Abstract
Objective:
To determine the feasibility and efficacy of using a structured Nintendo Wii protocol to improve range of motion, strength, and quality of life in patients with shoulder impingement syndrome.
Methods:
A total of 14 patients with shoulder pain were randomized to perform a structured Wii protocol (n = 8) or conventional therapy (n = 6). Pain-free shoulder range of motion, strength, shoulder pain and disability, and quality of life were assessed pre- and post-treatment.
Results:
All 8 patients completed the Wii protocol, and 3 completed conventional therapy. The Wii protocol conferred significant improvements in shoulder range of motion, pain and disability, and quality of life but not strength, whereas conventional therapy conferred a significant improvement in strength.
Conclusions:
As compared to conventional treatment, the structured Wii protocol implemented in this pilot study was a viable adjunct to therapy for shoulder impingement syndrome. Gaming may have a supplemental benefit by increasing motivation, pleasure, and/or adherence. Further investigation in larger cohorts is warranted.
Keywords: Shoulder impingement syndrome, Shoulder pain, Rehabilitation, Gaming, Motivation
1. Introduction
The annual prevalence and incidence of shoulder problems among adults is 2.4% and 1.5%, respectively [1]. Shoulder disorders represent approximately one-fifth of all disability payments for musculoskeletal disorders [2], with significant economic impact [3,4]. The most common shoulder disorder in general practice is shoulder impingement syndrome (SIS) [5], which is caused by compression of the rotator cuff tendons, most prominently the supraspinatus tendon and long head of the biceps along with their bursae in the subacromial space [6].
The primary risk factor for SIS is repetitive activity at or above the shoulder level, which may include work or recreational activities [7–9]. Age is an additional influencing factor because the incidence of SIS is increased among people older than 40 years [10]. The underlying mechanisms are thought to include inflammation and/or degeneration of the tendon(s) or bursa(e), dysfunctional scapulothoracic and glenohumeral mechanics, debilitated scapular and/or rotator cuff musculature, joint capsule irregularities, postural abnormalities of the neck and/or shoulder, and morphological abnormalities of the relevant skeletal elements [2]. Repetitive activity, particularly during overhead work, heavy lifting and forceful work, as well as working in an awkward posture increases the risk of shoulder disorders [8,9]. During arm elevation, the scapula must externally rotate, upwardly torque and tilt posteriorly [11]. Abnormal scapular kinematics is common in SIS [12] and may include reduced upward rotation and external rotation of the scapula, along with increased elevation and retraction of the clavicle [13], although increased upward rotation of the scapula has also been noted [14,15].
Shoulder pain and dysfunction secondary to SIS is often precipitated or exacerbated by an imbalance between the various muscle groups of the shoulder: the deltoids [16,17], the rotator cuff (including the supraspinatus, infraspinatus, teres minor, and subscapularis) [18–21], and the scapular stabilizers (including the trapezius, serratus anterior, rhomboids, levator scapula, and pectoralis major) [22,23]. The relative difference in activation of specific muscles affects the biomechanics of the shoulder and may lead to changes in articulation between the glenoid fossa of the scapula and the humeral head [24]. These imbalances are often exacerbated by overhead activity, as subjectively reported [25]; however, objective evidence suggests that acromiohumeral distance may be shortest during activities closer to 90° [26]. Therapy for SIS involves restoring the balance between these muscle groups to optimize the kinematics of shoulder movement, minimize wear and tear, and decrease pain [27].
Therapeutic exercises for SIS focus on 3 goals. First, the scapular stabilizers must be strengthened to provide a stable skeletal scaffold for the rotator cuff muscles [28,29]. Second, imbalances between the rotator cuff muscles must be corrected. Typically the internal rotators are stronger than the external rotators, which must be addressed by strengthening the external rotators to create net neutral forces [30,31]. Third, after the rotator cuff muscles have been strengthened, coordination in compound shoulder movements, involving movements in multiple planes, must be improved [32,33]. Improvements in strength and coordination will then facilitate activities of daily living and broader functional goals.
A major obstacle in the treatment of musculoskeletal pain is compliance with and motivation to perform the prescribed exercise program [34–36]. Conventional therapy is effective as long as the patient remains engaged. The repetitive nature of the therapy may become tedious for patients who are unaccustomed to exercise, which can limit rehabilitation outcomes and recovery. “Gamification” of therapy (or game-based therapy) in rehabilitation is a strategy that can potentially address motivation and compliance and has been shown to increase compliance [37]. However, gaming, if not performed properly can also lead to injury [38].
We developed a structured protocol for game-based rehabilitation of shoulder movements using the Nintendo Wii system. The goal of this pilot randomized controlled trial was to examine the feasibility and efficacy of a structured Wii protocol and compare it to conventional therapy for improving pain-free shoulder range of motion (ROM), strength, and quality of life in patients with SIS.
2. Methods
2.1. Study design
2.1.1. Patients
All patients were recruited from the outpatient rehabilitation facilities at Mount Sinai Medical Center, New York, and informed consent was obtained as per the Institutional Review Board and the Declaration of Helsinki.
The inclusion criteria were:
clinical diagnosis of SIS: subacromial bursitis and/or rotator cuff impingement with positive sign in 1 of 3 tests (Neer, Empty Can, and Hawkins);
subjective pain relief on current medication regimen to be able to perform basic activities of daily living (self-reported), thereby suggesting the ability to participate in therapy;
no neurological or cognitive disorders.
The exclusion criteria were:
history of surgery or other significant injury to either upper extremity;
presence of full thickness rotator cuff tear confirmed on MRI;
presence of radicular pain and other neurological signs indicating nerve pathology;
shoulder instability diagnosed by a positive apprehension test.
We recruited 15 patients who were pseudo-randomized in an alternating manner into the 2 treatment groups once they signed informed consent and completed baseline tests: 8 were allocated to the Wii group and 7 to the conventional therapy (control) group. However, after allocation, one control patient withdrew. After attrition, 8 patients remained in the Wii group (mean age 52 ± 25 years) and 3 in the control group (mean age 61 ± 23 years). Among the 6 patients randomized to the control group, one withdrew because of lack of interest during initial assessments, another because of a work-related injury, and a third because of dizziness after completing 3 weeks of therapy (Fig. 1).
Fig. 1.
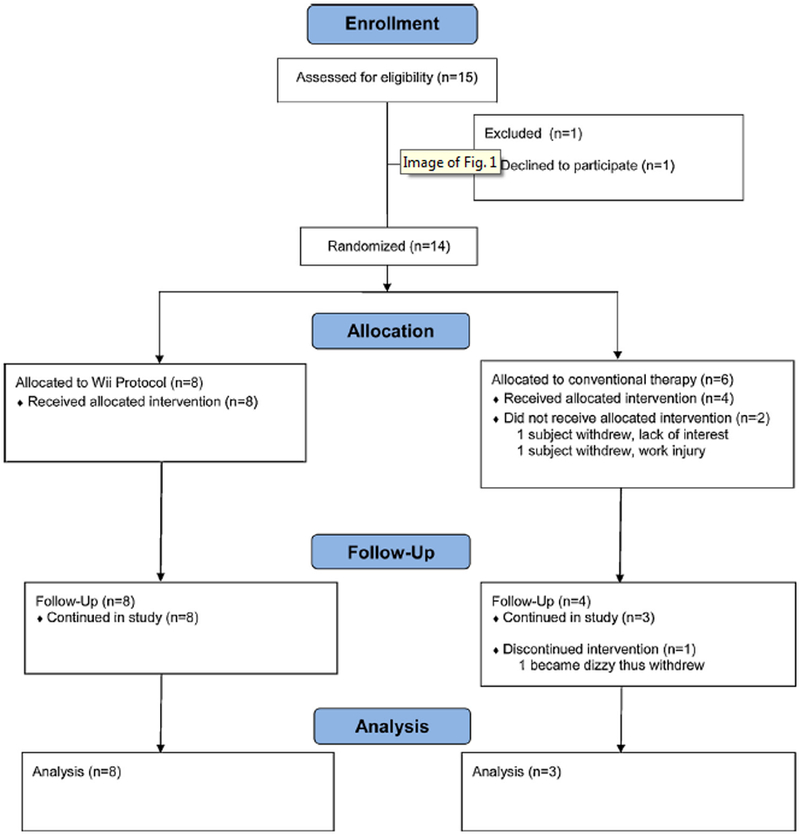
Flow of patients in the study.
2.1.2. ROM analysis
Maximum, active, pain-free, shoulder ROM in the frontal, sagittal and horizontal planes was assessed using Dartfish video analysis (Dartfish, Atlanta, GA) [39–41]. The patients wore dark clothes with reflective markers positioned over the shoulder and elbow joints at defined anatomical locations. Patients stood erect with their arms by their sides before starting each movement. The instructed movements and corresponding camera positions used for assessing ROM in each plane are detailed below. Three trials were recorded for each movement with the affected side only and the average ROM was obtained.
2.1.2.1. Frontal plane.
The camera was positioned in front of and perpendicular to the patient at a distance of 2 m. Patients were asked to abduct their shoulder from the anatomical position to 180°.
2.1.2.2. Sagittal plane.
The camera was positioned to the side and perpendicular to the patient at a distance of 2 m. Patients were asked to forward flex their shoulder from the anatomical position to 180°.
2.1.2.3. Horizontal plane.
The camera was mounted on the ceiling and the patient stood directly below it. Patients were asked to first touch the opposite shoulder, then externally rotate the shoulder and extend the arm maximally to the side in the horizontal plane.
2.1.3. Strength testing
Strength was tested in the shoulder internal and external rotators as well as scapular stabilizers by using a digital scale that we validated in the laboratory for reliability (Balanzza, Miami, FL, USA model BZ100). The scale was affixed to a stable platform (a heavy height-adjustable table) and patients were asked to grasp the handle of the scale while pulling with maximum force for each of the outlined movements; the arm was positioned uniquely for each of the strength assessments as described below. Three trials were recorded for each movement with the affected side only and the average strength was obtained.
2.1.3.1. Internal and external rotator strength.
Patients were seated upright in a chair with the elbow joint at 90° and the shoulder joint at 0° (i.e., the upper arm held close to the body). While grasping the handle of the scale, patients were instructed to internally and externally rotate their arm with maximum force as readings were taken.
2.1.3.2. Scapular stabilizer strength.
Patients were seated upright with the elbow joint at 90°, the hand/wrist was at the side of the body, and the shoulder was extended and abducted 30° with neutral rotation (0° internal/external rotation). Patients were instructed to grasp the handle of the scale and adduct their upper arm (towards their body) with maximum force by activating the scapular stabilizers (e.g., rhomboids) as readings were taken.
2.1.4. Pain and disability assessment
Pain was measured using the Shoulder Pain and Disability Index (SPADI) [42] which consists of 13 items divided into 2 sections: pain and disability. Each item is scored on a scale from 1 to 10, for a maximum of 130 points. The SPADI has been found valid, reliable, and responsive to change in patients with shoulder pathology [43]. The first section consists of 5 items that assess perception of pain during specific activities. A high score indicates more pain, and the total score is obtained by summing the scores for each item, expressed as a percentage of the maximum score. The second section assesses disability on 8 items, and the total score is expressed as a percentage of the maximum score. The total SPADI score summarizes both pain and disability scores.
2.1.5. Quality of life assessment
Quality of life was measured by the Western Ontario Rotator Cuff Index (WORC) [44], shown to have adequate-to-good validity, reliability, internal consistency, and responsiveness [45–47]. The WORC is a 21-item self-administered questionnaire with 5 subscales: physical symptoms, sports/recreation, work, lifestyle, and emotions. Each item response is marked on a 100-mm visual analog scale (VAS) and summed to provide a total score out of 2100, which is converted to a percentage. Patients were asked to answer the questions based on how they felt during the past week. A low score on each subscale and the aggregate score and a high percentage score indicate high quality of life.
2.2. Treatment protocol
2.2.1. Conventional therapy
The conventional therapy protocol was identical to the protocol used at Mount Sinai’s outpatient rehabilitation facility for patients with SIS. Patients attended two 30- to 40-min sessions per week for 6 weeks. To maintain consistency, all sessions were administered by one occupational therapist. Sessions began by measuring pain on a VAS, followed by flexibility exercises for 5 to 10 min selected from the sets of exercises in the Appendix.
The therapist then exercised specific muscle groups for approximately 15 to 20 min targeting:
scapular stabilizers with lateral pull-downs, rowing, shoulder shrugs and scapular protraction/retraction exercises in the supine position;
rotator cuff muscles with resistance bands during internal and external rotations;
the coordination of muscles with compound movements.
The strengthening program was standardized in terms of the exercises [48], but the number of repetitions and order of exercises was varied on a case-by-case basis across 12 sessions over 6 weeks of treatment. The session ended with a 5-min cool-down. The flexibility exercises from the exercise sets performed in sessions were provided as a standardized home-based exercise program (see Appendix) to be performed up to twice a day, and compliance was monitored in a self-reporting exercise diary. The exercise sets increased as the patient’s condition improved.
2.3. Structured Wii protocol
Training with the structured Wii protocol paralleled the length, frequency, and purpose of the conventional therapy for shoulder pain but was provided with the Nintendo Wii System (Nintendo, Japan) for 30 to 40 min twice a week for 6 weeks. One researcher administered all the training sessions. Each session involved a warm-up, exercises with the Wii sports games, and a cool-down. The Wii protocol included movements from bowling and boxing games during supervised sessions using the Wii remote (model RVL-003) and the Wii ‘‘Nunchuck’’ (model RVL-004). The Wii remote (a remote controller with a 3-axis accelerometer and optical sensor) was held in the hand with the painful shoulder, and the Nunchuck (a remote controller connected to the Wii remote with a cable includes a 3-axis motion sensor, analog stick, and 2 buttons) was held in the other hand. Straps connected to the Wii remotes were secured onto the patient’s wrists to prevent accidental release of the remote.
2.3.1. Warm-up
Patients first performed warm-up and stretching exercises for 10 min. The warm-up consisted of gentle circular movements of both shoulders, which included elevation, retraction, depression, and protraction movements of the scapulae. Patients then reached forward to touch targets marked around the circumference of a circle (61 cm in diameter but adjustable to fit the patient’s ROM) with their painful arm. A metronome was used so that the patient extended the arm to touch a target on one beat and retracted the arm on the alternate beat, moving sequentially around the circumference of the circle. This movement was performed for 3 turns clockwise and then 3 turns counterclockwise with the metronome set to 60 beats/min. The speed of the metronome was increased to 120 beats/min for a second set, and to 240 beats/min for a third set. This warm-up protocol was used at each session before the patient played the Wii games.
2.3.2. Wii games
The Wii games were progressively advanced to facilitate specific movements needed to restore biomechanical balance across the various shoulder muscle groups). Each game segment lasted approximately 15 to 20 min. Patients were given rest breaks when needed to prevent fatigue, and pain was assessed on a VAS during each session [49].
The Wii bowling game involves retraction of the scapula to swing the virtual ball back, followed by protraction of the scapula to release the ball. This game was used to re-train the scapular stabilizers first, then train coordination between the scapular stabilizers and the shoulder flexors. The Wii boxing game has a “dodging” exercise used to re-train shoulder internal and external rotation.
Patients played the Wii bowling and boxing games in 5 phases: phase 1 lasted 2 weeks (4 sessions) and the other 4 phases lasted 1 week each (2 sessions), for a total of 12 sessions (Table 1). In phase 1, patients focused on scapular retraction movements to strengthen the scapular stabilizers. During the bowling game, patients were asked to retract the scapula as the arm swung the virtual ball back before releasing it. The researcher showed patients how to perform the requested movement, and errors in execution were corrected verbally and by hands-on guidance. In phase 2, patients continued to train scapular retraction, with additional focus on internal and external rotation at the shoulder. Patients began the session with 10 frames of bowling, retraction only, and then progressed to the dodging exercise in the Wii boxing game. The upper arms were restrained to the side of the body with a band to prevent shoulder abduction, and a wrist guard deterred motions at the wrist. The upper arms were then only able to rotate from side to side in a “windshield-wiper” manner, thereby focusing on internal and external rotation of the shoulder, just as boxers move their arms in synchrony with a dodging movement from side to side. In phase 3, training of shoulder internal and external rotation continued, and the proper technique for scapular protraction was emphasized. Patients began with the dodging game and then progressed to bowling. The goal of bowling this time was to focus on swinging the arm forward to release the ball. Phase 4 focused on coordinating scapular retraction and protraction movements while continuing to strengthen the shoulder rotators. Patients began with the dodging game and proceeded to bowling. The focus of bowling was to smoothly coordinate the retraction and protraction motions. In phase 5, the emphasis was on shoulder coordination using the Wii boxing game’s punching exercises. Patients began with the dodging game and progressed to boxing. Patients punched 3 times with one hand (moving medially to laterally), then switched to the opposite hand, repeating until the round was over. Each round lasted approximately 90 sec and the game ended when 3 rounds were finished.
Table 1.
Structured Wii protocol.
| Phase | Weeks | Session(s) | Therapy |
|---|---|---|---|
| 1 | 1–2 | 1–4 | Dodging: (held) Bowling: retraction only Boxing: (held) |
| 2 | 3 | 5–6 | Dodging: game for internal and external rotators Bowling: retraction only Boxing: (held) |
| 3 | 4 | 7–8 | Dodging: game for internal and external rotators Bowling: protraction Boxing: (held) |
| 4 | 5 | 9–10 | Dodging: game for internal and external rotators Bowling: coordination of retraction and protraction Boxing: (held) |
| 5 | 6 | 11–12 | Dodging: game for internal and external rotators Bowling: (held) Boxing: punching exercises; punching three times with one hand from medial to lateral and then switching |
2.3.3. Cool-down
At the end of each session, patients performed cool-down exercises for 5–10 min. Using the same target as for the warm-up, patients again reached out to the targets on the circle to a metronome beat, first at a faster rate (240 beats/min) and then more slowly to the pace of the initial warm-up (60 beats/min). The same standardized home-based exercise program as provided to the control group was to be performed up to twice a day, and compliance was monitored with a self-reporting exercise diary. The exercise sets increased as the patient’s condition improved.
2.4. Data analysis
Pre- and post-treatment differences in ROM, strength, pain and disability (SPADI), and quality of life (WORC) scores were compared between the Wii and control groups. Because all measures violated the normality assumption of the Student t-test, the Wilcoxon signed-rank test was used. For several Wilcoxon tests, data are pooled across sub-measures or muscle groups. Although these pooled-data tests violate independence, they nevertheless provide a measure of overall change that is of particular interest when statistical power would otherwise be too low to detect performance differences. We used the Wilcoxon rank-sum test for comparing groups. P < 0.05 was considered statistically significant.
3. Results
Table 2 shows the characteristics of patients that completed the study. The treatment groups did not differ in SPADI scores for pain and disability or WORC scores for quality of life (P > 0.05). After treatment, both groups showed a decrease in pain and disability (Fig. 2), which was statistically significant only for the Wii group (total SPADI score P = 0.03). The Wii group showed a significant improvement in all WORC quality of life scores after treatment (composite score, P =0.015; Fig. 3), but the difference in the conventional treatment (control) group was not statistically significant (P > 0.05). By pooling data across subscales of the SPADI and WORC, we found significant overall differences in the WORC score after treatment for both the Wii (P < 0.05) and control groups (P = 0.002) and in the SPADI for the Wii group only (P = 0.001).
Table 2.
Patient characteristics.
| Patients | Age | Group | Affected Side | Provocative testsa | Symptom durationb | MRI resultsc |
|---|---|---|---|---|---|---|
| 1 | 27 | Wii | L | H(+), N(−), EC(−) | Subacute | Minimal anterolateral supraspinatus tendinosis; supraspinatus hypertrophy; type I acromion; mild-moderate AC joint osteoarthritis with bony spurs; small joint effusion with accompanying fluid in subscapularis recess |
| 2 | 31 | Wii | L | H(−), N(−), EC(+) | Chronic | Mild supraspinatus tendinosis; mild fatty atrophy teres minor; osseous lesion at humeral head; type I acromion is low lying; mild AC joint osteoarthritis with bony spurs; small effusion; old non-displaced left clavicular fracture |
| 3 | 73 | Wii | L | H(+), N(−), EC(+) | Chronic | Supra/infraspinatus tendinosis; mild AC joint arthritis; mild glenohumeral joint arthritis |
| 4 | 54 | Wii | L | H(+), N(−), EC(+) | Subacute | Supraspinatus and subscapularis tendinosis; small glenohumeral effusion; mild subdeltoid-subacromial bursitis |
| 5 | 62 | Wii | R | H(+), N(+), EC(+) | Chronic | Not available |
| 6 | 51 | Wii | L | H(+), N(+), EC(+) | Subacute | Not available |
| 7 | 64 | Wii | L | H(+), N(+), EC(+) | Chronic | Posterolateral supraspinatus and lateral subscapularis tendinpathy/tendinosis; type I acromion with inferolateral tilt; small joint effusion with fluid in subscapularis recess |
| 8 | 56 | Wii | L | H(+), N(+), EC(+) | Chronic | Posterolateral supraspinatus and lateral subscapularis tendinopathy; type I acromion with inferolateral tilt; small joint effusion with fluid in subscapularis recess |
| 9 | 70 | Con | R | H(+), N(+), EC(+) | Chronic | Partial thickness supraspinatus tear, biceps tendinosis, AC joint osteoarthritis |
| 10 | 76 | Con | L | H(+), N(+), EC(+) | Chronic | Moderate lateral supraspinatus tendinosis with possible partial tear at mediolateral tendon; mild lateral infraspinatus tendinosis; type I acromion with inferolateral tilt; moderate AC joint osteroarthritis with spurs; moderate tendinosis long head of biceps with fluid; small joint effusion with fluid in subscapular recess and rotator interval; mild subacromial/subdeltoid bursitis |
| 11 | 38 | Con | R | H(+), N(+), EC(−) | Chronic | Not available |
Provocative tests: H: Hawkin’s test; N: Neer’s test; EC: Empty Can test.
Symptom duration was defined as acute, < 1 month; subacute, 1–6 months; chronic, > 6 months.
Results of clinical MRI of the affected shoulder obtained before enrollment.
Fig. 2.
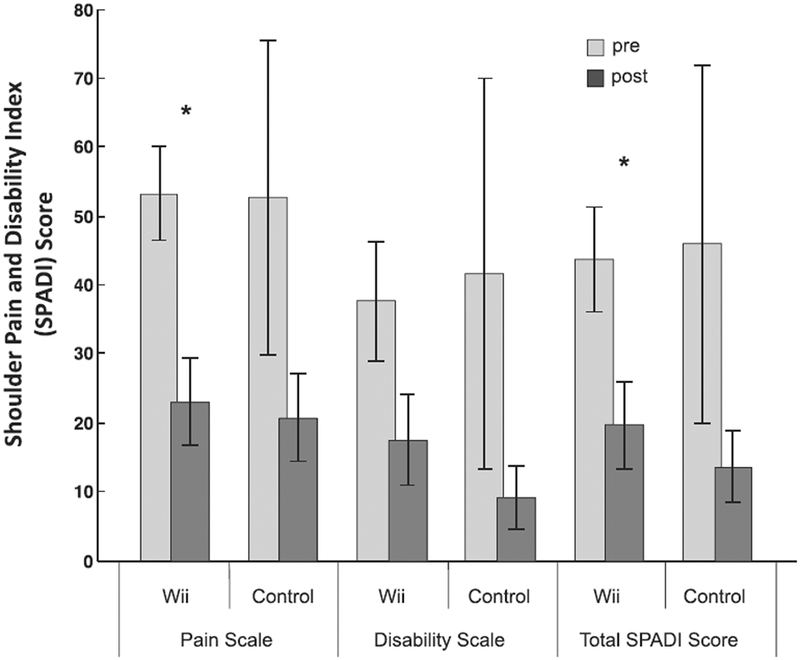
Shoulder Pain and Disability Index (SPADI) scores pre- and post-treatment for the Wii and conventional treatment groups. Data are mean ± SD. *P < 0.05.
Fig. 3.
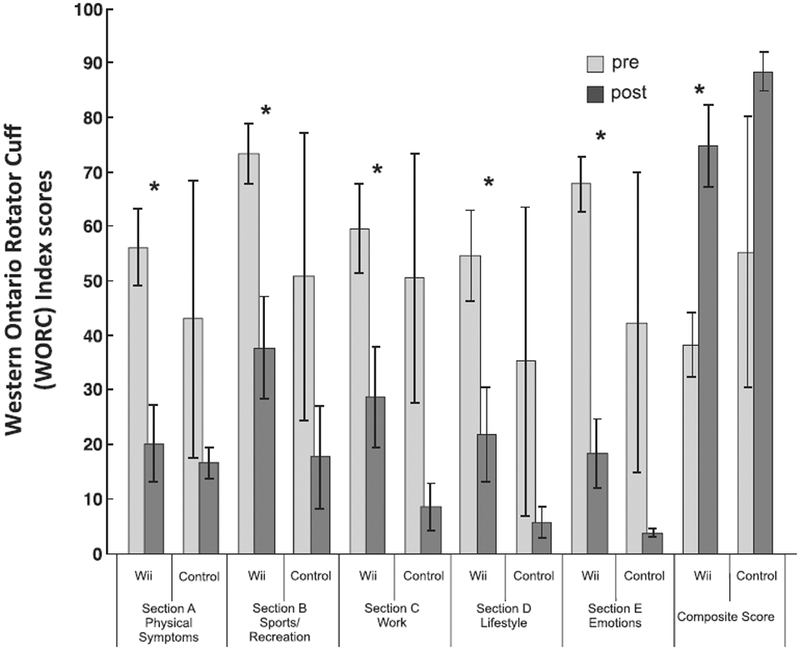
Western Ontario Rotator Cuff (WORC) scores pre- and post-treatment for the Wii and conventional treatment groups. Data are mean ± SD. *P < 0.05.
Before treatment, the 2 groups did not differ in maximum, active, pain-free, shoulder ROM in the sagittal and frontal planes, although ROM in the horizontal plane was greater for the Wii than control group (Fig. 4). Post-treatment, the Wii group showed a significant increase in ROM in the frontal plane (121.3–141.8°; P < 0.0016) and a marginal increase in ROM in the sagittal plane (139.4–156.1°; P = 0.055), but the conventional therapy group showed no significant increases in ROM (all P > 0.05). By pooling all ROM measures, we found a significant overall increase in ROM for the Wii group (P = 0.0014) but not for the control group (P > 0.05).
Fig. 4.

Shoulder range of motion (ROM) in degrees in the sagittal, frontal and horizontal planes pre- and post-treatment for the Wii and conventional treatment groups. Data are mean ± SD. *P < 0.05.
Before treatment, strength of the external rotators was weaker for the control than the Wii group (P = 0.024). After treatment, neither group showed significant changes in muscle strength in any of the 3 muscle groups (all P > 0.05, Fig. 5), although pooling data over all measures showed a significant increase in strength for the control group (P = 0.03) but not for the Wii group (P > 0.05).
Fig. 5.

Muscle strength of the scapular stabilizers, internal rotators and external rotators pre- and post-treatment for the Wii and conventional treatment groups. Data are mean ± SD.
4. Discussion
This pilot randomized controlled trial tested the feasibility and efficacy of using a structured Wii protocol to improve ROM, strength, and quality of life in patients with SIS. The protocol improved pain and disability, quality of life, and pain-free shoulder ROM in the sagittal and frontal planes but not strength. The structured Wii protocol we used in the treatment of SIS led to a higher rate of compliance relative to conventional treatment.
4.1. Gaming as therapy
“Gamification” of therapy has been shown to increase enjoyment and motivation and can increase adherence to rehabilitation programs [37]. In our study, patients randomized to the Wii group may have been more easily immersed in therapy because of the inherently entertaining nature of the games. By contrast, conventional therapy tends to be repetitive and may be tedious for patients not interested in exercise. Executing dynamic shoulder movements while playing a game may not be considered repetitive but rather a pleasurable experience. In addition, patients may have benefited from visual feedback from the avatar and tracking of repetitions, which could have reinforced performance and maximized training effort [50]. However excessive immersion in a game and focus on improving scores can also lead to excessive strain and disregard for how the movements are actually performed [51]. This situation has been shown to contribute to injury [52]. None of the patients were injured while using the Wii in this study, which suggests that deconstructing a game to train specific movements as part of a structured protocol can enhance training while preserving the enjoyment, immersion and compliance that result from gaming.
4.2. Structured gaming led to improved ROM
The improvement in subjective measures of pain and disability and quality of life after Wii training were not surprising, but the improvement in ROM measured objectively in 2 of the 3 planes assessed is notable. The structured Wii protocol progressively increased the use of specific movements at the shoulder during gaming. For example, the bowling game required shoulder retraction followed by protraction in the sagittal plane. The improvements in ROM may be attributed to the logical, stepwise advancement of isolated movements needed for shoulder mobility. Early scapular stabilization, as highlighted in this exercise program, is essential for rehabilitation in SIS [23]. Gliding, arclike movements, as performed during arm retraction while bowling, have been shown to be ideal for joint surface health because the articular surfaces are appropriately bathed in synovial fluid [48]. The gliding movements performed within a physiologic range, combined with distraction from the gaming elements of training may have helped facilitate the increased ROM in the sagittal and frontal planes [53]. The lack of significant improvement in the horizontal plane for shoulder internal and external rotation may have been due to a less-than-ideal game in the current system for promoting this specific ROM.
However, muscle strength did not improve with the Wii protocol, perhaps because the patients were not particularly weak - patients in the control group were weaker than those in the Wii group. As well, the Wii protocol did not provide the resistance that is typically provided in conventional therapy to increase strength. The Wii controllers are light-weight (Controller 0.21 kg and Nunchuk 0.18 kg) and designed primarily to facilitate a wide range of movements. Adding weights to the controllers may improve the strength of specific muscle groups during gaming. Additionally, resistive bands or the use of weights strapped on the wrist or forearms could increase resistance without modifying the weight of the controller to create a more comprehensive Wii-habilitation platform for therapy.
4.3. Limitations
The results are limited by the small sample size, 50% attrition in the control group, and a pseudo-randomized sampling technique with pre-treatment differences in strength between the 2 groups. The results were also limited by the nature of the gaming system implemented for the Wii protocol: the games leveraged to simulate functional ROM were restricted to the platform that is currently commercially available. Additionally, the digital scale used for strength assessment was not a validated medical device. Finally, our ROM analysis was limited to 2-D video analysis. In the future, we plan to implement 3-D motion tracking and incorporate functional movements during assessment of shoulder movements, as differences have been shown between scapular kinematics during constrained and functional movements [54,55].
4.4. Conclusions
This pilot study revealed that a structured Wii protocol could be a viable adjunct for improving pain, disability, quality of life and pain-free active ROM in patients with SIS. Gaming may confer a supplemental benefit by increasing motivation, pleasure, and/or therapy adherence. Protocol modifications to add resistance to improve strength may be warranted. Further investigations are needed to test this protocol in larger cohorts and to explore its value in reducing the burden of disability from shoulder pain.
Acknowledgements
The authors are grateful to Alexandra Reingold, Dr. Candice Burnette, and Dr. Errold Reid Jr. for their assistance with the study.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.rehab.2016.10.004.
Footnotes
Disclosure of interest
The authors declare that they have no competing interest.
References
- [1].Linsell L, Dawson J, Zondervan K, Rose P, Randall T, Fitzpatrick R, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology (Oxford) 2006;45:215–21. [DOI] [PubMed] [Google Scholar]
- [2].Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. J Hand Ther 2004;17:152–64. [DOI] [PubMed] [Google Scholar]
- [3].Meislin RJ, Sperling JW, Stitik TP. Persistent shoulder pain: epidemiology, pathophysiology, and diagnosis. Am J Orthop 2005;34:5–9. [PubMed] [Google Scholar]
- [4].Jacobs JJ, King TR, Klippel JH, Berven SH, Burr DB, Caskey PM, et al. Beyond the decade: strategic priorities to reduce the burden of musculoskeletal disease. J Bone Joint Surg Am 2013;95:e1251–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].van der Windt DA, Koes BW, de Jong BA, Bouter LM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis 1995;54:959–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fu FH, Harner CD, Klein AH. Shoulder impingement syndrome. A critical review. Clin Orthop Relat Res 1991;269:162–73. [PubMed] [Google Scholar]
- [7].Lo YP, Hsu YC, Chan KM. Epidemiology of shoulder impingement in upper arm sports events. Br J Sports Med 1990;24:173–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders of the shoulder - a systematic review of the literature. Scand J Work Environ Health 2010;36:189–201. [DOI] [PubMed] [Google Scholar]
- [9].Linaker CH, Walker-Bone K. Shoulder disorders and occupation. Best Pract Res Clin Rheumatol 2015;29:405–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hsiao MS, Cameron KL, Tucker CJ, Benigni M, Blaine TA, Owens BD. Shoulder impingement in the United States military. J Shoulder Elbow Surg 2015. [DOI] [PubMed] [Google Scholar]
- [11].Seitz AL, McClure PW, Lynch SS, Ketchum JM, Michener LA. Effects of scapular dyskinesis and scapular assistance test on subacromial space during static arm elevation. J Shoulder Elbow Surg 2012;21:631–40. [DOI] [PubMed] [Google Scholar]
- [12].Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med 2013;47:877–85. [DOI] [PubMed] [Google Scholar]
- [13].Timmons MK, Thigpen CA, Seitz AL, Karduna AR, Arnold BL, Michener LA. Scapular kinematics and subacromial-impingement syndrome: a meta-analysis. J Sport Rehabil 2012;21:354–70. [DOI] [PubMed] [Google Scholar]
- [14].Graichen H, Stammberger T, Bonel H, Wiedemann E, Englmeier KH, Reiser M, et al. Three-dimensional analysis of shoulder girdle and supraspinatus motion patterns in patients with impingement syndrome. J Orthop Res 2001;19:1192–8. [DOI] [PubMed] [Google Scholar]
- [15].McClure PW, Michener LA, Karduna AR. Shoulder function and 3-dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther 2006;86:1075–90. [PubMed] [Google Scholar]
- [16].McMahon PJ, Debski RE, Thompson WO, Warner JJ, Fu FH, Woo SL. Shoulder muscle forces and tendon excursions during glenohumeral abduction in the scapular plane. J Shoulder Elbow Surg 1995;4:199–208. [DOI] [PubMed] [Google Scholar]
- [17].Escamilla RF, Andrews JR. Shoulder muscle recruitment patterns and related biomechanics during upper extremity sports. Sports Med 2009;39:569–90. [DOI] [PubMed] [Google Scholar]
- [18].Blanche DW. Injuries of the musculotendinous cuff of the shoulder. CalifMed 1953;79:20–4. [PMC free article] [PubMed] [Google Scholar]
- [19].Bechtol CO. Biomechanics ofthe shoulder. Clin Orthop RelatRes 1980;146:37–41. [PubMed] [Google Scholar]
- [20].Perry J. Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics, and tennis. Clin Sports Med 1983;2:247–70. [PubMed] [Google Scholar]
- [21].Herrera JE, Stubblefield MD. Rotator cuff tendonitis in lymphedema: a retrospective case series. Arch Phys Med Rehabil 2004;85:1939–42. [DOI] [PubMed] [Google Scholar]
- [22].Labriola JE, Lee TQ, Debski RE, McMahon PJ. Stability and instability of the glenohumeral joint: the role of shoulder muscles. J Shoulder Elbow Surg 2005;14:32s–8s. [DOI] [PubMed] [Google Scholar]
- [23].Escamilla RF, Yamashiro K, Paulos L, Andrews JR. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Med 2009;39:663–85. [DOI] [PubMed] [Google Scholar]
- [24].Gagey O, Hue E. Mechanics of the deltoid muscle. A new approach. Clin Orthop Relat Res 2000;375:250–7. [DOI] [PubMed] [Google Scholar]
- [25].Smith-Forbes EV, Moore-Reed SD,Westgate PM, Kibler WB, Uhl TL. Descriptive analysis of common functional limitations identified by patients with shoulder pain. J Sport Rehabil 2015;24:179–88. [DOI] [PubMed] [Google Scholar]
- [26].Giphart JE, van der Meijden OA, Millett PJ. The effects of arm elevation on the 3-dimensional acromiohumeral distance: a biplane fluoroscopy study with normative data. J Shoulder Elbow Surg 2012;21:1593–600. [DOI] [PubMed] [Google Scholar]
- [27].Cailliet R. Shoulder pain. Philadelphia, PA: F.A. Davis Co; 1991. [Google Scholar]
- [28].Bennell K, Coburn S, Wee E, Green S, Harris A, Forbes A, et al. Efficacy and cost-effectiveness of a physiotherapy program for chronic rotator cuff pathology: a protocol for a randomised, double-blind, placebo-controlled trial. BMC Musculoskelet Disord 2007;8:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kromer TO, de Bie RA, Bastiaenen CH. Effectiveness of individualized physiotherapy on pain and functioning compared to a standard exercise protocol in patients presenting with clinical signs of subacromial impingement syndrome. A randomized controlled trial. BMC Musculoskelet Disord 2010;11:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].van der Meijden OA, Westgard P, Chandler Z, Gaskill TR, Kokmeyer D, Millett PJ. Rehabilitation after arthroscopic rotator cuff repair: current concepts review and evidence-based guidelines. Int J Sports Phys Ther 2012;7:197–218. [PMC free article] [PubMed] [Google Scholar]
- [31].Roddy E, Zwierska I, Hay EM,Jowett S, Lewis M, Stevenson K, et al. Subacromial impingement syndrome and pain: protocol for a randomised controlled trial of exercise and corticosteroid injection (the SUPPORT trial). BMC Musculoskelet Disord 2014;15:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ellenbecker TS, Cools A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: an evidence-based review. Br J Sports Med 2010;44:319–27. [DOI] [PubMed] [Google Scholar]
- [33].Holmgren T, Bjornsson Hallgren H, Oberg B, Adolfsson L, Johansson K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. BMJ 2012;344:e787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Friedrich M, Gittler G, Halberstadt Y, Cermak T, Heiller I. Combined exercise and motivation program: effect on the compliance and level of disability of patients with chronic low back pain: a randomized controlled trial. Arch Phys Med Rehabil 1998;79:475–87. [DOI] [PubMed] [Google Scholar]
- [35].Alexandre NM, Nordin M, Hiebert R, Campello M. Predictors of compliance with short-term treatment among patients with back pain. Rev Panam Salud Publica 2002;12:86–94. [DOI] [PubMed] [Google Scholar]
- [36].Petersen T, Larsen K, Jacobsen S. One-year follow-up comparison of the effectiveness of McKenzie treatment and strengthening training for patients with chronic low back pain: outcome and prognostic factors. Spine (Phila Pa 1976) 2007;32:2948–56. [DOI] [PubMed] [Google Scholar]
- [37].Ravenek KE, Wolfe DL, Hitzig SL. A scoping review of video gaming in rehabilitation. Disabil Rehabil Assist Technol 2015;1–9. [DOI] [PubMed] [Google Scholar]
- [38].Jalink MB, Heineman E, Pierie JP, Hoedemaker ten Cate HO. Nintendo related injuries and other problems: review. BMJ 2014;349:g7267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Norris BS, Olson SL. Concurrent validity and reliability of two-dimensional video analysis of hip and knee joint motion during mechanical lifting. Physiother Theory Pract 2011;27:521–30. [DOI] [PubMed] [Google Scholar]
- [40].Ugbolue UC, Papi E, Kaliarntas KT, Kerr A, Earl L, Pomeroy VM, et al. The evaluation of an inexpensive, 2D, video based gait assessment system for clinical use. Gait Posture 2013;38:483–9. [DOI] [PubMed] [Google Scholar]
- [41].Paul JC, Petrizzo A, Rizzo JR, Bianco K, Maier S, Errico TJ, et al. Feasibility of a cost-effective, video analysis software-based mobility protocol for objective spine kinematics and gait metrics: a proof of concept study. PM R 2015;7:336–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res 1991;4:143–9. [PubMed] [Google Scholar]
- [43].Ludewig PM, Borstad JD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occup Environ Med 2003;60:841–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kirkley A, Alvarez C, Griffin S. The development and evaluation of a diseasespecific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med 2003;13:84–92. [DOI] [PubMed] [Google Scholar]
- [45].Alvarez CM, Litchfield R, Jackowski D, Griffin S, Kirkley A. A prospective, double-blind, randomized clinical trial comparing subacromial injection of betamethasone and xylocaine to xylocaine alone in chronic rotator cuff tendinosis. Am J Sports Med 2005;33:255–62. [DOI] [PubMed] [Google Scholar]
- [46].de Witte PB, Henseler JF, Nagels J, Vliet Vlieland TP, Nelissen RG. The Western Ontario rotator cuff index in rotator cuff disease patients: a comprehensive reliability and responsiveness validation study. Am J Sports Med 2012;40:1611–9. [DOI] [PubMed] [Google Scholar]
- [47].Longo UG, Saris D, Poolman RW, Berton A, Denaro V. Instruments to assess patients with rotator cuff pathology: a systematic review of measurement properties. Knee Surg Sports Traumatol Arthrosc 2012;20: 1961–70. [DOI] [PubMed] [Google Scholar]
- [48].McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther 2004;84:832–48. [PubMed] [Google Scholar]
- [49].Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983;16:87–101. [DOI] [PubMed] [Google Scholar]
- [50].Dahl-Popolizio S, Loman J, Cordes CC. Comparing outcomes of kinect videogame-based occupational/physical therapy versus usual care. Games Health J 2014;3:157–61. [DOI] [PubMed] [Google Scholar]
- [51].Sparks DA, Coughlin LM, Chase DM. Did too much Wii cause your patient’s injury? J Fam Pract 2011;60:404–9. [PubMed] [Google Scholar]
- [52].Sparks D, Chase D, Coughlin L. Wii have a problem: a review of self-reported Wii related injuries. Inform Prim Care 2009;17:55–7. [DOI] [PubMed] [Google Scholar]
- [53].Parry IS, Bagley A, Kawada J, Sen S, Greenhalgh DG, Palmieri TL. Commercially available interactive video games in burn rehabilitation: therapeutic potential. Burns 2012;38:493–500. [DOI] [PubMed] [Google Scholar]
- [54].Amasay T, Karduna AR. Scapular kinematics in constrained and functional upper extremity movements. J Orthop Sports Phys Ther 2009;39:618–27. [DOI] [PubMed] [Google Scholar]
- [55].Roren A, Lefevre-Colau MM, Roby-Brami A, Revel M, Fermanian J, Gautheron V, et al. Modified 3D scapular kinematic patterns for activities of daily living in painful shoulders with restricted mobility: a comparison with contralateral unaffected shoulders. J Biomech 2012;45:1305–11. [DOI] [PubMed] [Google Scholar]


