Abstract
The objective of this study was to determine whether the interaction between type of serious mental illness (SMI) and pre-treatment drinking severity, assessed by ethyl glucuronide (EtG), predicts EtG-positive urine samples submitted during treatment in outpatients with co-occurring alcohol dependence and SMI. Seventy-nine participants were randomized to treatment-as-usual or treatment-as-usual and contingency management (CM) targeting alcohol abstinence. Generalized estimating equations were used to assess the interaction of pre-treatment drinking (heavy drinking or light drinking) and SMI diagnosis (major depression, bipolar, or schizophrenia-spectrum disorders) across a 12-week treatment period. In the overall sample, the interaction of drinking severity and SMI diagnosis (p = 0.006) was associated with alcohol abstinence. Exploratory analyses of the interaction term among participants randomized to CM (n = 40; p = 0.008) were associated with alcohol abstinence during CM. Type of SMI diagnosis was associated with treatment outcomes in individuals who engaged in heavy drinking, but not light drinking, prior to treatment.
Keywords: Serious mental illness, Co-occurring disorders, Alcohol treatment, Ethyl glucuronide, Heavy drinking, Contingency management
Nearly 50% of people with serious mental illness (SMI), defined as schizophrenia-spectrum, bipolar, and recurrent major depressive disorders experience a co-occurring alcohol use disorder in their lifetimes (Davis et al. 2008; Koskinen et al. 2009; Regier et al. 1990). These individuals have high levels of psychotic symptoms, inpatient psychiatric and emergency care utilization, treatment dropout, and suicide as a result of co-occurring disorders (Buckley and Brown 2006; Gonzalez et al. 2007; Kreyenbuhl et al. 2009; McGovern et al. 2007). Various behavioral treatments (e.g., cognitive behavior therapy, contingency management (CM)) or a combination of treatments are associated with reductions in alcohol and drug use in adults with SMI (Barrowclough et al. 2010; Bellack et al. 2006; Bradizza et al. 2014; McDonell et al. 2013, 2017). However, less is known about the predictors of treatment outcomes in those receiving co-occurring disorder treatment for alcohol and schizophrenia-spectrum, bipolar I and II, or major depressive disorders.
CM provides reinforcers for targeted behavior, typically abstinence verified by urine drug tests, and is associated with decreased substance use, psychiatric symptoms, and hospitalization in outpatients diagnosed with an SMI (Bellack et al. 2006; McDonell et al. 2013, 2017). In two randomized trials of CM, one targeting stimulant drug use and the other alcohol use, pre-treatment alcohol or drug positive urine tests were associated with poor treatment outcomes (Angelo et al. 2013). In a trial of CM targeting alcohol use, participants submitted urine samples that were tested for ethyl glucuronide (EtG), an alcohol metabolite, for 4 weeks before randomization. Participants who had pre-randomization EtG levels consistent with regular heavy drinking (EtG > 499 ng/mL) attained a period of alcohol abstinence during CM that was 2.5 times shorter than those who were light drinkers (McDonell et al. 2017).
Findings have been inconsistent in terms of the association between type of SMI diagnosis and treatment outcomes. We observed that higher levels of psychological distress (e.g., anxiety, stress), rather than type of SMI diagnosis was a predictor of abstinence among adults with SMI receiving CM for stimulant use (Angelo et al. 2013). In non-SMI populations, depressive symptoms were associated with poorer treatment outcomes in CM for cocaine dependence (García-Fernández et al. 2013). Another study found that the diagnosis of major depression or antisocial personality disorder predicted poorer treatment outcomes at 1-year follow-up among adults in drug treatment (Compton et al. 2003).
Pre-treatment substance use and psychiatric symptom severity have been independently associated with treatment outcomes in CM, and initial evidence suggests that type of psychiatric diagnosis is associated with addiction treatment outcomes. However, to our knowledge no research has tested whether the interaction of these variables predicts addiction treatment outcomes. Understanding how the heterogeneity in alcohol use and SMI diagnosis interact could provide clinicians with valuable information to improve and tailor treatment for subgroups of adults with co-occurring disorders. The purpose of this study was to explore whether the interaction of pre-treatment drinking severity (heavy versus light drinking) assessed by EtG and type of SMI diagnosis (major depression, bipolar, or schizophrenia-spectrum disorders) predicted alcohol abstinence in the overall sample of adults with SMI and AUDs receiving treatment-as-usual (TAU; N = 79), as well as in those randomized to CM (n = 40).
Methods
Sample
Participants were recruited from multiple community mental health and substance use treatment agencies in Washington State. Seventy-nine adults who met criteria for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) diagnoses of alcohol dependence and co-occurring schizophrenia-spectrum (n = 29), bipolar (n = 24), or major depressive disorders (n = 27), assessed by the Mini International Neuro-psychiatric Interview (M.I.N.I) were enrolled (Sheehan et al. 1998). Other inclusion criteria (detailed in McDonell et al. 2017) included alcohol use on 5 out of the prior 30 days. The mean age of participants was 45.38 (SD = 10.20) years, and 65% (n = 51) were male, 53% (n = 42) were white, 29% (n = 23) black, 15% (n = 12) other, and 3% (n = 2) of unknown racial identify. Fifty-three percent (n = 42) were heavy drinkers as defined by pre-treatment EtG levels. Participants provided written informed consent and the study was approved by the University of Washington’s Institutional Review Board.
Study Design and Procedures
McDonell et al. (2017) conducted a 16-week randomized controlled trial of CM for alcohol dependence (clinicaltrials.govidentifier:NCT01567943). Participants engaged in a 4-week induction period (weeks 1–4), developed to increase study retention after randomization that included treatment-as-usual(TAU). Participants received reinforcers (prize draws) three times a week for submitting urine samples regardless of whether it was positive or negative and for alcohol and provided self-reported data on alcohol use. After the induction period, participants who provided at least one EtG-positive urine sample continued to receive TAU and were randomized (weeks 5–16) to either the CM (n = 40) or non-contingent (NC; n = 39) control conditions for the 12-week treatment period. Following the treatment period, participants completed a 3-month follow-up (weeks 17–28) period.
Study Interventions
TAU occurred at three sites of a large urban community mental health center in Seattle, WA. Addiction treatment consisted of group counseling sessions 2–4 times a week. Additional services were provided by site staff, including individual addiction counseling, case management, medication management, and housing support.
The variable magnitude of reinforcement procedure was utilized and involved “prize draws” from a bucket that contained tokens that reflected various values. Fifty percent of the tokens read “good job,” 41.8% read “small” ($1 value), 8.0% read “large” ($20 value), and 0.2% read “jumbo” ($80 value). NC control participants earned at least three prize draws per urine sample submitted regardless of results, and CM participants earned prize draws for each EtG-negative sample submitted and an additional draw for each consecutive week of abstinence. EtG-positive urine tests resulted in no prize draws and a reset to three prize draws the next time an EtG-negative sample was provided. CM participants also received gift cards if they attended some ($5) or all ($10) of their addiction treatment groups each week. NC control participants received the average value of gift cards received by the CM condition regardless of addiction treatment group attendance.
Measures
Participants completed an enrollment interview that included the M.I.N.I., which was used to determine type of SMI diagnosis and assess for alcohol dependence and drug use disorders. M.I.N.I. major depressive episode, manic episode, psychotic disorders, and drug and alcohol dependence/abuse diagnostic sections were administered by trained research staff. Urine samples were collected at each study visit and assessed for EtG using Diagnostic Reagents Incorporated EtG-immunoassay onsite with a Thermo Fisher Indiko analyzer (Fremont, CA), with a detectable range of 0 to 2000 ng/mL. Mean EtG levels were calculated across the 4-week induction period for each participant to determine pre-treatment drinking severity, those with EtG >499ng/mL (i.e., heavy drinking) or EtG <500 ng/mL (i.e., light drinking) (McDonell et al. 2015). The outcome variable was number of EtG-positive (EtG > 149 ng/mL) urine samples submitted during the 36-visit treatment period.
Data Analysis
Generalized estimating equation (GEE) analyses were used to assess the relationship variables of interest and alcohol use during the 12-week treatment period. The first model (N = 79) controlled for treatment condition, SMI diagnosis (schizophrenia-spectrum, bipolar, major depressive disorders), pre-treatment drinking severity, and the interaction between type of SMI diagnosis and pre-treatment drinking severity with the outcome being EtG-positive urine samples during treatment (1 = yes, 0 = no). The second model within the CM condition only (n = 40) assessed whether the interaction of pre-treatment drinking severity and SMI diagnosis was associated with EtG-positive urine samples, controlling for pre-treatment drinking severity and SMI diagnosis. In both analyses, all possible pairwise comparisons were conducted on the interaction term utilizing Bonferroni correction to avoid inflation of the alpha rate. Odds ratios (OR) were reported, 95% confidence intervals (CI), and significance was set at p < 0.05. Analyses were performed using IBM SPSS 24.0 and post hoc tests were conducted in Stata 12.0 (StataCorp, College Station, TX).
Results
Across the entire sample, after controlling for treatment conditions (χ2 (1) = 7.86, p = 0.005), pre-treatment drinking severity (χ2 (1) = 38.55, p = 0.001), and SMI diagnosis (χ2 (2) = 7.64, p = 0.022), the interaction of pre-treatment drinking severity and SMI diagnosis (χ2 (2) = 10.39, p = 0.006) was a significant predictor of submitting EtG-positive urine samples during the treatment period.
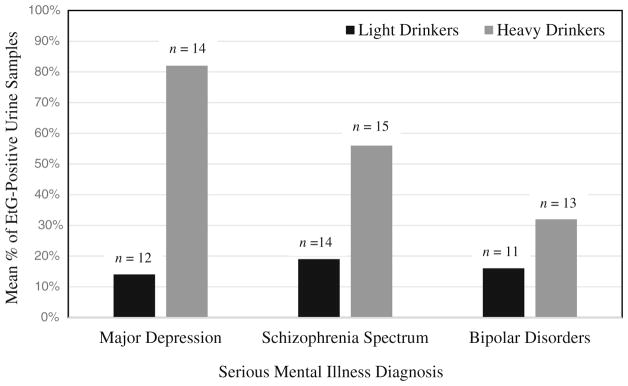
Post hoc tests for the interaction term revealed that heavy drinkers with bipolar disorders (OR = 0.09, 95% CI 0.04–0.22) and schizophrenia-spectrum disorders (OR = 0.25, 95% CI 0.11–0.58) were less likely than heavy drinkers with major depression to submit EtG-positive urine samples during the treatment period. Heavy drinkers with schizophrenia-spectrum disorders were 2.83 times (95% CI 1.32–6.09) more likely than heavy drinkers with bipolar disorder to submit EtG-positive urine samples during the treatment period (see Fig. 1). No significant differences were found among light drinkers across SMI diagnoses. Although, among those with major depression (OR = 29.28, 95% CI 10.53–81.45) and schizophrenia-spectrum (OR = 5.62, 95% CI 2.37–13.35) disorders, heavy drinkers were more likely than light drinkers to submit EtG-positive samples during treatment. Differences between heavy and light drinkers in those with bipolar were not significant.
Fig. 1.
Mean percentage of ethyl glucuronide (EtG)-positive urine samples during treatment across heavy and light drinkers and serious mental illness diagnoses (N = 79). Note: EtG, ethyl glucuronide; significance of main effects: pre-treatment drinking severity (p = 0.001) and SMI diagnosis (p = 0.022)
Similar findings were observed when analyses were conducted on participants randomized to CM only. After controlling for pre-treatment drinking severity (χ2 (1) = 23.41, p = 0.001) and SMI diagnosis (χ2 (2) = 2.07, p = 0.36), the interaction of pre-treatment drinking severity and SMI diagnosis (χ2 (2) = 9.72, p = 0.008) was associated with EtG-positive urine samples during the treatment period. Bonferroni post hoc tests, conducted on the interaction term revealed that heavy drinkers with bipolar (OR = 0.13, 95% CI 0.03–0.47) and schizophrenia-spectrum (OR = 0.13, 95% CI 0.03–0.47) disorders were less likely than heavy drinkers with major depression to submit EtG-positive urine samples during the treatment period. No significant differences were found among light drinkers across SMI diagnoses. However, among those with major depression (OR = 87.02, 95% CI 17.08–443.23) and schizophrenia-spectrum (OR = 5.57, 95% CI 1.52–20.45) disorders, heavy drinkers were more likely than light drinkers to submit EtG-positive samples during treatment. Differences between heavy and light drinkers in those with bipolar were not significant.
Discussion
Previous findings have suggested that light drinkers relative to heavy drinkers were significantly less likely to submit EtG-positive urine samples during the treatment period and that psychiatric distress rather than SMI diagnosis predicted outcomes (Angelo et al. 2013; McDonell et al. 2017). Although not a CM trial, research has revealed that individuals with a major depression diagnosis were more likely to meet criteria for alcohol dependence compared to other psychiatric disorders(Compton et al. 2003). Contrary to previous research that found psychiatric distress not SMI was a significant predictor of outcomes, our study found that alcohol use during the treatment period varied by SMI diagnosis in heavy, but not light drinkers, as seen in Fig. 1. Heavy drinkers with major depression were more likely to submit EtG-positive urine samples during treatment compared to heavy drinkers with bipolar and schizophrenia-spectrum disorders. Similar results were also found when analyses were restricted to the CM condition only. In contrast, outcomes did not differ across SMI diagnoses in light drinkers.
Results suggest that the heterogeneity of both alcohol use and psychiatric diagnosis are important predictors of treatment out comes in adults with co-occurring disorders. While a number of frameworks for conceptualizing heterogeneity of substance use and psychiatric disorders have been proposed (McGovern et al. 2007; Ries 1993), our findings suggest that simple tools, such as urine tests for EtG and psychiatric diagnosis, can be used to identify who is likely to respond to TAU and CM. The implications from this study in addition to findings from our other study (Oluwoye et al., Under Review) examining the differences in treatment outcomes among individuals with stimulant use disorders and various SMIs (i.e., schizophrenia, bipolar, and major depressive disorders) suggest that personalized treatment approaches should be tailored to specific SMI diagnosis and substance use severity among adults with co-occurring disorders.
The relatively small sample size of this study, particularly when analyzing outcomes in the CM group, resulted in small numbers of individuals in specific groups (e.g., light drinkers with depression). Therefore, it is possible that outliers may have influenced results. Participant recruitment from one treatment facility may also limit the generalizability of study findings. Replication of our findings in a larger sample recruited across multiple agencies is needed. While it is possible that diagnostic errors could have occurred, we used a structured diagnostic interview and other procedures including the use of trained research staff to assure accuracy of diagnosis.
Conclusions
Findings provide initial evidence that the interaction between drinking severity and psychiatric diagnosis, rather than the effect of each of these variables in isolation, is important when predicting alcohol treatment response in those who suffer from co-occurring disorders. If validated in larger samples, this finding may have important implications for improving outcomes of heavy drinkers, especially those who suffer from co-occurring major depression.
Footnotes
Compliance with Ethical Standards
Informed Consent All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Disclosures OO, EL, JS, KH, DS, and MM have no disclosures to report. SM and JR have received research funding from the Bristol-Myers Squibb Foundation. SM has also received funding from the Orthopedic Specialty Institute. This funding is in no way related to the investigation reported here. SM and JR have no disclosures to report. RR has been on the speaker of bureaus of Janssen, Alkermes, and Reckitt Benckiser in the past 3 years but has no disclosures to report.
References
- Angelo FN, McDonell MG, Lewin MR, Srebnik D, Lowe J, Roll J, Ries R. Predictors of stimulant abuse treatment outcomes in severely mentally ill outpatients. Drug and Alcohol Dependence. 2013;131(1):162–165. doi: 10.1016/j.drugalcdep.2012.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrowclough C, Haddock G, Wykes T, Beardmore R, Conrod P, Craig T, et al. Integrated motivational interviewing and cognitive behavioural therapy for people with psychosis and comorbid substance misuse: randomised controlled trial. British Medical Journal (Clinical Research Ed) 2010;341:c6325. doi: 10.1136/bmj.c6325. https://doi.org/10.1136/bmj.c6325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellack AS, Bennett ME, Gearon JS, Brown CH, Yang Y. A randomized clinical trial of a new behavioral treatment for drug abuse in people with severe and persistent mental illness. Archives of General Psychiatry. 2006;63(4):426–432. doi: 10.1001/archpsyc.63.4.426. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR, Dermen KH. Behavioral interventions for individuals dually diagnosed with a severe mental illness and a substance use disorder. Current Addiction Reports. 2014;1(4):243–250. doi: 10.1007/s40429-014-0032-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley PF, Brown ES. Prevalence and consequences of dual diagnosis. The Journal of Clinical Psychiatry. 2006;67(7):1–1. doi: 10.4088/jcp.0706e01. [DOI] [PubMed] [Google Scholar]
- Compton WM, III, Cottler LB, Jacobs JL, Ben-Abdallah A, Spitznagel EL. The role of psychiatric disorders in predicting drug dependence treatment outcomes. American Journal of Psychiatry. 2003;160(5):890–895. doi: 10.1176/appi.ajp.160.5.890. [DOI] [PubMed] [Google Scholar]
- Davis L, Uezato A, Newell JM, Frazier E. Major depression and comorbid substance use disorders. Current Opinion in Psychiatry. 2008;21(1):14–18. doi: 10.1097/YCO.0b013e3282f32408. https://doi.org/10.1097/YCO.0b013e3282f32408. [DOI] [PubMed] [Google Scholar]
- García-Fernández G, Secades-Villa R, García-Rodríguez O, Peña-Suárez E, Sánchez-Hervás E. Contingency management improves outcomes in cocaine-dependent outpatients with depressive symptoms. Experimental and Clinical Psychopharmacology. 2013;21(6):482. doi: 10.1037/a0033995. [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, Bradizza CM, Vincent PC, Stasiewicz PR, Paas ND. Do individuals with a severe mental illness experience greater alcohol and drug-related problems? A test of the supersensitivity hypothesis. Addictive Behaviors. 2007;32(3):477–490. doi: 10.1016/j.addbeh.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Koskinen J, Löhönen J, Koponen H, Isohanni M, Miettunen J. Prevalence of alcohol use disorders in schizophrenia—a systematic review and meta-analysis. Acta Psychiatrica Scandinavica. 2009;120(2):85–96. doi: 10.1111/j.1600-0447.2009.01385.x. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J, Nossel IR, Dixon LB. Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: a review of the literature. Schizophrenia Bulletin. 2009;35(4):696–703. doi: 10.1093/schbul/sbp046. https://doi.org/10.1093/schbul/sbp046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonell MG, Srebnik D, Angelo F, McPherson S, Lowe JM, Sugar A, et al. Randomized controlled trial of contingency management for stimulant use in community mental health patients with serious mental illness. American Journal of Psychiatry. 2013;170(1):94–101. doi: 10.1176/appi.ajp.2012.11121831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonell MG, Skalisky J, Leickly E, McPherson S, Battalio S, Nepom JR, et al. Using ethyl glucuronide in urine to detect light and heavy drinking in alcohol dependent outpatients. Drug and Alcohol Dependence. 2015;157:184–187. doi: 10.1016/j.drugalcdep.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonell MG, Leickly E, McPherson S, Skalisky J, Srebnik D, Angelo F, et al. A randomized controlled trial of ethyl glucuronide-based contingency management for outpatients with co-occurring alcohol use disorders and serious mental illness. American Journal of Psychiatry. 2017;174:370–377. doi: 10.1176/appi.ajp.2016.16050627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Clark RE, Samnaliev M. Co-occurring psychiatric and substance use disorders: a multistate feasibility study of the quadrant model. Psychiatric Services. 2007;58(7):949–954. doi: 10.1176/ps.2007.58.7.949. [DOI] [PubMed] [Google Scholar]
- Oluwoye O, Hirchak K, Leickly E, Skalisky J, McPherson S, Srebnik D, Roll JM, Ries RK, McDonell MG. Co-occurring stimulant use disorders and serious mental illness associated with poor treatment outcomes. (Under Review) [PMC free article] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- Ries R. Clinical treatment matching models for dually diagnosed patients. Psychiatric Clinics of North America. 1993;16(1):167–175. [PubMed] [Google Scholar]
- Sheehan DV, Lecruibier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The miniinternational neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSMM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–57. [PubMed] [Google Scholar]