diversity of PBMT application protocols in nerve lesions is large, with the wavelength varying from 632.8 to 904 nm, a varied range of energy and energy density, in addition to the time of application, despite the similarity in the type of lesion targeted in each experiment. As shown, the infrared spectrum has good experimental results. The red spectrum (600 to 700 nm) [50] was seen in 15 studies with satisfactory morphological and electrophysiological results, immunological factors, and tissue markers [2,30,31,33,34,35,36,38,39,41,42,43,44,46,47]. It was also possible to verify the lack of standardization in relation to the application protocols, noting that 6 studies were discarded due to lack of data information regarding energy density and time of application of PBMT.
In a general critical analysis of the articles for the detailed study, a consensus was observed on the effectiveness of PBMT, with the use of low-level laser therapy on the improvement of the morphological and morphometric aspects of the regenerated peripheral nerve, as well as on the reduction of events inflammatory and painful sensitivity, providing faster and higher quality functional recovery [51,52].
In the perspective of new fronts of study, in the last decade, optogenetic and chemogenetic techniques have been used more frequently in the investigation of neuronal circuits, as well as in the study of non-neuronal cells in the brain and peripheral nerves. Optogenetics is effective in generating patterns that mimic neuron responses using a pulse generator that produces lights with different frequencies and pulse durations. Photostimulation can be performed in different subcellular regions, being useful for the study of neuronal circuits in the brain. Chemogenetics are less invasive in animal experiments and do not require the installation of a fiber optic cable into the brain or the connection of the cable to a light source, such as a laser or a light emitting diode (LED).
5. Conclusions
At the end of the present study, it can be seen that the data presented in the current articles helped us to understand the beneficial and helpful effects of photobiomodulation on regeneration and functionality after nerve injury. In spite of the great variety of parameters presented, great results were observed, mainly when related to the faster nervous regeneration process.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Angeletti P., Pereira M.D., Gomes H.C., Hino C.T., Ferreira L.M. Effect of low-level laser therapy (GaAlAs) on bone regeneration in midpalatal anterior suture after surgically assisted rapid maxillary expansion. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010;109:e38–e46. doi: 10.1016/j.tripleo.2009.10.043. [DOI] [PubMed] [Google Scholar]
- 2.Buchaim R.L., Andreo J.C., Barraviera B., Ferreira Junior R.S., Buchaim D.V., Rosa Junior G.M., de Oliveira A.L., de Castro Rodrigues A. Effect of low-level laser therapy (LLLT) on peripheral nerve regeneration using fibrin glue derived from snake venom. Injury. 2015;46:655–660. doi: 10.1016/j.injury.2015.01.031. [DOI] [PubMed] [Google Scholar]
- 3.Buchaim D.V., de Castro Rodrigues A., Buchaim R.L., Barraviera B., Junior R.S., Junior G.M., Bueno C.R., Roque D.D., Dias D.V., Dare L.R., et al. The new heterologous fibrina sealant in combination with low-level laser therapy (LLLT) in the repair of the buccal branch of the facial nerve. Lasers Med. Sci. 2016;31:965–972. doi: 10.1007/s10103-016-1939-2. [DOI] [PubMed] [Google Scholar]
- 4.De Oliveira Gonçalves J.B., Buchaim D.V., de Souza Bueno C.R., Pomini K.T., Barraviera B., Júnior R.S.F., Andreo J.C., de Castro Rodrigues A., Cestari T.M., Buchaim R.L. Effects of low-level laser therapy on autogenous bone graft stabilized with a new heterologous fibrin sealant. J. Photochem. Photobiol. B. 2016;162:663–668. doi: 10.1016/j.jphotobiol.2016.07.023. [DOI] [PubMed] [Google Scholar]
- 5.De Vasconcellos L.M., Barbara M.A., Rovai E.S., de Oliveira França M., Ebrahim Z.F., de Vasconcellos L.G., Porto C.D., Cairo C.A. Titanium scaffold osteogenesis in healthy and osteoporotic rats is improved by the use of low-level laser therapy (GaAlAs) Lasers Med. Sci. 2016;31:899–905. doi: 10.1007/s10103-016-1930-y. [DOI] [PubMed] [Google Scholar]
- 6.Buchaim D.V., Andreo J.C., Ferreira Junior R.S., Barraviera B., Rodrigues A.C., Macedo M.C., Rosa Junior G.M., Shinohara A.L., Santos German I.J., Pomini K.T., et al. Efficacy of Laser Photobiomodulation on Morphological and Functional Repair of the Facial Nerve. Photomed. Laser Surg. 2017;35:442–449. doi: 10.1089/pho.2016.4204. [DOI] [PubMed] [Google Scholar]
- 7.Rosso M.P.O., Rosa Júnior G.M., Buchaim D.V., German I.J.S., Pomini K.T., de Souza R.G., Pereira M., Favaretto Júnior I.A., Bueno C.R.S., Gonçalves J.B.O., et al. Stimulation of morphofunctional repair of the facial nerve with photobiomodulation, using the end-to-side technique or a new heterologous fibrin sealant. J. Photochem. Photobiol. B. 2017;175:20–28. doi: 10.1016/j.jphotobiol.2017.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Sulewski J.G. Historical survey of laser dentistry. Dent. Clin. N. Am. 2000;44:717–752. [PubMed] [Google Scholar]
- 9.Ginani F., Soares D.M., Barreto M.P., Barboza C.A. Effect of low-level laser therapy on mesenchymal stem cell proliferation: A systematic review. Lasers Med. Sci. 2015;30:2189–2194. doi: 10.1007/s10103-015-1730-9. [DOI] [PubMed] [Google Scholar]
- 10.Morries L.D., Cassano P., Henderson T.A. Treatments for traumatic brain injury with emphasis on transcranial near-infrared laser phototherapy. Neuropsychiatr. Dis. Treat. 2015;20:2159–2175. doi: 10.2147/NDT.S65809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang W.D., Wu J.H., Wang H.J., Jiang J.A. Therapeutic outcomes of low-level laser therapy for closed bone fracture in the human wrist and hand. Photomed. Laser Surg. 2014;32:212–218. doi: 10.1089/pho.2012.3398. [DOI] [PubMed] [Google Scholar]
- 12.Gladsjo J.A., Jiang S.I. Treatment of surgical scars using a 595-nm pulsed dye laser using purpuric and nonpurpuric parameters: A comparative study. Dermatol. Surg. 2014;40:118–126. doi: 10.1111/dsu.12406. [DOI] [PubMed] [Google Scholar]
- 13.Keaney T.C., Tanzi E., Alster T. Comparison of 532 nm potassium titanyl phosphate laser and 595 nm pulsed dye laser in the treatment of erythematous surgical scars: A randomized, controlled, Open-label study. Dermatol. Surg. 2016;42:70–76. doi: 10.1097/DSS.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 14.Li W.T., Chen H.L., Wang C.T. Effect of light emitting diode irradiation on proliferation of human bone marrow mesenchymal stem cells. J. Med. Biol. Eng. 2006;26:35–42. [Google Scholar]
- 15.Wu Y.H., Wang J., Gong D.X., Gu H.Y., Hu S.S., Zhang H. Effects of low-level laser irradiation on mesenchymal stem cell proliferation: A microarray analysis. Lasers Med. Sci. 2012;27:509–519. doi: 10.1007/s10103-011-0995-x. [DOI] [PubMed] [Google Scholar]
- 16.Hashmi J.T., Huang Y.Y., Osmani B.Z., Sharma S.K., Naeser M.A., Hamblin M.R. Role of low-level laser therapy in neurorehabilitation. PM&R. 2010;2:292–305. doi: 10.1016/j.pmrj.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yazdani S.O., Golestaneh A.F., Shafiee A., Hafizi M., Omrani H.A., Soleimani M. Effects of low level laser therapy on proliferation and neurotrophic factor gene expression of human schwann cells in vitro. J. Photochem. Photobiol. B. 2012;107:9–13. doi: 10.1016/j.jphotobiol.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Martínez de Albornoz P., Delgado P.J., Forriol F., Maffulli N. Non-surgical therapies for peripheral nerve injury. Br. Med. Bull. 2011;100:73–100. doi: 10.1093/bmb/ldr005. [DOI] [PubMed] [Google Scholar]
- 19.Ziago E.K., Fazan V.P., Iyomasa M.M., Sousa L.G., Yamauchi P.Y., da Silva E.A., Borie E., Fuentes R., Dias F.J. Analysis of the variation in low-level laser energy density on the crushed sciatic nerves of rats: A morphological, quantitative, and morphometric study. Lasers Med. Sci. 2017;32:369–378. doi: 10.1007/s10103-016-2126-1. [DOI] [PubMed] [Google Scholar]
- 20.Gigo-Benato D., Geuna S., Rochkind S. Phototherapy for enhancing peripheral nerve repair: A review of the literature. Muscle Nerve. 2005;31:694–701. doi: 10.1002/mus.20305. [DOI] [PubMed] [Google Scholar]
- 21.Rosso M.P.O., Buchaim D.V., Rosa Junior G.M., Andreo J.C., Pomini K.T., Buchaim R.L. Low-Level Laser Therapy (LLLT) Improves the Repair Process of Peripheral Nerve Injuries: A Mini Review. Int. J. Neurorehabilit. 2017;4:260. doi: 10.4172/2376-0281.1000260. [DOI] [Google Scholar]
- 22.Gigo-Benato D., Geuna S., de Castro Rodrigues A., Tos P., Fornaro M., Boux E., Battiston B., Giacobini-Robecchi M.G. Low-power laser biostimulation enhances nerve repair after end-to-side neurorrhaphy: A double-blind randomized study in the rat median nerve model. Lasers Med. Sci. 2004;19:57–65. doi: 10.1007/s10103-004-0300-3. [DOI] [PubMed] [Google Scholar]
- 23.Rochkind S., Drory V., Alon M., Nissan M., Ouaknine G.E. Laser phototherapy (780 nm), a new modality in treatment of long-term incomplete peripheral nerve injury: A randomized double-blind placebo-controlled study. Photomed. Laser Surg. 2007;25:436–442. doi: 10.1089/pho.2007.2093. [DOI] [PubMed] [Google Scholar]
- 24.Khullar S.M., Brodin P., Messelt E.B., Haanaes H.R. The effects of low level laser treatment on recovery of nerve conduction and motor function after compression injury in the rat sciatic nerve. Eur. J. Oral Sci. 1995;103:299–305. doi: 10.1111/j.1600-0722.1995.tb00030.x. [DOI] [PubMed] [Google Scholar]
- 25.Stainki D.R., Raiser A.G., Graça D.L., Becker C., Fernandez G.M.S. Gallium arsenide (GaAs) laser radiation in the radial nerve regeneration submitted secondary to surgical repair. Braz. J. Vet. Res. Anim. Sci. 1999;35:37–40. [Google Scholar]
- 26.De Medinaceli L., Freed W.J., Wyatt R.J. An index of the functional condition of rat sciatic nerve based on measurements made from walking tracks. Exp. Neurol. 1982;7:634–643. doi: 10.1016/0014-4886(82)90234-5. [DOI] [PubMed] [Google Scholar]
- 27.Gasparini A.L.P., Barbieri C.H., Mazzer N. Correlation between different methods of gait functional evaluation in rats with ischiatic nerve crushing injuries. Acta Ortop. Bras. 2007;15:285–289. doi: 10.1590/S1413-78522007000500011. [DOI] [Google Scholar]
- 28.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group referred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alessi Pissulin C.N., Henrique Fernandes A.A., Sanchez Orellana A.M., Rossi E., Silva R.C., Michelin Matheus S.M. Low-level laser therapy (LLLT) accelerates the sternomastoid muscle regeneration process after myonecrosis due to bupivacaine. J. Photochem. Photobiol. B. 2017;168:30–39. doi: 10.1016/j.jphotobiol.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 30.Takhtfooladi M.A., Sharifi D. A comparative study of red and blue light-emitting diodes and low-level laser in regeneration of the transected sciatic nerve after an end to end neurorrhaphy in rabbits. Lasers Med. Sci. 2015;30:2319–2324. doi: 10.1007/s10103-015-1813-7. [DOI] [PubMed] [Google Scholar]
- 31.Takhtfooladi M.A., Jahanbakhsh F., Takhtfooladi H.A., Yousefi K., Allahverdi A. Effect of low-level laser therapy (685 nm, 3 J/cm2) on functional recovery of the sciatic nerve in rats following crushing lesion. Lasers Med. Sci. 2015;30:1047–1052. doi: 10.1007/s10103-015-1709-6. [DOI] [PubMed] [Google Scholar]
- 32.Wang C.Z., Chen Y.J., Wang Y.H., Yeh M.L., Huang M.H., Ho M.L., Liang J.I., Chen C.H. Low-level laser irradiation improves functional recovery and nerve regeneration in sciatic nerve crush rat injury model. PLoS ONE. 2014;13:e103348. doi: 10.1371/journal.pone.0103348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shen C.C., Yang Y.C., Liu B.S. Large-area irradiated low-level laser effect in a biodegradable nerve guide conduit on neural regeneration of peripheral nerve injury in rats. Injury. 2011;42:803–813. doi: 10.1016/j.injury.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 34.Shen C.C., Yang Y.C., Liu B.S. Effects of large-area irradiated laser phototherapy on peripheral nerve regeneration across a large gap in a biomaterial conduit. J. Biomed. Mater. Res. 2013;101:239–252. doi: 10.1002/jbm.a.34314. [DOI] [PubMed] [Google Scholar]
- 35.Medalha C.C., Di Gangi G.C., Barbosa C.B., Fernandes M., Aguiar O., Faloppa F., Leite V.M., Renno A.C. Low-level laser therapy improves repair following complete resection of the sciatic nerve in rats. Lasers Med. Sci. 2012;27:629–635. doi: 10.1007/s10103-011-1008-9. [DOI] [PubMed] [Google Scholar]
- 36.Shen C.C., Yang Y.C., Huang T.B., Chan S.C., Liu B.S. Low-Level Laser-Accelerated Peripheral Nerve Regeneration within a Reinforced Nerve Conduit across a Large Gap of the Transected Sciatic Nerve in Rats. Evid. Based Complement. Altern. Med. 2013;2013:175629. doi: 10.1155/2013/175629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen Y.J., Wang Y.H., Wang C.Z., Ho M.L., Kuo P.L., Huang M.H., Chen C.H. Effect of low level laser therapy on chronic compression of the dorsal root ganglion. PLoS ONE. 2014;9:e89894. doi: 10.1371/journal.pone.0089894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Belchior A.C., dos Reis F.A., Nicolau R.A., Silva I.S., Perreira D.M., de Carvalho P.D.T.C. Influence of laser (660 nm) on functional recovery of the sciatic nerve in rats following crushing lesion. Lasers Med. Sci. 2009;24:893–899. doi: 10.1007/s10103-008-0642-3. [DOI] [PubMed] [Google Scholar]
- 39.Barbosa R.I., Marcolino A.M., de Jesus Guirro R.R., Mazzer N., Barbieri C.H., de Cássia Registro Fonseca M. Comparative effects of wavelengths of low-power laser in regeneration of sciatic nerve in rats following crushing lesion. Lasers Med. Sci. 2010;25:423–430. doi: 10.1007/s10103-009-0750-8. [DOI] [PubMed] [Google Scholar]
- 40.Marcolino A.M., Barbosa R.I., das Neves L.M., Mazzer N., de Jesus Guirro R.R., de Cássia Registro Fonseca M. Assessment of functional recovery of sciatic nerve in rats submitted to low-level laser therapy with different fluences. An experimental study: Laser in functional recovery in rats. J. Hand Microsurg. 2013;5:49–53. doi: 10.1007/s12593-013-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Akgul T., Gulsoy M., Gulcur H.O. Effects of early and delayed laser application on nerve regeneration. Lasers Med. Sci. 2014;29:351–357. doi: 10.1007/s10103-013-1355-9. [DOI] [PubMed] [Google Scholar]
- 42.Gigo-Benato D., Russo T.L., Tanaka E.H., Assis L., Salvini T.F., Parizotto N.A. Effects of 660 and 780 nm low-level laser therapy on neuromuscular recovery after crush injury in rat sciatic nerve. Lasers Surg. Med. 2010;42:673–682. doi: 10.1002/lsm.20978. [DOI] [PubMed] [Google Scholar]
- 43.Dos Reis F.A., Belchior A.C.G., de Carvalho P.T.C., da Silva B.A., Pereira D.M., Silva I.S., Nicolau R.A. Effect of laser therapy (660 nm) on recovery of the sciatic nerve in rats after injury through neurotmesis followed by epineural anastomosis. Lasers Med. Sci. 2009;24:741–747. doi: 10.1007/s10103-008-0634-3. [DOI] [PubMed] [Google Scholar]
- 44.Yang C.C., Wang J., Chen S.C., Hsieh Y.L. Synergistic effects of low-level laser and mesenchymal stem cells on functional recovery in rats with crushed sciatic nerves. J. Tissue Eng. Regener. Med. 2016;10:120–131. doi: 10.1002/term.1714. [DOI] [PubMed] [Google Scholar]
- 45.De Oliveira Martins D., Martinez dos Santos F., Evany de Oliveira M., de Britto L.R., Benedito Dias Lemos J., Chacur M. Laser therapy and pain-related behavior after injury of the inferior alveolar nerve: Possible involvement of neurotrophins. J. Neurotrauma. 2013;30:480–486. doi: 10.1089/neu.2012.2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gomes L.E., Dalmarco E.M., André E.S. The brain-derived neurotrophic factor, nerve growth factor, neurotrophin-3, and induced nitric oxide synthase expressions after low-level laser therapy in an axonotmesis experimental model. Photomed. Laser Surg. 2012;30:642–647. doi: 10.1089/pho.2012.3242. [DOI] [PubMed] [Google Scholar]
- 47.Hsieh Y.L., Chou L.W., Chang P.L., Yang C.C., Kao M.J., Hong C.Z. Low-level laser therapy alleviates neuropathic pain and promotes function recovery in rats with chronic constriction injury: Possible involvements in hypoxia-inducible factor 1α (HIF-1α) J. Comp. Neurol. 2012;520:2903–2916. doi: 10.1002/cne.23072. [DOI] [PubMed] [Google Scholar]
- 48.Sene G.A., Sousa F.F., Fazan V.S., Barbieri C.H. Effects of laser therapy in peripheral nerve regeneration. Acta Ortop. Bras. 2013;21:266–270. doi: 10.1590/S1413-78522013000500005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dias F.J., Issa J.P., Coutinho-Netto J., Fazan V.P., Sousa L.G., Iyomasa M.M., Papa P.C., Watanabe I.S. Morphometric and high-resolution scanning electron microscopy analysis of low-level laser therapy and latex protein (Hevea brasiliensis) administration following a crush injury of the sciatic nerve in rats. J. Neurol. Sci. 2015;349:129–137. doi: 10.1016/j.jns.2014.12.043. [DOI] [PubMed] [Google Scholar]
- 50.Moore P., Ridgway T.D., Higbee R.G., Howard E.W., Lucroy M.D. Effect of wavelength on low-intensity laser irradiation-stimulated cell proliferation in vitro. Lasers Surg. Med. 2005;36:8–12. doi: 10.1002/lsm.20117. [DOI] [PubMed] [Google Scholar]
- 51.Bang J., Kim H.Y., Lee H. Optogenetic and Chemogenetic Approaches for Studying Astrocytes and Gliotransmitters. Exp. Neurobiol. 2016;25:205–221. doi: 10.5607/en.2016.25.5.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Iyer S.M., Vesuna S., Ramakrishnan C., Huynh K., Young S., Berndt A., Lee S.Y., Gorini C.J., Deisseroth K., Delp S.L. Optogenetic and chemogenetic strategies for sustained inhibition of pain. Sci. Rep. 2016;6:30570. doi: 10.1038/srep30570. [DOI] [PMC free article] [PubMed] [Google Scholar]