Abstract
Objective
The Care Transitions Intervention (CTI) has potential to improve the emergency department (ED)-to-home transition for older adults. Community paramedics may function as the CTI coaches; however, this requires the appropriate knowledge, skills, and attitudes, which they do not receive in traditional emergency medical services (EMS) education. This study aimed to define community paramedics’ perceptions regarding their training needs to serve as CTI coaches supporting the ED-to-home transition.
Methods
This study forms part of an ongoing randomized controlled trial evaluating a community paramedic-implemented CTI to enhance the ED-to-home transition. The community paramedics’ training covered the following domains: the CTI program, geriatrics, effective coaching, ED discharge processes, and community paramedicine. Sixteen months after starting the study, we conducted audio-recorded semi-structured interviews with community paramedics at both study sites. After transcribing the interviews, team members independently coded the transcripts. Ensuing group analysis sessions led to the development of final codes and identifying common themes. Finally, we conducted member checking to confirm our interpretations of the interview data.
Results
We interviewed all eight participating community paramedics. Participants consisted solely of non-Hispanic whites, included five women, and had a mean age of 43. Participants had extensive backgrounds in healthcare, primarily as EMS providers, but minimal experience with community paramedicine. All reported some prior geriatrics training. Four themes emerged from the interviews: (1) paramedics with positive attitudes and willing to acquire the needed knowledge and skills will succeed as CTI coaches; (2) active rather than passive learning is preferred by paramedics; (3) the existing training could benefit from adjustments such as added content on mental health, dementia, and substance abuse issues, as well as content on coaching subjects with a range of illness severity; and (4) continuing education should address the paramedic coaches’ evolving needs as they develop proficiency with the CTI.
Conclusions
Paramedics as CTI coaches represent an untapped resource for supporting ED-to-home care transitions. Our results provide the necessary first step to make the community paramedic CTI coach more successful. These findings may apply to training for similar community paramedicine roles, but additional research must investigate this possibility.
Keywords: Care transitions, community paramedicine, older adults
INTRODUCTION
Older adults use emergency care at the highest rate of any age group in the United States.1,2,3,4 Moreover, within one month of discharge from the emergency department (ED), up to 20% return to the ED for further care, require hospital admission, or die.5,6,7,8 Prior studies have identified potential reasons for such poor outcomes. These include older patients’ failure to follow up with primary care, adhere to prescribed medications, and understand “red flag” symptoms. Poor care transitions between different health care providers may also contribute to the problem.9,10,11,12,13,14
Given the success of evidence-based transitional care programs in the acute care setting, an effective program improving the ED-to-home transition has a high likelihood of enhancing healthcare for many older adults, including decreasing return visits to the ED. A potential solution is to translate the Care Transitions Intervention (CTI) from the hospital-to-home setting to the ED-to-home setting. The CTI uses a coaching strategy, traditionally delivered by specially trained nurses, to enhance patients’ self-care capacity following hospital discharge, resulting in a 30% decrease in hospital readmissions within 30 days.15,16,17 Although we currently do not know the effect of the CTI on outcomes after ED discharge, we are pursuing that research in our larger project.
Although community paramedics have not yet, to our knowledge, served as CTI coaches, they may represent a viable option, particularly for high-volume ED-to-home programs that must serve patients soon after discharge home from the ED. Like nurses, paramedics find themselves well-positioned to serve in this role. However, unlike nurses, paramedics serve in all communities and have universal availability (including evenings, nights, and weekends). Additionally, whereas transitional care nurses are in short supply in some areas, paramedics are under-utilized in many communities.12,18,19 Importantly, the CTI coach role differs in important ways from that of the traditional paramedic: while paramedics act quickly to solve immediate problems, coaches assist patients through active listening and encouragement to solve their own problems. A successful community paramedic-delivered CTI program requires that paramedics possess CTI-appropriate attitude, knowledge, and skills, which they do not receive in traditional emergency medical services (EMS) education.
Accordingly, this study aimed to define community paramedics’ perceptions regarding their training needs to serve as CTI coaches who support the ED-to-home transition. Using detailed feedback from participating paramedics, we identified themes based on their perspectives and derived recommendations for refining the program to improve its contribution to community paramedicine.
METHODS
Study Design
We performed a qualitative evaluation of a community paramedicine training program created as part of a multi-center randomized controlled trial evaluating a community paramedic-delivered CTI to improve the ED-to-home transition of older adults. The study received approval by the University of Wisconsin-Madison Institutional Review Board. We followed all COnsolidated criteria for REporting Qualitative research (COREQ) criteria.
Study Setting and Subjects
We identified potential participants from a list of active community paramedics currently acting as CTI coaches in Madison, Wisconsin and Rochester, New York as part of the ongoing randomized controlled trial. We structured the recruitment in two ways to prevent coercion. First, the universities involved and the research teams did not employ or manage the paramedics, meaning non-participation could not affect their jobs. Second, we structured the research processes so that only the medical student researcher (HSL) knew who participated in this qualitative study. Specifically, the recruitment process consisted of the study team notifying the coaches of this qualitative study during a meeting that was part of the controlled trial evaluating the CTI. They were further told that a medical student researcher (HSL) who was unaffiliated with the EMS agencies that employed the paramedics and who did not participate in the larger study evaluating the community-paramedic delivered CTI would contact them via email to gauge interest. The student researcher only sent one email to each paramedic. For those willing to participate, the student researcher then obtained consent, scheduled the interview, and performed the interview. This process also allowed the paramedics to simply not respond to the query if they did not wish to participate in the study. To ensure that each paramedic’s participation remained confidential, all transcripts were deidentified by the student prior to being reviewed by the study team.
Care Transitions Intervention
The traditional hospital-to-home CTI consists of a four-week program uniquely focused on the transfer of self-management skills to patients discharged from the hospital. A coach provides one in-person visit in the hospital prior to discharge, one in-person home visit (approximately one hour), and up to three phone calls following discharge. During these encounters, the coach uses motivational interviewing to provide education, behavior modeling, and role playing. This coaching helps patients address the “Four Pillars” (core concerns) of the CTI: (1) taking ownership of a reliable medication management that fits into the patient’s routine, (2) performing timely follow-up with a physician, (3) maintaining awareness of “red flags” (warning signs) relevant to the patient’s medical history and knowing what to do if one appears, and (4) keeping a “personal health record” (PHR) that documents relevant features of the patient’s condition.
In adapting the CTI to the ED-to-home transition, we rejected as impractical an in-person coaching visit during each patient’s ED stay. This modification necessitated that the in-person home visit occur soon after ED discharge, ideally within 24-48 hours. This timing addresses the likelihood that patients need the greatest support in the first few days following discharge. We left intact all other aspects of the traditional CTI to retain the beneficial features that have made it successful. Providers did not deliver any other community paramedicine services, such as delivering vaccinations or screening for conditions, during the home visits.
Training Program
The study team, a multidisciplinary group with expertise in geriatrics, emergency medicine, and prehospital medicine, developed the community paramedicine training program under evaluation. The program consisted of a curriculum for training paramedics to serve as care transition coaches. Our panel identified five domains in which candidate coaches require proficiency and/or familiarity: (1) the CTI, (2) effective coaching, (3) geriatrics care, (4) the ED discharge process, and (5) community paramedicine (Table 1).
Table 1.
Training the Community Paramedic Coaches for the Modified Care Transitions Intervention.
| Training Domains | Resources |
|---|---|
| 1. Care Transitions Intervention (CTI) | Care Transitions Program® at the University of Colorado a. Website review: http://caretransitions.org b. Completion of the CTI® Web-based Introduction to Coach Training Unit, Sections 1-4 |
| 2. Effective Coaching | Motivational interviewing training and mentored coaching a. Class on motivational interviewing b. Coach shadowing, 1-2 home visits c. Mentored coaching, 1-2 visits |
| 3. Geriatrics Care | Readings on caring for older patients |
| Video podcasts on caring for older patients and dementia a. E.g.,https://www.mlrems.org/training/cme-vodcasts/ | |
| Geriatrician Shadowing | |
| 4. ED Discharge Process | Shadowing an ED physician and patient |
| Readings on failures of the process | |
| Review of patient discharge handouts | |
| 5. Community Paramedicine | Readings on the role of community paramedicine |
The Care Transitions Program, led by Dr. Eric Coleman who developed the CTI, provided the CTI training.17 It consisted of on-line modules which took approximately eight hours to complete, and then a one day training in Denver, Colorado. The panel expanded the traditional CTI training to include added support such as shadowing veteran coaches, participating in home-visit simulations, and receiving coach mentoring. To address the other domains, we identified a variety of training resources, including readings, video podcasts, in-person training, and shadowing experiences. Finally, the panel developed a continuing education module, with coaches participating in monthly teleconferences delivered by the national Care Transitions Program, as well as regular review sessions that discussed patients and challenges that coaches encountered at each study site.
Study Methods
To qualitatively evaluate the training program, we used semi-structured interviews to gather first-person accounts, allowing for the identification of themes not a priori identified by the research team. We iteratively revised the interview guide through testing on non-coach study team members. The interviews first queried subjects’ demographic background, past healthcare experience, and experience with the ED-to-home coaching program. We then probed for opinions about each domain of training and how well it prepared candidate coaches (Figure 1).
Figure 1.
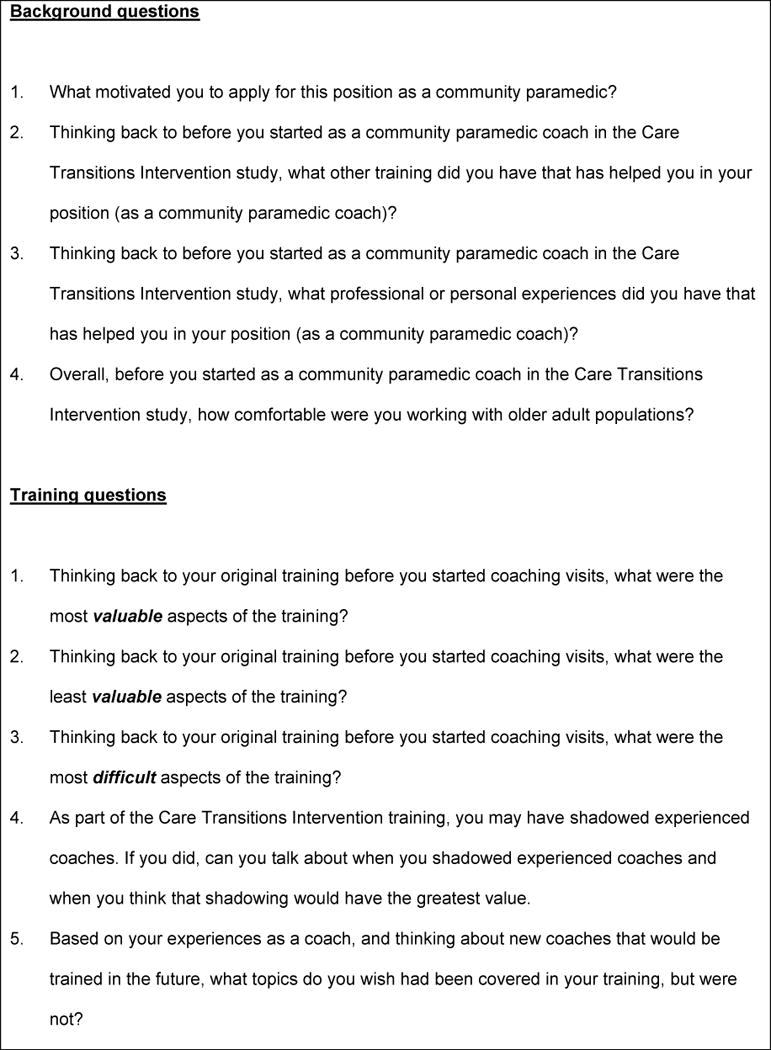
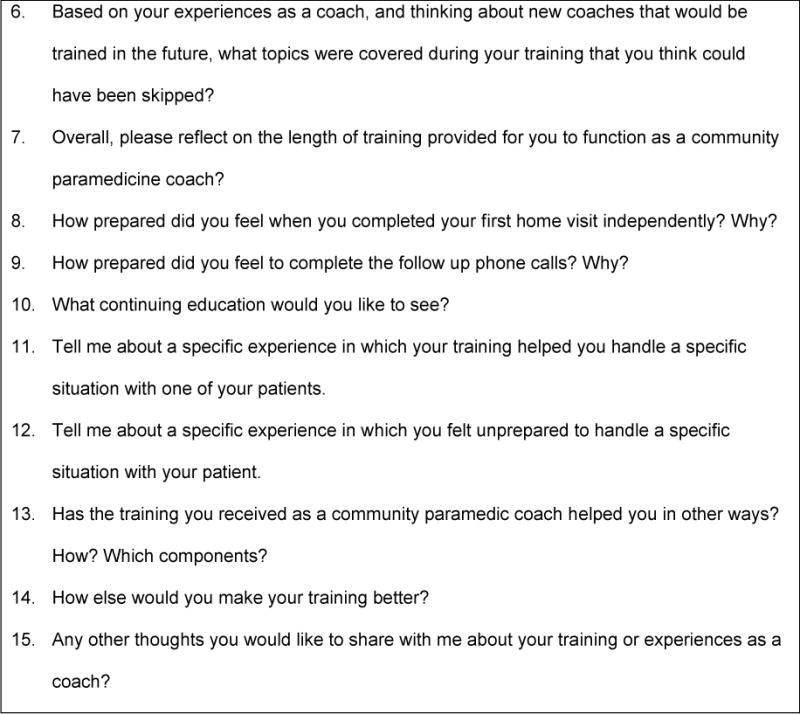
Interview guide (abridged).
Sixteen months after the primary study began, during May 2017, we began conducting the audio-recorded semi-structured interview with eight community paramedics from both cities. One study team member (HSL) completed all interviews. Since participants did not previously know him and he had not participated in the overall research program, his role as the interviewer minimized bias in questioning. He had completed a course in qualitative research and also had practiced interviewing study team members prior to starting the study. He completed all interviews in person (Madison paramedics) or over the phone (Rochester paramedics), audio-recording, transcribing, and deidentifying all interviews. We completed all interviews by July 2017.
Data Coding and Analysis
Three study team members (HSL, MMH, MNS) used directed content analysis to examine the interview transcripts and identify overarching themes relevant to training program evaluation.20 The community paramedic viewpoint on training has received little previous attention, and thus forms a topic lending itself to directed content analysis, a structured methodological approach that extends or validates existing knowledge.21 Prior to coding, we identified several potential codes of interest through consultation of relevant literature, the aims of the randomized controlled trial, and group discussion among study team members. We independently developed provisional codes and then discussed the codes as a group, minimizing individual researcher biases.22 Moreover, two investigators (HSL, MMH) had minimal familiarity with the larger study, contributing to coding reliability by limiting the extent to which pre-existing knowledge could influence our analyses. We then discussed, revised, and finalized codes to achieve consensus. We used Dedoose (SocioCultural Research Consultants, LLC, Manhattan Beach, CA) software to code the transcripts. Finally, we used the codes to identify overall themes relevant to program evaluation emerging from the interview data. We confirmed our interpretation of these themes by member checking, a process in which two subjects provided feedback on our identified themes.23
RESULTS
All 8 eligible community paramedics participated in interviews. Table 2 summarizes their demographic and professional information. Participants typically had extensive backgrounds in healthcare, primarily as EMS providers, but less experience with community paramedicine. All but one participant had logged considerable time as CTI coaches, and at the start of the interviews had cared for an average of 44 older adult patients (range = 4-85).
Table 2.
Participant Demographic Data (N=8).
| Variable | Value |
|---|---|
| Age, mean (Min, Max) | 43 (28, 65) |
| Female (percent) | 5 (62.5%) |
| Race, white (percent) | 8 (100%) |
| Ethnicity, non-Hispanic white (percent) | 8 (100%) |
| Years of EMS experience, mean (standard deviation) | 16 (7) |
| Years of paramedic experience, mean (standard deviation) | 13 (6) |
We identified four themes related to subjects’ perspectives on the community paramedic training they received (Tables 3 and 4):
Table 3.
Quotations illustrating Themes 1-2.
| Theme | # | Quote |
|---|---|---|
| Successful coaches | 1 | “…[S]eeing that the value of choosing the right people from the community paramedicine job, right? The more experienced… a little bit more insightful people that have more patience are better for this than some of our little more ‘type A’ personality, younger, hard-charging, ‘let’s fix this and get going’ type thing.” |
| 2 | “I just enjoy dealing with the elderly population, in general. I think their lives, they’re interesting to talk to, they have, you know, a different worldview than someone who is 20 or 30 years old.” | |
| 3 | “I think it’s [geriatrics readings] useful to, just to get a basic knowledge, and I’m going to say basic because that’s…how much I, you know, I still feel like there’s plenty to learn as far as…the difference between dementia and…delirium, different things like that.” | |
| 4 | “[I]t’s totally different than when I was on the med unit. You know, and the med unit I go in and I’m taking charge of the scene [clap] and, duh duh duh, and ‘you’re going to do this’ and ‘you’re doing this’, and you’re in this very different role…[N]ow when I go in, I would say 90% of the visits I go in with the idea of ‘I don’t want to be rushed…I want to feel like I can really listen…And I just kind of like nestle in, hear the story, and try to figure it out. I think I’m a much better listener when I’m in there…” | |
| Active learning | 5 | “I’m not a good book learner. I’m very much a visual hands-on kind of learner. And you know, we did a lot of readings and that was okay, but I learn best, a little bit more, by actual doing…I prefer the hands-on classroom style learning as opposed to just reading articles.” |
| 6 | “The weakness is again for me the format. Reading assignments at [my age]…like it’s hard, I’d rather have a dynamic speaker…I like teaching, and I like engagement…So I didn’t feel like articles really helped me understand it…” | |
| 7 | “I don’t remember [the geriatrics readings], sorry.” |
Table 4.
Quotations illustrating Themes 3-4.
| Theme | # | Quote |
|---|---|---|
| Training adjustments | 8 | “I think that Coleman [CTI training in Denver] was extremely valuable, even though it was a one day training and we kind of went over, but understanding those forms and role playing the whole afternoon and using those forms in a really controlled setting.” |
| 9 | “[A] lot of the patients are getting enrolled into the [study]…are actually very healthy. So, it’s not as, it’s not as cut and dry in terms of figuring out, and you know having the patients be able to kind of develop those goals and really be able to apply those goals to their care and stuff like that. So, you know, if anything I would say something that it would be nice to be added to that would be dealing with…those people that are actually healthy to a large extent…” | |
| 10 | “…I feel like mental health is an extremely important aspect [not covered]…And, even if it’s from depression to anxiety to straight up dementia…I find that that is a challenge, for sure.” | |
| Continuing education | 11 | “A lot of the conversation [in the national conference calls]…was around just specific patients that people were seeing and it was…I don’t know, it was a little, a little vague and not incredibly helpful…” |
| 12 | “The weaknesses [of the national conference calls] are that I just felt like it was more of a complain-o…I didn’t feel like I was learning technique and stuff, I didn’t feel like anything. I feel like it was a self-help group.” | |
| 13 | “It’s kind of like learning how to do IVs, right? If you teach me how to do IVs and then I don’t do them again for three years, I’m not going to be as proficient…if you’re going to continue this with the Coleman model what I would do is once a month you have training refresh boot camp. Where you spend two hours going over Coleman material on the website, having a conference call…and refreshing on the motivation interviewing stuff so those are kept fresh.” |
Theme 1: Paramedics with positive attitudes and willingness to acquire needed knowledge and skills will succeed
Participants emphasized that for a paramedic to succeed in the training program s/he must display a positive attitude and willingness to acquire the relevant knowledge and skills. First, they argued that the right kind of attitude is foundational. Coaches must have a positive mindset about working with older adults, and specifically must have a genuine appreciation of the CTI philosophy and how it may differ from traditional paramedicine values (Table 3, Quotes 1-2). Second, paramedics must acquire relevant knowledge pertaining to three areas in particular: geriatric care, the CTI, and ED discharge processes. Participants specified how particular aspects of the training that conveyed such knowledge were important (Table 3, Quote 3). Third, participants described the critical possession of relevant skills. These included the ability to make the frame shift away from paramedicine’s orientation to immediate action toward patient empowerment through active listening (Table 3, Quote 4).
Theme 2: Active rather than passive learning methods is preferred by paramedics
Participants placed great value on active learning techniques, and typically expressed less interest in more passive ones. Curriculum components involving a participatory or practical dimension – coaching simulations, mock interviews, geriatric physician shadowing, dynamic speakers – tended to receive the greatest praise (Table 3, Quote 5). By contrast, the more passive training components, particularly readings and videos, received less enthusiasm and even criticism (Table 3, Quote 6). When asked about passive modules, subjects often had trouble remembering their content or even participating in them, whereas this was much less common with active ones (Table 3, Quote 7).
Theme 3: Although quite valuable, the existing training could benefit from adjustments
Participants highly valued the training provided to them, as they felt it prepared them well for their role. The most highly valued components (in no particular order) included geriatrician shadowing; the CTI training in Denver, Colorado; the motivational interviewing training; and mock patient simulations (Table 4, Quote 8).
Criticism of the existing program primarily related to deficient or absent topics which participants thought had potential value. These included: 1) skills for coaching relatively healthy patients who may not have issues to discuss; 2) challenging topics such as mental health, dementia, and substance abuse; 3) and administrative requirements of the program (Table 4, Quotes 9-10).
Theme 4: Continuing education could better address coaches’ evolving needs
Participants had mixed feelings about continuing education. Generally, participants rated local case review meetings highly, serving the immediate need of feedback and benchmarking. Although the Care Transitions Program facilitated a similar discussion between programs, participants felt it was irrelevant to their issues because the calls focused on the hospital-to-home transitions (Table 4, Quotes 11-12). However, participants, though noting burdensome aspects of continuing education, did generally acknowledge the usefulness of refresher training in areas targeted to their local group’s needs – especially the CTI method, motivational interviewing, and coaching skills and techniques (Table 4, Quote 13).
DISCUSSION
Paramedics have tremendous potential to provide a range of community health interventions that may result in a reduction in need for ED and EMS services, but require proper preparation to effectively deliver those services.24 In this study, we evaluated a training program that enabled community paramedics to serve as coaches in an ED-to-home care transitions program. We learned from our participants that to effectively serve as coaches in the CTI Program, EMS leaders must select the right coaches and deliver training to augment the skills necessary for the program. While paramedics valued the specific training we provided, they felt it could be improved in certain focused areas.
Because traditional EMS courses do not generally include training related to most community health interventions and because the current state oversight regarding community paramedicine scope of practice varies, EMS medical directors must ensure sufficient training exists to ensure the paramedics’ and programs’ success.25 The participants in this study felt that participating paramedics must first have a positive attitude regarding community health activities, here specifically related to older adults and the CTI program. As demonstrated in studies by Lerner and Jaslow, the majority of EMS providers surveyed believe they should participate in disease and injury prevention, but a notable minority do not have interest in these types of programs.26,27 Second, community paramedics must acquire the necessary knowledge and skills to succeed as a CTI coach. Participants viewed the skill transition from acute care and rapid emergency action to community health and CTI approaches such as active listening and coaching as initially difficult, but achievable and ultimately essential to their success as coaches (Table 3, Quote 4). The need to provide paramedics added education to allow them to provide community health interventions has also been highlighted previously. Jaslow found that paramedics likely do not provide primary injury prevention education partially due to their lack of education on this topic. Additionally, we found that by providing the Geriatrics Education for EMS training, EMS providers in a rural New York community were more comfortable caring for elder abuse or neglect and evaluating for risk of falling, two topics with which they had previously lacked familiarity.26,28
Despite participants’ generally positive attitudes about their training, they pointed to three major ways it could be improved. First, they felt that active learning methods should replace passive ones such as reading articles or watching videos. In retrospect, this finding makes sense: modern educational research has generally found that active learning methods outperform passive ones.29 That coaches even had trouble remembering if they had completed the passive modules (e.g., community paramedicine readings) further reinforces the value of more active training methods (Table 3, Quote 7).
Second, several unmet perceived training needs should receive attention (Table 4, Quotes 9-10). For instance, participants sought more instruction on how to manage atypical CTI patients, especially those in relatively good health. The traditional CTI program has supported the hospital-to-home transition, preparing coaches to work with patients with multiple comorbidities and complex acute illnesses who required inpatient hospitalization. By contrast, community paramedics in our study work with healthier patients, as their enrollment required discharge from the ED. Adding training to address this issue therefore seems important.
Community paramedic subjects reported feeling unprepared to handle patients with dementia and with mental health problems, including loneliness, depression, and anxiety, during home visits. Older adults commonly experience these conditions, with one study finding 13% of transported older adults displaying cognitive impairment, and 14% exhibiting depression, making this a significant deficiency in the coach training.30 A related concern pertained to the lack of training in substance abuse, specifically recognizing signs and symptoms of addiction and how to discuss potentially addictive medications (e.g., opioids) during the home visit. Coaches may require such training to accurately perceive warning signs in patient behavior indicative of mental health crisis, suicide risk, or addiction, all common among older adults and underdiagnosed.
Third, any new program will generate unforeseen problems for its practitioners, and continuing education represents an effective means for addressing these. Indeed, our participants repeatedly underlined its importance. However, as with preferred learning styles, they value continuing education characterized by concreteness, specificity, and direct applicability to their local activities and problems. Such attitudes toward continuing education are likely not specific to this program, since a recent systematic literature review by Gent found that paramedics need much more continuing education, and especially more structured training.31 A community paramedicine-based CTI program may therefore require a combination of ongoing local education with periodic regional or national events that renew experienced coaches’ connection to the overall CTI methodology.
Study Limitations
This study has three important limitations that future research should address. First, our examination of community paramedics’ assessments of the CTI training relied on a small sample of participants who may not reflect all paramedics in the two participating EMS agencies. In qualitative studies, a participant sample of eight does not necessarily present problems, especially given the saturation of themes we observed. However, the observations and themes may not achieve generalizability for another reason: since the paramedics requested to participate in the evaluation of the CTI program, they likely differ from those who did not volunteer. Secondly, the participating paramedics displayed a wide range in experience (4-85 patients). Although not all paramedics had extensive experience, this heterogeneity potentially strengthens the study, as it reflects potential real-world circumstances. Finally, this study evaluated a single, unique community paramedicine training program that leverages a validated hospital-to-home CTI program. As community paramedicine programs develop and engage a myriad of methods to improve the health of their community, our results – though potentially generalizable to some programs – may nevertheless not find applicability to every community paramedic program, or the intervention(s) used by that program.
CONCLUSION
Paramedics represent a potentially valuable and largely untapped resource for supporting ED-to-home care transitions, such as through the CTI. Participating community paramedics identified ways in which to improve future training and enhance education to support their roles as coaches. Providing training in the most effective manner for the students and targeting content to student needs will lead to effective implementation of community paramedic-delivered CTI programs. These findings may apply to training for similar community paramedicine roles, but additional research must confirm this possibility.
Acknowledgments
Research reported in this publication received support from the University of Wisconsin-Madison School of Medicine and Public Health Shapiro Research Program, and the National Institute On Aging of the National Institutes of Health under Award Numbers R01AG050504 and K24AG054560. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Albert M, Ashman J. Emergency department visits by persons aged 65 and over: United States 2009–2010. Natl Cent Health Stat. 2013 [PubMed] [Google Scholar]
- 2.Duong HV, Herrera LN, Moore JX, Donnelly J, Jacobson KE, Carlson JN, Mann NC, Wang HE. National Characteristics of Emergency Medical Services Responses for Older Adults in the United States. Prehospital Emergency Care. 2017 doi: 10.1080/10903127.2017.1347223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hwang U, Shah MN, Han JH, Carpenter CR, Siu AL, Adams JG. Transforming emergency care for older adults. Health Aff Proj Hope. 2013;32(12):2116–2121. doi: 10.1377/hlthaff.2013.0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCusker J, Cardin S, Bellavance F, Belzile E. Return to the emergency department among elders: patterns and predictors. Acad Emerg Med. 2000;7(3):249–259. doi: 10.1111/j.1553-2712.2000.tb01070.x. [DOI] [PubMed] [Google Scholar]
- 5.Caplan GA, Brown A, Croker WD, Doolan J. Risk of admission within 4 weeks of discharge of elderly patients from the emergency department–the DEED study. Discharge of elderly from emergency department. Age Ageing. 1998;27(6):697–702. doi: 10.1093/ageing/27.6.697. [DOI] [PubMed] [Google Scholar]
- 6.Friedmann PD, Jin L, Karrison TG, Hayley DC, Mulliken R, Walter J, Chin MH. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med. 2001;19(2):125–129. doi: 10.1053/ajem.2001.21321. [DOI] [PubMed] [Google Scholar]
- 7.Pines JM, Mullins PM, Cooper JK, Feng LB, Roth KE. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc. 2013;61(1):12–17. doi: 10.1111/jgs.12072. [DOI] [PubMed] [Google Scholar]
- 8.Lowenstein SR, Crescenzi CA, Kern DC, Steel K. Care of the elderly in the emergency department. Ann Emerg Med. 1986;15(5):528–535. doi: 10.1016/s0196-0644(86)80987-8. [DOI] [PubMed] [Google Scholar]
- 9.Hastings SN, Oddone EZ, Fillenbaum G, Sloane RJ, Schmader KE. Frequency and predictors of adverse health outcomes in older Medicare beneficiaries discharged from the emergency department. Med Care. 2008;46(8):771–777. doi: 10.1097/MLR.0b013e3181791a2d. [DOI] [PubMed] [Google Scholar]
- 10.Hastings SN, Schmader KE, Sloane RJ, Weinberger M, Goldberg KC, Oddone EZ. Adverse health outcomes after discharge from the emergency department–incidence and risk factors in a veteran population. J Gen Intern Med. 2007;22(11):1527–1531. doi: 10.1007/s11606-007-0343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sellers C, Duckles J, Shah M, Christensen T. What makes for “successful” transitions from the emergency department to home and community among older adults? Int J Qual Methods. 2013;(12):815–816. [Google Scholar]
- 12.Shah MN, Caprio TV, Swanson P, Rajasekaran K, Ellison JH, Smith K, Frame P, Cypher P, Karuza J, Katz P. A novel emergency medical services-based program to identify and assist older adults in a rural community. J Am Geriatr Soc. 2010;58(11):2205–2211. doi: 10.1111/j.1532-5415.2010.03137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guttman A, Afilalo M, Guttman R, Colacone A, Robitaille C, Lang E, Rosenthal S. An emergency department-based nurse discharge coordinator for elder patients: does it make a difference? Acad Emerg Med. 2004;11(12):1318–1327. doi: 10.1197/j.aem.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Vashi A, Rhodes KV. “Sign right here and you’re good to go”: a content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2011;57(4):315–322. doi: 10.1016/j.annemergmed.2010.08.024. [DOI] [PubMed] [Google Scholar]
- 15.Coleman EA, Berenson R. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141:533–6. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 16.Coleman EA, Smith JD, Frank JC, Min S-J, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52(11):1817–1825. doi: 10.1111/j.1532-5415.2004.52504.x. [DOI] [PubMed] [Google Scholar]
- 17.Coleman EA, Parry C, Chalmers S, Min S-J. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 18.Juraschek SP, Zhang X, Ranganathan VK, Lin VW. Unites States Registered Nurse Workforce Report Card and Shortage Forecast. American Journal of Medical Quality. 2012;27(3):241–49. doi: 10.1177/1062860611416634. [DOI] [PubMed] [Google Scholar]
- 19.Hoyle S, Swain AH, Fake P, Larsen PD. Introduction of an extended care paramedic model in New Zealand. Emerg Med Australas EMA. 2012;24(6):652–656. doi: 10.1111/j.1742-6723.2012.01608.x. [DOI] [PubMed] [Google Scholar]
- 20.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Health Sci. 2013;15(3):398–405. doi: 10.1111/nhs.12048. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 22.Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Educ Today. 1991;11(6):461–66. doi: 10.1016/0260-6917(91)90009-y. [DOI] [PubMed] [Google Scholar]
- 23.Lincoln YS, Guba EG. Naturalistic Inquiry. Sage; 1985. [Google Scholar]
- 24.Tavares W, Drennan I, Van Diepen K, Abanil M, Kedzierski N, Spearen C. Building capacity in healthcare by reexamining clinical services in paramedicine. Prehospital Emergency Care. 2017;21(5):652–661. doi: 10.1080/10903127.2017.1311391. [DOI] [PubMed] [Google Scholar]
- 25.Glenn M, Zoph O, Weidenaar K, Barraza L, Greco W, Jenkins K, Paode P, Fisher J. State regulation of community paramedicine programs, a national analysis. Prehospital emergency care. 2017 doi: 10.1080/10903127.2017.1371260. [DOI] [PubMed] [Google Scholar]
- 26.Jaslow D, Marsh R. Primary injury prevention in emergency medical services: Is education a part of emergency treatment? Acad Emerg Med. 1999;(6):465. [Google Scholar]
- 27.Lerner EB, Fernandez AR, Shah MN. Do EMS professionals think they should participate in disease prevention? Prehospital Emerg Care. 2009;13(1):64–70. doi: 10.1080/10903120802471915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shah MN, Rajasekaran K, Sheahan WD, Wimbus T, Karuza J. The effect of the Geraitrics Education for Emergency medical Services training program in a rural community. Journal of the American Geriatrics Society. 2008;56:1134–1139. doi: 10.1111/j.1532-5415.2008.01738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Niemi H. Active learning—a cultural change needed in teacher education and schools. Teaching and Teacher Education. 2002;18:763–80. [Google Scholar]
- 30.Shah MN, Jones CMC, Richardson TM, Conwell Y, Katz P, Schneider SM. Prevalence of depression and cognitive impairment in older adult EMS patients. Prehospital Emergency Care. 2011;15(1):4–11. doi: 10.3109/10903127.2010.514093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gent P. Continuing professional development for paramedics: A systematic literature review. Australasian Journal of Paramedicine. 2016;13(4):1–9. [Google Scholar]


