Abstract
Growing evidence suggests that workload has an adverse effect on quality of care and patient safety in nursing homes. A novel job resource that may improve quality of care and patient safety and alleviate the negative effect of workload in nursing homes is team support for strengths use. This refers to team members’ beliefs concerning the extent to which the team they work in actively supports them in applying their individual strengths at work. The objective was to investigate the relationships between workload, team support for strengths use, quality of care, and patient safety in nursing homes. We collected (cross-sectional) survey data from 497 caregivers from 74 teams in seven different nursing homes. The survey included measures on perceived workload, team support for strengths use, caregivers’ perception of the quality of care provided by the team and four safety incidents (i.e. fall incidents, medication errors, pressure ulcers, incidents of aggression). After controlling for age, team size, team tenure, organizational tenure, and nursing home, multilevel regression analyses (i.e. individual and team level) showed that perceived workload was not significantly related to perceived team-based quality of care and the frequency of safety incidents. Team support for strengths use was positively related to perceived team-based quality of care, negatively related to medication errors, but not significantly related to fall incidents, pressure ulcers, and aggression incidents. Finally, we found that perceived workload had a negative effect on perceived team-based quality of care when team support for strengths use is low and no significant effect on perceived team-based quality of care when team support for strengths use is high. This study provides promising evidence for a novel avenue for promoting team-based quality of care in nursing homes.
Introduction
Concerns about workload in nursing homes have increased in the past few decades. Nursing homes deal with an increasing workload due to the rising number of elderly people, financial difficulties, understaffing, increased complexity of care, and higher expectations regarding the quality of care [1]. Excessive workload is associated with undesirable outcomes and is internationally recognized as an urgent topic [2–9]. Scholaski et al. [10] showed that workload has a negative effect on nurse-perceived quality of care and patient safety and several studies show that the workload of nurses has an adverse effect on patient safety issues such as infections [3], patient falls,[4] medication errors [4], and patient mortality [2, 5, 6]. Because caregivers interact intensively with the patient, they are able to assess the patient’s condition and listen to any concerns that the patient may voice [11]. However, when confronted with a high workload caregivers may not have the time to assess the psychosocial and physical status of patients due to limited opportunities to interact with patients and other caregivers [11, 12]. This may hinder the proactive care that detects early signs of clinical deterioration or complications and arranges follow-up interventions, resulting in leaving at least one essential task undone [11, 12]. Consequently, quality of care and patient safety will be diminished [11–14].
Team support for strengths use
Job resources refer to the physical, psychological, social, or organizational aspects of the job that facilitate the achievement of work goals and counteract the strain associated with job demands [15, 16]. In this paper, we argue that team support for strengths use is a novel job resource that may improve the quality and safety of care in nursing homes. It refers to team members’ beliefs concerning the extent to which the team they work in actively supports them in applying their individual strengths at work [17, 18]. Individual strengths are trait-like abilities that potentially allow a person to perform at their personal best [19]. When applied, strengths are personal assets that can buffer against stressors and help a person to overcome setbacks [20]. For instance, a nurse with a good sense of humor can make use of this strength to calm a patient in distress. Recent studies have shown that support for the use of strengths is a resource that facilitates job performance and alleviates the negative effects of job demands [21, 22].
In nursing homes, the team is an important contextual factor [23] that may influence whether caregivers are able to leverage their strengths. If team members know what strengths their co-workers have and tasks are allocated in line with their unique qualities, caregivers might be better able to leverage their strengths at work [21, 22]. For instance, in a nursing home team, nurses may stimulate self-management by training patients in the necessary skills or by their interactions with individual patients during daily activities. When a team offers strengths-use support, a nurse whose strength is social intelligence could choose to enhance patient self-management by engaging in social interaction, potentially freeing other team members to enhance self-management in ways that better suit their own strengths.
Employees who feel supported to use their strengths can be more authentic [24], resulting in lower levels of stress and higher levels of energy and coping skills [25]. Therefore, caregivers who work in a team that offers strengths-use support may experience fewer error-inducing conditions such as stress and fatigue which may lead to a higher quality and safety of care delivery [24–26]. Moreover, these caregivers are more likely to appreciate their colleagues for their strengths, thereby potentially creating a blame-free environment in which caregivers are willing to report errors and develop strategies to improve the quality and safety of care [26].
The moderating role of team support for strengths use
Baethge, Muller, and Rigotti show that nurses who focus their resources on specific goals as opposed to spreading them across multiple goals are better able to maintain performance while facing a high workload [27]. In line with this principle, we also expect that caregivers who can capitalize on their strengths, instead of having to be a jack of all trades, can better maintain the quality and safety of care when confronted with a high workload. These caregivers experience higher levels of self-esteem because they feel valued for their unique qualities that they bring to the team [19]. In turn, enhanced self-esteem compensates for the threats to self-esteem that occur in response to the appraisal of stress resulting from a high workload, making caregivers more effective in coping with high job demands [28]. Furthermore, emotional or distressing situations cause less stress when caregivers can approach these situations from their own strengths. In the previous example of the nurse, enhancing patient self-management in addition to other tasks may add to the workload, but it will be less stressful if the nurse can choose to deal with this task in line with his/her individual strengths. Using team support for strengths use as a coping strategy helps caregivers deal with high workload as it creates the ability to alleviate stress [29]. Buffering or reducing the stress level of caregivers within a team is generally seen as an effective way to reduce safety errors and improve the quality of care provided by the team [29].
Aim
The aim of this study was to investigate the relationships between perceived workload, team support for strengths use, the perception of the quality of care provided by the team, and the four most frequently registered indicators of patient safety in Dutch nursing homes, namely fall incidents, medication errors, pressure ulcers, and aggression incidents [29].
Hypothesis 1: Perceived workload is negatively related to (a) perceived team-based quality of care and positively related to perceived frequency of (b) fall incidents, (c) medication errors, (d) pressure ulcers, and (e) aggression incidents.
Hypothesis 2: Team support for strengths use is positively related to (a) perceived patient safety and negatively related to perceived frequency of (b) fall incidents, (c) medication errors, (d) pressure ulcers, and (e) aggression incidents.
Hypothesis 3: Team support for strengths use weakens the relationship between perceived workload on the one hand and perceived (a) team-based quality of care, (b) fall incidents, (c) medication errors, (d) pressure ulcers, and (e) aggression incidents on the other hand.
Methods
Field of study
The way in which nursing homes are organized and financed differs per country. For instance, Dutch nursing homes are relatively large, with an average of approximately 189 beds in comparison to an average of 107 beds in US nursing homes. In addition, the majority of caregivers in Dutch nursing homes are licensed practical nurses, whereas in US nursing homes certified aides form the majority of the staff. Registered nurses are more common in US nursing homes in comparison to Dutch nursing homes [30–33]. However, in spite of these differences, in most developed countries with high life expectancy (such as the Netherlands, Belgium, Denmark, Germany, and US), nursing homes face similar issues that increase the workload, such as an increase in number of elderly people (with multiple chronic diseases), financial restrictions, understaffing, and increased quality expectations [33, 34]. As a response to those issues, a major trend in Europe is the marketization and privatization of nursing homes, which is similar to the well-established pattern in the US. Nevertheless, currently the majority of Dutch nursing homes are non-profit organizations, whereas for-profit nursing homes form the majority of US nursing home [33, 34].
Sample
For this study ‘Strengthening Patient Safety in Nursing Homes’ (i.e. SPS4NH) we conducted a cross-sectional survey amongst nursing homes in the Netherlands that were part of our personal network. Seven nursing homes agreed to participate in a cross-sectional survey with several teams of nurse aides, registered nurses, and licensed practical nurses. In some cases, occupational, speech, and physical therapists were also members of the team. We asked the HR director and/ or the unit managers of the nursing homes to select participating teams that were representative for their whole organization in terms of type of patients and type of teams. The nursing homes were located across the Netherlands and their size ranged from small (800 employees) to large (5500 employees).
In 2015 data were collected among 1116 employees in 84 teams that provide direct care to clients. The researchers sent these participants a questionnaire with a cover letter that introduced the aim of the project and ensured their anonymity. After two weeks the respondents were sent a reminder to complete the survey. In total, 497 respondents (74 teams within 7 nursing homes) completed the questionnaire, resulting in a response rate of 44.5%. Team size varied from 5–40 team members with a mean of 16.96 members (SD = 8.79).
Measures
We measured perceived workload with an eight-item scale developed by De Jonge et al. [35]. This scale has been validated in several studies, with Cronbach’s alpha’s varying between .86 and .89 [36–40]. In line with other researchers [e.g. 27, 37, 38, 41–44], we chose to measure perceived workload instead of objective workload because caregivers may perceive the same workload differently dependent on their employment status, career goals and expectations, coping mechanisms, and work ethics [44, 45]. Moreover, indicators of actual workload only take into account quantitative aspects, whereas the scale by De Jonge et al. takes both quantitative and qualitative aspects of workload into account. An example item is: “In my team, too much work needs to be done”. In this study, perceived workload had a Cronbach’s alpha of .87.
Team support for strengths use was based upon a validated scale [46, 47], but was adapted to refer to the team context. We investigated the validity of this adapted seven-item scale with the following procedure. First, we made a random split of our dataset so that we could conduct an Exploratory Factor Analysis (EFA) on one half of the dataset (N = 228), and a Confirmatory Factor Analysis (CFA) on the other half of the data (N = 269). Results of the EFA indicated that the seven items loaded on one factor, with an Eigenvalue of 3.59, explaining 51.31% of the variance. Second, we conducted a Confirmatory Factor Analysis (CFA) on the other half of the data (N = 269). Results of the CFA indicated that this one factor model had an acceptable fit to the data (χ2(14) = 63.17, CFI = .92, SRMR = .05). An example item is “In this team, my tasks are adjusted to suit my strengths”. The Cronbach’s alpha of team support for strengths use was .84.
In this study quality of care refers to caregivers’ perception of the quality of care provided by the team and is therefore labelled as perceived team-based quality of care. Caregivers have an ideal position for assessing the quality of care that is provided by the team as they build their perception overtime on various encounters and processes, based on interactions with fellow caregivers, informal caregivers, and patients [48, 49]. Moreover, previous studies found that nurse-reported quality of care is associated with objective outcomes such as hospital mortality rates, 30 day inpatient mortality, 30 day failure to rescue, and survival probabilities [48, 50]. Perceived team-based quality of care was measured by a self-developed scale, which consisted of five items. “The way our team works guarantees a good quality of care” is an example item. We applied the same validation procedure as for the strengths-based team support scale. Results of the EFA indicated that the five items loaded on one factor, with an Eigenvalue of 2.62, explaining 52.83% of the variance. Results of the CFA showed that this one factor model had a good fit to the data (χ2(5) = 14.33, CFI = .97, SRMR = .03). Perceived quality of care had a Cronbach’s alpha of .75.
In addition, we performed a CFA that included perceived workload, strengths-based team support and perceived team-based quality of care. A CFA three-factor model with all three scales loading on three separate factors (χ2(167) = 346.36, CFI = .91, SRMR = .07,) fitted significantly better to the data than a two-factor model with perceived workload and quality of care loading on one factor and team support for strengths use loading on a second (∆χ2(2) = 338.08, p < .001; CFI = .74, SRMR = .13), a model with team support for strengths use and quality of care loading on one factor and perceived workload loading on a second factor (∆χ2(2) = 168.24, p < .001; CFI = .83, SRMR = .08), and a model with all three scales loading on one common factor (∆χ2(3) 806.91, p < .001; CFI = .51, SRMR = .18.
Perceived workload, team support for strengths use, and perceived quality of care were all measured with five-point Likert scales ranging from 1 (strongly disagree) to 5 (strongly agree).
We measured perceived patient safety by asking respondents to rate four safety indicators, namely the frequency of fall incidents, medication errors, pressure ulcers, and aggression incidents on a five-point Likert scale from (1) never to (5) often.
Gender, age, education, number of team members, team tenure, organizational tenure, and job title were included as control variables. All measures that were included in this study are presented in S1 File.
Data analysis
The analyses were conducted using SPSS (Statistical Package for Social Science) 15.0. Hypotheses were tested with multilevel regression analyses using the linear mixed-effects model procedure in SPSS [51] such that the effects of the individual-level variables were examined while accounting for the non-independence of observations within groups [52]. We computed deviance scores (differences in the -2 log likelihood) to compare the different models and to test their significance [53]. Measures of model fit for all models were obtained by comparing deviance scores using a Chi-squared distribution table.
Ethical consideration
The ethic committee confirmed that this study fell outside the scope of the Netherlands' Medical Research Involving Human Subjects Act (WMO) and therefore no formal ethical approval was needed. Although our research was conducted in a medical setting, it met none of the WMO criteria (http://www.ccmo.nl/en/your-research-does-it-fall-under-the-wmo). First, no patients were involved. Second, the study content and methodology did not constitute an infringement of the physical and/or psychological integrity of the participants. Survey questions on patient safety referred to the team level and were therefore not traceable to individual patients.
Results
Sample characteristics
Most of our respondents were female (95.5%), which is slightly more than the percentage of female employees in the Dutch long-term care setting (85%) [54]. The average age of the respondents was 41.06 years (SD = 12.35), and ranged from 16 to 65 years. This is comparable to the general Dutch long-term care sector where the average age of employees is 40.10 years [54]. In comparison with the distribution in Dutch nursing homes our sample included fewer practical nurses (47.4%, compared to 77% in the Dutch population), more nurse aides (21.4%, compared to 11% in the Dutch population), and more registered nurses (15.0%, compared to 7% in the Dutch population), as shown in Table 1 [55]. Respondents had an average team tenure of 4.54 years (SD = 4.51) and an average organizational tenure of 11.42 years (SD = 8.74).
Table 1. Characteristics of respondents.
| Characteristics | n (%) |
|---|---|
| Gender (6 missing values) Female | 469 (95.5) |
| Education (12 missing values) | |
| Secondary degree | 102 (21.0) |
| Vocational degree | 349 (72.0) |
| Bachelor degree | 30 (6.2) |
| Master degree | 4 (0.8) |
| Job title (24 missing values) | |
| Aid | 101 (21.4) |
| Practical nurse | 224 (47.4) |
| Registered nurse | 71 (15.0) |
| Occupational therapist | 11 (2.3) |
| Student nurse | 37 (7.8) |
| Paramedic support | 2 (0.4) |
| Coordinator | 27 (5.7) |
Descriptive statistics of the main variables are presented in Table 2. The majority of respondents (74.5%) perceived their workload as problematic (i.e. score between 3 and 5 on a 5 point Likert scale) and 22.1% of the respondents perceived their workload as very high (i.e. score between 4 and 5 on a 5 point Likert scale). Most respondents (68.2%) perceived some support (i.e. a score between 3 and 4), and 17.2% experienced strong support for individual strength-use within their team (i.e. a score between 4 and 5). Quality of care provided by the team was considered a problem by 13.3% of the respondents (i.e. score between 1 and 3), whereas 13.4% of the respondents considered the team to provide care of high quality (i.e. score between 4 and 5 score). 22.3% of respondents experienced aggression incidents frequently (i.e. score between 4 and 5), whereas fall incidents, medication errors and pressure ulcers were frequently experienced by only 7.7%, 4.9%, and 0.4% of the respondents, respectively.
Table 2. Descriptive statistics.
| Mean | SD | % score 1–2 | % score 2–3 | % score 3–4 | % score 4–5 | ||
| Perceived workload* | 3.50 | .71 | 1.9 | 23.6 | 52.4 | 22.1 | |
| Team support for strengths use* | 3.60 | .58 | 2.1 | 12.5 | 68.2 | 17.2 | |
| Perceived team-based quality of care* | 3.63 | .52 | 1.1 | 12.2 | 73.3 | 13.4 | |
| Mean | SD | % score 1 | % score 2 | % score 3 | % score 4 | % score 5 | |
| Fall incidents** | 3.11 | .91 | 1.7 | 24.2 | 43.6 | 22.8 | 7.7 |
| Medication error** | 2.94 | .89 | 2.9 | 28.9 | 44.2 | 19.2 | 4.9 |
| Pressure ulcers** | 2.51 | .80 | 8.0 | 43.8 | 37.9 | 9.9 | 0.4 |
| Incidents of aggression** | 3.65 | 1.00 | 1.4 | 11.6 | 30.0 | 34.7 | 22.3 |
*score on a 5 point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree)
** score on a 5 point Likert scale ranging from 1 (never) to 5 (often)
Correlations
As can be seen in the correlation matrix (Table 3), perceived workload was negatively related to perceived team-based quality of care (r = -.12, p < .05), and positively related to perceived frequency of fall incidents (r = .19, p < .01), medication errors (r = .19, p < .01), pressure ulcers (r = .16, p < .01), and incidents of aggression (r = .13, p < .01). Team support for strengths use was positively related to perceived team-based quality of care (r = .41, p < .01) and negatively related to fall incidents (r = -.12, p < .05), medication errors (r = -.12, p < .05), and pressure ulcers (r = -.12, p < .05). Team support for strengths use did not relate significantly to aggression incidents (r = -.05, ns). Perceived team-based quality of care was negatively related to safety in terms of fall incidents (r = .24, p < .01), medication errors (r = .32, p < .01), pressure ulcers (r = .20, p < .01), and aggression incidents (r = .18, p < .01).
Table 3. Correlation matrix.
| Mean | SD | MV | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Perceived workload | 3.50 | .71 | 18 | 1 | ||||||||||||
| 2. Team Support for Strengths use | 3.60 | .58 | 10 | -.13** | 1 | |||||||||||
| 3. Perceived team-based quality of care | 3.64 | .53 | 21 | -.12* | .41** | 1 | ||||||||||
| 4. Fall incidents | 3.11 | .91 | 18 | .19** | -.12* | -.24** | 1 | |||||||||
| 5. Medication errors | 2.94 | .89 | 44 | .19** | -.12* | -.32** | .21** | 1 | ||||||||
| 6. Pressure ulcers | 2.51 | .80 | 33 | .16** | -.12* | -.20** | .16** | .22** | 1 | |||||||
| 7. Incidents of aggression | 3.65 | 1.00 | 13 | .13** | -.05 | -.18** | .35** | .13** | .12* | 1 | ||||||
| 8. Gender (1 = man, 2 = female) | 1.96 | .21 | 6 | .05 | .07 | .05 | -.08 | .02 | -.05 | -.05 | 1 | |||||
| 9. Age | 41.06 | 12.35 | 35 | .21** | -.03 | -.05 | .05 | .00 | -.07 | .01 | .03 | 1 | ||||
| 10. Education | 4.33 | 1.69 | 12 | -.06 | -.07 | -.03 | -.01 | .09 | -.03 | .03 | .03 | -.24** | 1 | |||
| 11. Team size | 16.96 | 8.79 | 0 | .24** | -.04 | -.09 | .39** | .18** | .16** | .21** | .01 | .04 | .00 | 1 | ||
| 12. Team tenure | 4.54 | 4.51 | 37 | .19** | -.04 | .04 | .08 | .09 | .11* | -.02 | .01 | .32** | -.17** | .17** | 1 | |
| 13. Organizational tenure | 11.42 | 8.74 | 26 | .10* | .06 | .03 | -.02 | .05 | .02 | .01 | .03 | .50** | -.24** | .07 | .38** | 1 |
| 14. Nursing homes: | 0 | |||||||||||||||
| 1 (n = 81) | -.22** | -.13** | -.07 | -.20** | -.26** | .01 | -.05 | -.04 | .01 | -.05 | -.54** | -.01 | .01 | |||
| 2 (n = 49) | -.09* | .01 | .12** | -.02 | .10* | .07 | -.07 | .01 | -.06 | -.02 | -.05 | -.06 | -.03 | |||
| 3 (n = 119) | .00 | .05 | .15** | -.17** | -.15** | -.19* | -.17** | .00 | .04 | -.02 | -.17** | .02 | -.05 | |||
| 4 (n = 54) | .01 | -.11* | -.19** | -.00 | .03 | .08 | -.00 | .03 | -.05 | .08 | .09 | -.03 | -.01 | |||
| 5 (n = 82) | .12** | .12** | -.03 | -.05 | .09 | -.10* | .27** | -.04 | -.04 | .06 | -.07 | -.17** | .00 | |||
| 6 (n = 12) | -.02 | .05 | -.03 | .11* | .28** | .06 | -.19** | .01 | -.06 | -.02 | .02 | .01 | -.04 | |||
| 7 (n = 100) | .17** | -.06 | -.07 | .32** | .01 | .16** | .17** | .04 | .09* | .01 | .80** | .19** | .09* |
**significant at .01 level (2-tailed)
*significant at .05 level (2-tailed)
MV = missing values
Perceived workload was positively related to age (r = .21, p < .01), team size (r = .24, p < .01), team tenure (r = .19, p < .01), and organizational tenure (r = .10, p < .05). Team size was positively related to fall incidents (r = .39, p < .01), medication errors (r = .18, p < .01), pressure ulcers (r = .16, p < .01), and aggression incidents (r = .21, p < .01). Team tenure was positively related to pressure ulcers (r = .11, p < .05). Perceived team-based quality of care was significantly higher in two nursing homes and significantly lower in another nursing home. The same holds for perceived workload and perceived frequency of safety incidents; two nursing homes showed a significantly higher level of perceived workload and more perceived safety incidents, while two other nursing homes showed a significantly lower level of perceived workload and fewer perceived safety incidents. Therefore, dummy variables were included for each of the nursing homes as control variables in further analyses.
Multilevel analyses
Multilevel analyses are presented in Tables 4–6. All variables were centered before they were entered in the analyses (except for the dummy variables representing the organizations). For each of the outcome variables, model A includes only the control variables. In model B, perceived workload and team support for strengths use were added as main effects while model C also includes the interaction between perceived workload and team support for strengths use. Tables 4–6 shows that perceived workload was not significantly related to perceived team-based quality of care (B = -.03, CI = -.10, .04) or any of the safety indicators (B = .06, CI = -.05, .18; B = .05 CI = -.07, .17; B = .07 CI = -.04, .18; B = .06 CI = -.08, .19, respectively), thereby not providing support for Hypothesis 1. Team support for strengths use was positively related to perceived team-based quality of care (B = .38, CI = .30, .46), negatively related to medication errors (B = -.18, CI = -.31, -.05), and not significantly related to fall incidents, pressure ulcers, or aggression incidents (B = -.11, CI = -.24, .02; B = -.08, CI = -.20, .04; B = -.05, CI = -.20, .10 respectively), thereby only providing support for Hypotheses 2a and 2c.
Table 4. Two-level multilevel regression analysis: Perceived team-based quality of care and frequency of fall incidents.
| Perceived team-based quality of care | Frequency of fall incidents | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |||||||
| Estimate [C.I.] | p | Estimate [C.I.] | p | Estimate [C.I.] | p | Estimate [C.I.] | p | Estimate [C.I.] | p | Estimate [C.I.] | p | |
| Intercept | 3.76[3.63,3.90] | .000 | 3.72 [3.61,3.84] | .000 | 3.73 [3.62, 3.84] | .000 | 2.83 [2.57, 3.10] | .000 | 2.85[2.58, 3.11] | .000 | 2.84 [2.58, 3.11] | .000 |
| Age | -.00 [-.01,.00] | .185 | -.00 [-.01,.00] | .514 | -.00 [-.01, .00] | .643 | .00 [-.00, .01] | .172 | .00 [-.00, .01] | .424 | .00 [-.00, .00] | .493 |
| Team size | -.02 [-.04,-.00] | .030 | -.01 [-.03,.-00] | .049 | -.01 [-.02, -.00] | .032 | .04 [.00, .07] | .028 | .04 [.00, .07] | .035 | .04 [.00, .07] | .033 |
| Team tenure | .00 [-.01,.02] | .655 | .00 [-.01,.01] | .566 | .00 [-.01, .01] | .635 | .01 [-.01, .03] | .354 | .00 [-.02, .02] | .707 | .00 [-.01, .02] | .672 |
| Organizational tenure | .00 [-.00,.01] | .158 | .00 [-.00,.01] | .360 | .00 [-.00, .01] | .369 | -.00 [-.01, .01] | .367 | -.00 [-.01, .01] | .559 | -.00 [.01, .01] | .575 |
| Nursing home 1Nursing home 2Nursing home 4Nursing home 5Nursing home 6Nursing home 7 | -.43 [-.67,-.19].05 [-.20,.30]-.91 [-1.29,-.52]-.20 [-.41,.01]-.16 [-.38,.06] .05 [-.28,.39] | .001.679.000.062.147.763 | -.26 [-.45,-.06].06 [-.14,.25]-.70 [-1.02,-.38]-.22 [-.39,-.06]-.15 [-.32,.03].05 [-.20, .31] | .011.550.000.009.097.685 | -.27 [-.46, -.08].07 [-.12, .26]-.67 [-.99, -.36]-.24 [-.41, -.08]-.15 [-.32, .03].07 [-.18, .33] | .007.492.000.004.096.563 | .30 [-.15, .75].27 [-.21, .74].49 [-.21, 1.19].17 [-.24, .59].50 [.08, .92].35 [-.33, 1.02] | .196.270.168.409.021.313 | .30 [-.16, .76].24 [-.23, .72].42 [-.28, 1.12].16 [-.25, .58].50 [.08, .92].35 [-.32, 1.02] | .194.312.234.435.021.301 | .31 [-.15, .77].24 [-.24, .72].40 [-.30, 1.11].18 [-.24, 60].50 [.07, .92].34 [-.34, 1.02] | .184.326.261.393.022.323 |
| Perceived workloadTeam Support for Strengths use Interaction Perceived workload* TSS | -.03 [-.10, .04].38 [.30, .46] | .451.000 | -.04 [-.11, .03].36 [.28, .44].14 [.03, .25] | .279.000.013 | .06 [-.05, .18]-.11 [-.24, .02] | .243.085 | .08 [-.04, .20]-.10 [-.23, .03]-.11 [-.29, .06] | .175.148.192 | ||||
| Teamlevel (intercept) | .03 [.01,.06] | .024 | .01 [.00, .05] | .36 | .01 [.00, .06] | .40 | .18 [.11, .28] | .000 | .18 [.11, .28] | .000 | .18 [.11, .28] | .000 |
| -2 Log Likelihood | 613.99 | 502.85 | 496.64 | 947.42 | 900.80 | 899.10 | ||||||
| Deviance change (Δχ2 (df)) | - | 111.14 (2)** | 6.21 (1)* | - | 46.62 (2)** | 1.70 (1) | ||||||
| AIC | 639.99 | 532.85 | 528.64 | 973.42 | 930.80 | 931.10 | ||||||
| BIC | 692.48 | 592.65 | 592.42 | 1026.12 | 990.82 | 995.12 | ||||||
Table 6. Two-level multilevel regression analysis: Perceived frequency of incidents of aggression.
| Frequency of incidents of aggression | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| Estimate [C.I.] | p | Estimate [C.I.] | p | Estimate [C.I.] | p | |
| Intercept | 3.47 [3.18, 3.76] | .000 | 3.46 [3.17, 3.76] | .000 | 3.46 [3.16, 3.75] | .000 |
| Age | -.00 [-.01, .01] | .770 | -.00 [-.01, .01] | .561 | -.00 [-.01, .01] | .487 |
| Team size | .05 [.01, .09] | .008 | .05 [.01, .09] | .007 | .05 [.02, .09] | .006 |
| Team tenure | .01 [-.02, .03] | .627 | .00 [-.02, .02] | .957 | .00 [-.02, .02] | .900 |
| Organizational tenure | -.00 [-.01, .01] | .928 | .00 [-.01, .01] | .678 | .00 [-.01, .01] | .657 |
| Nursing home 1Nursing home 2Nursing home 4Nursing home 5Nursing home 6Nursing home 7 | .70 [.19, 1.20]-.29 [-.83, .24].40 [-.39, 1.19].80 [.34, 1.26]-.38 [-.86, .09]-.22 [-.96, .53] | .007.276.321.001.111.560 | .68 [.17, 1.19]-.32 [-.86, .21].39 [-.40, 1.18].81 [.34, 1.27]-.37 [-.85, .10]-.20 [-.95, .54] | .010.229.330.001.124.585 | .69 [.18, 1.20]-.33 [-.87, .20].36 [-.43, 1.15].82 [.36, 1.29]-.37 [-.85, .10]-.22 [-.97, .52] | .009.219.364.001.122.551 |
| Perceived workload | .06 [-.08, .19] | .414 | .07 [-.07, .20] | .320 | ||
| Team Support for Strengths use | -.05 [-.20, .10] | .520 | -.03 -.18, .12] | .685 | ||
| Interaction perceived workload*TSS | -.13 [-.32, .07] | .209 | ||||
| Teamlevel (intercept) | .21 [.13, .35] | .000 | .21 [.12, .35] | .06 | .21 [.13, .35] | .000 |
| -2 Log Likelihood | 1089.00 | 1024.30 | 1022.72 | |||
| Deviance change (Δχ2 (df)) | - | 65.60 (2)** | 1.58 (1) | |||
| AIC | 1115.00 | 1054.30 | 1054.72 | |||
| BIC | 1167.80 | 1114.43 | 1118.86 | |||
**significant at .01 level
*significant at .05 level
TSS = Team support for strengths use
Table 5. Two-level multilevel regression analysis: Perceived frequency of medication errors and pressure ulcers.
| Frequency of medication errors | Frequency of pressure ulcers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |||||||
| Estimate [C.I.] | p | Estimate [C.I.] | p | Estimate [C.I.] | P | Estimate [C.I.] | p | Estimate [C.I.] | p | Estimate [C.I.] | p | |
| Intercept | 2.77 [2.52, 3.02] | .000 | 2.74 [2.49, 2.98] | .000 | 2.73 [2.49, 2.98] | .000 | 2.36 [2.11, 2.60] | .000 | 2.36 [2.11, 2.60] | .000 | 2.35 [2.10, 2.60] | .000 |
| Age | .00 [-.00, .01] | .513 | .00 [-.01, .01] | .752 | .00 [-.01, .01] | .816 | -.00 [-.01, .00] | .102 | -.01 [-.01, .00] | .069 | -.01 [-.01, .00] | .051 |
| Team size | .01 [-.02, .04] | .436 | .01 [-.02, .04] | .625 | .01 [-.02, .04] | .596 | .01 [-.02, .04] | .519 | .01 [-.02, .04] | .641 | .01 [-.02, .04] | .605 |
| Team tenure | .01 [-.00, .03] | .161 | .01 [-.01, .03] | .259 | .01 [-.01, .03] | .252 | .02 [.00, .04] | .041 | .02 [-.00, .03] | .073 | .02 [-.00, .04] | .067 |
| Organizational tenure | .00 [-.01, .01] | .738 | .00 [-.01, .01] | .423 | .00 [-.01, .01] | .409 | -.00 [-.01, .01] | .487 | -.00 [-.01, .01] | .504 | -.00 [-.01, .01] | .524 |
| Nursing home 1Nursing home 2Nursing home 4Nursing home 5Nursing home 6Nursing home 7 | -.16 [-.60, .28].42 [-.05, .88].38 [-.30, 1.06].40 [.00, .80].86 [.45, 1.26]-.02 [-.67, .63] | .463.080.275.049.000.954 | -.21 [-.64, .22].41 [-.05, .86].32 [-.34, .98].44 [.05, .82].91 [.51, 1.30].05 [-.57, .67] | .335.079.339.027.000.869 | -.20 [-.64, .23].40 [-.05, .86].30 [-.36, .97].45 [.06, .83].90 [.51, 1.30].04 [-.58, .66] | .347.081.362.024.000.904 | .28 [-.15, .70].20 [-.24, .64].61 [-.04, 1.27]-.04 [-.42, .35].23 [-.16, .62].22 [-.40, .85] | .197.373.067.849.251.472 | .25 [-.19, .68].16 [-.29, .61].57 [-.09, 1.23]-.02 [-.41, .37].24[-.15, .64].26 [-.37, .89] | .261.484.090.902.228.418 | .25 [-.18, .69].15 [-.30, .60].54 [-.12, 1.21]-.01 [-.40, .38].24 [-.16, .64].24 [-.39, .87] | .246.507.106.958.236.454 |
| Perceived workload | .05 [-.07, .17] | .396 | -.06 [-.06, .18] | .334 | .07 [-.04, .18] | .200 | .08 [-.03, .19] | .143 | ||||
| Team Support for Strengths use Interaction Perceived workload*TSS | -.18 [-.31, -.05] | .008 | -.17 [-.30, -.04]-.08 [-.26, .10] |
.013.384 | -.08 [-.20, .04] | .193 | -.07 [-.19, .06]-.12 [-.28, .05] |
.287.158 | ||||
| Teamlevel (intercept) | .15[.09, .26] | .000 | .13 [.08, .24] | .000 | .13 [.08, .23] | .000 | .14 [.08, .25] | .000 | .15 [.09, .26] | .000 | .15 [.09, .26] | .000 |
| -2 Log Likelihood | 912.56 | 863.45 | 862.70 | 888.34 | 833.94 | 831.94 | ||||||
| Deviance change (Δχ2 (df)) | - | 49.11 (2)** | 0.75 (1) | - | 54.40 (2)** | 2.00 (1) | ||||||
| AIC | 938.56 | 893.45 | 894.70 | 914.34 | 863.94 | 863.94 | ||||||
| BIC | 990.51 | 952.75 | 957.95 | 996.58 | 923.58 | 927.56 | ||||||
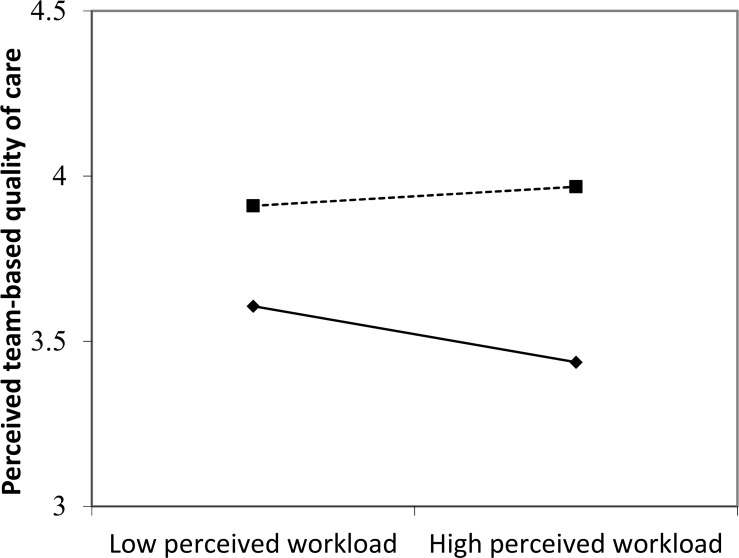
Finally, the interaction between perceived workload and team support for strengths use was significant for perceived team-based quality of care (B = .14, CI = .03,.25), but not for fall incidents, medical errors, pressure ulcers, and aggression incidents (B = -.11, CI = -.29, .06; B = -.08, CI = -.26, .10; B = -.12, CI = -.28, .05; B = -.13, CI = -.32, .07, respectively). Fig 1 shows that perceived workload has a significant negative effect on perceived team-based quality of care when team support for strengths use is low (- 1 SD) (B = -.12, p = .02), but is unrelated to perceived team-based quality of care when team support for strengths use is high (+1 SD) (B = .04, p = .34). Based on the significance of the interaction term, Hypothesis 3a can be confirmed whereas Hypotheses 3b, 3c, 3d, and 3e remain unsupported.
Fig 1. Relationship between perceived team-based workload, team support for strengths use, and perceived quality of care.
–◆– Low team support for strength use. —■-—High team support for strength use.
Discussion
Key findings and discussion points
In contrast to previous studies [3–10] we did not find a significant relationship between perceived workload on the one hand and perceived team-based quality of care and patient safety on the other hand. This is in line with Myny et al. [56] who posit that so-called “non-direct patient care” factors such as hospital and ward characteristics, nursing team characteristics, characteristics of the individual nurse, patient and family characteristics may impact nursing workload and its effect on output.
Possibly, perceived workload is only associated with diminished quality and safety of care when job resources are lacking, as is also indicated by the interaction effect that we found between team support for strengths use and perceived workload. Our results point to strengths-based team support as a new job resource that might affect team performance and buffer the relationship between job demands and performance. Caregivers who perceive that their strengths are appreciated in their team and feel that they can capitalize on their strengths perceive higher quality of care provided by the team and this perception seems not to be affected by a heavy workload. Team support for strengths use may help caregivers to deal with high work load by alleviating stress levels, thereby reducing the risk that the quality of care is compromised. Our results demonstrate that leveraging the strengths of individual caregivers in the care team is directly associated with a higher perceived team-based quality of care and a lower perceived frequency of medication errors. However, perceived frequency of pressure ulcers, aggression, and fall incidents were not associated with the level of support given to caregivers’ strengths. Possibly, the general perception of quality of care provided by the team responds more quickly to team support for strengths use than more specific perceptions of the occurrence of adverse events. Another possible explanation is that these safety indicators depend more on the patients’ condition [57], such as their health, comorbidity, and self-efficacy, and are therefore less influenced by caregivers’ activities in comparison to medication errors. This may also explain why team support for strengths use did diminish the effect of perceived workload on perceived team-based quality of care, but did not diminish the effect of perceived workload on perceived frequency of adverse events (i.e., patient falls, medication errors, pressure ulcers, and aggression incidents).
Implications for nursing management
Whereas providing skills training to caregivers often stimulates more concern for quality and safety of care [58], our results indicate that leveraging the unique strengths of individual caregivers in nursing home teams is also positively associated with perceived team-based quality of care and patient safety. Although personal strengths are trait-like characteristics that are energizing to the user, this does not mean that individuals are always aware of having them [59] or that strengths use is self-evident. Many people report not to make full use of their strengths at work [60, 61], due to their perceptions of normative demands at work, the appropriateness of strengths use, or their inclination to focus on fitting in at the expense of their authenticity [61, 62]. To create more awareness of the individual strengths present in a team, managers may use such instruments as Strengthsfinder [63], or the Values In Action Inventory of Strengths (VIA-IS) [24]. Alternatively, managers may conduct feedforward interviews (as opposed to feedback interviews), inviting employees to talk about moments when they felt energized at work, or caregivers may ask their colleagues in the team for feedback on when they are their ‘best self’ [64]. In a next step, managers and teams can discuss opportunities for team workers with complementary strengths to join forces, so that they can complement each other’s unique strengths.
Limitations and implications for future research
The first limitation of this study is its cross-sectional design, which does not allow us to make causal inferences. Second, we used subjective measures of quality and safety of care because objective indicators at the team level were not available. So far, only few studies within the healthcare setting have combined subjective performance measures (e.g., satisfaction, perceived team-based quality of care, perceived performance, and processes) with objective performance measures (e.g., length of stay, nurse retention, hospitalization rates) [65]. Future research should attempt to apply a longitudinal design and to combine subjective and objective safety indicators in order to investigate two equally valuable angles on safety. Third, the relationship between team support for strengths use on the one hand and quality of care and patient safety on the other hand may be affected by common method bias because all constructs were rated by team members in one and the same questionnaire [66]. However, the results of a Harman’s one factor test in which all items that measured our three latent variables were loaded onto one common factor explained only 24.65% of the total variance, suggesting that common method bias does not affect our data [67]. Furthermore, the results from confirmatory factor analyses clearly indicated that loading all items on one common factor did not fit our data well, which suggests that common method bias may be limited. Also, the moderation effect that we found is unlikely to be biased by common source variance [68]. Nevertheless, future research should attempt to include data regarding quality of care and patient safety that is based on other sources, such as objective data, or ratings by team managers. A fourth limitation is that although our sample was fairly representative for Dutch nursing homes in terms of gender and age, it was not fully representative in terms of job title. Therefore, future studies should aim to collect randomly selected samples that are representative of the variety in nursing homes characteristics.
Future research could also explore the balance between tasks that need a uniform approach from all caregivers, and tasks that allow for individual differences and specialization. There is no doubt that caregivers need to be able to carry out a basic set of core tasks on the job, and must adhere to safety guidelines. However, for many tasks, such as dealing with aggressive or distressed patients, it is possible to allow for individual differences in the way the task is done, in line with the personal qualities of the caregiver [69]. Other tasks (e.g., drawing up schedules or communicating with relatives) may even be allocated to specific caregivers based on their individual strengths. The effect of team support for strengths use on the quality and safety of care is in line with the worldwide trend in specialization of the nursing profession, which often has a positive effect on nurses’ workload and job satisfaction, but is also fragmenting care delivery [70]. Future studies could further explore this balance between specialization based on individual strengths on the one hand, and uniformity on the other hand.
Supporting information
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1.Meijer A, Van Campen C, Kerkstra A. A comparative study of the financing, provision and quality of care in nursing homes. The approach of four European countries: Belgium, Denmark, Germany and the Netherlands. Journal of Advanced Nursing 2000;32(3):554–561. [DOI] [PubMed] [Google Scholar]
- 2.Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Critical care medicine 2010;38(7):1521–1528. doi: 10.1097/CCM.0b013e3181e47888 [DOI] [PubMed] [Google Scholar]
- 3.Hugonnet S, Chevrolet JC, Pittet D. The effect of workload on infection risk in critically ill patients. Critical Care Medicine 2007;35(1): 76–81. doi: 10.1097/01.CCM.0000251125.08629.3F [DOI] [PubMed] [Google Scholar]
- 4.Duffield C, Diers D, O'Brien-Pallas L, Aisbett C, Roche M, King M, et al. Nursing staffing, nursing workload, the work environment and patient outcomes. Applied Nursing Research 2011;24(4):244–255. doi: 10.1016/j.apnr.2009.12.004 [DOI] [PubMed] [Google Scholar]
- 5.Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta analysis. Medical care 2007;45(12):1195–1204. doi: 10.1097/MLR.0b013e3181468ca3 [DOI] [PubMed] [Google Scholar]
- 6.West E, Barron DN, Harrison D, Rafferty AM, Rowan K, Sanderson C. Nurse staffing, medical staffing and mortality in intensive care: an observational study. International journal of nursing studies 2014;51(5):781–794. doi: 10.1016/j.ijnurstu.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 7.Nantsupawat A, Srisuphan W, Kunaviktikul W, Nantsupawat A, Srisuphan W, Kunaviktikul W, et al. Impact of nurse work environment and staffing on hospital nurse and quality of care in Thailand. Journal of Nursing Scholarship 2011;43(4):426–432. doi: 10.1111/j.1547-5069.2011.01419.x [DOI] [PubMed] [Google Scholar]
- 8.Holden RJ, Scanlon MC, Patel NR, Kaushal R, Escoto KH, Brown RL, et al. A human factors framework and study of the effect of nursing workload on patient safety andemployee quality of working life. BMJ quality & safety 2011;20(1):15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH.Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Jama 2002;288(16):1987–1993. [DOI] [PubMed] [Google Scholar]
- 10.Sochalski J. Is more better?: the relationship between nurse staffing and the quality of nursing care in hospitals. Medical care 2004;42(2):II–67. [DOI] [PubMed] [Google Scholar]
- 11.Jones TL, Hamilton P, Murry N. Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. International Journal of Nursing Studies 2015;52(6):1121–1137. doi: 10.1016/j.ijnurstu.2015.02.012 [DOI] [PubMed] [Google Scholar]
- 12.Lankshear AJ, Sheldon TA, Maynard A. Nurse staffing and healthcare outcomes: a systematic review of the international research evidence. Advances in Nursing Science 2005;28(2):163–174. [DOI] [PubMed] [Google Scholar]
- 13.Ball JE, Murrells T, Rafferty AM, Morrow E, Griffiths P. Care left undone’ during nursing shifts: associations with workload and perceived quality of care. BMJ quality & safety 2013;23:92–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cho E, Lee NJ, Kim EY, Kim S, Lee K, Park KO, et al. Nurse staffing level and overtime associated with patient safety, quality of care, and care left undone in hospitals: a cross-sectional study. International journal of nursing studies 2016;60:263 271. doi: 10.1016/j.ijnurstu.2016.05.009 [DOI] [PubMed] [Google Scholar]
- 15.Bakker AB, Demerouti E, Euwema MC. Job resources buffer the impact of job demands on burnout. Journal of occupational health psychology 2005;10:170–180. doi: 10.1037/1076-8998.10.2.170 [DOI] [PubMed] [Google Scholar]
- 16.Xanthopoulou D, Bakker AB, Dollard MF, Demerouti E, Schaufeli WB, Taris TW, et al. When do job demands particularly predict burnout? The moderating role of job resources. Journal of managerial psychology 2007;22(8):766–786. [Google Scholar]
- 17.Keenan EM, Mostert K. Perceived organisational support for strengths use: The factorial validity and reliability of a new scale in the banking industry. SA Journal of Industrial Psychology 2013;39(1):1–12. [Google Scholar]
- 18.Van Woerkom M, Tjepkema S. Positive and critical: Enhancing constructive critical reflection in groups. In: Walton J, Valentin C. (Eds.) Human Resource Development: Practices and Orthodoxies. 2013:58–82. [Google Scholar]
- 19.Wood AM, Linley PA, Maltby J, Kashdan TB, Hurling R.Using personal and psychological strengths leads to increases in well-being over time: A longitudinal study and the development of the strengths use questionnaire. Personality and Individual Differences 2011;50(1):15–19. [Google Scholar]
- 20.Meyers MC, van Woerkom M, de Reuver RS, Bakk Z, Oberski DL. Enhancing psychological capital and personal growth initiative: Working on strengths or deficiencies. Journal of Counseling Psychology 2015;62(1):50–62. doi: 10.1037/cou0000050 [DOI] [PubMed] [Google Scholar]
- 21.Van Woerkom M, Meyers MC. My Strengths Count! Human Resource Management 2015;54(1):81–103. [Google Scholar]
- 22.Van Woerkom M, Oerlemans WGA, Bakker AB. Strengths use and work engagement: A weekly diary study. European Journal of Work and Organizational Psychology 2016;25(3):384–397 [Google Scholar]
- 23.Havig AK, Skogstad A, Veenstra M, Romøren TI. Real teams and their effect on the quality of care in nursing homes. BMC health services research 2013;13(1):499 510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peterson C, Seligman ME. Character strengths and virtues: A handbook and classification Oxford University Press; 2004. [Google Scholar]
- 25.Kernis MH, Goldman BM. A multicomponent conceptualization of authenticity: Theory and research. Advances in experimental social psychology 2006;38:283–357. [Google Scholar]
- 26.Wagner LM, Capezuti E, Ouslander JG. Reporting near-miss events in nursing homes. Nursing outlook 2006;54(2):85–93. doi: 10.1016/j.outlook.2006.01.003 [DOI] [PubMed] [Google Scholar]
- 27.Baethge A, Müller A, Rigotti T. Nursing performance under high workload: A diary study on the moderating role of selection, optimization and compensation strategies. Journal of advanced nursing 2016;72(3):545–557. doi: 10.1111/jan.12847 [DOI] [PubMed] [Google Scholar]
- 28.Chen MF, Ho CH, Lin CF, Chung MH, Chao WC, Chou HL, et al. Organisation‐based self esteem mediates the effects of social support and job satisfaction on intention to stay in nurses. Journal of nursing management 2016;24(1):88–96. doi: 10.1111/jonm.12276 [DOI] [PubMed] [Google Scholar]
- 29.De Veer AJE, Francke AL, Poortvliet EP, Eliens A. Care in nursing homes is getting more and more complex according to nurses (Translated from Dutch: Verzorgenden vinden zorg in verpleeg-en verzorgingshuizen steeds complexer) NIVEL: Utrecht: 2007. [Google Scholar]
- 30.Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R, Caffrey C, Rome V, et al. Long term care providers and services users in the United States: data from the National Study of Long-Term Care Providers, 2013–2014. Vital & health statistics 2016;38:x–xii. [PubMed] [Google Scholar]
- 31.Van der Windt W, Talma H. The labor market for licensed and practical nurses, and social workers in the healthcare sector 2004–2008 (Translated from Dutch: De arbeidsmarkt voor verpleegkundigen, verzorgenden en sociaal-pedagogen in de zorgsector 2004–2008). Prismant, Utrecht 2005.
- 32.Brummelman EG. Scale and care. International comparison (Translated from Dutch: Schaal en zorg. Internationale vergelijking) RVZ Publications, Den Haag: 2008. [Google Scholar]
- 33.Harrington C, Armstrong H, Halladay M, Havig AK, Jacobsen FF, MacDonald M, et al. Comparison of nursing home financial transparency and accountability in four locations. Ageing International 2016;41(1):17–39. [Google Scholar]
- 34.Meijer A, Van Campen C, Kerkstra A. A comparative study of the financing, provision and quality of care in nursing homes. The approach of four European countries: Belgium, Denmark, Germany and the Netherlands. Journal of Advanced Nursing 2000;32(3):554–561. [DOI] [PubMed] [Google Scholar]
- 35.De Jonge J, Landeweerd JA, Nijhuis FJN. Construction and validation of the questionnaire for the ‘job autonomy project (Translated from Dutch: Constructie en validering van de vragenlijst ten behoeve van het project ‘autonomie in het werk). Studies bedrijfsgezondheidszorg nummer 9 1993. [Google Scholar]
- 36.Houkes I, Janssen PP, de Jonge J, Bakker AB.Personality, work characteristics and employee well-being: A longitudinal analysis of additive and moderating effects. Journal of Occupational Health Psychology 2003;8(1):20–38. [DOI] [PubMed] [Google Scholar]
- 37.Tummers G, van Merode F, Landeweerd A, Candel M. Individual-Level and Group-Level Relationships Between Organizational Characteristics, Work Characteristics and Psychological Work Reactions in Nursing Work: A Multilevel Study. International Journal of Stress Management 2003;10(2):111–136. [Google Scholar]
- 38.Gandi JC, Beben WW, Gyarazama Y. Nurse’s roles and the mediating effects of stress on job performance in low and developing economies. Psychology 2011;2(4):323. [Google Scholar]
- 39.Janssen PP, Schaufelioe WB, Houkes I. Work-related and individual determinants of the three burnout dimensions. Work & Stress 1999;13(1):74–86. [Google Scholar]
- 40.De Jonge J, Dollard MF, Dormann C, Le Blanc PM, Houtman IL. The demand-control model: Specific demands, specific control, and well-defined groups. International Journal of Stress Management 2000;7(4):269–287. [Google Scholar]
- 41.Greenglass ER, Burke R J, Fiksenbaum L. Workload and burnout in nurses. Journal of community & applied social psychology 2001;11(3):211–215. [Google Scholar]
- 42.Gurses AP, Carayon P, Wall M. Impact of performance obstacles on intensive care nurses' workload, perceived quality and safety of care, and quality of working life. Health services research 2009;44(2):422–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shirom A, Nirel N, Vinokur AD. Work hours and caseload as predictors of physician burnout: the mediating effects by perceived workload and by autonomy. Applied Psychology 2010;59(4):539–565. [Google Scholar]
- 44.Zeytinoglu IU, Denton M, Davies S, Baumann A, Blythe J, Boos L. Deteriorated external work environment, heavy workload and nurses' job satisfaction and turnover intention. Canadian Public Policy 2007; 33(1):S31–S47. [Google Scholar]
- 45.Hart SM, Warren AM. Understanding nurses’ work: exploring the links between changing work, labour relations, workload, stress, retention and recruitment. Economic and Industrial Democracy 2015:36(2):305–329. [Google Scholar]
- 46.Van Woerkom M, Bakker AB, Nishii LH. Accumulative job demands and support for strength use: Fine-tuning the Job Demands-Resources model using Conservation of Resources Theory. Journal of Applied Psychology 2016;101(1):141–150. doi: 10.1037/apl0000033 [DOI] [PubMed] [Google Scholar]
- 47.Van Woerkom M, Mostert K, Els C, Bakker AB, De Beer L, Rothmann S Jr. Strengths use and deficit correction in organizations: Development and validation of a questionnaire. European Journal of Work and Organizational Psychology 2016;25(6):960–975. [Google Scholar]
- 48.McHugh MD, Stimpfel AW. Nurse reported quality of care: a measure of hospital quality. Research in nursing & health 2012;35(6):566–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pinder RJ, Greaves FE, Aylin PP, Jarman B, Bottle A. Staff perceptions of quality of care: an observational study of the NHS Staff Survey in hospitals in England. BMJ Qual Saf 2013;22:563–570. doi: 10.1136/bmjqs-2012-001540 [DOI] [PubMed] [Google Scholar]
- 50.Tvedt C, Sjetne IS, Helgeland J, Bukholm G. An observational study: associations between nurse reported hospital characteristics and estimated 30-day survival probabilities. BMJ Qual Saf 2014;23:757–764. doi: 10.1136/bmjqs-2013-002781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heck RH, Thomas SL, Tabata L. Multilevel and longitudinal analysis using SPSS Routeledge, 2013. [Google Scholar]
- 52.Diez-Roux AV. Multilevel analysis in public health research. Annual Review of Public Health 2000;21:171–192. doi: 10.1146/annurev.publhealth.21.1.171 [DOI] [PubMed] [Google Scholar]
- 53.Bickel R. Multilevel analysis for applied research: It’s just regression New York, NY: Guilford Press, 2007. [Google Scholar]
- 54.RVZ (Raad van Volksgezondheid). Labor market and the demand for care (Translated from Dutch: Arbeidsmarkt en zorgvraag) RVZ Publications, Den Haag: 2006. [Google Scholar]
- 55.Brink M, Joldersma C. Staff and training in nursing homes (Translated from Dutch: Personeel en opleiden in verpleeghuizen). Report. 2016
- 56.Myny D, Van Goubergen D, Gobert M, Vanderwee K, Van Hecke A, Defloor T.Non direct patient care factors influencing nursing workload: A review of the literature. Journal of Advanced Nursing 2011;67(10):2109–2129. doi: 10.1111/j.1365-2648.2011.05689.x [DOI] [PubMed] [Google Scholar]
- 57.McDonald KM, Romano PS, Geppert J, Davies SM, Duncan BW, Shojania KG, et al. Measures of patient safety based on hospital administrative data-the patient safety indicators. Technical Reviews 2002. [PubMed] [Google Scholar]
- 58.Weaver SJ, Lyons R, DiazGranados D, Rosen MA, Salas E, Oglesby J, et al. The anatomy of health care team training and the state of practice: a critical review. Academic Medicine 2010;85(11):1746 1760. doi: 10.1097/ACM.0b013e3181f2e907 [DOI] [PubMed] [Google Scholar]
- 59.Linley AP, Joseph S, Harrington S, Wood AM. Positive psychology: Past, present, and (possible) future. The Journal of Positive Psychology 2006;1(1):3–16. [Google Scholar]
- 60.Harzer C, Ruch W. When the job is a calling: The role of applying one’s signature strengths at work. The Journal of Positive Psychology 2012;7:362–371. [Google Scholar]
- 61.Harzer C, Ruch W. The application of signature character strengths and positive experiences at work. Journal of Happiness Studies 2013;14:965–983. [Google Scholar]
- 62.Lee JJ, Gino F, Cable D, Staats BR. Preparing the self for team entry: How relational affirmation improves team performance. Harvard Business School Working Papers 2016.
- 63.Rath T. StrengthsFinder 2.0, Simon and Schuster 2007.
- 64.Bouskila-Yam O, Kluger AN. Strength-based performance appraisal and goal setting. Human Resource Management Review 2011;21(2):137–147. [Google Scholar]
- 65.Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature. Medical Care Research and Review 2006:63(3):263–300. doi: 10.1177/1077558706287003 [DOI] [PubMed] [Google Scholar]
- 66.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of applied psychology 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- 67.Podsakoff PM, Organ DW. Self-reports in organizational research: Problems and prospects. Journal of management 1986;12(4):531–544. [Google Scholar]
- 68.Evans MG. A Monte Carlo study of the effects of correlated method variance in moderated multiple regression analysis. Organizational behavior and human decision processes 1985;36(3):305–323. [Google Scholar]
- 69.Edward KL, Ousey K, Warelow P, Lui S.Nursing and aggression in the workplace: a systematic review. British Journal of Nursing 2014;23(12):653–659. doi: 10.12968/bjon.2014.23.12.653 [DOI] [PubMed] [Google Scholar]
- 70.Ranchal A, Jolley MJ, Keogh J, Lepiesová M, Rasku T, Zeller S.The challenge of the standardization of nursing specializations in Europe. International nursing review 2015;62(4):445–452. doi: 10.1111/inr.12204 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.