Abstract
Background
Primary care-based memory clinics were established to meet the needs of persons with memory concerns. We aimed to identify: 1) physical examination maneuvers required to assess persons with possible dementia in specialist-supported primary care-based memory clinics, and 2) the best-suited clinicians to perform these maneuvers in this setting.
Methods
We distributed in-person and online surveys of clinicians in a network of 67 primary care-based memory clinics in Ontario, Canada.
Results
90 surveys were completed for an overall response rate of 66.7%. Assessments of vital signs, gait, and for features of Parkinsonism were identified as essential by most respondents. There was little consensus on which clinician should be responsible for specific physical examination maneuvers.
Conclusions
While we identified specific physical examination maneuvers deemed by providers to be both necessary and feasible to perform in the context of primary care-based memory clinics, further research is needed to clarify interprofessional roles related to the examination.
Keywords: dementia, assessment, interprofessional, consensus, examination
Introduction
The rising prevalence of Alzheimer’s disease and related dementias (ADRD) is a major global health system challenge. (1) Enhancing health-care system capacity to provide effective early diagnostic and management services is essential to mitigate the impact of ADRD on patients, caregivers, and health-care systems.(2,3) In light of a shortage of geriatric specialists, primary care-based memory clinics (PCMCs) are being established across Canada and other jurisdictions to assess persons with cognitive concerns.(4–11) In Ontario, interdisciplinary assessments in PCMCs support ADRD management in primary care, while identifying and referring individuals who require specialist attention. Initial evaluations suggest that PCMCs can provide timely assessment, lead to a high degree of satisfaction among referring physicians, patients, and caregivers, and streamline access to a specialist.(9–11)
The management of patients with complex chronic conditions such as ADRD in primary care is facilitated by access to allied health professionals and specialist support, time-based physician remuneration, and care processes that provide sufficient time for patient assessment and care planning.(12,13) Nevertheless, time, human resources, and remuneration limitations continue to impose important constraints on chronic disease management in primary care settings. In particular, the diagnosis of ADRD requires a potentially lengthy clinical assessment that includes a detailed history from patients and collateral sources, and psychometric testing.(14) Clinical practice guidelines also recommend that the assessment of a person with cognitive impairment include a physical examination to identify the presence of features specific to particular diagnoses or that might inform management decisions.(15,16) However, descriptions of what constitutes an appropriate physical examination vary widely, with guidelines ranging from vague (e.g., “look for any focal neurological signs”(17)), to detailed—and even exhaustive.(18) Furthermore, recent studies of telemedicine ADRD assessment raise questions about the value of the physical examination.(19,20)
In the resource-constrained primary care context, it is important to identify which, if any, physical examination maneuvers are required to inform the differential diagnosis or management decisions such as referral to a specialist for further assessment.(21) In the context of a larger study to obtain consensus among PCMC clinicians and specialists on a Quality Assurance framework for dementia care,(22) we sought to identify which physical examination maneuvers are essential to ADRD diagnosis and management. We also explored perceptions about which clinicians are best suited to perform specific components of the physical examination.
METHODS
We searched PubMed, Web of Science, Scopus, JAMA evidence, ProQuest, and websites of non-profit and governmental organizations such as the Alzheimer Society of Canada and the National Institutes of Health, to identify literature relating to the physical examination of persons with cognitive impairment. Search terms included Dementia, Physical Examination, Neurological Examination, Diagnosis, Physical Assessment, Guidelines, and Review.
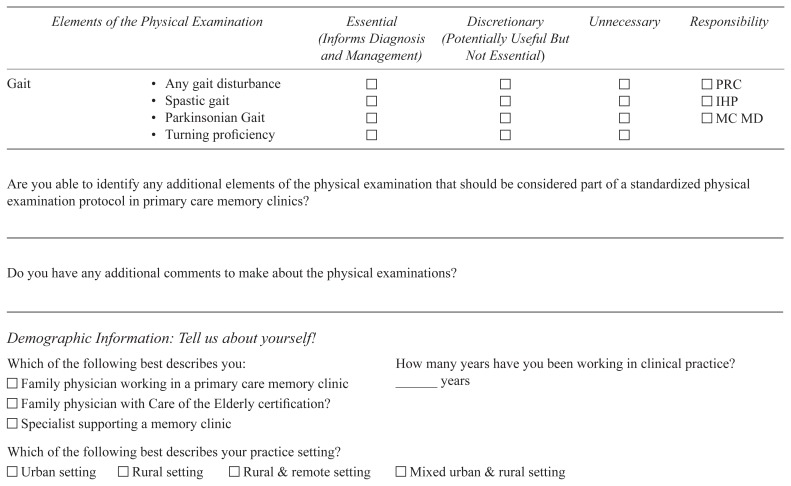
Based on this review, we designed a survey (please see Appendix 1) asking participants to rank physical and neurological examination components as essential (informs assessment and management), discretionary (potentially useful but not essential), or unnecessary to the diagnostic process. The survey also asked participants to identify which health-care providers involved with the PCMC (referring clinicians, PCMC physicians, and/or interprofessional health providers such as nurses and occupational therapists) should be most responsible for the execution of each examination component.
We distributed the survey to 112 family physicians (PCMC MDs) and 23 geriatricians supporting a network of 67 PCMCs in Ontario. Participants completed the survey either in-person during an annual Continuing Medical Education day for PCMCs(23) or online. We distributed a weblink to the online survey via email to all PCMC team members and supporting specialists.
Respondent characteristics (years in practice, location of practice: urban, rural, rural and remote, mixed urban and rural) and open text comments, if any, were collected. We calculated the proportion of respondents who ranked each physical examination maneuver as “essential,” with emerging consensus recognized when ≥60% of rankings were “essential”. Chi-squared and Fisher’s exact tests were used to investigate differences between PCMC MD and specialist responses. We used p < .01 as a stringent threshold for significance to reduce the risk of false positives created by multiple comparisons. We also determined the frequency with which each health-care provider (or providers) was identified as best suited to perform a specific maneuver. We used SAS software version 9.4 (Cary, NC, U.S.A.) for statistical analyses. Summative content analysis was used to analyze and present open text comments.(24) This study was approved by University of Waterloo Office of Research Ethics.
RESULTS
Literature Review
We identified numerous physical examination components relevant to assessments of persons with cognitive impairment which we categorized by system and summarized in Table 1 (please see Appendix 2 for complete reference list).
TABLE 1.
Categories and components of the physical examination
| Category | Components | |
|---|---|---|
| General Physical Examination | Vital signs | Heart rate, respiratory rate, orthostatic vitals |
| Chest | Auscultation | |
| Cardiovascular | Jugular venous pressure, cardiac auscultation, edema | |
| Abdomen | Presence of masses or organomegaly, tenderness | |
| Other | Malnutrition, bruising, hygiene | |
| Neurological Examination | Cranial nerves | Facial movement asymmetry, extraocular movements, pupillary response, optic discs |
| Primitive reflexes | Frontal release signs | |
| Motor (pyramidal) | Weakness, spasticity, hyperreflexia, Babinski/extensor plantar responses | |
| Motor (extrapyramidal) | Tremor, cerebellar findings, rigidity/cogwheeling, facial masking, bradykinesia | |
| Sensory | Glove and stocking numbness, decreased distal proprioception, Romberg’s test | |
| Gait | Any gait disturbance, spastic gait, Parkinsonian gait, turning proficiency |
Respondents
Of 135 surveys distributed, 90 were completed for an overall response rate of 66.7%. Response rates were greater among PCMC physicians (69.6%) than specialists (39.1%). Respondents had extensive clinical practice experience (Table 2); the majority were family physicians (n=78), eight of whom had a Care of the Elderly certification from the College of Family Physicians of Canada; approximately half (53.3%) of the respondents practiced in urban settings.
TABLE 2.
Characteristics of respondents; N = 90
|
Role
|
|||
|---|---|---|---|
| PCMC MD (n=78) | Supporting Specialist (n=9) | Unspecified (n=3) | |
| Mean Years in Clinical Practice | 17.6±12.5 | 16.8±8.6 | 7.7±10.7 |
| Practice Setting (%) | |||
| Urban | 48.7 | 88.9 | 66.7 |
| Rural | 29.2 | 11.1 | 0 |
| Rural and remote | 2.6 | 0 | 33.3 |
| Mixed (rural and urban) | 19.2 | 0 | 0 |
| Lack of respondent response | 0.3 | 0 | 0 |
General Physical Examination
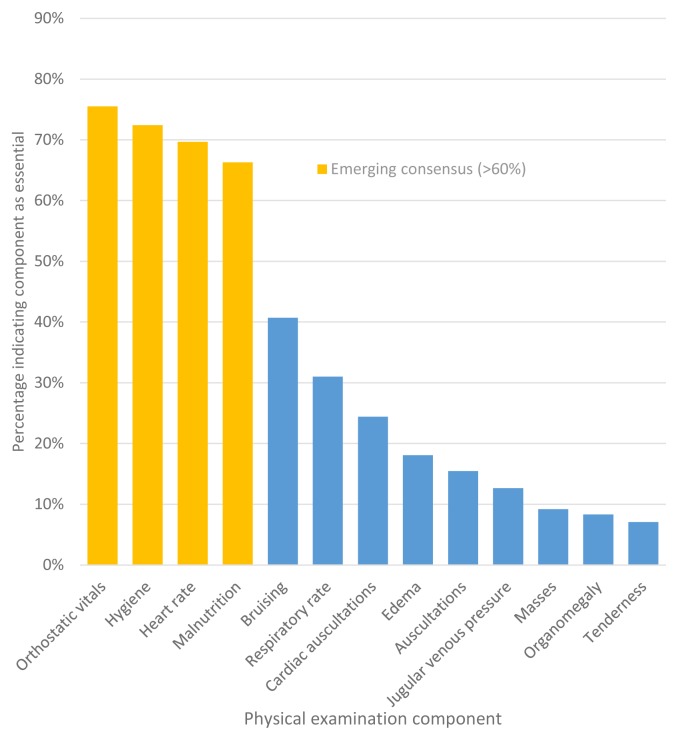
Consensus emerged on four general physical examination maneuvers deemed essential: orthostatic vitals (76%), assessment of hygiene (72%), pulse (70%), and assessment of nutritional status (66%) (Figure 1). Others were ranked as discretionary, with the exception of an abdominal examination, which most respondents considered unnecessary. There were no significant differences between PCMC MD and specialist rankings. Seventy-six percent of PCMC MDs and 89% of specialists suggested that interprofessional health providers be involved in assessing vital signs. Referring clinicians were considered best suited to perform the general physical examination, except for assessments of nutrition, bruising, and hygiene, for which PCMC MDs were considered most suited.
FIGURE 1.
Percentage of respondents indicating each general physical examination component as “essential”; there were no significant differences between PCMC physicians and specialists’ responses
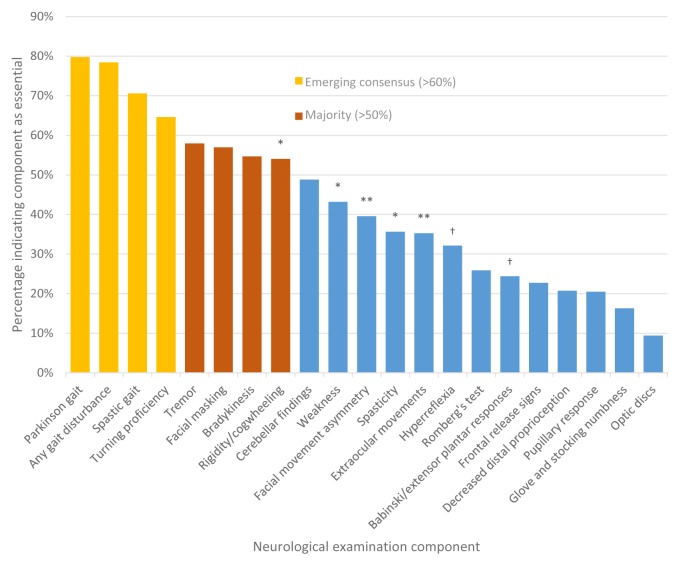
Neurological Examination
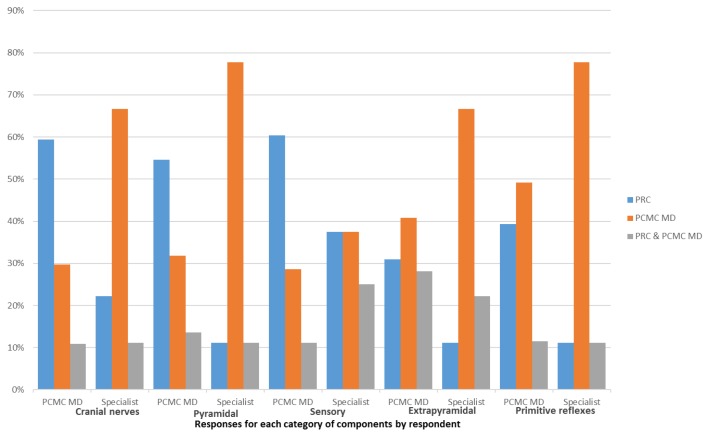
The majority of respondents ranked eight of 21 neurological examination components relating to features of Parkinsonism or gait as essential, but only those pertaining to gait assessment exceeded the threshold for consensus (Figure 2). Specialists were more likely to rate maneuvers to assess pyramidal function as essential, whereas PCMC MDs were more likely to rate these as discretionary. With the exception of gait assessment, respondent opinions were divided as to which health-care provider should perform specific assessments (Figure 3). Interprofessional health providers were most frequently identified as best suited to assess gait. On the other hand, cranial nerves, pyramidal, and sensory assessments were more likely to be designated to referring clinicians by PCMC MDs than by specialists, who considered these the purview of PCMC MDs. Respondents were more likely to identify PCMC MDs as most responsible for a primitive reflex and extrapyramidal assessment.
FIGURE 2.
Percentage of respondents indicating each neurological examination component as essential
* Significant difference between PCMC physicians (PCMC MDs) and specialists’ responses, p<.01.
** Significant difference between PCMC MDs and specialists’ responses, p<.001.
† Significant difference between PCMC MDs and specialists’ responses, p<.0001.
FIGURE 3.
Designated providers by neurological examination component, as identified by survey respondents
PRC = primary referring clinician to PCMC; PCMC MD = PCMC physician.
Open-Text Comments
Twenty-eight participants provided additional comments relating to physical examinations. Thirteen of these comments related to barriers to conducting examinations, with eight citing lack of time to complete a physical examination as part of the memory clinic assessment. Furthermore, six participants desired better communication between PCMCs and referring clinicians, with many suggesting that a standard template be created to document examination findings. There were 10 comments surrounding the overall usefulness of physical examination, with only four endorsing them as important. Others considered most aspects of the examination outside of the scope of PCMC MDs, citing resource and time constraints as the main determinants.
DISCUSSION
This survey of primary care and specialist physicians involved with PCMCs suggests that the most important physical examination maneuvers in the evaluation of patients with cognitive impairment are the assessment of vital signs, gait, and examination for features of Parkinsonism. Specialists considered examination of the pyramidal system as essential, whereas PCMC MDs considered these discretionary. There was little consensus about which provider is best suited to perform specific maneuvers.
PCMCs can play an important role in the community care of persons with dementia, including streamlining access to specialists for patients requiring additional assessment for complex or unusual presentations. In the context of limited resources and complex care processes, physical examination maneuvers with little value to the assessment and management of persons with cognitive impairment should be discarded.(25) According to Bayes’ theorem, a clinically valuable maneuver must allow for meaningful revisions of initial probability estimates to inform management decisions, such as the referral to specialists of patients with unusual neurological features.(26)
PCMCs in Ontario aim to improve access to ADRD care in the most appropriate setting, such that most patients can receive timely diagnosis, management, and interprofessional team-based care within primary care, with the most complex cases, usually requiring a more detailed physical examination, referred to and assessed by specialists. Small case series of telemedicine ADRD assessments by specialist geriatricians reinforce the notion that the physical examination often contributes minimally to a diagnosis.(19) However, the deliberate performance of specific “high-yield” physical examination maneuvers has the potential to reduce the need for diagnostic tests and imaging.(26)
An important consideration is the erosion of clinical skills in physical(26) and neurological(27) examinations, which has been documented among physicians and other professionals(28) who may have limited confidence and ability to perform and interpret necessary examination maneuvers, and may thus not recognize their potential importance.(26,27,29) We have previously shown that close integration of specialists within PCMCs can serve as a means to increase capacity, and this could apply to training related to a standardized physical examination.(22,30) Furthermore, the lack of agreement among respondents regarding which providers are best suited for specific assessment components mirrors our previous results regarding the integration of PCMCs within the broader health system, and the related need for clarity on mutually understood roles among all clinicians across the system.(22)
Limitations
Certain limitations of this work must be emphasized. There was a low response rate from specialists compared to PCMC MDs, so overall results are more reflective of PCMC MD perceptions. The exclusion of other health-care professionals precludes commenting on the applicability of findings to settings with access to other disciplines. In addition, our findings may not be applicable to other ADRD primary care models that do not triage the most complex patients to specialists, which is a standard feature of PCMCs in Ontario. Lastly, though a formal systematic literature review was not conducted to identify all possible physical examination components in the assessment of persons with suspected ADRD, the review of published guidelines and compendiums likely identified examination maneuvers potentially most relevant to PCMC MDs.
CONCLUSIONS
This study has found that most PCMC MDs and specialists consider that the assessment of gait, vital signs (including orthostatic vitals), and features of Parkinsonism is sufficient for most patients being assessed for possible ADRD in the context of a PCMC. Disagreement existed between specialists and PCMC physicians regarding assessment of the pyramidal system. There was no consensus on which provider should be responsible for specific physical examination maneuvers. Optimal and efficient care of seniors with complex conditions requires greater system integration, and a shared and mutually agreed upon understanding among providers of tasks, roles, and accountability. Greater integration of PCMC clinics and specialists will not only facilitate capacity building, but also permit further research to elucidate the clinical utility of specific physical examination components in the assessment of persons with cognitive impairment.
ACKNOWLEDGEMENTS
This study was supported by funding from the Alzheimer Society of Canada.
APPENDICES
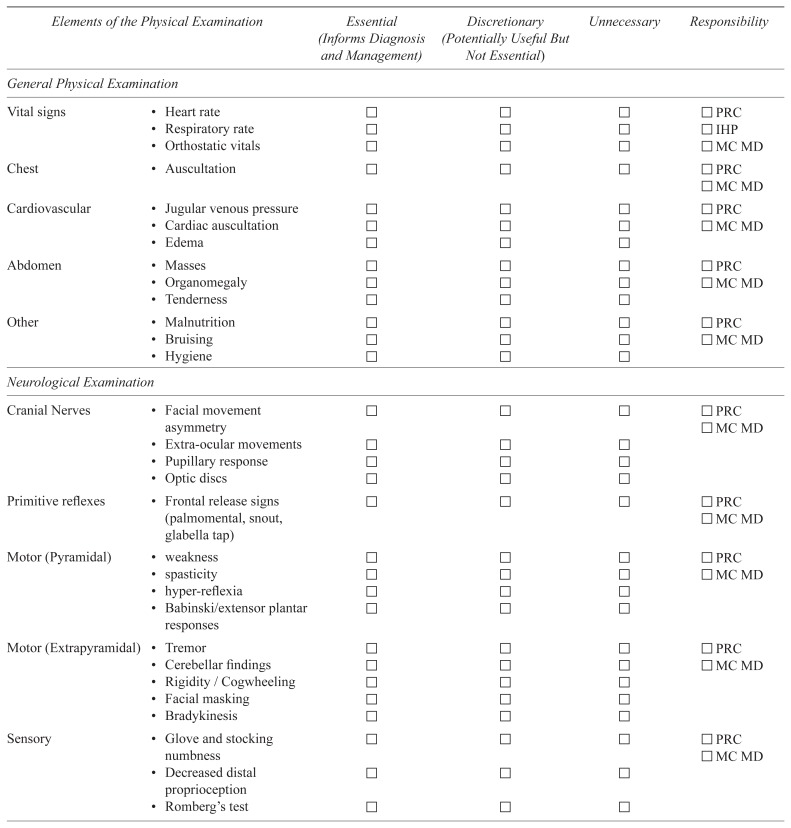
APPENDIX 1. Physical examination survey presented to participants
Please rate the extent to which you consider that each element of the physical examination is essential/important to the diagnostic process in primary care-based memory clinics, using the following scale: Essential, Discretionary, Unnecessary. In addition, please indicate who should be responsible for completing the element (PRC = primary referring clinician—family physician/nurse practitioner; MC MD = memory clinic physician; IHP = interprofessional health provider).
APPENDIX 2. Categories and components of the physical examination
| Category | Components | Guideline(s) Indicating Components | |
|---|---|---|---|
| General physical examination(5–15) | Vital signs(16,17) | Heart rate, respiratory rate, orthostatic vitals(18) | Third Canadian Consensus Conference on Diagnosis and Treatment of Dementia(1), European Federation of Neurological Societies (EFNS)(2), Ministry of Health Singapore (MOHS)(3), Clinical Research Center for Dementia of South Korea (CRCDSK)(4) |
| Chest | Auscultation | ||
| Cardiovascular | Jugular venous pressure, cardiac auscultation, edema | ||
| Abdomen | Presence of masses or organomegaly, tenderness(19) | ||
| Other(20) | Malnutrition, bruising, hygiene | ||
| Neurological examination(6–8,10,14,17,18) | Cranial nerves (16,21) | Facial movement asymmetry, extraocular movements, pupillary response, optic discs | EFNS, MOHS |
| Primitive reflexes | Frontal release signs | MOHS | |
| Motor (pyramidal) (16,22,23) | Weakness, spasticity, hyperreflexia, Babinski/extensor plantar responses24 | EFNS, MOHS | |
| Motor (extrapyramidal) (16,22) | Tremor, cerebellar findings, rigidity/cogwheeling, facial masking, bradykinesia | EFNS, MOHS, CRCDSK | |
| Sensory(16,20, 1) | Glove and stocking numbness, decreased distal proprioception, Romberg’s test | EFNS, MOHS | |
| Gait(20,23) | Any gait disturbance(24), spastic gait, Parkinsonian gait, turning proficiency | EFNS, MOHS |
REFERENCES
- 1.Third Canadian Consensus Conference on Diagnosis and Treatment of Dementia. Final Recommendations. 2007. [Accessed 2017 August 1]. Available from: http://www.cccdtd.ca/pdfs/Final_Recommendations_CCCDTD_2007.pdf.
- 2.Sorbi S, Hort J, Erkinjuntti T, et al. EFNS-ENS Guidelines on the diagnosis and management of disorders associated with dementia. Eur J Neurol. 2012;19(9):1159–79. doi: 10.1111/j.1468-1331.2012.03784.x. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health Singapore. Dementia MOH Clinical Practice Guidelines. 2013. [Accessed 2017 August 1]. Available from: https://www.moh.gov.sg/content/dam/moh_web/HPP/Doctors/cpg_medical/current/2013/Dementia/Dementia%2010%20Jul%202013%20-%20Booklet.pdf.
- 4.Clinical Research Center for Dementia of South Korea. Clinical practice guideline for dementia Part I: Diagnosis & evaluation. Seoul, Republic of Korea: Clinical Research Center for Dementia of South Korea; 2011. [Accessed 2017 August 1]. Available from: http://jkma.org/src/SM/jkma-54-861-s002.pdf. [Google Scholar]
- 5.Fortinsky RH, Wasson JH. How do physicians diagnose dementia? Evidence from clinical vignette responses. Am J Alzheimers Dis Other Demen. 1997;12(2):51–61. [Google Scholar]
- 6.Patterson CJ, Gauthier S, Bergman H, et al. The recognition, assessment and management of dementing disorders: conclusions from the Canadian Consensus Conference on Dementia. CMAJ. 1999;160(12 Suppl):S1–S15. Epub 1999/07/20. [PMC free article] [PubMed] [Google Scholar]
- 7.Dementia Study Group of the Italian Neurological Society. Guidelines for the diagnosis of dementia and Alzheimer’s disease. Neurol Sci. 2000;21(4):187–94. doi: 10.1007/s100720070075. [DOI] [PubMed] [Google Scholar]
- 8.Musicco M, Caltagirone C, Sorbi S, et al. Italian Neurological Society guidelines for the diagnosis of dementia: revision I. Neurol Sci. 2004;25(3):154–67. doi: 10.1007/s10072-004-0252-1. [DOI] [PubMed] [Google Scholar]
- 9.Robillard A. Clinical diagnosis of dementia. Alzheimers Dement. 2007;3(4):292–98. doi: 10.1016/j.jalz.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Hort J, O’Brien JT, Gainotti G, et al. EFNS guidelines for the diagnosis and management of Alzheimer’s disease. Eur J Neurol. 2010;17(10):1236–48. doi: 10.1111/j.1468-1331.2010.03040.x. [DOI] [PubMed] [Google Scholar]
- 11.Alves L, Correia AS, Miguel R, et al. Alzheimer’s disease: a clinical practice-oriented review. Front Neurol. 2012;3:63. doi: 10.3389/fneur.2012.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galvin JE, Sadowsky CH, Nincds A. Practical guidelines for the recognition and diagnosis of dementia. J Am Board Fam Med. 2012;25(3):367–82. doi: 10.3122/jabfm.2012.03.100181. [DOI] [PubMed] [Google Scholar]
- 13.Alzheimer Society of Canada [website] The diagnostic process: assessments and tests. Toronto, ON: Alzheimer Society of Canada; 2015. [Accessed 2017 August 1]. Available from: http://www.alzheimer.ca/en/About-dementia/Diagnosis/Assessments-and-tests. [Google Scholar]
- 14.Alzheimer’s Association [website] Tests for Alzheimer’s disease and dementia. Chicago, IL: Alzheimer’s Association; 2016. [Accessed 2017 August 1]. Available from: http://www.alz.org/alzheimers_disease_steps_to_diagnosis.asp. [Google Scholar]
- 15.Holsinger T, Deveau J, Boustani M, et al. Does this patient have dementia? JAMA. 2007;297(21):2391–404. doi: 10.1001/jama.297.21.2391. [DOI] [PubMed] [Google Scholar]
- 16.National Chronic Care Consortium and the Alzheimer’s Association. Chronic Care Networks for Alzheimer’s Disease initiative. Chicago, IL: Alzheimer’s Association; 2003. [Accessed 2017 August 1]. Tools for early identification, assessment, and treatment for people with Alzheimer’s disease and dementia. Available from: http://www.alz.org/documents/national/CCN-AD03.pdf. [Google Scholar]
- 17.Christensen MD, White HK. Dementia assessment and management. J Am Med Dir Assoc. 2007;8(3 Suppl 2):e89–e98. doi: 10.1016/j.jamda.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 18.National Institutes of Health [website] The dementias: hope through research. Bethesda, MD: National Institutes of Health; 2015. [Accessed 2017 August 1]. Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Dementia-Hope-Through-Research#19213_10. [Google Scholar]
- 19.Waldemar G, Dubois B, Emre M, et al. Recommendations for the diagnosis and management of Alzheimer’s disease and other disorders associated with dementia: EFNS guideline. Eur J Neurol. 2007;14(1):e1–e26. doi: 10.1111/j.1468-1331.2006.01605.x. [DOI] [PubMed] [Google Scholar]
- 20.Finkel SI, Woodson C. History and physical examination of elderly patients with dementia. Int Psychogeriatr. 1997;9(Suppl 1):71–75. doi: 10.1017/s1041610297004729. [DOI] [PubMed] [Google Scholar]
- 21.Bothe MR, Uttner I, Otto M. Sharpening the boundaries of Parkinson-associated dementia: recommendation for a neuropsychological diagnostic procedure. J Neural Transm (Vienna) 2010;117(3):353–67. doi: 10.1007/s00702-010-0370-2. [DOI] [PubMed] [Google Scholar]
- 22.Small GW, Rabins PV, Barry PP, et al. Diagnosis and treatment of Alzheimer disease and related disorders. Consensus statement of the American Association for Geriatric Psychiatry, the Alzheimer’s Association, and the American Geriatrics Society. JAMA. 1997;278(16):1363–71. [PubMed] [Google Scholar]
- 23.Simmons BB, Hartmann B, Dejoseph D. Evaluation of suspected dementia. Am Fam Physician. 2011;84(8):895–902. [PubMed] [Google Scholar]
- 24.Feldman HH, Jacova C, Robillard A, et al. Diagnosis and treatment of dementia: 2. Diagnosis. CMAJ. 2008;178(7):825–36. doi: 10.1503/cmaj.070798. [DOI] [PMC free article] [PubMed] [Google Scholar]
Footnotes
Previously presented as an abstract at the 35th Annual Scientific Meeting of the Canadian Geriatrics Society, Montreal, April 2015.
CONFLICT OF INTEREST DISCLOSURES
VB receives salary support from CIHR, Conestoga College, and Schlegel Villages. DS served on an advisory board for Eli-Lilly in 2013. We have no other conflicts of interest to declare.
REFERENCES
- 1.Prince M, Bryce R, Albanese E, et al. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63–75 e2. doi: 10.1016/j.jalz.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Wimo A, Jonsson L, Bond J, et al. The worldwide economic impact of dementia 2010. Alzheimers Dement. 2013;9(1):1–11 e3. doi: 10.1016/j.jalz.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 3.Connell CM, Janevic MR, Gallant MP. The costs of caring: impact of dementia on family caregivers. J Geriatr Psychiatry Neurol. 2001;14(4):179–87. doi: 10.1177/089198870101400403. [DOI] [PubMed] [Google Scholar]
- 4.Abrams RC, Young RC. Crisis in access to care: geriatric psychiatry services unobtainable at any price. Public Health Rep. 2006;121(6):646–49. doi: 10.1177/003335490612100603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hogan DB, Borrie M, Basran JF, et al. Specialist physicians in geriatrics—report of the Canadian Geriatrics Society Physician Resource Work Group. Can Geriatr J. 2012;15(3):68–79. doi: 10.5770/cgj.15.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sumaya CV, Opara CM, Espino DV. The geriatrician and geriatric psychiatrist workforce in Texas: characteristics, challenges, and policy implications. J Aging Health. 2013;25(6):1050–64. doi: 10.1177/0898264313497511. [DOI] [PubMed] [Google Scholar]
- 7.Callahan CM, Boustani MA, Weiner M, et al. Implementing dementia care models in primary care settings: The Aging Brain Care Medical Home. Aging Ment Health. 2011;15(1):5–12. doi: 10.1080/13607861003801052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greening L, Greaves I, Greaves N, et al. Positive thinking on dementia in primary care: Gnosall Memory Clinic. Community Pract. 2009;82(5):20–23. [PubMed] [Google Scholar]
- 9.Morgan DG, Crossley M, Kirk A, et al. Improving access to dementia care: development and evaluation of a rural and remote memory clinic. Aging Ment Health. 2009;13(1):17–30. doi: 10.1080/13607860802154432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vickrey BG, Mittman BS, Connor KI, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Ann Intern Med. 2006;145(10):713–26. doi: 10.7326/0003-4819-145-10-200611210-00004. [DOI] [PubMed] [Google Scholar]
- 11.Lee L, Hillier LM, Stolee P, et al. Enhancing dementia care: a primary care-based memory clinic. J Am Geriatr Soc. 2010;58(11):2197–204. doi: 10.1111/j.1532-5415.2010.03130.x. [DOI] [PubMed] [Google Scholar]
- 12.Beaulieu MD, Haggerty J, Tousignant P, et al. Characteristics of primary care practices associated with high quality of care. CMAJ. 2013;185(12):e590–96. doi: 10.1503/cmaj.121802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee L, Heckman G, McKelvie R, et al. Physicians’ perceptions of capacity building for managing chronic disease in seniors using integrated interprofessional care models. Can Fam Physician. 2015;61(3):e148–57. [PMC free article] [PubMed] [Google Scholar]
- 14.Moore A, Patterson C, Lee L, et al. Fourth Canadian Consensus Conference on the Diagnosis and Treatment of Dementia: recommendations for family physicians. Can Fam Physician. 2014;60(5):433–38. [PMC free article] [PubMed] [Google Scholar]
- 15.Sorbi S, Hort J, Erkinjuntti T, et al. EFNS-ENS Guidelines on the diagnosis and management of disorders associated with dementia. Eur J Neurol. 2012;19(9):1159–79. doi: 10.1111/j.1468-1331.2012.03784.x. [DOI] [PubMed] [Google Scholar]
- 16.Ngo J, Holroyd-Leduc JM. Systematic review of recent dementia practice guidelines. Age Ageing. 2015;44(1):25–33. doi: 10.1093/ageing/afu143. [DOI] [PubMed] [Google Scholar]
- 17.Robinson L, Tang E, Taylor JP. Dementia: timely diagnosis and early intervention. BMJ. 2015;350:h3029. doi: 10.1136/bmj.h3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scott KR, Barrett AM. Dementia syndromes: evaluation and treatment. Expert Rev Neurother. 2007;7(4):407–22. doi: 10.1586/14737175.7.4.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin-Khan M, Flicker L, Wootton R, et al. The diagnostic accuracy of telegeriatrics for the diagnosis of dementia via video conferencing. J Am Med Dir Assoc. 2012;13(5):487 e19–24. doi: 10.1016/j.jamda.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Martin-Khan M, Varghese P, Wootton R, et al. Differences in diagnosis for cognitive assessment following an in-person physical examination versus a telegeriatric evaluation. Alzheimers Dement. 2009;5(5):e6. [Google Scholar]
- 21.Reuben DB, Roth C, Kamberg C, et al. Restructuring primary care practices to manage geriatric syndromes: the ACOVE-2 intervention. J Am Geriatr Soc. 2003;51(12):1787–93. doi: 10.1046/j.1532-5415.2003.51565.x. [DOI] [PubMed] [Google Scholar]
- 22.Heckman GA, Boscart VM, Franco BB, et al. Quality of dementia care in the community: identifying key quality assurance components. Can Geriatr J. 2016;19(4):164–81. doi: 10.5770/cgj.19.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee L, Kasperski MJ, Weston WW. Building capacity for dementia care. Training program to develop primary care memory clinics. Can Fam Physician. 2011;57(7):e249–52. [PMC free article] [PubMed] [Google Scholar]
- 24.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 25.Mangione S, Peitzman SJ. Physical diagnosis in the 1990s. Art or artifact? J Gen Intern Med. 1996;11(8):490–93. doi: 10.1007/BF02599046. [DOI] [PubMed] [Google Scholar]
- 26.Herrle SR, Corbett EC, Jr, Fagan MJ, et al. Bayes’ theorem and the physical examination: probability assessment and diagnostic decision-making. Acad Med. 2011;86(5):618–27. doi: 10.1097/ACM.0b013e318212eb00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nicholl DJ, Appleton JP. Clinical neurology: why this still matters in the 21st century. J Neurol Neurosurg Psychiatry. 2015;86(2):229–33. doi: 10.1136/jnnp-2013-306881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fennessey A, Wittmann-Price RA. Physical assessment: a continuing need for clarification. Nurs Forum. 2011;46(1):45–50. doi: 10.1111/j.1744-6198.2010.00209.x. [DOI] [PubMed] [Google Scholar]
- 29.Moore FGA, Chalk C. The essential neurologic examination. What should medical students be taught? Neurology. 2009;72(23):2020–23. doi: 10.1212/WNL.0b013e3181a92be6. [DOI] [PubMed] [Google Scholar]
- 30.Heckman GA. Integrated care for the frail elderly. Health Care Pap. 2011;11(1):62–68. doi: 10.12927/hcpap.2011.22255. discussion 86–91. [DOI] [PubMed] [Google Scholar]
- 1.Third Canadian Consensus Conference on Diagnosis and Treatment of Dementia. Final Recommendations. 2007. [Accessed 2017 August 1]. Available from: http://www.cccdtd.ca/pdfs/Final_Recommendations_CCCDTD_2007.pdf.
- 2.Sorbi S, Hort J, Erkinjuntti T, et al. EFNS-ENS Guidelines on the diagnosis and management of disorders associated with dementia. Eur J Neurol. 2012;19(9):1159–79. doi: 10.1111/j.1468-1331.2012.03784.x. [DOI] [PubMed] [Google Scholar]
- 3.Ministry of Health Singapore. Dementia MOH Clinical Practice Guidelines. 2013. [Accessed 2017 August 1]. Available from: https://www.moh.gov.sg/content/dam/moh_web/HPP/Doctors/cpg_medical/current/2013/Dementia/Dementia%2010%20Jul%202013%20-%20Booklet.pdf.
- 4.Clinical Research Center for Dementia of South Korea. Clinical practice guideline for dementia Part I: Diagnosis & evaluation. Seoul, Republic of Korea: Clinical Research Center for Dementia of South Korea; 2011. [Accessed 2017 August 1]. Available from: http://jkma.org/src/SM/jkma-54-861-s002.pdf. [Google Scholar]
- 5.Fortinsky RH, Wasson JH. How do physicians diagnose dementia? Evidence from clinical vignette responses. Am J Alzheimers Dis Other Demen. 1997;12(2):51–61. doi: 10.1177/153331759701200202. [DOI] [Google Scholar]
- 6.Patterson CJ, Gauthier S, Bergman H, et al. The recognition, assessment and management of dementing disorders: conclusions from the Canadian Consensus Conference on Dementia. CMAJ. 1999;160(12 Suppl):S1–S15. Epub 1999/07/20. [PMC free article] [PubMed] [Google Scholar]
- 7.Dementia Study Group of the Italian Neurological Society. Guidelines for the diagnosis of dementia and Alzheimer’s disease. Neurol Sci. 2000;21(4):187–94. doi: 10.1007/s100720070075. [DOI] [PubMed] [Google Scholar]
- 8.Musicco M, Caltagirone C, Sorbi S, et al. Italian Neurological Society guidelines for the diagnosis of dementia: revision I. Neurol Sci. 2004;25(3):154–67. doi: 10.1007/s10072-004-0252-1. [DOI] [PubMed] [Google Scholar]
- 9.Robillard A. Clinical diagnosis of dementia. Alzheimers Dement. 2007;3(4):292–98. doi: 10.1016/j.jalz.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Hort J, O’Brien JT, Gainotti G, et al. EFNS guidelines for the diagnosis and management of Alzheimer’s disease. Eur J Neurol. 2010;17(10):1236–48. doi: 10.1111/j.1468-1331.2010.03040.x. [DOI] [PubMed] [Google Scholar]
- 11.Alves L, Correia AS, Miguel R, et al. Alzheimer’s disease: a clinical practice-oriented review. Front Neurol. 2012;3:63. doi: 10.3389/fneur.2012.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galvin JE, Sadowsky CH, Nincds A. Practical guidelines for the recognition and diagnosis of dementia. J Am Board Fam Med. 2012;25(3):367–82. doi: 10.3122/jabfm.2012.03.100181. [DOI] [PubMed] [Google Scholar]
- 13.Alzheimer Society of Canada [website] The diagnostic process: assessments and tests. Toronto, ON: Alzheimer Society of Canada; 2015. [Accessed 2017 August 1]. Available from: http://www.alzheimer.ca/en/About-dementia/Diagnosis/Assessments-and-tests. [Google Scholar]
- 14.Alzheimer’s Association [website] Tests for Alzheimer’s disease and dementia. Chicago, IL: Alzheimer’s Association; 2016. [Accessed 2017 August 1]. Available from: http://www.alz.org/alzheimers_disease_steps_to_diagnosis.asp. [Google Scholar]
- 15.Holsinger T, Deveau J, Boustani M, et al. Does this patient have dementia? JAMA. 2007;297(21):2391–404. doi: 10.1001/jama.297.21.2391. [DOI] [PubMed] [Google Scholar]
- 16.National Chronic Care Consortium and the Alzheimer’s Association. Chronic Care Networks for Alzheimer’s Disease initiative. Chicago, IL: Alzheimer’s Association; 2003. [Accessed 2017 August 1]. Tools for early identification, assessment, and treatment for people with Alzheimer’s disease and dementia. Available from: http://www.alz.org/documents/national/CCN-AD03.pdf. [Google Scholar]
- 17.Christensen MD, White HK. Dementia assessment and management. J Am Med Dir Assoc. 2007;8(3 Suppl 2):e89–e98. doi: 10.1016/j.jamda.2006.12.011. [DOI] [PubMed] [Google Scholar]
- 18.National Institutes of Health [website] The dementias: hope through research. Bethesda, MD: National Institutes of Health; 2015. [Accessed 2017 August 1]. Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Dementia-Hope-Through-Research#19213_10. [Google Scholar]
- 19.Waldemar G, Dubois B, Emre M, et al. Recommendations for the diagnosis and management of Alzheimer’s disease and other disorders associated with dementia: EFNS guideline. Eur J Neurol. 2007;14(1):e1–e26. doi: 10.1111/j.1468-1331.2006.01605.x. [DOI] [PubMed] [Google Scholar]
- 20.Finkel SI, Woodson C. History and physical examination of elderly patients with dementia. Int Psychogeriatr. 1997;9(Suppl 1):71–75. doi: 10.1017/S1041610297004729. [DOI] [PubMed] [Google Scholar]
- 21.Bothe MR, Uttner I, Otto M. Sharpening the boundaries of Parkinson-associated dementia: recommendation for a neuropsychological diagnostic procedure. J Neural Transm (Vienna) 2010;117(3):353–67. doi: 10.1007/s00702-010-0370-2. [DOI] [PubMed] [Google Scholar]
- 22.Small GW, Rabins PV, Barry PP, et al. Diagnosis and treatment of Alzheimer disease and related disorders. Consensus statement of the American Association for Geriatric Psychiatry, the Alzheimer’s Association, and the American Geriatrics Society. JAMA. 1997;278(16):1363–71. doi: 10.1001/jama.1997.03550160083043. [DOI] [PubMed] [Google Scholar]
- 23.Simmons BB, Hartmann B, Dejoseph D. Evaluation of suspected dementia. Am Fam Physician. 2011;84(8):895–902. [PubMed] [Google Scholar]
- 24.Feldman HH, Jacova C, Robillard A, et al. Diagnosis and treatment of dementia: 2. Diagnosis. CMAJ. 2008;178(7):825–36. doi: 10.1503/cmaj.070798. [DOI] [PMC free article] [PubMed] [Google Scholar]