Introduction
Intravesical administration of BCG < Bacillus Calmette Guerin> a live attenuated strain of Mycobacterium Bovis has become a mainstay of adjunctive therapy for superficial (non-muscle invasive) bladder cancer, The most common complications associated with BCG treatment are relatively minor. They include urinary frequency, cystitis, fever, and hematuria. Although serious complications are rare, patients can develop severe, life-threatening sepsis with disseminated mycobacterial infection. More serious complications include granulomatous prostatitis, pneumonitis, and hepatitis. Most of the BCG immunotherapy-associated symptoms are a result of the immune stimulation that is required to effectively eradicate cancer cells 1.
Case report
A 52-year-old man with low -grade non-muscle invasive bladder cancer was managed with transurethral resection followed by Bacillus Calmette-Guérin (BCG) course 5 years ago, one month ago he was diagnosed with tumor relapse that needs another treatment with BCG bladder instillation.
The recent catheterisation had been easy and non traumatic,after the 3rd dose of BCG the patient develop high grade fever >48h,chills,nausea and vomiting. Examination revealed normal pulse, blood pressure and respiratory rate. Temperature was initially 39 °C, but rose to 39.4 °C later on that day. Oxygen saturations were 93% on room air. Examination of the heart, chest and abdomen was normal. Initial blood tests included a white blood cell count of 4.9 × 109/L and C-reactive protein of 28 mg/L with high liver enzymes: SGOT203U/L,SGPT249U/L,GGT394,Alkaline phosphatase941U/L, bilirubine total 1.44,direct 0.56, a diagnosis of cholangitis was suggested,patient started on broad spectrum antibiotics and didn't improved.Ultrasound of the abdomen was normal with no dilatation of common bile duct,MRCP done and it was normal, patient still having high grade fever with high LFT'S. Three sets of blood cultures showed no bacterial growth, and the urine specimen from admission showed normal results. A systemic BCG infection was suspected on the basis of the recent BCG instillation and the failure to improve despite several days of antibiotic treatment.PCR in blood for mycobacterial DNA was negative.
A liver biopsy was performed 7 days after BCG bladder instillation, Histological examination showed several noncaseating epitheloid granulomas. No acid-fast bacilli were seen with Ziehl-Neelsen staining,culture of liver tissue for Mycobacteria Bovis was negative.
The PCR performed on homogenised liver tissue was positive for mycobacteria Bovis.
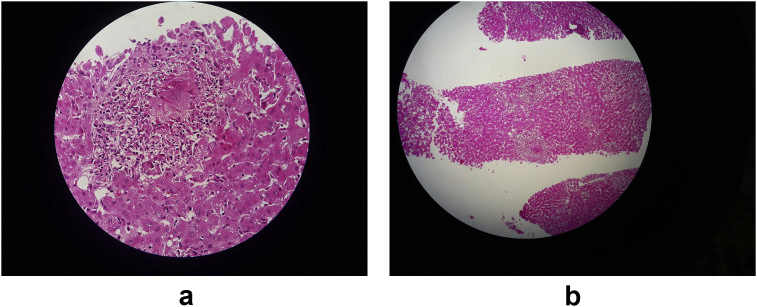
A systemic BCG infection causing granulomatous hepatitis was diagnosed(Fig. 1a–b) and treatment with isoniazid and rifampicin and ethambutol was started 10 days of BCG instillation.
Figure 1.
a/b: Non caseating granuloma seen in liver biopsy.
The clinical condition of the patient gradually improved. Fever subsided after two weeks of treatment. Liver enzymes decreased after two weeks of treatment. Currently the patient is in a good clinical condition and the liver function tests are normal.
Discussion
Disseminated BCG disease is a rare but life-threatening complication of BCG administration. The spectrum of symptoms may be similar to that of tuberculosis infection, including persistent fever, night sweats and weight loss. The pathogenesis is thought to involve a combination of mycobacteraemia and local inflammatory hypersensitivity at various sites including the liver. This is supported by the identification of M. bovis in some reported cases.2,3 Lamn et al reported that granulomatous hepatitis occurred with a probability of 0.7% 1 The pathogenesis of the granulomatous hepatitis is unclear. Because of the importance of distinguishing between a hypersensitivity reaction and infection for treatment of our patient, we used a recently developed PCR to assess mycobacterial DNA. M bovis dissemination is clinically and pathologically indistinguishable from M tuberculosis, and therefore a primer targeting the pncA gene of M bovis was also performed, based on the fact that the sequence of the pncA gene for the 2 strains differs at the 169C position (C[G). The PCR proved the presence of DNA from Myco bovis BCG in the patient's liver tissue. The rapidity with which an accurate result is obtained with PCR is especially important because Ziehl-Neelsen staining for mycobacteria is frequently negative, as in our case. The granulomatous hepatitis was caused by BCG infection of the liver after haematogenous dissemination of BCG, rather than hypersensitivity. Patients with granulomatous hepatitis present with symptoms and signs of hepatitis, including fever, anorexia and jaundice. Non-caseating granulomas and eosinophilia can be found on liver biopsies from these patients.4
Mycobacterium bovis BCG and M. Bovis are intrinsically resistant to pyrazinamide. Resistance to β-lactams, macrolides (except clarithromycin) and some aminoglycosides has recently been reported. The suggested first-line antimicrobial treatment for M. Bovis BCG is isoniazide 300 mg daily and rifampin 600 mg daily with or without ethambutol 1200 mg daily by mouth for 6 months.5
Conclusion
We encountered a case of Granulomatous hepatitis caused by Bacillus Calmette-Guerin (BCG) infection after BCG bladder instillation for bladder cancer, the granulomatous hepatitis was caused by BCG infection of the liver after haematogenous dissemination of BCG, rather than hypersensitivity.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eucr.2018.05.012
Contributor Information
M. Moussa, Email: mohamadamoussa@hotmail.com.
M. Abou Chakra, Email: mohamedabouchakra@hotmail.com.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Lamm D.L. Efficacy and safety of bacille Calmette-Guérin immunotherapy in superficial bladder. Clin Infect Dis. 2000;31(Suppl 3):S86–90. doi: 10.1086/314064. [DOI] [PubMed] [Google Scholar]
- 2.Kristjansson M., Green P., Manning H.L. Molecular confirmation of bacillus Calmette–Guerin as the cause of pulmonary infection following urinary tract instillation. Clin Infect Dis. 1993;17(2):228–230. doi: 10.1093/clinids/17.2.228. [DOI] [PubMed] [Google Scholar]
- 3.McParland D.J., Cotton K.S., Gowda V.H., Hoeppner W.T., Martin P.F. WeckworthMiliary Mycobacterium bovis induced by intravesical bacilli Calmette–Guerin immunotherapy. Am Rev Respir Dis. 1992;146(5:1):1330–1333. doi: 10.1164/ajrccm/146.5_Pt_1.1330. [DOI] [PubMed] [Google Scholar]
- 4.Case records of the Massachusetts General Hospital Weekly clinicopathological exercises. Case 29-1998. A 57-year-old man with fever and jaundice after intravesical instillation of bacille Calmette-Guérin for bladder cancer. N Engl J Med. 1998 Sep 17;339(12):831–837. doi: 10.1056/NEJM199809173391209. [DOI] [PubMed] [Google Scholar]
- 5.Management of complications of bacillus Calmette-Guérin immunotherapy in the treatment of bladder cancer. Huang TCAnn Pharmacother. 2000 Apr;34(4):529–532. doi: 10.1345/aph.19145. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.