Abstract
Transplant medicine is fraught with clinical–ethical issues. It is not uncommon to have ethicists on transplant teams to help navigate ethically complex cases and ethical questions. Clinical ethicists work in hospitals and/or other healthcare institutions identifying and addressing value-laden conflict and ethical uncertainties.
As ethicists, we set out to describe our process and involvement in cases involving extracorporeal membrane oxygenation (ECMO). Our work centers on monitoring and optimizing communication among clinicians, families, and patients, with the goals of (1) aligning patient/family understanding of the nature and purpose of ECMO while encouraging realistic expectations for possible outcomes, and (2) proactively mitigating the moral distress of providers involved in complex ECMO cases. We close with recommendations for how to measure the impact of ethicists' involvement in ECMO cases.
Keywords: decision making, extracorporeal membrane oxygenation, ECMO, ethics, end of life, mechanical circulatory support
INTRODUCTION
Transplant medicine is fraught with clinical–ethical issues. It is not uncommon to include ethicists on transplant teams to help navigate ethically complex cases and questions. Clinical ethicists work in hospitals and/or other healthcare institutions identifying and addressing value-laden conflict and ethical uncertainties. Although they may work on ethics committees, clinical ethicists most frequently work in small teams with other ethicists or address cases on an independent consultant basis.1 Ethics consultations typically involve seemingly intractable conflicts between stakeholders about personal, value-laden ethical issues, such as end-of-life decision making, confidentiality and privacy concerns, informed consent, surrogate decision making, and professional or institutional responsibilities. Ideally, clinical ethicists work efficiently and systematically to elicit morally relevant perspectives, synthesize information, identify ethically appropriate courses of action, and help parties move towards an ethically appropriate course of action.
ROLE OF THE ETHICIST IN ECMO CASES
The earliest published account of ethicists on transplant teams dates back to 1993, although we suspect ethicists' involvement might have preceded formal documentation of their inclusion.2 What we can say with some confidence is that ethicists are becoming increasingly involved within transplant programs, both in the number of institutions that now include ethicists on their transplant teams and in the degree and scope of ethicists' responsibilities within those teams.3
In the heart and lung transplant programs at Houston Methodist Hospital, ethicists participate on the Medical Review Board for each transplant service and during multidisciplinary rounds in the cardiovascular intensive care unit (ICU), where we are readily available to address ethical questions and concerns in real time. Within the past 3 years, we have expanded our participation to cases involving extracorporeal membrane oxygenation (ECMO) or extracorporeal life support (ECLS).4 ECMO is recognized by clinical ethicists and clinicians to be a unique form of life-sustaining intervention because, unlike ventilator and dialysis support, the trajectories of treatment for ECMO patients are limited.5 ECMO is initiated to serve as a bridge to achieve one of two goals: (1) native organ recovery (i.e., bridge to recovery) or (2) organ transplantation or device implantation (i.e., bridge to transplant/implantation). Native organ recovery is pursued by default if the patient is not a transplant or device candidate. In this case, if recovery of the patient's native organ function becomes highly unlikely, the only option is to discontinue ECMO and shift goals to focus on comfort care (i.e., bridge to nowhere).6,7
Given the high level of clinical uncertainty regarding ECMO's efficacy and likelihood of success, particularly in adult patient populations, it can be challenging to manage the expectations of families, patients, and clinicians regarding the purpose, nature, and intended duration of ECMO use.5 It takes several physicians to coordinate the care of an ECMO patient in critical care settings, which makes it especially difficult to maintain consistent communication between the medical team and the patient and family.6,7 Team-based dynamics present opportunities for miscommunication that, in turn, can have a negative effect on patient care and result in moral distress for the medical team, especially in cases where ethical dilemmas arise secondary to ECMO's failure to meet its intended trajectory.8
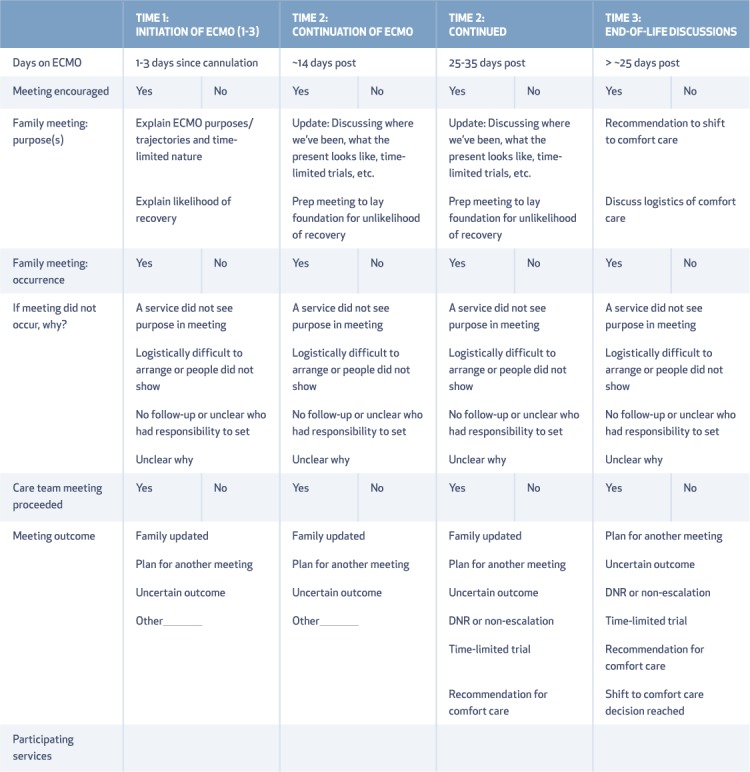
Our involvement on the ethics team centers on monitoring and optimizing clinician-family-patient communication, with the goals of (1) aligning patient and family understanding of the nature and purpose of ECMO while encouraging realistic outcome expectations, and (2) proactively mitigating the moral distress of providers involved in complex ECMO cases. Multidisciplinary care teams including physicians, nurses, social workers, case managers, chaplains, and clinical ethics consultants are integrally involved in the care of ECMO patients, as are various specialists such as cardiothoracic surgeons, cardiologists, pulmonologists, intensivists, infectious disease specialists, and palliative care clinicians.6 With so many team members involved, we find it necessary to delineate responsibilities between clinicians and the ancillary services that are consulted to assist in the management and coordination of care. Table 1 is a checklist we use to assist in identifying key personnel involved in each patient's case. We also use this checklist to confirm that the family has been appropriately updated and informed and that decisions are being made in an appropriate and timely way.
Table 1.
Guidelines for managing patients on extracorporeal membrane oxygenation (ECMO).
In each case, we first identify a physician point person (generally the patient's attending physician, surgeon, or cardiologist who placed the ECMO) as the primary agent for managing the patient's clinical care and communicating the consensus of the clinical team to the patient and/or family. The point person is expected to work with the other clinicians to stay updated on the latest clinical developments and how those may or may not impact the patient's overall status and prognosis.
The role of social work in these cases is to support ECMO patients and surrogates and assist in planning family meetings between clinicians, surrogates, and any other involved family as needed. Depending on the goals of care, they will also assist in creating either a safe discharge or plan for transfer or transition towards hospice care. Chaplaincy assesses spiritual needs, offers spiritual support and prayer, and informs the team of how the family and patient are coping. Chaplains also play an important role in supporting the clinicians and especially bedside nurses who are involved in caring for the patient directly, particularly in cases involving significant emotional distress.
If available, a palliative care service is routinely consulted for all ECMO patients; this allows the palliative care team to take on a meaningful role in building patient and family rapport in case a complication occurs that would abruptly shift the intended trajectory of care. Should a complication occur, the hope would be that the palliative care team would have a trusting relationship with the patient or family so that they could smoothly transition to comfort care if and when such a transition becomes appropriate.
As the patient's status changes, so too does the role of the clinical ethics consultant. Throughout each phase of ECMO, the ethics consultant collaborates closely with the clinical team to identify the point at which the care trajectory will shift to support patients and families who must endure an uncertain outcome. Upon ECMO initiation, the clinical ethicist lays a foundation for decision points with the clinicians and holds them accountable for discussing whether ECMO continuation provides a greater benefit than risk of complication to the patient. If and when there is disagreement among physicians, the ethicist should coordinate a team meeting with the clinicians to come to a consensus regarding whether to continue ECMO before offering a recommendation to the family. If the patient fails to improve and the clinical team agrees that recovery with continued use of ECMO is unlikely or impossible, then the ethicist should collaborate with the team to recommend discontinuation.
The following case illustrates the role of the clinical ethics team in the setting of ECMO.
CASE
Mr. Z is a 68-year-old man with no significant past medical history other than mild chronic obstructive pulmonary disease. He is admitted to the cardiovascular ICU for acute respiratory distress syndrome (ARDS) and severe hypoxemia secondary to bilateral pneumonia and emergently placed on venovenous ECMO. Before taking Mr. Z to the operating room (OR), the clinical team tells Mrs. Z, the patient's wife and surrogate decision maker, that Mr. Z will be placed on ECMO to “buy him more time” as a bridge to recovery from his ARDS. Mrs. Z is distraught when her husband is taken to the OR and is focused on staying by his side until he is wheeled away, telling the team to “do what you can to save him!”
ECMO INITIATION
The goal of initiating ECMO is to sustain cardiac and/or pulmonary function until the patient's status improves or the patient can be evaluated for transplant. During ECMO initiation or shortly thereafter, ethicists meet with the clinicians and decision makers (usually the ICU intensivist and the patient's family) to lay the groundwork for a dynamic model of decision making that depends on changes in the patient's clinical status. The conversation entails a description of the nature, purpose, and risks of ECMO to explicitly inform families that ECMO is a time-limited intervention that cannot sustain life for prolonged periods. In addition, the team should offer an explanation of the patient's current trajectory and what could happen if the intended trajectory does not occur (i.e., the patient is faced with a bridge to nowhere).4 By introducing this possible trajectory early on, surrogates are given more time to prepare themselves for the worst-case scenario. Surrogates often respond to conversations about the end of life as though the conversations are unexpected and jarring because a foundation was not laid. This is why it is pivotal to lay the groundwork for the possibility of a negative outcome if it is within the realm of possible outcomes.
In the case of Mr. Z, the ethicist meets with the ICU intensivist to clarify Mr. Z's trajectory and learns that he is being evaluated by the lung transplant service to determine if he is a potential candidate for transplantation, as his lung disease seems so severe that he may not recover enough to be taken off ECMO. If Mr. Z is rejected for transplantation, he will still be on ECMO as a bridge to recovery rather than a bridge to transplant. The ethicist and intensivist then meet with Mrs. Z and her daughter to elucidate understanding of Mr. Z's current care plan. Understandably, Mrs. Z is unable to explain her understanding of the plan because “everything happened so fast” that she cannot remember exactly what the physicians told her before Mr. Z went to the OR. At the invitation of the ethicist, an intensivist reiterates the nature, purpose, and risks of ECMO to Mrs. Z and informs her that as Mr. Z's clinical status or prognosis changes, the goals of care may need to be reevaluated. The intensivist outlines the circumstances in which ECMO may need to be discontinued should Mr. Z not be a transplant candidate and his status further deteriorate.
ECMO CONTINUATION
Shared decision making should persist in conversations between surrogates and the clinical team regarding the continuation of ECMO support. The designated physician point person confers with all invested clinicians to ensure that the full clinical team is on the same page regarding recommendations for continuation and projections for either improvement or transplant candidacy. Families and surrogates should receive updates from the full team regarding the patient's overall clinical status and likelihood of recovery or transplantation at least weekly if not more frequently. This multidisciplinary perspective is offered routinely in addition to frequent updates about clinical details. Throughout this process, clinicians who rotate off service should update the oncoming clinician about the ongoing plan discussed in previous conversations and what meetings are anticipated. If colleagues disagree about the plan during handoff, the oncoming clinician should discuss his/her concerns with colleagues and reestablish consensus before any changes occur.
In some cases, patients encounter several setbacks—which can be a consequence of their underlying disease or of ECMO itself—that necessitate a longer period of time on ECMO. In these cases, the clinical team may be uncertain about whether the trajectory should shift. If there is disagreement between clinicians about whether the possible benefit still outweighs the risk, a member of the care team coordinates a meeting between the clinicians to discuss the patient's status and determine whether, or when, it would be clinically appropriate to move towards discontinuation. If agreement cannot be achieved, a middle-ground approach is considered. For example, the team might agree on a time-limited trial in which ECMO would be continued for 1 to 2 weeks (possibly even as little as 24–48 hours) and specify the clinical criteria that should be met to support ongoing continuation.9 If these parameters for improvement are not met at the end of the established time period, then the team will plan to shift goals of care to focus on comfort and palliation.
Once the team is in agreement about the care plan moving forward, the plan is discussed with the family in a manner that manages the family's expectations for improvement. As the team explains the clinical criteria that will be evaluated over the defined time period, they should encourage the family to focus on the big picture of what is happening with the patient's organ systems and how he/she is responding to ECMO rather than focusing on the numerical details such as ECMO settings and blood tests.
After 3 weeks on ECMO and 4 days after tracheostomy, Mr. Z's candidacy for transplant becomes questionable since he suffers from nosocomial infections that are not responding well to treatment. He also requires continuous renal replacement therapy (CRRT) for his acute kidney injury. Since he has not regained meaningful interactive capacity, he is unable to ambulate. Mr. Z experiences deteriorating cardiac function despite improved gas exchange and is converted to veno-arterial ECMO to help his decreasing cardiac output. Between the infections, lack of ambulation, and dialysis, Mr. Z's intensivist is concerned that there are too many contraindications to lung transplantation. The transplant pulmonologist agrees that transplantation is unlikely, but he believes that Mr. Z remains a bridge to recovery candidate.
During a family meeting in which the transplant team conveys that Mr. Z is not a transplant candidate, the ethicist helps the clinicians formulate a time-limited trial with the patient's family; that is, the patient and family agree upon 2 more weeks on ECMO to see if the patient improves or deteriorates according to specific clinical parameters (which they identify as wakefulness and regaining capacity, coming off of CRRT, and clearing the current infections that prohibit transplantation and immune suppression).
ECMO DISCONTINUATION
When it is clear that the patient is no longer a transplant candidate and can no longer benefit from ECMO, a family meeting is arranged to discuss the discontinuation of ECMO until the entire team is in agreement about shifting to that trajectory. Even when recovery is unlikely, it is appropriate to continue ECMO for a few days before engaging in a final endof-life conversation as part of an incremental decision-making process. Doing so allows for an adjustment period for families to begin coming to terms with the patient's condition and prepare for moving towards end-of-life considerations.
Before having the final discussion recommending ECMO discontinuation, we consider it helpful to arrange a preparatory meeting between the team and the family. During this preparatory meeting, the responsible clinician updates the family regarding the patient's critical status and likely decline. Here we argue that setting parameters for a time-limited trial (e.g., ≤ another week) of continuing ECMO prior to withdrawal allows the family to work towards accepting the patient's prognosis and expiration while demonstrating that the team is continuing aggressive treatment in the short-term to give the patient every possible chance to recover, even when the chances are extremely low.
Note that when ECMO discontinuation is the most clinically viable option, it is appropriate to shift from the shared decision-making model to a more direct approach in which the team makes a recommendation to withdraw ECMO and shift to comfort care since continuing ECMO would be medically inappropriate.10 Using a collaborative communication approach at this point would place a significant burden on the patient and/or family and implies the possibility of an extremely unlikely recovery. A direct recommendation to discontinue ECMO still requires assent from the family or surrogate but offers them guidance in a challenging and unfamiliar situation. This approach recognizes that there are very few options yet still gives the patient or family a sense of control when used compassionately and in a supportive matter. Being clear about the clinically appropriate course may help relieve surrogates of the burdens associated with “giving up” on their loved ones.
On day 23 of ECMO support, Mr. Z experiences a major limb vessel occlusion by the arterial cannula as well as an arterial embolism and refractory cannula site bleeding. A few days thereafter, Mr. Z suffers a cardiac arrest likely triggered by refractory ventricular fibrillation secondary to his multiorgan failure and evolving myocardial dysfunction. Following prolonged attempts to convert, two physicians determine that Mr. Z has experienced neurologically devastating injuries from a presumed embolic event; this was confirmed by a head CT showing a significant stroke. An electroencephalogram shows that Mr. Z has minimal activity, though not in burst suppression. His neurologist opines that Mr. Z is showing indicators that he will likely be in a persistent vegetative state.
In a final family meeting, the ethicist helps the team convey a direct message that ECMO is no longer serving as a bridge to recovery due to recent neurological injuries. The team then recommends shifting the trajectory of treatment towards supporting the family in its decision to transition Mr. Z to comfort care and plan the timing of terminal decannulation.
CONCLUSION
There is limited research on practical recommendations for the ethical management of surrogate decision making as it relates to ECMO patients. Further engagement is needed between physicians and ethicists in ICUs across the country to establish best practices in managing communication in an ECMO setting and to improve the experience for patients, families, and the clinical teams. In our experience, implementing our guidelines for managing ECMO patients has helped to streamline communication among all stakeholders through regularly scheduled meetings between the clinical team and family; this includes additional pre-meetings between the responsible physicians to ensure that there is agreement regarding the plan of care when the possibility of conflict or communication breakdown is detected. We have observed that consistent messaging between team members and to patients/families has decreased the confusion about the planned course of care for both the families and for those directly involved in the patient's care, specifically the nursing staff. While responses to our involvement have been overwhelmingly positive, we anticipate possible future tension in cases where members of the team are unable to agree on when to transition a patient's trajectory. In such cases, management approaches to meetings may vary due to the team dynamics at play.
As our endeavors progress, it will be beneficial to develop satisfaction surveys to determine whether the clinical team experiences a benefit from our involvement or if there are cases in which our involvement may feel excessive. A survey could also identify if and how use of these guidelines helps mitigate the presence and experience of moral distress for physicians and clinical staff in complex ECMO cases (i.e., those patients who have a long duration on ECMO). These types of surveys would offer opportunities for quality improvement by helping to ensure best practices and productive use of the ethics team's expertise to best serve patients, families, and clinical care teams.
KEY POINTS
Ethics consultations typically involve conflicts between stakeholders about personal, value-laden ethical issues such as end-of-life decision making, confidentiality and privacy concerns, informed consent, surrogate decision making, and professional or institutional responsibilities.
Management of patients on ECMO involve multidisciplinary care teams that include physicians, nurses, social workers, case managers, chaplains, and clinical ethics consultants.
The ethics team serves to monitor and optimize clinician-family-patient communication, with the goals of (1) aligning patient and family understanding of the nature and purpose of ECMO while encouraging realistic outcome expectations, and (2) proactively mitigating the moral distress of providers involved in complex ECMO cases.
Throughout each phase of ECMO, the ethics consultant collaborates closely with the clinical team to identify the point at which the care trajectory will shift to support patients and families who must endure an uncertain outcome.
Acknowledgments
The authors would like to thank the many supportive, collaborative clinicians whom they interact with on complex ECMO cases.
Footnotes
Conflict of Interest Disclosure: The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
REFERENCES
- 1. Tarzian AJ; Asbh Core Competencies Update Task Force 1. . Health care ethics consultation: an update on core competencies and emerging standards from the American Society For Bioethics and Humanities' core competencies update task force. Am J Bioeth. 2013; 13 2: 3– 13. [DOI] [PubMed] [Google Scholar]
- 2. Finder S, Fox MD, Frist WH, Zaner RM.. The ethicist's role on the transplant team: a study of heart, lung, and liver transplantation programs in the United States. Clin Transplant. 1993; 7: 559– 64. [PubMed] [Google Scholar]
- 3. Bramstedt KA, Chalfant A, Wright C.. Emergency consults in the setting of transplant medicine: dilemmas for social workers and bioethicists. Prog Transplant. 2007. March 1; 17 1: 36– 9. [DOI] [PubMed] [Google Scholar]
- 4. Extracorporeal Life Support Organization [Internet]. Ann Arbor: Extracorporeal Life Support Organization; c2018. General Guidelines for all ECLA Cases; 2013 Nov [cited 2018 Jan 31]. Available from: https://www.elso.org/Portals/0/IGD/Archive/FileManager/929122ae88cusersshyerdocumentselsoguidelinesgeneralalleclsversion1.3.pdf [Google Scholar]
- 5. Meltzer EC, Ivascu NS, Acres CA, . et al. Extracorporeal membrane oxygenation in adults: a brief review and ethical considerations for nonspecialist health providers and hospitalists. J Hosp Med. 2014. December; 9 12: 808– 13. [DOI] [PubMed] [Google Scholar]
- 6. Doll JA, Ohman EM, Patel MR, . et al. A team-based approach to patients in cardiogenic shock. Catheter Cardiovasc Interv. 2016. September; 88 3: 424– 33. [DOI] [PubMed] [Google Scholar]
- 7. MacLaren G, Combes A, Bartlett RH.. Contemporary extracorporeal membrane oxygenation for adult respiratory failure: life support in the new era. Intensive Care Med. 2012. February; 38 2: 210– 20. [DOI] [PubMed] [Google Scholar]
- 8. Abrams DC, Prager K, Blinderman CD, Burkart KM, Brodie D.. Ethical dilemmas encountered with the use of extracorporeal membrane oxygenation in adults. Chest. 2014. April; 145 4: 876– 82. [DOI] [PubMed] [Google Scholar]
- 9. Bruce CR, Liang C, Blumenthal-Barby JS, . et al. Barriers and Facilitators to Initiating and Completing Time-Limited Trials in Critical Care. Crit Care Med. 2015. December; 43 12: 2535– 43. [DOI] [PubMed] [Google Scholar]
- 10. White DB, Malvar G, Karr J, Lo B, Curtis JR.. Expanding the paradigm of the physician's role in surrogate decision-making: an empirically derived framework. Critical Care Med. 2010. March; 38 3: 743– 50. [DOI] [PMC free article] [PubMed] [Google Scholar]


