Abstract
Intensive care unit telemedicine (tele-ICU) is technology enabled care delivered from off-site locations that was developed to address the increasing complexity of patients and insufficient supply of intensivists. Although tele-ICU deployment is increasing, it continues to cover only a small proportion of ICU patients. This is primarily due to expense, with first-year costs exceeding $50,000 per bed. Meta-analyses of outcomes indicate survival benefits and quality improvements, albeit with significant heterogeneity. Depending on the context, a wide range of estimated incremental cost-effectiveness ratios reflects variable effects on cost and outcomes, such as mortality or length of stay.
Tele-ICUs may fit within a hybrid model of care to complement high-intensity ICU staff coverage. However, more research is required to foster consensus and determine best practices. This review summarizes data on tele-ICU structure, operations, outcomes, and costs. Evidence was extracted from meta-analyses, with secondary data from Cleveland Clinic's tele-ICU experience.
Keywords: ICU, intensive care unit, telemedicine, critical care, outcomes, cost-effectiveness
INTRODUCTION
Critical care is resource intensive and demands meticulous process control. The complexity of intensive care unit (ICU) support has increased due to aging demographics and surgical advances.1 This is especially magnified for cardiovascular patients with the expansion of mechanical cardiac support. Improved outcomes are predicated with early recognition of illness in tandem with defined care processes. Also, patient–physician ratios, timing of admission, and staffing models all interplay to affect outcomes.2,3 Even so, growth projections indicate an insufficient supply of intensivists to meet future demand.4
Research has shown more favorable outcomes with high-intensity staffing models that include closed units and/or mandatory intensivist consultation. For example, Pronovost et al. showed reduced hospital mortality with high-intensity coverage.5 Despite this, 24/7 onsite intensivist coverage is controversial. Wallace et al. reported enhanced quality and risk-adjusted mortality, whereas Wilcox et al. found no ICU mortality benefit for 24/7 versus daytime coverage.6,7 Kerlin et al. also reported no survival benefit with 24/7 coverage in a 2017 meta-analysis.8 In a cardiac surgery cohort, Kumar et al. found that 24/7 intensivist coverage (versus resident physician coverage with intensivist backup) neither improved mortality nor ICU length of stay (LOS).9 However, sepsis, renal failure, blood product use, and hospital LOS were reduced.
There is a possibility that 24/7 coverage may benefit subsets of patients, but the optimal contexts remain undefined. Regardless, limited availability of intensivists and increased costs may make 24/7 models untenable. Accordingly, ICU telemedicine (tele-ICU) has been proposed to increase access to critical care expertise.10 This review examines evidence for the use of tele-ICU including its structure, operations, outcomes, and costs.
METHODS
A narrative review was chosen for the research design to encompass a comprehensive view.11 Evidence was abstracted from systematic reviews and meta-analyses in PubMed, PMC, EMBASE, and Cochrane Reviews along with state-of-the-art reviews, observational studies, and key historical publications. Referenced statistics are presented from the original publications, and information about Cleveland Clinic's tele-ICU is included to provide relevant perspective.
POTENTIAL FOR TELE-ICU
The premise for tele-ICU is that remote video visualization of patients and biomedical devices and access to electronic medical records (EMR) confers an advantage to the teleintensivist relative to the on-call intensivist, depending on verbal relay of information by the bedside caregivers. Tele-ICU platforms leverage algorithms to scrutinize patient data, combining physiological parameters with clinical risk factors to predict deterioration and provide decision support. Insights afforded by embedded risk-prediction algorithms and push-notification dashboards may facilitate more efficient interventions to reduce ICU risk. Thus, the tele-intensivist can augment conventional coverage in multiple ICUs where onsite support is unavailable and bridge gaps in nocturnal care.
HISTORICAL DEVELOPMENT
In 1977, a study by Grundy et al. demonstrated feasibility of tele-ICU from an academic medical center to a private hospital.12 This observational study showed the potential for tele-intensivist consultation and scheduled tele-ICU rounds. In a more recent feasibility study of home-based intensivists using advanced telemedicine tools for surgical ICU patients, Rosenfeld et al. showed reduced severity-adjusted ICU and hospital mortality, ICU complications, LOS, and cost savings from averted complications.10
Although tele-ICU adoption has grown since these earlier studies, to date they support only a minority of critically ill patients in the United States. A 2014 study examined tele-ICU deployments between 2002 and 2010 using data from the Centers for Medicare and Medicaid Services (CMS).13 The number of hospitals adopting tele-ICUs increased from 16 (0.4%) to 213 (4.6%) while covered beds increased from 598 (0.9%) to 5,799 (7.9%). Lilly et al. confirmed this growth in their 2014 study showing that tele-ICUs supported patients in 11% of non-federal U.S. hospitals.14 Tele-ICUs now support various patient populations, including medical, neurological, cardiac, and surgical patients in both urban and rural settings.
Opportunities for Cardiovascular Emergency and Critical Care
Telemedicine adoption has improved emergency cardiac care, and consensus guidelines have emphasized multiple time-based interventions to optimize patient outcomes.15 These include (1) prehospital diagnoses of acute myocardial infarction with electrocardiogram transmission, (2) monitoring of patients with chronic heart failure, (3) long-distance device assessment/control (pacemakers, defibrillators, extracorporeal membrane oxygenation, left ventricular assist devices, and intra-aortic balloon pumps), (4) continuous monitoring and interventions for cardiac arrhythmias, (5) transmission of echocardiography images for consultation, and (6) online patient consultation and triage to higher levels of care. Additionally, in the context of higher-severity illness, the need for care integration, and advances in specialized cardiovascular care, Na et al. demonstrated an association between cardiac intensivist-directed care and severity-adjusted reductions in mortality.16 Clearly, potential exists for expanding tele-ICU support of cardiac critical care patients, enhancing 24-hour care and reducing response times for complex issues.
TELE-ICU PROGRAM DESIGN
Components
Tele-ICU delivers technology-enabled care from a remote command center. At its simplest, mobile platforms provide on-demand, two-way, audiovisual (AV) communication between ICUs and the tele-ICU center. Typical infrastructure is more complex and involves a tiered system of fixed AV communication, access to EMRs, telemetry, and imaging systems for data retrieval and documentation, plus risk stratification and decision support (Figure 1).17 In the United States, there is one predominant system called Philips eICU (Royal Philips).18
Figure 1.
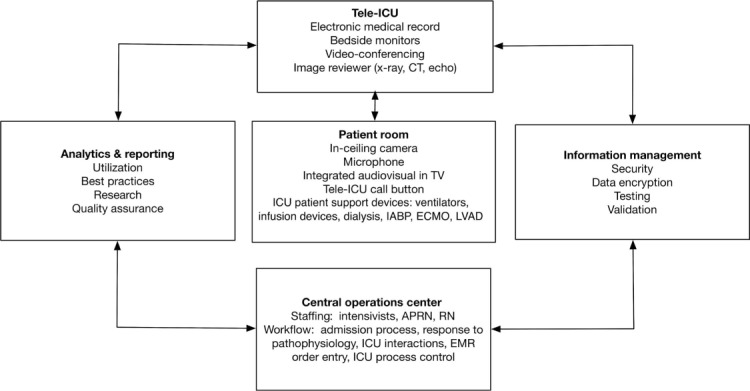
The operational structure of a tele-ICU program based on the experience at Cleveland Clinic. tele-ICU: telemedicine intensive care unit; CT: computed tomography; APRN: advanced practice registered nurse; RN: registered nurse; EMR: electronic medical records; IABP: intra-aortic balloon pump; ECMO: extracorporeal membrane oxygenation; LVAD: left ventricular assist device
Staffing
There are two tele-ICU staffing models to date: hospitals staff their own centers with intensivists, nurses, and other personnel (depending on institutional needs and limitations), or the center is outsourced to other hospitals or independent firms that support networks of ICUs. Regulatory requirements for licensure and credentialing impose significant constraints for interstate networking.
In 2014, Cleveland Clinic developed and gradually deployed its own telemedicine platform called eHospital. It features a risk-stratification dashboard with EMR context synchronization and two-way AV functionality (Figure 1). Two teams of intensivists, nurse practitioners, and ICU nurses provide nocturnal support to almost 300 beds across 11 hospitals in the health system, including cardiac surgery patients at three tertiary ICUs.
Operations
Tele-ICU platforms provide overviews of ICU patients to optimize clinical care and assure quality. The tele-intensivist oversees the execution or necessary modification of patients' care plans aided by risk stratification and notification dashboards. However, hands-on clinician involvement for technical procedures, such as endotracheal intubation or central vascular access, still requires onsite providers in the hospital or access to on-call intensivists.
Costs
Cost is a primary driver influencing tele-ICU deployment. A systematic review of related costs by Kumar et al. in 2013 noted variable implementation and operational costs ranging between $50,000 and $100,000 per ICU bed for the first year.17 These included costs for hardware, installation, software licenses, staffing, and other operational expenses. Further, there was heterogeneity in variable costs ranging from a decrease of $3,000 to a $5,600 increase per patient. These financial considerations will change given the recent approval of reimbursement for tele-ICU by CMS, albeit with geographic restrictions.
OUTCOMES
Clinical Outcomes
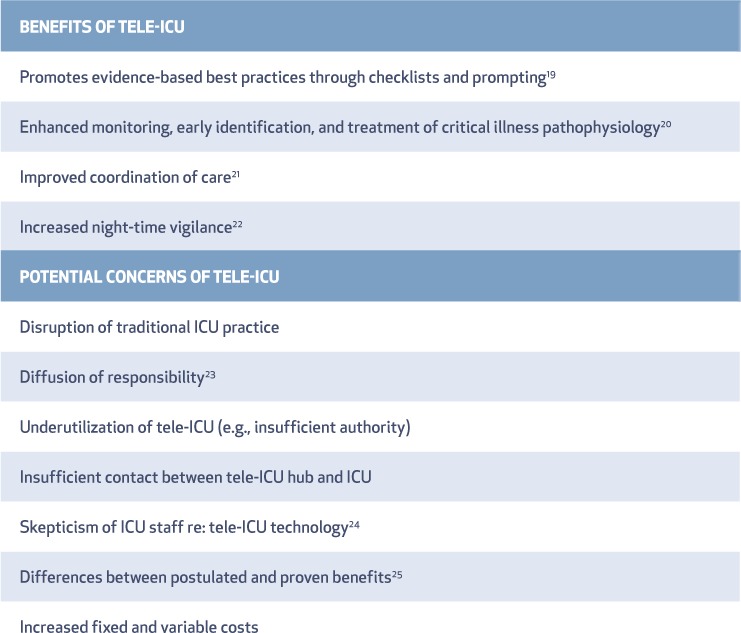
Tele-ICU interventions have been characterized and include clinical assessments of physiological trend alerts, notification/correction of abnormal laboratory values, and virtual rounding by the tele-ICU team (Table 1).19–25 In one study, 80% of interventions occurred when the onsite ICU team was absent; although only 0.6% of interventions were described as directly lifesaving, 57% of interventions altered the care plan. Notably, these investigators recognized that interventions were influenced by ICU and hospital culture, institutional protocols, and clinical privileges of the tele-ICU team.26 Nonetheless, in a study by Lilly et al. of 6,290 patients in seven ICUs, tele-ICU was associated with increased best-practice adherence, including prophylaxis for ventilator-associated pneumonia, catheter-related infection, stress ulcers, and deep vein thrombosis, with similar outcomes for medical, surgical, and cardiovascular patients.27
Table 1.
This table depicts the rationale and concerns about tele-ICU with associated references.19–25 Tele-ICU: telemedicine intensive care unit
Early data had been mixed with regard to mortality and LOS. In 2004, an observational study in two tertiary ICUs with medical and surgical patients showed significantly reduced hospital mortality (RR 0.73; 95% CI 0.55–0.95) and reduced ICU LOS, 3.63 versus 4.35 days, (95% CI, 3.93–4.78), among patients exposed to tele-ICU.28 In contrast, a 2009 study by Thomas et al. examining outcomes before and after tele-ICU implementation between 2003 and 2006 found no differences in ICU or hospital mortality, LOS, or ICU complications after adjusting for severity of illness.29 The authors noted that onsite attending physicians determined the level of authority delegated to the tele-ICU team, and minimal delegation was chosen for 66.1% of patients, thus influencing the care.
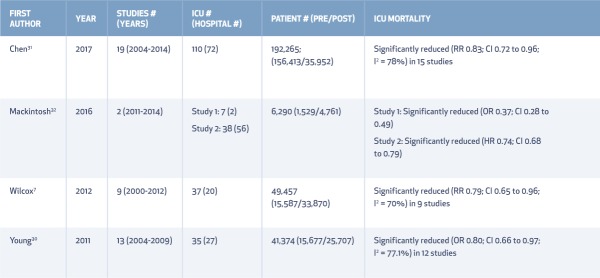
Larger recent studies were more favorable. In 2011, Young et al.'s meta-analysis of 13 studies involving 35 ICUs and 41,374 patients (Table 2)30 showed that tele-ICUs were associated with decreased ICU mortality (pooled OR 0.82, 95% CI 0.66–0.97) and decreased ICU LOS (mean difference −1.26 days, 95% CI −2.21 to −0.30). However, tele-ICU was not associated with lower in-hospital mortality or LOS, and heterogeneity was significant for both ICU (I2 = 77.1%) and hospital mortality (I2 = 84.9%). Similarly, a meta-analysis of 19 trials by Chen et al. found that tele-ICU was associated with reductions in ICU mortality, hospital mortality, and ICU LOS but not with hospital LOS.31
Table 2.
Table 2.
Extended
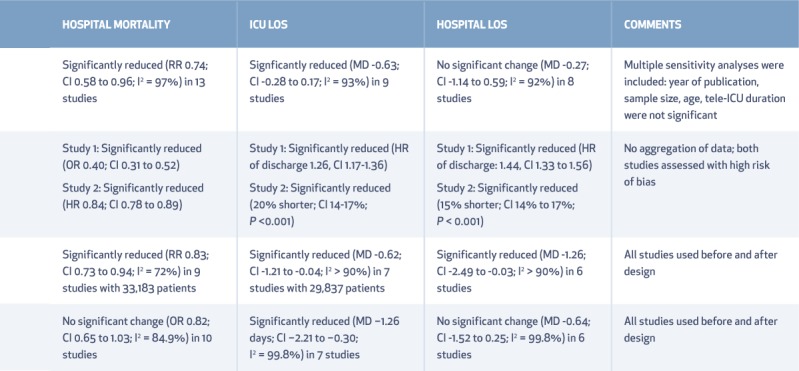
Conversely, a systematic review by Mackintosh et al. in 2016 assessed the impact of tele-ICU programs with 24/7 decision support (Table 2)32 and found decreased hospital mortality (adjusted OR 0.40, 95% CI 0.31–0.52). One of those studies reported pre-post data from 38 hospitals and 56 adult ICUs and found that tele-ICUs were associated with reduced ICU and hospital LOS and mortality.32 Also in 2016, Kahn et al. examined 132 hospitals with tele-ICUs and 389 hospitals without tele-ICUs using CMS data from 2001 to 2010 (Table 2).18 Controlling for hospital size, case-mix, and geographic proximity, they showed that ICU-telemedicine adoption was associated with decreased 90-day mortality compared with non-adopters (ratio of odds ratios = 0.96, 95% CI 0.95–0.98, P < 0.001). Notably, 81.1% of hospitals showed no difference in 90-day mortality. A significant post-adoption 90-day mortality difference was seen in 12.2% of the hospitals, which were more likely to have high volumes and urban location, while 6.1% of the hospitals had increased 90-day mortality.
Cost-Effectiveness
Cost-effectiveness analyses are valuable in determining if tele-ICU optimizes resource allocation in a cost-constrained health system. In 2016, Yoo et al. estimated the incremental cost-effectiveness ratio (ICER) of tele-ICU from the healthcare system perspective using a standard decision model based on published literature.33 Effectiveness was quantified by cumulative quality-adjusted life years (QALYs) gained over 5 years post-ICU discharge. The model estimated tele-ICU to extend 0.011 QALYs with an incremental cost of $516 per patient compared to ICUs without telemedicine, yielding an ICER of $45,320 per additional QALY. The 95% CI range of ICER estimates spanned from −$229,016 to $375,870, reflecting significant variability in key outcomes among the published studies. In a willingness-to-pay context of $100,000 per QALY gained, their analysis estimated that the ICER would fall below this threshold in 66.8% of the simulations. The wide range of ICER estimates reflects how tele-ICU programs in different patient populations and settings have variable impacts on cost and outcomes.
Acceptance of Tele-ICU
Clinician acceptance of tele-ICUs is crucial to ensure favorable clinical and financial outcomes. Studies of acceptance yielded varying results regarding perceptions of increased workload, burdens of continuous monitoring, and potential conflict between bedside providers and tele-ICU staff. These concerns were often mitigated following implementation of a tele-ICU and evolution of effective communication and utilization patterns between the teams.34 A systematic review by Young et al. examined 23 studies about acceptance of tele-ICU and found that 82.3% to 100% of respondents thought telemedicine coverage enhanced quality of care.35 Also, more than 60% of resident physicians who trained in an ICU with telemedicine support reported a desire to work in ICUs with such programs post-residency.
Interhospital Transfers
There is interest in how tele-ICUs affect ICU referral and continuity of care. A supporting hypothesis for tele-ICU has been that it allows less-resourced ICUs to support patients, thus limiting the need for transfers and overuse of tertiary care hospitals. This, however, was challenged in a study by Pannu et al., which found that implementation of a tele-ICU program is associated with an increase in interhospital transfers from less resourced ICUs36; this was not related to illness severity. There was no such increase from ICUs with high-intensity coverage. Similarly, the Cleveland Clinic experience has found no increase in transfers from ICUs with high-intensity coverage. For selected populations (e.g., pediatric ICU patients), tele-ICU appears to be an important tool for consultation and triaging patients.37
Additional Outcomes
Tele-ICU studies have focused on clinical and financial outcomes. Barely explored is the impact on hospital operations, logistics, and support beyond the ICU, such as for rapid response teams. Personnel outcomes may also be relevant, such as intensivist and nurse job satisfaction, backup resources for less-experienced bedside clinicians, or career extension for clinicians physically unable to continue bedside work. These outcomes are important because burnout, for example, continually depletes the existing ICU workforce and exacerbates supply constraints.38 Indeed, early data from the Cleveland Clinic shows more than a 60% decrease in overnight pages and calls to on-call intensivists at covered hospitals. This allows for longer stretches of uninterrupted sleep and improved quality of life.
LIMITATIONS
This narrative review relied on systematic reviews, meta-analyses, and observational studies that were non-blinded, with before-and-after designs and potential risks for bias. We recognized the concerns about overviews of systematic reviews that have been previously described.39 Importantly, early tele-ICU outcomes may be overestimated, affected by other contemporaneous improvements in ICU care (e.g., weaning from mechanical ventilation, sedation management, and sepsis protocols). Other options of ICU coverage now exist—such as nurse practitioners and physician assistants—to augment ICU teams and quality of care.37
Importantly, the benefits of tele-ICU have not been uniformly positive.29 As cited, significant variability exists in ICU and hospital survival as well as LOS among published studies. Implementation of tele-ICUs has been heterogeneous with variable coverage models (24/7, evenings and weekends, or as needed).23 Heterogeneity in outcomes may reflect differences in telemedicine software, process control, training, acceptance, and clinical privileges of tele-ICU intensivists (e.g., limited care management delegation/authority). Given the identified need for high-level research to improve tele-ICU, an expert consensus collaborative has published recommendations targeting key areas for research, including standardized methods for program evaluation, and best practices for optimal outcomes.40
CONCLUSION
Tele-ICUs may serve within a hybrid model of care to support high-intensity coverage and bridge the gap for nocturnal ICU care. Tele-ICU is associated with improved ICU mortality and decreased LOS, albeit with significant heterogeneity among studies. It also has the potential for additional benefits, such as enhancing cardiovascular critical care, reducing interhospital transfers and improving staff satisfaction. Continuing research into best practices for this technology-enhanced model of care and improved understanding of its impact, breadth of outcomes, and cost-effectiveness is prudent.
KEY POINTS
Adoption of tele-ICU is increasing as part of a hybrid model to support high-intensity critical care delivery.
Heterogeneity among studies notwithstanding, tele-ICU is associated with benefits including improved ICU mortality and decreased length of stay.
Although cost-effectiveness of tele-ICU practice has been demonstrated, implementation costs are still high.
Continuing research into best practices for this technology-enhanced model of care is prudent.
Footnotes
Conflict of Interest Disclosure:
The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
REFERENCES
- 1. Lilly CM, Swami S, Liu X, Riker RR, Badawi O.. Five-Year Trends of Critical Care Practice and Outcomes. Chest. 2017. October; 152 4: 723– 35. [DOI] [PubMed] [Google Scholar]
- 2. Neuraz A, Guérin C, Payet C, . et al. Patient Mortality Is Associated With Staff Resources and Workload in the ICU: A Multicenter Observational Study. Crit Care Med. 2015. August; 43 8: 1587– 94. [DOI] [PubMed] [Google Scholar]
- 3. Han L, Sutton M, Clough S, Warner R, Doran T.. Impact of out-of-hours admission on patient mortality: longitudinal analysis in a tertiary acute hospital. BMJ Qual Saf. 2017. September 29 [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Angus DC, Kelley MA, Schmitz RJ, . et al .; Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS) Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000. December 6; 284 21: 2762– 70. [DOI] [PubMed] [Google Scholar]
- 5. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL.. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002. November 6; 288 17: 2151– 62. [DOI] [PubMed] [Google Scholar]
- 6. Wallace DJ, Angus DC, Barnato AE, Kramer AA, Kahn JM.. Nighttime intensivist staffing and mortality among critically ill patients. N Engl J Med. 2012. May 31; 366 22: 2093– 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wilcox ME, Chong CA, Niven DJ, . et al. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. 2013. October; 41 10: 2253– 74. [DOI] [PubMed] [Google Scholar]
- 8. Kerlin MP, Adhikari NK, Rose L, . et al .; ATS Ad Hoc Committee on ICU Organization An Official American Thoracic Society Systematic Review: The Effect of Nighttime Intensivist Staffing on Mortality and Length of Stay among Intensive Care Unit Patients. Am J Respir Crit Care Med. 2017. February 1; 195 3: 383– 93. [DOI] [PubMed] [Google Scholar]
- 9. Kumar K, Singal R, Manji RA, . et al .; Cardiovascular Health Research in Manitoba Investigator Group The benefits of 24/7 in-house intensivist coverage for prolonged-stay cardiac surgery patients. J Thorac Cardiovasc Surg. 2014. July; 148 1: 290– 97.e6. [DOI] [PubMed] [Google Scholar]
- 10. Rosenfeld BA, Dorman T, Breslow MJ, . et al. Intensive care unit telemedicine: alternate paradigm for providing continuous intensivist care. Crit Care Med. 2000. December; 28 12: 3925– 31. [DOI] [PubMed] [Google Scholar]
- 11. Ferrari R. Writing narrative style literature reviews. Medical Writing. 2015. December; 24 4: 230– 5. [Google Scholar]
- 12. Grundy BL, Crawford P, Jones PK, . et al. Telemedicine in critical care: an experiment in health care delivery. JACEP. 1977. October; 6 10: 439– 44. [DOI] [PubMed] [Google Scholar]
- 13. Kahn JM, Cicero BD, Wallace DJ, Iwashyna TJ.. Adoption of ICU telemedicine in the United States. Crit Care Med. 2014. February; 42 2: 362– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lilly CM, Zubrow MT, Kempner KM, . et al .; Society of Critical Care Medicine Tele-ICU Committee Critical care telemedicine: evolution and state of the art. Crit Care Med. 2014. November; 42 11: 2429– 36. [DOI] [PubMed] [Google Scholar]
- 15. Caldarola P, Gulizia MM, Gabrielli D, . et al. ANMCO/SIT Consensus Document: telemedicine for cardiovascular emergency networks. Eur Heart J Suppl. 2017. May; 19 Suppl D: D229– D243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Na SJ, Chung CR, Jeon K, . et al. Association Between Presence of a Cardiac Intensivist and Mortality in an Adult Cardiac Care Unit. J Am Coll Cardiol. 2016. December 20; 68 24: 2637– 48. [DOI] [PubMed] [Google Scholar]
- 17. Kumar G, Falk DM, Bonello RS, Kahn JM, Perencevich E, Cram P.. The costs of critical care telemedicine programs: a systematic review and analysis. Chest. 2013. January; 143 1: 19– 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kahn JM, Le TQ, Barnato AE, . et al. ICU Telemedicine and Critical Care Mortality: A National Effectiveness Study. Med Care. 2016. March; 54 3: 319– 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kahn JM, Gunn SR, Lorenz HL, Alvarez J, Angus DC.. Impact of nurse-led remote screening and prompting for evidence-based practices in the ICU. Crit Care Med. 2014. April; 42 4: 896– 904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hravnak M, Devita MA, Clontz A, Edwards L, Valenta C, Pinsky MR.. Cardiorespiratory instability before and after implementing an integrated monitoring system. Crit Care Med. 2011. January; 39 1: 65– 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM.. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med. 2010. February 22; 170 4: 369– 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kahn JM. Intensive care unit telemedicine: promises and pitfalls. Arch Intern Med. 2011. March 28; 171 6: 495– 6. [DOI] [PubMed] [Google Scholar]
- 23. Dayton E, Henriksen K. Communication failure: basic components, contributing factors, and the call for structure. Jt Comm J Qual Patient Saf. 2007; 33 1: 34– 47. [DOI] [PubMed] [Google Scholar]
- 24. Plumb JJ, Hains I, Parr MJ, Milliss D, Herkes R, Westbrook JI.. Technology meets tradition: The perceived impact of the introduction of information and communication technology on ward rounds in the intensive care unit. Int J Med Inform. 2017. September; 105: 49– 58. [DOI] [PubMed] [Google Scholar]
- 25. Black AD, Car J, Pagliari C, . et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011. January 18; 8 1: e1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lilly CM, Thomas EJ. Tele-ICU: experience to date. J Intensive Care Med. 2010. Jan-Feb; 25 1: 16– 22. [DOI] [PubMed] [Google Scholar]
- 27. Lilly CM, Cody S, Zhao H, . et al .; University of Massachusetts Memorial Critical Care Operations Group Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011. June 1; 305 21: 2175– 83. [DOI] [PubMed] [Google Scholar]
- 28. Breslow MJ, Rosenfeld BA, Doerfler M, . et al. Effect of a multiple-site intensive care unit telemedicine program on clinical and economic outcomes: an alternative paradigm for intensivist staffing. Crit Care Med. 2004. January; 32 1: 31– 8. [DOI] [PubMed] [Google Scholar]
- 29. Thomas EJ, Lucke JF, Wueste L, Weavind L, Patel B.. Association of telemedicine for remote monitoring of intensive care patients with mortality, complications, and length of stay. JAMA. 2009. December 23; 302 24: 2671– 8. [DOI] [PubMed] [Google Scholar]
- 30. Young LB, Chan PS, Lu X, Nallamothu BK, Sasson C, Cram PM.. Impact of telemedicine intensive care unit coverage on patient outcomes: a systematic review and meta-analysis. Arch Intern Med. 2011. March 28; 171 6: 498– 506. [DOI] [PubMed] [Google Scholar]
- 31. Chen J, Sun D, Yang W, . et al. Clinical and Economic Outcomes of Telemedicine Programs in the Intensive Care Unit: A Systematic Review and Meta-Analysis. J Intensive Care Med. 2017. January 1: 885066617726942. [DOI] [PubMed] [Google Scholar]
- 32. Mackintosh N, Terblanche M, Maharaj R, . et al. Telemedicine with clinical decision support for critical care: a systematic review. Syst Rev. 2016. October 18; 5 1: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yoo BK, Kim M, Sasaki T, Melnikow J, Marcin JP.. Economic Evaluation of Telemedicine for Patients in ICUs. Crit Care Med. 2016. February; 44 2: 265– 74. [DOI] [PubMed] [Google Scholar]
- 34. Thomas JT, Moeckli J, Mengeling MA, . et al. Bedside Critical Care Staff Use of Intensive Care Unit Telemedicine: Comparisons by Intensive Care Unit Complexity. Telemed J E Health. 2017. September; 23 9: 718– 25. [DOI] [PubMed] [Google Scholar]
- 35. Young LB, Chan PS, Cram P.. Staff acceptance of tele-ICU coverage: a systematic review. Chest. 2011. February; 139 2: 279– 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pannu J, Sanghavi D, Sheley T, . et al. Impact of Telemedicine Monitoring of Community ICUs on Interhospital Transfers. Crit Care Med. 2017. August; 45 8: 1344– 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kahn JM, Rubenfeld GD. The myth of the workforce crisis. Why the United States does not need more intensivist physicians. Am J Respir Crit Care Med. 2015. January 15; 191 2: 128– 34. [DOI] [PubMed] [Google Scholar]
- 38. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN.. An Official Critical Care Societies Collaborative Statement-Burnout Syndrome in Critical Care Health-care Professionals: A Call for Action. Chest. 2016. July; 150 1: 17– 26 [DOI] [PubMed] [Google Scholar]
- 39. McKenzie JE, Brennan SE. Overviews of systematic reviews: great promise, greater challenge. Syst Rev. 2017. September 8; 6 1: 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kahn JM, Hill NS, Lilly CM, . et al. The research agenda in ICU telemedicine: a statement from the Critical Care Societies Collaborative. Chest. 2011. July; 140 1: 230– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]