Abstract
Introduction
Lumbar discectomy patients with large annular defects are at a high risk for reherniation and reoperation, which could be mitigated through the use of an annular closure device (ACD). To identify the most effective treatment pathways for this high-risk population, it is critical to understand the clinical outcomes and socioeconomic costs among reoperated patients as well as the utility of ACD for minimizing reoperation risk.
Methods
This was a post hoc analysis of a prospective, multicenter, randomized controlled trial (RCT) designed to investigate the safety and efficacy of an ACD. All 550 patients (both ACD treated and control) from the RCT with follow-up data through 2 years were included in this analysis (69 reoperated and 481 non-reoperated). Reoperations were defined as any revision surgery of the index level, regardless of indication. Equivalent U.S. Medicare expenditures for reoperations were estimated through cost multipliers derived from the commercially available PearlDiver database.
Results
A significantly greater number of control patients (45/278; 16%) compared to ACD patients (24/272; 9%) underwent a revision surgery at the index level within 2 years of followup (p=0.01). At 2 years of follow-up, the reoperated patients had significantly worse Oswestry Disability Index scores and visual analog scale for leg and back pain scores compared to their non-reoperated counterparts (p<0.0001). The total estimated direct medical costs for reoperation were US $952,348 ($13,802 per reoperated patient), with control patients accounting for the majority of this cost burden ($565,188; 59%).
Conclusion
Post-discectomy reoperation is associated with significantly increased patient morbidity, missed work, and direct treatment costs in a population at high risk for reherniation. Annular closure helped minimize this clinical and socioeconomic burden by reducing the incidence of reoperation by nearly 50% (16% control vs 9% ACD).
Keywords: lumbar discectomy, annular closure device, patient-reported outcomes, direct costs, reherniation, reoperation
Introduction
Lumbar discectomy is a highly effective procedure to address back and leg pain associated with intervertebral disc herniation and is one of the most common spinal procedures globally. In the USA alone, the procedure is performed on nearly 500,000 patients per year.1 Retrospective studies have reported lumbar discectomy reoperation rates of 3%–21% to treat reherniation of the disc, loss of disc height, and/or accelerated degeneration.2–15 There are multiple patient factors that pose significant risk for reoperation, such as annular defect size, age, smoking status, as well as surgical technique.2,5,16–19 To this end, a large annular defect has been reported as a significant risk factor for reherniation and revision surgery.2,5,20,21 Recurrent herniation has been reported to range from 1% to 7% in patients with small annular defects (<6 mm) and 15%–27% in patients with large annular defects (≥6 mm).2,5,20,21 In one study, reoperation was required in only 1% of patients with small annular defects (<6 mm) vs 21% of patients with large annular defects (≥6 mm).5
Discectomy is generally a successful and cost-effective means of treatment for patients with herniated nucleus pulposus who do not respond well to conservative therapy.22–27 However, there is some controversy as to whether the clinical outcomes of reoperated patients reach the same level of success as patients who do not require revision surgery.11,16,28–34 Additionally, the costs associated with revision surgeries, associated therapies, and missed work pose a substantial socioeconomic burden.35–37 Therefore, annular closure devices (ACDs) have been developed to help avoid reherniation and reoperation, particularly in high-risk patients with large annular defects. Yet, further research is required to understand the extent of additional patient morbidity and costs for reoperated patients as well as the potential for an ACD to minimize the risk of reoperation. The aim of this study was to examine the patient-reported outcomes (PROs) and socioeconomic costs among reoperated patients following primary discectomy surgery as well as the utility of ACD for reducing the rates and associated burden of reoperation.
Methods
A prospective, multicenter, randomized controlled trial (RCT) (Clinicaltrials.gov ID: NCT01283438) was designed to examine the safety and efficacy of a novel ACD (Barricaid®; Intrinsic Therapeutics, Inc., Woburn, MA, USA) following standard limited discectomy vs limited discectomy alone for the treatment of high-risk patients with large annular defects (4–6 mm tall and 6–10 mm wide).
Patient sample
Patients who met the inclusion and exclusion criteria were randomly assigned intraoperatively 1:1 to limited discectomy (control) or limited discectomy followed by placement of the ACD (investigational group). The study was approved by the local ethics committee at each of the study sites and all patients provided written informed consent. Study enrollment took place across 21 international sites between December 2010 and October 2014. Please refer to Clinicaltrials.gov ID: NCT01283438 for a list of the study sites. Patients were stratified on an as-treated basis for the current analyses. Further details regarding this study rationale, design, and methods have been previously described.38
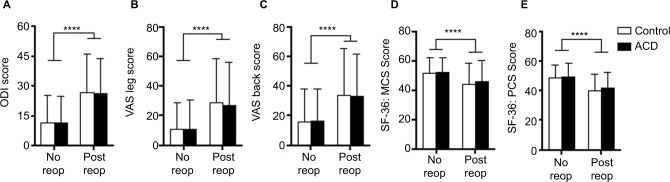
Annular closure device
The Barricaid® ACD (Intrinsic Therapeutics, Inc.) is intended to serve as an adjunct to lumbar discectomy by occluding the annular defect and retaining the nucleus pulposus within the normal anatomic disc space. The device consists of a rigid titanium anchor to ensure proper fixation into the selected adjacent vertebral body and a flexible polymer occlusion component that inserts into the annular defect and prevents subsequent migration of the nuclear material (Figure 1). A radiopaque platinum-iridium marker is embedded in the occlusion component and is visible on radiographs, allowing for visualization and proper placement during implantation.
Figure 1.
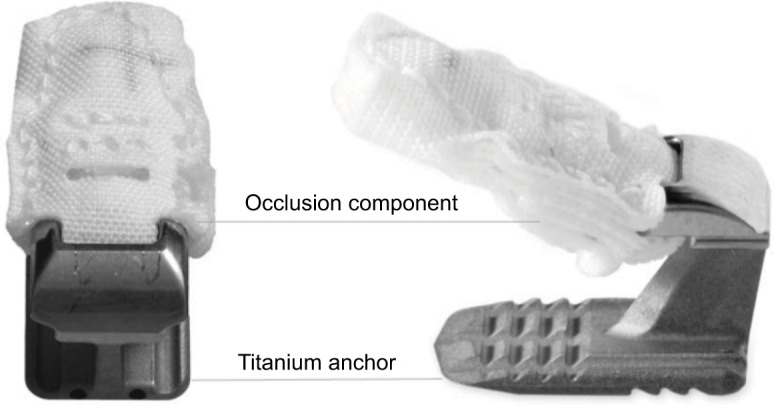
The Barricaid® annular closure device consists of a titanium anchor, which secures the device into the cranial or caudal vertebral body, and a polymer occlusion component that inserts into the annular defect to retain the nucleus pulposus within the intradiscal space.
Inclusion/exclusion criteria and interventions
All subjects received a standard limited discectomy for the treatment of a single-level symptomatic posterior or posterolateral lumbar disc herniation after failing at least 6 weeks of conservative treatment. Neural compression was confirmed via standard lumbar spine magnetic resonance imaging (MRI). Inclusion criteria included a posterior disc height of at least 5 mm, no prior surgery at the index level, and a large annular defect measuring 6–10 mm wide and 4–6 mm high that was assessed during the index surgery. Electronic randomization (1:1) was performed intraoperatively following completion of the discectomy and measurement of the annular defect such that the control group was completed via standard incision closure and the ACD group received the device under fluoroscopic guidance prior to incision closure.
Follow-up and outcome metrics
Patient follow-up visits were completed at 6 weeks and 3, 6, 12, and 24 months after surgery. Baseline demographic, clinical, and surgical characteristics, including excised nuclear volume, were recorded. Imaging included MRI, low-dose CT, and plain radiographs, which were assessed and measured by independent board-certified radiologists. The primary PRO measures were Oswestry Disability Index (ODI) and visual analog scale (VAS; 100 point scale) for back and leg pain.39 Secondary PROs included the Physical Component Summary (PCS) and Mental Component Summary (MCS) scores calculated from the Medical Outcomes Study 36-Item Short-Form General Health Survey (SF-36) scale. The patients’ working status, hours of missed work, duration of physiotherapy, and number of inpatient days due to a serious adverse event (SAE) were collected. SAE was defined in this RCT according to the guidelines of the International Organization for Standardization (ISO) document 14155:2011.40 Data on the physiotherapy time and hours of missed work were collected from a subset of the population following an addendum to the study protocol, which proceeded from the study group’s interest in the topic. This subset included 51/272 (19%) ACD-treated patients and 65/278 (23%) control patients.
Data analysis
Patients were divided into four groups for analysis based on the intervention they received and whether reoperation was required within 24 months: 1) Control-Not Reoperated, 2) Control-Reoperated, 3) ACD-Not Reoperated, and 4) ACD-Reoperated. These groups were used to analyze the effects of reoperation regardless of treatment assignment, while also seeking to understand whether the ACD had an effect on the reoperation rate. Reoperations were defined to include any revision surgery of the index level, regardless of indication. Patient data were only included in the reoperation group at time points following the first reoperation (Post Reop) in order to accurately assess the post-reoperation outcomes against the index operation outcomes of non-reoperated patients. Mean values and differences from baseline for each metric were calculated at each follow-up time point through 2 years following the primary discectomy. Additionally, minimum clinically important difference (MCID) thresholds were set based on a previous study of lumbar discectomy: ODI=13, VAS leg=15, and VAS back=15.41 A raw score threshold of 25, 45, and 55 was used for ODI, VAS leg, and VAS back, respectively, to define failure to improve.41 Patients were deemed to have clinically significant improvement if both of the following criteria were met: 1) ODI/VAS score was below the raw score threshold and 2) the change in score from baseline exceeded the MCID threshold.
Considering that the RCT was conducted across multiple international sites, the equivalent U.S. Medicare expenditures on reoperations were estimated by applying cost multipliers derived from the commercially available PearlDiver database (PearlDiver Technologies, West Conshohocken, PA, USA: 2017). Diagnosis Related Group (DRG) and Current Procedural Terminology (CPT) codes with paid 2014 Medicare claim amounts for inpatient fusion reoperations and outpatient repeat discectomy reoperations were queried in the database. Reoperations that were unrelated to the success of the primary discectomy (eg, infection management) were not included in this cost analysis. CPT and DRG codes for complications leading up to and through inpatient fusion included those for physical therapy (CPT 97110, 97112, 97116, 97140, 97530, 97535), MRI and CT imaging (CPT 72148, 72132), therapeutic steroid injection (CPT 62311), clinic visits (CPT 99215), and surgeon/facility (DRG 459, 460). CPT and DRG codes for complications leading up to and through outpatient repeat discectomy included all of these same codes, except for surgeon and facility costs, which were each assigned CPT 63042.
Statistical analysis
PRO scores were compared amongst the patient cohorts using two-way ANOVA with Sidak’s test for post hoc comparisons when the interaction term was significant. Differences in proportions were compared through Fisher’s exact test, and the 95% CI of binomial proportions was calculated using Wilson’s score method. Relative risk was calculated using the Koopman asymptotic score. Differences were considered statistically significant for p-values <0.05 and relative risk ratio 95% CIs excluding 1.0. Statistical analyses were conducted in Prism v7 (GraphPad Software Inc.; La Jolla, CA, USA).
Results
Baseline comparisons and incidence of reoperation
A total of 272 patients were treated with ACD in addition to limited discectomy and 278 patients were treated with limited discectomy alone (control). Follow-up compliance through 2 years was 93% in the ACD group and 91% in the control group. The reoperated (n=69) and non-reoperated (n=481) groups had statistically significant baseline differences for sex (42% male vs 62% male; p=0.02) and active smokers (61% vs 42%; p=0.004). ODI and MCS baseline scores (prior to index surgery) were not significantly different between reoperated and non-reoperated patients; however, baseline VAS leg, VAS back, and PCS scores were significantly worse in the reoperated group (p<0.05; Table 1).
Table 1.
Demographic, surgical, and clinical scores at baseline for reoperated and non-reoperated groups
| Non-reoperated (N=481) | Reoperated (N=69) | p-value | |
|---|---|---|---|
| Mean age (SD), years | 43.5 (10.5) | 43.5 (11.9) | 0.969 |
| Mean BMI (SD), kg/m2 | 26.3 (4.1) | 26.2 (4.1) | 0.805 |
| Sex: % male (n) | 62% (298) | 42% (29) | 0.002* |
| Current smoking status: % yes (n) | 42% (202) | 61% (42) | 0.004* |
| Operative side: % right (n) | 46% (222) | 43% (30) | 0.700 |
| Operative level: % (n) | |||
| L2/3 | 0.4% (2) | 1.5% (1) | 0.434 |
| L3/4 | 2.5% (12) | 1.5% (1) | |
| L4/5 | 40.3% (194) | 44.9% (31) | |
| L5/S1 | 56.8% (273) | 52.2% (36) | |
| Defect type: % (n) | |||
| Bulge/weakness | 29.9% (144) | 30.4% (21) | |
| Fissure | 17.1% (82) | 27.5% (19) | 0.157 |
| Full thickness defect | 52.6% (253) | 42.0% (29) | |
| None | 0.4% (29) | 0.0% (0) | |
| Defect geometry: % (n) | |||
| Box | 63.2% (304) | 53.6% (37) | |
| Cruciate | 5.2% (25) | 5.8% (4) | |
| Puncture/slit | 27.0% (130) | 36.2% (25) | |
| None | 4.6% (22) | 4.4% (3) | 0.394 |
| Herniation type: % (n) | |||
| Contained fragment | 26.0% (125) | 31.9% (22) | |
| Extruded fragment | 36.8% (177) | 31.9% (22) | |
| Sequestered fragment | 37.0% (178) | 36.2% (25) | |
| None | 0.2% (1) | 0.0% (0) | 0.602 |
| Mean nucleus removed (SD), cc | 1.3 (0.9) | 1.2 (0.8) | 0.486 |
| Mean defect width (SD), mm | 7.9 (1.3) | 8.0 (1.3) | 0.337 |
| Mean defect height (SD), mm | 4.9 (0.7) | 4.8 (0.7) | 0.512 |
| Mean defect area (SD), mm2 | 38.7 (8.8) | 39.0 (9.2) | 0.779 |
| Mean baseline SF-36 PCS (SD) | 29.0 (6.2) | 27.3 (4.6) | 0.024* |
| Mean baseline SF-36 MCS (SD) | 40.9 (12.9) | 38.6 (13.3) | 0.177 |
| Mean baseline VAS back (SD) | 54.5 (30.9) | 67.3 (26.9) | 0.001* |
| Mean baseline VAS leg (SD) | 80.3 (15.1) | 84.6 (12.4) | 0.025* |
| Mean baseline ODI (SD) | 58.4 (13.1) | 60.1 (13.0) | 0.304 |
Note: Statistically significant at p<0.05.
Abbreviations: BMI, body mass index; SF-36, 36-Item Short-Form General Health Survey; PCS, Physical Component Summary; MCS, Mental Component Summary; ODI, Oswestry Disability Index.
There were 24/272 (9%; 95% CI: 6%–13%) unique ACD patients and 45/278 (16%; 95% CI: 12%–21%) unique control patients who underwent at least one reoperation within 2 years of follow-up (p=0.01; Figure 2). The relative risk of reoperation in the control group over the ACD group was 1.84 (95% CI: 1.16–2.92). Of those reoperated patients, 14/24 (58%; 95% CI: 39%–76%) and 40/45 (89%; 95% CI: 77%–95%) were associated with an index-level symptomatic reherniation in the ACD and control groups, respectively (p=0.006; Table 2). Symptomatic reherniation was treated with either re-discectomy or fusion, as summarized in Table 2. Failure of the ACD occurred in 4/272 (1.5%) patients, which led to removal of the device and was classified as an outpatient re-discectomy for the cost analysis. For infection or wound healing disorders, there were zero reoperations in the ACD group and 3/278 (1.1%; 95% CI: 0.4%–3%) patients were reoperated in the control group. Some patients underwent multiple reoperations of various types (eg, re-discectomy followed later by fusion). The mean time to first reoperation was 7.8±6.7 months after primary discectomy.
Figure 2.
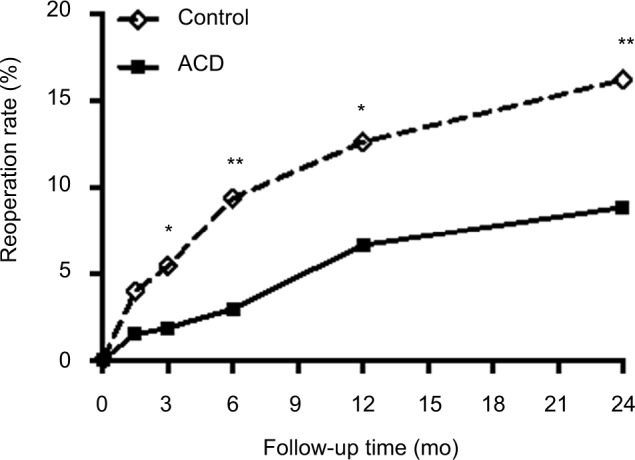
The incidence of reoperation is significantly lower among annular closure device (ACD)-treated patients compared with control patients through 2 years. The reoperation rate represents unique patients undergoing at least one reoperation. *p < 0.05; **p ≤ 0.01 by Fisher’s exact test at each time point.
Table 2.
Reasons and types of reoperations for ACD and control groups
| Reoperation
|
ACD (N=272)
|
Control (N=278)
|
p-value
|
||||
|---|---|---|---|---|---|---|---|
| Reason | Procedure | Procedures | Subjects | Procedures | Subjects | Procedures | Subjects |
| Reherniation | Re-discectomy | 10 (3.7%) | 10 (3.7%) | 37 (13.3%) | 35 (12.6%) | 0.0001* | 0.0003* |
| Fusion | 4 (1.5%) | 4 (1.5%) | 5 (1.8%) | 5 (1.8%) | |||
| Segmental instability | Fusion | 6 (2.2%) | 5 (1.8%) | 7 (2.5%) | 6 (2.2%) | 0.99 | 0.99 |
| Dural tear (not at primary procedure) | Dural tear repair | 1 (0.4%) | 1 (0.4%) | 0 | 0 | 0.49 | 0.49 |
| Hematoma | Decompression | 0 | 0 | 3 (1.1%) | 3 (1.1%) | 0.25 | 0.25 |
| Other | Decompression | 3 (1.1%) | 3 (1.1%) | 2 (0.7%) | 2 (0.7%) | 0.68 | 0.68 |
| Device failure | Removal | 4 (1.5%) | 4 (1.5%) | N/A | N/A | N/A | N/A |
| Infection or wound healing disorder | Wound revision | 0 | 0 | 6 (2.2%) | 3 (1.1%) | 0.03* | 0.25 |
| Total reoperations# | 28 (10.3%) | 27 (9.9%) | 60 (21.6%) | 54 (19.4%) | 0.0003* | 0.0017* | |
Notes: Other=Scar tissue, cyst, residual herniation, fibrosis, unspecified nerve root decompression.
Statistically significant by p<0.05.
Note that subject reoperation totals differ from the total number of unique patients who underwent reoperation because some patients underwent more than one type of reoperation.
Abbreviations: ACD, annular closure device; N/A, not applicable.
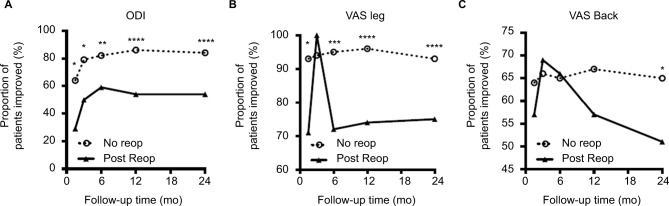
Patient-reported outcomes for disability, pain, and quality of life
At 12 and 24 months following primary discectomy, patients who had undergone a reoperation had significantly worse ODI, VAS pain, MCS, and PCS scores compared to their non-reoperated counterparts (p<0.0001 for each metric; Figure 3). The mean changes in ODI, VAS leg, and PCS scores from baseline (pre-index surgery) to 24 months were also significantly worse for reoperated compared to non-reoperated patients (p<0.001). The treatment (ACD vs control) did not significantly affect any of these postoperative PRO scores when stratified within the reoperated and non-reoperated groups (Figure 3). The proportion of patients with clinically significant improvements, based on the composite MCID and score threshold, was significantly greater in the non-reoperated compared to the reoperated group by 24 months for ODI (84% vs 54%; p<0.0001), VAS leg (93% vs 75%; p<0.0001), and VAS back scores (65% vs 51%; p=0.03; Figure 4).
Figure 3.
At 2-years of follow-up from the index procedure, the mean Oswestry Disability Index (ODI) (A), visual analog scale (VAS) leg (B), and VAS back (C) scores are significantly greater (worse) in patients who required reoperation (Post Reop) compared with patients who did not require reoperation (No Reop). The mean 36-Item Short-Form General Health Survey (SF-36) Mental Component Summary (MCS) and Physical Component Summary (PCS) scores were significantly lower (worse) in Post Reop patients compared to No Reop patients (D, E). Further stratifying the groups based on treatment demonstrated no significant differences between control and annular closure device (ACD)-treated patients for any of these metrics. ****p<0.0001 by two-way ANOVA. Bars represent mean and error bars represent SD.
Figure 4.
Significantly more patients who did not require reoperation (No Reop) experienced clinically significant improvements in Oswestry Disability Index (ODI) (A), visual analog scale (VAS) leg (B), and VAS back (C) scores by 2 years compared to patients who required reoperation (Post-Reop). Clinically significant improvement was defined as a patient experiencing a score improvement of >13 for ODI or 15 for VAS scores as well as reaching a raw score of <25 for ODI, 45 for VAS leg, and 55 for VAS back. *p<0.05, **p<0.01, ***p<0.001, and ****p<0.0001 by Fisher’s exact test.
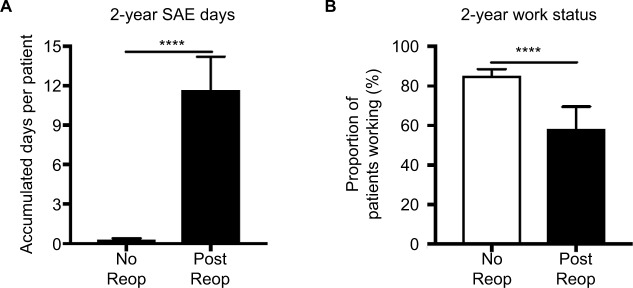
Post-operative socioeconomic burden
By 24 months, the reoperated patients had accumulated significantly more inpatient days due to an SAE (11.2±2.3 days vs 0.3±0.02 days; p<0.0001; Figure 5A) and significantly more hours of missed work (715±599 hrs vs 285±29 hrs; p=0.01). The proportion of patients that were working at 24-month follow-up was significantly greater among non-reoperated patients (85%; 95% CI: 81%–88%) compared to their reoperated counterparts (58%; 95% CI: 46%–69%; p<0.0001; Figure 5B). The mean physiotherapy time was not significantly different between reoperated (25±17 weeks) and non-reoperated (18±2 weeks) patients (p=0.24). Within the reoperated population, the control patients accounted for significantly more of the missed work time (1138±1888 hrs vs 290±218 hrs; p=0.01) and required more physiotherapy time (37±28 weeks vs 14±10 weeks; p=0.09) compared to the ACD-treated patients.
Figure 5.
A significantly greater socioeconomic burden is associated with reoperation. The reoperated patients spent significantly more time in the hospital following severe adverse events (SAEs) (A) and significantly fewer reoperated patients had returned to work by 2 years of post-index surgery (B). ****p<0.0001 by Mann–Whitney test in (A) and by Fisher’s exact test in (B). Bars in (A) represent the mean and error bars are standard error of the mean. Bars in (B) represent the proportion and error bars are the binomial 95% CI.
There were a total of 22 inpatient fusion reoperations and 51 categorized as outpatient repeat discectomies (due to reherniation and/or device failure; Table 2). The per-patient costs for inpatient fusion and outpatient repeat discectomy based on the PearlDiver database were $31,744 and $4,980, respectively, which led to estimated total reoperation costs of $698,368 for inpatient fusions and $252,980 for outpatient repeat discectomy or device removal. Control patients accounted for the majority of this estimated cost burden ($565,188; 59%) within the reoperated group and had greater per-patient costs for re-discectomy (Table 3).
Table 3.
Overall per-patient reoperation costs based on the type of reoperation procedure
| Reoperation procedure | Mean per-patient costs (95% CI)
|
|
|---|---|---|
| ACD | Control | |
| Re-discectomy | $256 ($154–421)* | $663 ($489–887)* |
| Fusion | $1,167 ($638–2,106) | $1,370 ($789–2,347) |
Notes: Lack of overlap in 95% CIs indicates statistically significant difference in ACD vs control. Values are USD.
Abbreviation: ACD, annular closure device.
Discussion
The evidence from this study demonstrates that high-risk patients who required reoperation following limited discectomy, with or without an ACD, fared worse than patients who did not require a reoperation through 2 years of follow-up. This was demonstrated through significantly worse disability, pain, and quality of life scores (Figure 3) and fewer patients achieving clinically significant improvement (Figure 4) within the reoperated group, which is consistent with findings from other studies.11,16,28–30
Leven et al and Abdu et al utilized intervertebral disc herniation data from the Spine Patient Outcomes Research Trial with 810 patients and observed significantly worse score improvements in revision patients for ODI, MCS, sciatica bothersomeness, physical function, and bodily pain compared to non-reoperated patients through 4 and 8 years of followup.11,16 Further, significantly fewer patients were somewhat or very satisfied with their symptom improvement in the reoperated group compared to the non-reoperated group after 4 (59% vs 69%; p<0.01) and 8 years of surgery (56% vs 74%; p<0.001). Similarly, using data from 8,497 patients in the Swedish National Spine Registry (Swespine), Fritzell et al observed significantly worse outcomes in ODI, VAS back and leg pain, and EQ-5D scores in reoperated patients through 2 years of follow-up. Only 58% of the reoperated patients compared with 79% of non-reoperated patients were satisfied with their surgery (p<0.001), while 65% and 74% were pain free or feeling much better in the reoperated and non-reoperated groups, respectively (p<0.01).28 Based on these findings and those of the current study, it may be important to implement conservative care for recurrent herniation prior to considering reoperation.
While other studies have suggested that revision outcomes are equivalent to primary discectomy,31–34 the underlying reasons for these disparate findings remain unclear. Differences in sample size, surgical, and/or patient factors between the studies may play a role in differentiating the patient outcomes. For example, McGirt et al observed that the incidence of reherniation after limited discectomy was greater than that for aggressive discectomy; however, aggressive discectomy was associated with a 2.5-fold increase in persistent leg and back pain beyond 2 years of follow-up.3
The patients included in this study were at a higher risk for reherniation due to the presence of a large annular defect. Consequently, higher rates of symptomatic reherniation (25%) and reoperation (16%) were observed in the control group compared to historical statistics; however, significantly fewer symptomatic reherniations (12%) and reoperations (9%) were observed in the ACD-treated patients compared to the controls. This significant reduction translated to a lower socioeconomic burden among the ACD-treated group compared to the control group.
Although this study is limited to 2 years of follow-up after primary discectomy, other studies observed that poor outcomes for reoperated patients persisted through at least 8 years of follow-up.11,30 These data suggest that reoperated patients are subject to more chronic pain and disability along with a lower quality of life and increased socioeconomic costs. In the present study, the total direct cost burden associated with re-discectomy and fusion reoperations was estimated to be $952,348 ($13,802 per reoperated patient), with control patients accumulating the majority of those costs (59%). Reducing the incidence of reoperation through preventive measures, such as an ACD, can minimize the patient morbidity and costs associated with post-discectomy reoperations.
Since the findings of this study are limited to high-risk patients with large annular defects undergoing limited discectomy, they may not translate to patients beyond these specific criteria. Another possible limitation of this study is that the reoperated patient cohort had significantly worse VAS back and leg pain scores as well as PCS scores at baseline compared to non-reoperated patients. Although statistically significant, these baseline differences in mean VAS leg pain (difference=4.3), VAS back pain (difference=12.8), and PCS score (difference=1.8) are unlikely to be clinically meaningful considering that they were less than the MCID values of 15 for VAS pain scores41 and 4.9 for PCS scores.42 Additionally, the missed work and physiotherapy time were only measured for a subset of the patient population (~20%) and the direct cost data were estimated per U.S. Medicare expenditures rather than collected directly from the international study sites.
Conclusion
At 2 years of follow-up, the rate of reoperated vs non-reoperated patients who did not achieve clinically significant improvement was 2.9 times higher based on ODI (46% vs 16%), 3.6 times higher based on VAS leg (25% vs 7%), and 1.4 times higher based on VAS back scores (49% vs 35%). The greater morbidity among the reoperated patients implied greater indirect costs due to 2.5 times more missed work and 37 times more inpatient hospital days. Reducing the incidence of reoperation by nearly 50% through annular closure reduced the number of patients subject to persistent or recurring morbidity and reduced the overall costs associated with reoperation.
Acknowledgments
The authors would like to thank the RCT study sites and coordinators for their efforts in quality data collection as well as Telos Partners LLC for their assistance in data analysis and construction of the graphs in this manuscript.
Footnotes
Disclosure
Intrinsic Therapeutics, Inc. provided support for the conduct of the study, analysis of the data, and preparation of this manuscript. PDK, FM, JI, and CT received consulting fees from Intrinsic Therapeutics, Inc. The authors report no other conflicts of interest in this work.
References
- 1.Sherman J, Cauthen J, Schoenberg D, Burns M, Reaven NL, Griffith SL. Economic impact of improving outcomes of lumbar discectomy. Spine J. 2010;10(2):108–116. doi: 10.1016/j.spinee.2009.08.453. [DOI] [PubMed] [Google Scholar]
- 2.McGirt MJ, Eustacchio S, Varga P, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine (Phila Pa 1976) 2009;34(19):2044–2051. doi: 10.1097/BRS.0b013e3181b34a9a. [DOI] [PubMed] [Google Scholar]
- 3.McGirt MJ, Ambrossi GL, Datoo G, et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery. 2009;64(2):338–344. doi: 10.1227/01.NEU.0000337574.58662.E2. discussion 344–335. [DOI] [PubMed] [Google Scholar]
- 4.Arts MP, Brand R, Koes BW, Peul WC. Effect modifiers of outcome of surgery in patients with herniated disc related sciatica? A subgroup analysis of a randomised clinical trial. J Neurol Neurosurg Psychiatry. 2010;81(11):1265–1274. doi: 10.1136/jnnp.2009.192906. [DOI] [PubMed] [Google Scholar]
- 5.Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85-A(1):102–108. [PubMed] [Google Scholar]
- 6.Carragee EJ, Spinnickie AO, Alamin TF, Paragioudakis S. A prospective controlled study of limited versus subtotal posterior discectomy: short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior anular defect. Spine (Phila Pa 1976) 2006;31(6):653–657. doi: 10.1097/01.brs.0000203714.76250.68. [DOI] [PubMed] [Google Scholar]
- 7.Daneyemez M, Sali A, Kahraman S, Beduk A, Seber N. Outcome analyses in 1072 surgically treated lumbar disc herniations. Minim Invasive Neurosurg. 1999;42(2):63–68. doi: 10.1055/s-2008-1053372. [DOI] [PubMed] [Google Scholar]
- 8.Fountas KN, Kapsalaki EZ, Feltes CH, et al. Correlation of the amount of disc removed in a lumbar microdiscectomy with long-term outcome. Spine (Phila Pa 1976) 2004;29(22):2521–2524. doi: 10.1097/01.brs.0000145413.79277.d0. discussion 2525–2526. [DOI] [PubMed] [Google Scholar]
- 9.Henriksen L, Schmidt K, Eskesen V, Jantzen E. A controlled study of microsurgical versus standard lumbar discectomy. Br J Neurosurg. 1996;10:289–293. doi: 10.1080/02688699650040160. [DOI] [PubMed] [Google Scholar]
- 10.Kim CH, Chung CK, Park CS, Choi B, Kim MJ, Park BJ. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine (Phila Pa 1976) 2013;38(7):581–590. doi: 10.1097/BRS.0b013e318274f9a7. [DOI] [PubMed] [Google Scholar]
- 11.Leven D, Passias PG, Errico TJ, et al. Risk factors for reoperation in patients treated surgically for intervertebral disc herniation: a subanalysis of eight-year SPORT data. J Bone Joint Surg Am. 2015;97(16):1316–1325. doi: 10.2106/JBJS.N.01287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 1998;23(7):814–820. doi: 10.1097/00007632-199804010-00015. [DOI] [PubMed] [Google Scholar]
- 13.Martin BI, Mirza SK, Flum DR, et al. Repeat surgery after lumbar decompression for herniated disc: the quality implications of hospital and surgeon variation. Spine J. 2012;12(2):89–97. doi: 10.1016/j.spinee.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomé C, Barth M, Scharf J, Schmiedek P. Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. J Neurosurg Spine. 2005;2(3):271–278. doi: 10.3171/spi.2005.2.3.0271. [DOI] [PubMed] [Google Scholar]
- 15.Osterman H, Sund R, Seitsalo S, Keskimäki I. Risk of multiple reoperations after lumbar discectomy: a population-based study. Spine (Phila Pa 1976) 2003;28(6):621–627. doi: 10.1097/01.BRS.0000049908.15854.ED. [DOI] [PubMed] [Google Scholar]
- 16.Abdu RW, Abdu WA, Pearson AM, Zhao W, Lurie JD, Weinstein JN. Reoperation for recurrent intervertebral disc herniation in the spine patient outcomes research trial: analysis of rate, risk factors and outcome. Spine (Phila Pa 1976) 2017;42(14):1106–1114. doi: 10.1097/BRS.0000000000002088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miwa S, Yokogawa A, Kobayashi T, et al. Risk factors of recurrent lumbar disk herniation: a single center study and review of the literature. J Spinal Disord Tech. 2015;28(5):E265–E269. doi: 10.1097/BSD.0b013e31828215b3. [DOI] [PubMed] [Google Scholar]
- 18.Huang W, Han Z, Liu J, Yu L, Yu X. Risk factors for recurrent lumbar disc herniation: a systematic review and meta-analysis. Medicine (Baltimore) 2016;95(2):e2378. doi: 10.1097/MD.0000000000002378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shimia M, Babaei-Ghazani A, Sadat BE, Habibi B, Habibzadeh A. Risk factors of recurrent lumbar disk herniation. Asian J Neurosurg. 2013;8(2):93–96. doi: 10.4103/1793-5482.116384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim KT, Lee DH, Cho DC, Sung JK, Kim YB. Preoperative risk factors for recurrent lumbar disk herniation in L5-S1. J Spinal Disord Tech. 2015;28(10):E571–E577. doi: 10.1097/BSD.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 21.Zhou B, Wang K, Hong X, et al. Adjacent level disc degeneration: a prognostic factor for recurrent lumbar disc herniation after transforaminal endoscopic lumbar discectomy in 409 cases. Int J Clin Exp Med. 2016;9:21854–21859. [Google Scholar]
- 22.Malter AD, Larson EB, Urban N, Deyo RA. Cost-effectiveness of lumbar discectomy for the treatment of herniated intervertebral disc. Spine (Phila Pa 1976) 1996;21(9):1048–1054. doi: 10.1097/00007632-199605010-00011. discussion 1055. [DOI] [PubMed] [Google Scholar]
- 23.Tosteson AN, Skinner JS, Tosteson TD, et al. The cost effectiveness of surgical versus nonoperative treatment for lumbar disc herniation over two years: evidence from the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33(19):2108–2115. doi: 10.1097/brs.0b013e318182e390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis R, Williams N, Matar HE, et al. The clinical effectiveness and cost-effectiveness of management strategies for sciatica: systematic review and economic model. Health Technol Assess. 2011;15(39):1–578. doi: 10.3310/hta15390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koerner JD, Glaser J, Radcliff K. Which variables are associated with patient-reported outcomes after discectomy? Review of SPORT disc herniation studies. Clin Orthop Relat Res. 2015;473(6):2000–2006. doi: 10.1007/s11999-014-3671-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33(25):2789–2800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sedighi M, Haghnegahdar A. Lumbar disk herniation surgery: outcome and predictors. Global Spine J. 2014;4(4):233–244. doi: 10.1055/s-0034-1390010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fritzell P, Knutsson B, Sanden B, Strömqvist B, Hägg O. Recurrent versus primary lumbar disc herniation surgery: patient-reported outcomes in the Swedish Spine Register Swespine. Clin Orthop Relat Res. 2015;473(6):1978–1984. doi: 10.1007/s11999-014-3596-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lebow RL, Adogwa O, Parker SL, Sharma A, Cheng J, McGirt MJ. Asymptomatic same-site recurrent disc herniation after lumbar discectomy: results of a prospective longitudinal study with 2-year serial imaging. Spine (Phila Pa 1976) 2011;36(25):2147–2151. doi: 10.1097/BRS.0b013e3182054595. [DOI] [PubMed] [Google Scholar]
- 30.Vik A, Zwart JA, Hulleberg G, Nygaard OP. Eight year outcome after surgery for lumbar disc herniation: a comparison of reoperated and not reoperated patients. Acta Neurochir (Wien) 2001;143(6):607–610. doi: 10.1007/s007010170066. discussion 610–611. [DOI] [PubMed] [Google Scholar]
- 31.Cinotti G, Roysam GS, Eisenstein SM, Postacchini F. Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br. 1998;80(5):825–832. doi: 10.1302/0301-620x.80b5.8540. [DOI] [PubMed] [Google Scholar]
- 32.Wera GD, Marcus RE, Ghanayem AJ, Bohlman HH. Failure within one year following subtotal lumbar discectomy. J Bone Joint Surg Am. 2008;90(1):10–15. doi: 10.2106/JBJS.F.01569. [DOI] [PubMed] [Google Scholar]
- 33.Ahsan K, Najmus S, Hossain A, Khan SI, Awwal MA. Discectomy for primary and recurrent prolapse of lumbar intervertebral discs. J Orthop Surg (Hong Kong) 2012;20(1):7–10. doi: 10.1177/230949901202000102. [DOI] [PubMed] [Google Scholar]
- 34.Papadopoulos EC, Girardi FP, Sandhu HS, et al. Outcome of revision discectomies following recurrent lumbar disc herniation. Spine (Phila Pa 1976) 2006;31(13):1473–1476. doi: 10.1097/01.brs.0000219872.43318.7a. [DOI] [PubMed] [Google Scholar]
- 35.Parker SL, Grahovac G, Vukas D, Ledic D, Vilendecic M, McGirt MJ. Cost savings associated with prevention of recurrent lumbar disc herniation with a novel annular closure device: a multicenter prospective cohort study. J Neurol Surg A Cent Eur Neurosurg. 2013;74(5):285–289. doi: 10.1055/s-0033-1341416. [DOI] [PubMed] [Google Scholar]
- 36.Ambrossi GL, McGirt MJ, Sciubba DM, et al. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery. 2009;65(3):574–578. doi: 10.1227/01.NEU.0000350224.36213.F9. discussion 578. [DOI] [PubMed] [Google Scholar]
- 37.O’Donnell JA, Anderson JT, Haas AR, et al. Treatment of recurrent lumbar disc herniation with or without fusion in workers’ compensation subjects. Spine (Phila Pa 1976) 2017;42(14):E864–E870. doi: 10.1097/BRS.0000000000002057. [DOI] [PubMed] [Google Scholar]
- 38.Klassen PD, Hes R, Bouma GJ, et al. A multicenter, prospective, randomized study protocol to demonstrate the superiority of a bone-anchored prosthesis for anular closure used in conjunction with limited discectomy to limited discectomy alone for primary lumbar disc herniation. Int J Clin Trials. 2016;3(3):120–131. [Google Scholar]
- 39.DeVine J, Norvell DC, Ecker E, et al. Evaluating the correlation and responsiveness of patient-reported pain with function and quality-of-life outcomes after spine surgery. Spine (Phila Pa 1976) 2011;36(Suppl 21):S69–S74. doi: 10.1097/BRS.0b013e31822ef6de. [DOI] [PubMed] [Google Scholar]
- 40.International Organization for Standardization Clinical investigation of medical devices for human subjects – Good clinical practice (ISO/DIS Standard 14155) 2011. [Accessed January 30, 2016]. Available from: https://www.iso.org/standard/45557.html.
- 41.Werner DAT, Grotle M, Gulati S, et al. Criteria for failure and worsening after surgery for lumbar disc herniation: a multicenter observational study based on data from the Norwegian Registry for Spine Surgery. Eur Spine J. 2017;26(10):2650–2659. doi: 10.1007/s00586-017-5185-5. [DOI] [PubMed] [Google Scholar]
- 42.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008;8(6):968–974. doi: 10.1016/j.spinee.2007.11.006. [DOI] [PubMed] [Google Scholar]