Abstract
Background/Aims
People around the world are increasingly choosing to undergo colorectal cancer screening via colonoscopy. As a result, guideline adherence to postpolypectomy colonoscopy surveillance has drawn increasing attention. The present study was performed to assess recognition and adherence to guidelines among primary care physicians and gastroenterologists and to identify characteristics associated with compliance.
Methods
A nationwide sample of primary care physicians employed at cancer screening facilities and registered members of the Korean Society of Gastrointestinal Endoscopy were recruited. Participants were asked to complete a survey of six hypothetical clinical scenarios designed to assess their potential course of action in response to screening or follow-up colonoscopy results. Frequencies and odds ratios and 95% confidence intervals for guideline adherence were estimated.
Results
The proportions of doctors recommending shortened colonoscopy surveillance intervals for low- and high-risk adenomas were greater than 90% among primary physicians and were much lower among gastroenterologists. Guideline adherence was relatively good among groups of doctors who were young, had a specialty in gastroenterology, worked at tertiary hospitals, and cared for an appropriate number of patients.
Conclusions
The present study reveals a remaining discrepancy between practitioner recommendations and current guidelines for postpolypectomy surveillance. Several factors were shown to be related to guideline adherence, suggesting a need for appropriate control and continuing education or training programs among particular groups of practitioners.
Keywords: Colonoscopy, Guideline adherence, Colorectal neoplasms, Early detection of cancer
INTRODUCTION
Colorectal cancer (CRC) screening by colonoscopy has been found to markedly reduce mortality from CRC, with high sensitivity and cost-effectiveness.1–3 Accordingly, colonoscopy rates have grown tremendously in many countries.4–6 Colonoscopy for the purpose of average-risk CRC screening has increased about 3-fold (up to 28.9%) in the United States.7 Meanwhile, Korea has experienced remarkable increases in screening rates for endoscopy by about 2.5-fold (from 14.4% in 2004; up to 35.2% in 2013).8
Cancer screening, or surveillance, involves repeated tests over most of the lifetime of an individual, rather than a transient one-time event.1 The risks and costs associated with screening tests, therefore, cannot be ignored. Balancing these with the benefits of the tests, experts must suggest appropriate guidelines for each individual screening modality, including surveillance intervals. Accordingly, gastrointestinal endoscopists have highlighted the need for a consensus on the optimal surveillance for colonoscopic polypectomy as a leading concern in the lower gastrointestinal endoscopy field.9
To date, several related guidelines have been suggested: the American Cancer Society and the American Gastroenterological Association proposed specific guidelines for colonoscopy surveillance after polypectomy in 2006;10 these were reviewed and updated in 2012 with support from more qualified evidence.11 A European study group and experts also have reported and developed appropriate guidelines.12,13 In Korea, the necessity for domestic guidelines has been continuously stressed, and several suggestions have been made.14,15
One concerning issue related with the above recommendations is guideline adherence, specifically in regards to adherence to surveillance intervals. Despite a continuing effort to lengthen intervals for follow-up colonoscopy, a number of surveys have indicated that most doctors still recommend more frequent surveillance colonoscopy than guidelines suggest.11,16–19 In Korea, a recent study reported by Sohn and Colonoscopy Study Group of the Korean Society of Coloproctology19 identified a need to evaluate discrepancies between guidelines and actual clinical practices among the nation’s doctors.
In the current study, a nationwide survey was conducted among primary care physicians and gastroenterologists, respectively, to ascertain their recognition of and recommendations for CRC screening and surveillance in clinical practice. The purpose of this study was to summarize and update understanding of their recommendations on colonoscopic surveillance intervals after polypectomy in comparison to current guidelines. Additionally, we aimed to outline characteristics associated with guideline adherence among the doctors.
MATERIALS AND METHODS
1. Study population
The survey described below was administered to a nationwide sample of primary care physicians at cancer screening facilities and to registered members of the Korean Society of Gastrointestinal Endoscopy. First, the target sizes of sampling units were calculated according to strata of geographic areas for 2,206 cancer screening facilities at the primary care level throughout the country. The printed survey questionnaire was mailed to the participants, and final responses were obtained from 241 respondents employed at 236 facilities. Second, specialists in gastroenterology were recruited through an online survey method. A total of 5,969 members (4,912 males and 1,057 females) of the Korean Society of Gastrointestinal Endoscopy were asked to participate in the survey. At the end of the recruitment period, completed survey entries with valid responses were obtained from 138 gastroenterologists (105 males and 33 females) and were included for analysis. Written informed consents were gained and ethical approval was obtained from the Institutional Review Board of the National Cancer Center, Korea (IRB number: NCCNCS08129).
2. Exposures and outcomes
For the purpose of assessing awareness and current practices for CRC screening among Korean doctors, a 7-page survey questionnaire, including a 1-page cover letter, was developed and administered to the study participants. For specific assessment and comparison with comparable international results, six hypothetical clinical scenarios based on the findings of a screening colonoscopy in a 55-year-old man were included in the questionnaire: the six scenarios were previously developed by Boolchand et al.18 in 2006. Respondents were asked to recommend follow-up colonoscopy surveillance intervals for each scenario. Details on the hypothetical questions and answer choices have been described elsewhere.18 As a reference, the primary standard guidelines were the Korean guidelines suggested in 2012 by the Korean Multi-Society Take Force;14,15 for instances in which foreign guidelines suggest longer follow-up intervals than the Korean guidelines do, we also included them into the reference range for judging the respondents’ adherence.
3. Statistical analysis
For the respondents, age and years in practice were categorized into 10-year interval groups. Distributions of general characteristics among the respondents were analyzed separately for the primary physicians and gastroenterologists. Frequencies of different responses to each question on the survey were also calculated.
Sample weights were generated based on distributions within geographic areas for primary care physicians and based on age and sex distributions for members of the Korean Society of Gastrointestinal Endoscopy for the gastroenterologists. These weights were incorporated into the SURVEYFREQ procedure incorporated in SAS software. Differences in frequencies were tested by the Rao-Scott modified chi-square test. All reported p-values were two-sided and considered statistically significant when p<0.05.
Both crude and adjusted odds ratios for adhering to guidelines on surveillance colonoscopy intervals after polypectomy were calculated by logistic regression models with sample weights, using the SURVEYLOGISTIC procedure. The multivariate logistic model included the following variables: practitioner’s age, sex, specialty, and medical facility type, as well as the number of patients seen per 1 day. All analyses were conducted using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
A total of 379 Korean doctors (241 primary care physicians and 138 gastroenterologists) responded to the survey (Table 1). The overall mean age was 45.0 years (range, 31 to 67 years); the primary care physicians were slightly older (46.9±7.2 years) than the gastroenterologists (41.8±6.5 years). More than 80% of the respondents were male, and the majority of the respondents had their specialty in internal medicine, even after excluding the specialists in gastroenterology. The most common type of medical facility at which the study participants were employed was a clinic, followed by a tertiary hospital.
Table 1.
Characteristics of Survey Respondents
| Characteristic | Primary physicians | Gastroenterologists | p-value* |
|---|---|---|---|
| Overall response | 241 (63.6) | 138 (36.4) | |
| Sex | 0.106 | ||
| Male | 215 (88.6) | 105 (81.9) | |
| Female | 26 (11.4) | 33 (18.1) | |
| Age, yr | 0.013 | ||
| 30–39 | 34 (15.2) | 59 (24.6) | |
| 40–49 | 121 (49.3) | 61 (32.5) | |
| ≥50 | 86 (35.5) | 18 (42.8) | |
| Years in practice† | 0.298 | ||
| <10 | 16 (6.1) | 29 (12.1) | |
| 10–19 | 93 (40.7) | 72 (34.6) | |
| 20–29 | 100 (40.6) | 33 (44.2) | |
| ≥30 | 30 (12.7) | 4 (9.0) | |
| Specialty | NA | ||
| Gastroenterology | 0 | 138 (100.0) | |
| General internal medicine | 195 (80.3) | 0 | |
| General surgery | 28 (11.6) | 0 | |
| Family medicine | 12 (5.5) | 0 | |
| Others | 6 (2.6) | 0 | |
| Type of medical facility | NA | ||
| Clinic | 240 (99.5) | 28 (24.7) | |
| Hospital | 1 (0.5) | 14 (8.6) | |
| General hospital | 0 | 30 (20.6) | |
| Tertiary hospital | 0 | 66 (46.1) | |
| No. of patients/day | <0.001 | ||
| <25 | 13 (5.9) | 25 (13.0) | |
| 25–49 | 50 (21.8) | 59 (37.1) | |
| 50–99 | 142 (58.3) | 50 (45.8) | |
| ≥100 | 36 (14.0) | 4 (4.2) |
Data are presented as unweighted numbers (weighted proportions).
NA, not available.
Rao-Scott modified chi-square test;
Missing: 2.
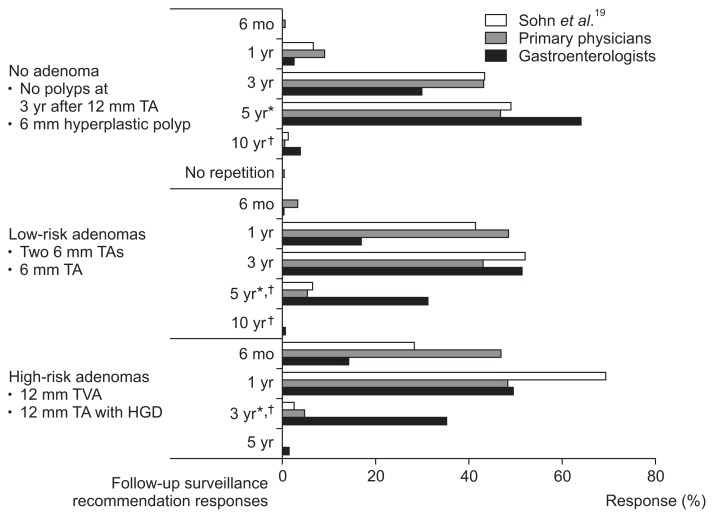
Table 2 shows the distributions of the answers from all respondents to each clinical scenario on follow-up colonoscopy interval recommendations. A large numbers of participants (from 36.0% to 83.5% of all respondents) responded with an earlier follow-up schedule than that recommend in current guidelines for each scenario. Fig. 1 depicts the responses according to the respondent’s specialty, along with results from a previous study using the same questions, separately according to risk classification of baseline colonoscopy findings. The discrepancy between the current guidelines and responses from the doctors overall was distinct for every risk level of baseline colonoscopy findings. The proportions of gastroenterologists who replied with shorter intervals than recommended by the reference guidelines were 32.3%, 68.3%, and 63.5% for cases of no adenoma, low-risk adenomas, and high-risk adenomas, respectively. Those for primary physicians were 52.8%, 94.6%, and 95.1%, respectively.
Table 2.
Responses from Korean Doctors on Postpolypectomy Follow-up Surveillance Recommendations in Comparison to Guideline Recommendations
| Clinical scenario | Recommendation in Korean guidelines, yr | Responses on follow-up surveillance intervals | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| 6 mo | 1 yr | 3 yr | 5 yr | 10 yr | No repetition | ||
| 6-mm Hyperplastic polyp | 5* | 1 (0.2) | 33 (7.0) | 124 (28.9) | 210 (61.1) | 9 (2.7) | 1 (0.2) |
| 6-mm TA | 5† | 4 (0.7) | 117 (26.9) | 182 (48.6) | 71 (23.5) | 1 (0.3) | 0 |
| 12-mm TA with HGD | 3 | 163 (34.1) | 168 (49.4) | 44 (15.8) | 2 (0.7) | 0 | 0 |
| 12-mm TVA | 3 | 99 (20.2) | 191 (48.4) | 84 (30.3) | 3 (1.0) | 0 | 0 |
| Two 6-mm TAs | 5† | 13 (2.2) | 150 (31.8) | 157 (47.3) | 55 (18.3) | 1 (0.4) | 0 |
| No polyps in a patient with a 12-mm TA 3 yr earlier | 5* | 2 (0.4) | 18 (3.2) | 159 (41.4) | 196 (52.9) | 3 (2.1) | 0 |
Data are presented as unweighted numbers (weighted proportions). Non-respondents to each question were excluded.
TA, tubular adenoma; HGD, high-grade dysplasia; TVA, tubulovillous adenoma.
The U.S. Multi-Society Task Force recommends an interval of 10 years; the European panel (EPAGE II) recommends 5.5 years;
The U.S. Multi-Society Task Force recommends an interval of 5–10 years; the European panel (EPAGE II) recommends 5 years.
Fig. 1.
Distribution of postpolypectomy follow-up surveillance responses.
TA, tubular adenoma; TVA, tubulovillous adenoma; HGD, high-grade dysplasia. *Recommended intervals in Korean guidelines; †Recommended intervals in the U.S. Multi-Society Task Force guideline.
The characteristics of the doctors that were found to be related with guideline adherence to follow-up colonoscopy surveillance intervals are outlined in Table 3. Having a specialty in gastroenterology was significantly associated with guideline adherence, compared to all of other specialties respectively. Older age, working at non-training hospitals, and caring for too many patients in a day remained as significant factors negatively affecting guideline adherence in multivariate analysis, after adjusting for other covariates.
Table 3.
Odds Ratios for Recommending an Appropriate Follow-up Colonoscopic Surveillance Interval in Comparison to Current Guidelines*
| Characteristic | Crude OR | Adjusted OR† | ||
|---|---|---|---|---|
|
|
|
|||
| Estimates | (95% CI) | Estimates | (95% CI) | |
| Sex | ||||
| Male | 1.00 | Reference | 1.00 | Reference |
| Female | 0.63 | (0.48–0.84) | 0.97 | (0.69–1.38) |
| Age, yr | ||||
| 30–39 | 1.00 | Reference | 1.00 | Reference |
| 40–49 | 0.54 | (0.43–0.67) | 0.53 | (0.40–0.72) |
| ≥50 | 0.52 | (0.37–0.74) | 0.50 | (0.34–0.75) |
| Specialty | ||||
| Gastroenterology | 1.00 | Reference | 1.00 | Reference |
| General internal medicine | 0.33 | (0.26–0.41) | 1.57 | (0.92–2.70) |
| General surgery | 0.13 | (0.08–0.23) | 0.70 | (0.33–1.51) |
| Family medicine or others | 0.18 | (0.09–0.35) | 0.93 | (0.40–2.17) |
| Type of medical facility | ||||
| Clinic | 0.11 | (0.08–0.15) | 0.09 | (0.05–0.17) |
| Hospital | 0.22 | (0.13–0.39) | 0.18 | (0.11–0.31) |
| General hospital | 0.38 | (0.23–0.61) | 0.35 | (0.21–0.58) |
| Tertiary hospital | 1.00 | Reference | 1.00 | Reference |
| No. of patients/day | ||||
| <25 | 0.91 | (0.61–1.34) | 0.58 | (0.34–1.00) |
| 25–49 | 1.00 | Reference | 1.00 | Reference |
| 50–99 | 0.87 | (0.65–1.15) | 1.09 | (0.77–1.54) |
| ≥100 | 0.23 | (0.14–0.35) | 0.54 | (0.32–0.91) |
OR, odds ratio; CI, confidence interval.
Adequate intervals include recommendations of the Korean and other international (U.S. and Europe) guidelines;
Adjusted for sex, age, specialty, type of medical facility, and number of patients per day.
DISCUSSION
In this nationwide survey, we found that most Korean practitioners tend to recommend shorter intervals for follow-up colonoscopy after a polypectomy than recommended in current guidelines. Adherence to guidelines on follow-up colonoscopy was relatively good among groups of doctors who were young, had specialty in gastroenterology, worked at tertiary hospitals, and took care of a proper number of patients. This study demonstrated the suspected discrepancy between established guidelines and actual clinical practice in postpolypectomy surveillance intervals among Korean doctors, via a nationally representative survey, for the first time.
A number of surveys have been conducted in other countries (mainly in the United States) to evaluate adherence to surveillance recommendations after polypectomy for colonoscopy screening.17–28 In Korea, Kang et al.29 surveyed intervals of postpolypectomy colonoscopy surveillance in practice among 131 Korean colonoscopists in 2006. Similar with reports from other studies, the study revealed that most of the doctors performed follow-up colonoscopy within shorter intervals than recommended. The authors explained that the most frequent reason for the lack of adherence with surveillance guidelines was concern for a missed polyp, according to survey results; the second reason for non-compliance was the relatively low cost of colonoscopy in Korea. Recently, Hong et al.30 investigated the practical state of postpolypectomy surveillance performance among Korean doctors, providing suggestions for Korean guidelines on postpolypectomy colonoscopic surveillance thereafter in 2011.14,31 They also reported a significant disagreement between actual practices and preferred guidelines. In 2012, Sohn and Colonoscopy Study Group of the Korean Society of Coloproctology19 reported results from a survey of members of the Korean Surgical Society using the questionnaire developed by Boolchand et al.18 They also described the use of intervals shorter than those recommended in guidelines. However, the authors of those studies mentioned limitations in their study of a relatively small number of doctors confined to a certain specialty, without any information on characteristics of the respondents.
The present study discovered shorter surveillance intervals comparable to those in the reports described above. Going further, however, we also identified characteristics related to guideline adherence. Unlike most related studies in the literature, our survey was carried out in both primary care physicians (internal medicine, general surgery, and family medicine) and specialists in gastroenterology. This allowed us to compare differences in screening recommendations according to various specialties and types of medical facilities at which the participants were employed. Our results stress the importance of training on the basis of evidence-based medicine for guideline adherence, because younger doctors who specialized in gastroenterology and who worked in tertiary or training hospitals showed better adherence than older doctors who had longer clinical experience.
For more detailed assessment of reasons for the respondents’ nonadherence to guidelines, we additionally analyzed responses to questions design to measure the respondents’ basic knowledge and behaviors regarding colonoscopic follow-up guidelines. To do so, we asked the doctors about appropriate surveillance intervals and their actual choices in practice upon obtaining normal colonoscopy findings. This enabled us to outline actual causes for recommending shorter intervals in each scenario, whether the doctors were ignorant about guidelines or whether there were other reasons for them not to follow established guidelines. We found that, on average, only about 11.1% of the respondents who recommended shorter surveillance intervals in each of the six scenarios demonstrated ignorance of the typical contents of the guidelines, whereas approximately 28.5% could be interpreted as disobedience or intentional shortening of follow-up intervals despite exhibiting basic knowledge of the guidelines. The percentages of the latter instances were much higher for ‘no adenoma’ scenarios (35.7% and 38.6%) and lower in ‘low- and high-grade adenoma’ scenarios (ranged from 25.1% to 26.9%). The respondents who appeared to deliberately disobey guidelines reported much stronger agreement with statements such as, “It is possible to overlook CRC during colonoscopy, and I feel some pressure of false-negatives,” or, “Colonoscopy is easy to recommend without regard for cost,” than others. This coincides with previous explanations about the reasons for shortened surveillance intervals, which include concern for interval cancer and the low cost of the examination in Korea: it was suggested that such reasons or factors would be more strongly related to nonadherence than unawareness or ignorance of recommended guidelines.
As was observed in the present study, previous studies have also reported significant shortening of surveillance intervals in cases of no adenoma or low-grade adenoma resection than in cases of high-grade adenoma resection.18,21,25 Interestingly, whereas colonoscopy is often found to be overused for low-risk or no adenomas, underuse of colonoscopy appears to be somewhat common for high-risk adenomas.22,23,28 When compared to a previous survey carried out in Korea, which was confined to summarize the practical status of postpolypectomy surveillance among doctors, rather than to measure it against established guidelines, our study showed relatively longer follow-up intervals, indicating better agreement to current guidelines.
The Korean guidelines developed by the Korean multi-society taskforce composed of the Korean Society of Gastroenterology and the Korean Society of Gastrointestinal Endoscopy14 differ from guidelines suggested by the U.S. Multi-Society Task Force (USMSTF).11 Korean guidelines were established upon systematic review and meta-analysis, along with obtaining expert opinions, to represent the characteristics of the Korean population and the medical environment in Korea.14 The Korean guidelines recommend 5-year and 3-year intervals for follow-up after resection of low-risk and high-risk adenoma, respectively, and 5-year intervals in cases of no adenoma or hyperplastic polyp. Meanwhile, although USMSTF guidelines give the same recommendations for high-risk adenoma, they allow for up to 10-year intervals for low-risk adenomas and negative findings. In contrast, the Korean Society of Coloproctology in 2012 recommended a 3-year surveillance interval after low-risk adenomas and a 1-year interval after high-risk adenomas,32 which could be a reason for the generally shortened intervals. This approach can be more reasonable when multiple high-risk findings are found in baseline colonoscopy examination.33
Concerns for an overlooked polyp or interval cancer seemed to be a major factor that affects the overuse of surveillance colonoscopy. However, such shortening or guidelines with shortened recommended intervals oppose recent efforts to lengthen surveillance intervals in light of increasing evidence on the benefits thereof. As Kang et al.29 emphasized in their paper, hastening the timing of follow-up due to fear of a missed polyp, when the endoscopic examination was performed adequately, is unwarranted. However, concerns for the quality of previous colonoscopy or completeness of polypectomy can be other plausible causes for shortened intervals,14 which stresses the importance of confirming the quality of colonoscopic examinations. On the other hand, ignorance of standard guidelines could be another reason for non-compliance, and thus, promotion and education on appropriate guidelines are needed.
There are several limitations in our study that should be considered. First, the results were obtained from doctors’ responses to a survey questionnaire, not from objective data; therefore, we found it difficult to reflect upon more specific patient or examination factors, including complex clinical conditions or observed findings, affecting the practical decisions. Also, response rates for the survey were low, especially among the gastroenterologist group. This could introduce selection bias in that the respondents may have had better adherence with standard guidelines than non-respondents. We carried out the survey through two methods, via a hard copy or online, and a potential bias could occur because of differences in the means of data collection. In addition, it was difficult to exactly figure out the reasons for non-compliance, whether it was due to lack of knowledge or due to other reasons for disobedience or intentional shortening of follow-up intervals despite exhibiting basic knowledge of guidelines. Regarding this problem, we could not obtain on-site or objective data; instead, we inferred them indirectly from the responses of other survey questions. It seems necessary to identify reasons for lack of adherence, because it can be helpful to develop and implement appropriate interventions.
Despite these limitations, the present study is the first nationwide survey on colonoscopic surveillance among the Korean doctors of various medical backgrounds after the Korean guidelines were suggested. Also, we concretely evaluated discrepancies between current guidelines and the actual recommendations doctors give for no adenoma, low-risk adenoma, and high-risk adenoma. Overall, this study revealed a lack of guideline awareness or adherence prevalent among Korean doctors, suggesting that proper evidence and interventions are needed to establish appropriate colonoscopic surveillance intervals. Guideline promotion and education to address ignorance and structured or evidence-based training to address distrust of guidelines or the fear of interval cancer may be warranted. Various environments that can influence doctors’ behavior, such as practical customs in medical communities or proper quality of the index colonoscopic examination, need to be reviewed, controlled, and assured. Similarly, the impact of policies or systems in Korea, such as third-party payment and reimbursement system, financial incentives, or health care delivery systems, should also be taken into account together with cooperation among practitioners and policy makers.
In summary, we demonstrated that the majority of Korean doctors fail to adhere to current guidelines on postpolypectomy colonoscopy surveillance intervals, including both primary care physicians and gastroenterologists. Consolidation of Korean-specific guidelines, followed by proper education and training of practitioners, should be sought to improve guideline adherence and to establish unified practice. Our study also highlighted factors predictive of shortened follow-up colonoscopy intervals that may be of use in devising educational programs tailored to the groups of doctors with noted characteristics.
ACKNOWLEDGEMENTS
This study was supported by a Grant-in-Aid for Cancer Research and Control from the National Cancer Center of Korea (#1610402).
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Inadomi JM. Screening for colorectal neoplasia. N Engl J Med. 2017;376:149–156. doi: 10.1056/NEJMcp1512286. [DOI] [PubMed] [Google Scholar]
- 2.Bresalier RS. Early detection of and screening for colorectal neoplasia. Gut Liver. 2009;3:69–80. doi: 10.5009/gnl.2009.3.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sonnenberg A, Delcò F, Inadomi JM. Cost-effectiveness of colonoscopy in screening for colorectal cancer. Ann Intern Med. 2000;133:573–584. doi: 10.7326/0003-4819-133-8-200010170-00007. [DOI] [PubMed] [Google Scholar]
- 4.Pox C, Schmiegel W, Classen M. Current status of screening colonoscopy in Europe and in the United States. Endoscopy. 2007;39:168–173. doi: 10.1055/s-2007-966182. [DOI] [PubMed] [Google Scholar]
- 5.Zapka J, Klabunde CN, Taplin S, Yuan G, Ransohoff D, Kobrin S. Screening colonoscopy in the US: attitudes and practices of primary care physicians. J Gen Intern Med. 2012;27:1150–1158. doi: 10.1007/s11606-012-2051-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Altobelli E, Lattanzi A, Paduano R, Varassi G, di Orio F. Colorectal cancer prevention in Europe: burden of disease and status of screening programs. Prev Med. 2014;62:132–141. doi: 10.1016/j.ypmed.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Lieberman DA, Williams JL, Holub JL, et al. Colonoscopy utilization and outcomes 2000 to 2011. Gastrointest Endosc. 2014;80:133–143. doi: 10.1016/j.gie.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 8.Suh M, Choi KS, Park B, et al. Trends in cancer screening rates among Korean men and women: results of the Korean National Cancer Screening Survey, 2004–2013. Cancer Res Treat. 2016;48:1–10. doi: 10.4143/crt.2014.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rees CJ, Ngu WS, Regula J, et al. European Society of Gastrointestinal Endoscopy: establishing the key unanswered research questions within gastrointestinal endoscopy. Endoscopy. 2016;48:884–891. doi: 10.1055/s-0042-110398. [DOI] [PubMed] [Google Scholar]
- 10.Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130:1872–1885. doi: 10.1053/j.gastro.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 11.Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143:844–857. doi: 10.1053/j.gastro.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Arditi C, Gonvers JJ, Burnand B, et al. Appropriateness of colonoscopy in Europe (EPAGE II): surveillance after polypectomy and after resection of colorectal cancer. Endoscopy. 2009;41:209–217. doi: 10.1055/s-0028-1119646. [DOI] [PubMed] [Google Scholar]
- 13.Hassan C, Quintero E, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2013;45:842–851. doi: 10.1055/s-0033-1344548. [DOI] [PubMed] [Google Scholar]
- 14.Yang DH, Hong SN, Kim YH, et al. Korean guidelines for postpolypectomy colonoscopy surveillance. Clin Endosc. 2012;45:44–61. doi: 10.5946/ce.2012.45.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee BI, Hong SP, Kim SE, et al. Korean guidelines for colorectal cancer screening and polyp detection. Clin Endosc. 2012;45:25–43. doi: 10.5946/ce.2012.45.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saini SD, Nayak RS, Kuhn L, Schoenfeld P. Why don’t gastroenterologists follow colon polyp surveillance guidelines? Results of a national survey. J Clin Gastroenterol. 2009;43:554–558. doi: 10.1097/MCG.0b013e31818242ad. [DOI] [PubMed] [Google Scholar]
- 17.Mysliwiec PA, Brown ML, Klabunde CN, Ransohoff DF. Are physicians doing too much colonoscopy? A national survey of colorectal surveillance after polypectomy. Ann Intern Med. 2004;141:264–271. doi: 10.7326/0003-4819-141-4-200408170-00006. [DOI] [PubMed] [Google Scholar]
- 18.Boolchand V, Olds G, Singh J, Singh P, Chak A, Cooper GS. Colorectal screening after polypectomy: a national survey study of primary care physicians. Ann Intern Med. 2006;145:654–659. doi: 10.7326/0003-4819-145-9-200611070-00007. [DOI] [PubMed] [Google Scholar]
- 19.Sohn DK Colonoscopy Study Group of the Korean Society of Coloproctology. A survey of colonoscopic surveillance after polypectomy. Ann Coloproctol. 2014;30:88–92. doi: 10.3393/ac.2014.30.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson JC, Baron JA, Ahnen DJ, et al. Factors associated with shorter colonoscopy surveillance intervals for patients with low-risk colorectal adenomas and effects on outcome. Gastroenterology. 2017;152:1933–1943.e5. doi: 10.1053/j.gastro.2017.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krist AH, Jones RM, Woolf SH, et al. Timing of repeat colonoscopy: disparity between guidelines and endoscopists’ recommendation. Am J Prev Med. 2007;33:471–478. doi: 10.1016/j.amepre.2007.07.039. [DOI] [PubMed] [Google Scholar]
- 22.Laiyemo AO, Pinsky PF, Marcus PM, et al. Utilization and yield of surveillance colonoscopy in the continued follow-up study of the polyp prevention trial. Clin Gastroenterol Hepatol. 2009;7:562–567. doi: 10.1016/j.cgh.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schoen RE, Pinsky PF, Weissfeld JL, et al. Utilization of surveillance colonoscopy in community practice. Gastroenterology. 2010;138:73–81. doi: 10.1053/j.gastro.2009.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ransohoff DF, Yankaskas B, Gizlice Z, Gangarosa L. Recommendations for post-polypectomy surveillance in community practice. Dig Dis Sci. 2011;56:2623–2630. doi: 10.1007/s10620-011-1791-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Radaelli F, Paggi S, Bortoli A, De Pretis G Italian Association of Hospital Gastroenterologists (AIGO) Overutilization of post-polypectomy surveillance colonoscopy in clinical practice: a prospective, multicentre study. Dig Liver Dis. 2012;44:748–753. doi: 10.1016/j.dld.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Kruse GR, Khan SM, Zaslavsky AM, Ayanian JZ, Sequist TD. Overuse of colonoscopy for colorectal cancer screening and surveillance. J Gen Intern Med. 2015;30:277–283. doi: 10.1007/s11606-014-3015-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Menees SB, Elliott E, Govani S, Anastassiades C, Schoenfeld P. Adherence to recommended intervals for surveillance colonoscopy in average-risk patients with 1 to 2 small (<1 cm) polyps on screening colonoscopy. Gastrointest Endosc. 2014;79:551–557. doi: 10.1016/j.gie.2014.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy CC, Sandler RS, Grubber JM, Johnson MR, Fisher DA. Underuse and overuse of colonoscopy for repeat screening and surveillance in the Veterans Health Administration. Clin Gastroenterol Hepatol. 2016;14:436–444.e1. doi: 10.1016/j.cgh.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang MS, Park DI, Park JH, et al. A survey on the interval of post-polypectomy surveillance colonoscopy. Korean J Gastrointest Endosc. 2006;33:339–345. [Google Scholar]
- 30.Hong SN, Yang DH, Kim YH, et al. A survey for post-polypectomy surveillance. Intest Res. 2011;9:118–128. doi: 10.5217/ir.2011.9.2.118. [DOI] [Google Scholar]
- 31.Hong SN, Yang DH, Kim YH, et al. Korean guidelines for post-polypectomy colonoscopic surveillance. Korean J Gastroenterol. 2012;59:99–117. doi: 10.4166/kjg.2012.59.2.99. [DOI] [PubMed] [Google Scholar]
- 32.Jeong SY, Sohn DK, Moon SH. Guideline for colorectal polyp management. 64th Annual Congress of the Korean Surgical Society; Seoul: Korean Surgical Society; 2012. pp. 256–257. [Google Scholar]
- 33.Lee SM, Kim JH, Sung IK, Hong SN. The risk of metachronous advanced colorectal neoplasia rises in parallel with an increasing number of high-risk findings at baseline. Gut Liver. 2015;9:741–749. doi: 10.5009/gnl14210. [DOI] [PMC free article] [PubMed] [Google Scholar]