Abstract
The term tension pneumocephalus (TP) means raised intracranial pressure due to air in the cranial cavity. This presentation is a rare case report and review on TP. Decompressing this raising intracranial pressure is a surgical emergency. Therefore, this presentation emphasises the importance of timely identification and management of TP in saving life. In this case, the acute signs of raising intracranial pressure were identified and promptly addressed surgically along with the maxillofacial injury management. This restored the deteriorating neurological status as well as his facial form and function. The etiological factors, pathophysiology and various treatment options are reviewed.
Keywords: Tension pneumocephalus, Intracranial pressure, Mt Fuji, Naso-orbito-ethmoidal, Glasgow Coma Scale
Introduction
The term tension pneumocephalus (TP) means raised intracranial pressure due to air in the cranial cavity. This term was proposed by Wolff in 1914 [1]. Ishiwata et al. described that the radiological image produced by TP is similar to the famous Fuji Volcano in Japan due to the separation of both the frontal lobes caused by subdural air collection [2, 3]. Tension pneumocephalus (TP) is a rare life-threatening complication arising mainly due to craniofacial trauma. Rapid deterioration of neurological parameters and Glasgow Coma Scale (GCS) are alarming signs of TP. It is a neurological emergency, mandating surgical intervention. We present a rare case of TP due to cranio-maxillofacial injury involving frontal and naso-orbito-ethmoidal complex. This case presentation highlights how an individual on sustaining blunt head injury can deteriorate rapidly on his neurological parameters and turn into a violent case of TP and how timely surgical intervention can restore his neurological status. The etiological factors, pathophysiology and various treatment options are discussed.
Case Report
A 32-year-old male sustained injury to the cranio-maxillofacial complex, due to motorcycle crash. He was attended by a medical officer at a peripheral healthcare facility and evacuated to our tertiary care centre for further investigations and management. Clinical examination revealed a well-built individual who was disoriented and confused. The GCS was E3V4M4. There was gross distortion of the nasal complex and deviation of nasal bridge to the right side (Fig. 1). Bilateral black eye and a cut and lacerated wound of left supraorbital area were noticed. Nasal bleed was controlled by nasal packing. There was no evidence of cerebrospinal fluid (CSF) rhinorrhea as the patient was in supine position. No other injury was found. Maxilla, mandible, temporomandibular joint (TMJ) and dental occlusion were normal. Vital parameters were within normal limit. The patient was clinically diagnosed as a case of closed head injury with fracture naso-orbito-ethmoidal (NOE) complex. Computed tomography (CT) 3D reformatted image revealed comminuted fracture of NOE region extending to right zygomatic-maxillary buttress and frontal bone involving the frontal sinus (Fig. 2). Pneumocephalus was restricted to right frontal lobe. The case was jointly discussed with neurosurgeon, maxillofacial surgeon and anaesthetist, and decision was taken to observe the patient for effect of head injury before taking up for definitive management of fracture. Patient was kept on nil-per-oral (NPO) with parenteral dose of dilantin sodium (15 mg/kg) and mannitol (1.5 g/kg) intravenous infusion.
Fig. 1.

Distortion of the nasal complex
Fig. 2.

Three-dimensional reformatted image showing comminuted NOE fracture
After 24 h, the condition of the patient started deteriorating. The GCS was E2V2M3. The patient was agitated, restless and was restrained to the bed. Suspecting the meningitis, empirical antibiotics were started. A repeat CT scan was ordered. Axial scan revealed bilateral pneumocephalus with Mt Fuji sign (Fig. 3). A diagnosis of tension pneumocephalus was done. The patent was taken up for emergency craniotomy and fixation of fractures through bi-coronal approach under general anaesthesia. Subdural air was released through burr hole one on each side of midline. The fractured anterior wall of the frontal sinus was removed and preserved. Frontal sinus was curetted. Fronto-nasal duct was identified and obturated. The posterior wall was debrided, and pedicled pericranial flap was placed. The sinus was packed with betadine-soaked gel foam. The preserved anterior wall was repositioned and fixed using titanium mini-plate and screws (Fig. 4). Vacuum drain was placed and wound sutured. Nasal fracture reduced and stabilised with modified nasal splint secured by transnasal wiring. Injectable antibiotics were continued for seven days as per the institutional protocol. Vacuum drain was removed on third postoperative day and sutures on seventh day. The postoperative healing was uneventful, and the CT scan showed resolving pneumocephalus (Fig. 5). The nasal splint was removed after two weeks. During 6-month follow-up the patient recovered completely without any neurological disability (Fig. 6).
Fig. 3.

Axial scan showing Mt Fuji sign
Fig. 4.
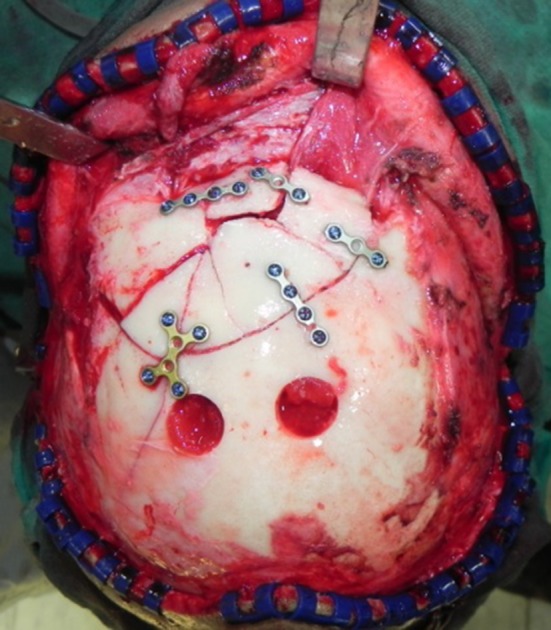
Bilateral burr hole and fracture fixation
Fig. 5.
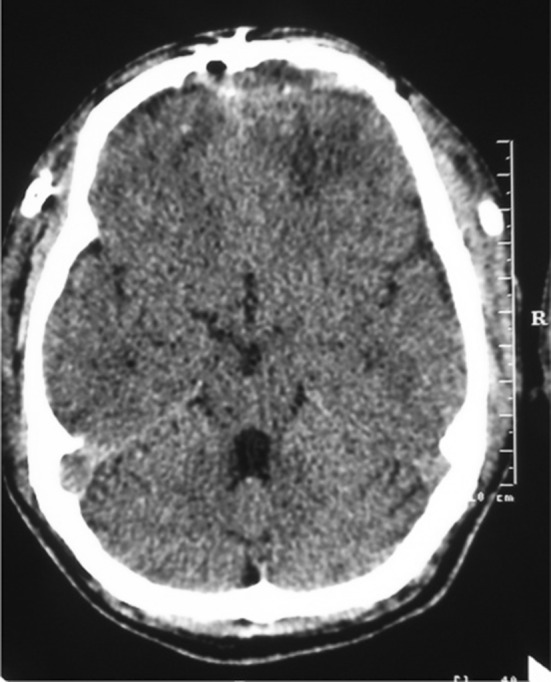
Axial scan showing resolving pneumocephalus
Fig. 6.

Follow-up frontal profile
Discussion
Pneumocephalus is defined as the presence of air in the cranial vault. Pneumocephalus develops due to a cranial or facial fracture through which air enters the intracranial cavity [4]. This air exerts a mass or pressure effect on the brain, leading to brain herniation [5]. It has been proposed that the volume of air as little 65 mL is sufficient enough to produce tension pneumocephalus [6]. Air in the cranial cavity means, communication with the exterior or with the paranasal sinus. The most common cause for the communication is trauma (74%) [7]. Other causes include surgery, infection or tumour. Congenital cranial bony defects, hydrocephalus, encephalocele, chronic otitis media are other common causes [8–10]. Head position during cranial surgery, duration of surgery, nitrous oxide (N2O) anaesthesia, intraoperative osmotherapy, hyperventilation, spinal anaesthesia, barotrauma, continuous CSF drainage via lumbar drain, epidural anaesthesia are suggested as surgical causes [11–13]. TP can also be secondary to infection from gas-forming organisms [14]. In our case, it is primarily the trauma that caused the leakage of air into the anterior cranial fossa. The pressure effect of this leaked air, compromising the cranial space, caused rapid deterioration of the neurological status.
Head injury causes TP possibly by three mechanisms as discussed in the literature: firstly, the trauma in anterior cranial base leads to cerebrospinal fluid leak, causing negative intracranial pressure resulting to inflow of air. This is described as “inverted bottle effect”. Secondly, the dural tear due to trauma acts as a one-way valve that allows air in but not out of cranial space. Thirdly, the cranial base fracture is responsible for air entrapment when subjected to positive pressure airway ventilation [15–18]. In our case, the probable cause of TP was dural tear, communicating the frontal sinus with the anterior cranial space. As the time progressed, the air volume kept increasing due to negative pressure and one-way valve effects. This deteriorated his neurological status because of increasing intracranial pressure. Persistent headache and CSF leak are the most persistent feature as referred in the literature [19, 20]. There are two pathognomonic signs of TP. One is rapid change in the level of consciousness with the increase in air flowing into the cranial cavity [18]. Secondly, a splashing sound heard by the patient on postural change. This is called as bruit hydroaérique (“succession splash”) [21, 22]. Other features include confusion, hemiparesis [4], mental changes, loss of consciousness, seizure and abducent nerve palsy [23]. In our case, rapidly deteriorating GCS and patient becoming agitative in a period of 24 h were the two evident features. CSF rhinorrhea was not evident clinically due to supine position and presence of nasal pack. The confirmatory diagnosis was made on the basis of CT image, depicting the entrapped air in anterior cranial region. The onset of TP may be acute which occurs within 72 h or delayed after 72 h. Our case had acute onset of TP within 48 h of trauma.
Majority of TP cases resolve with time. They are managed conservatively and monitored for neurological changes following trauma or exposure to other etiological factors. Management with oxygen is recently advocated. By increasing the partial pressure of oxygen, the intracranial nitrogen and other composite gases are displaced and drawn into the blood to get expired out (nitrogen washout effect) [23, 24]. Identifying the dural tear and repairing the site will cease further entrapment of air. Controlled decompression using a closed water-seal drainage system has also been described [25]. Other treatment options include burr hole aspiration of air, needle aspiration, craniotomy and ventriculostomy placement [19]. In our case, burr hole aspiration of air was done to manage TP. Fronto-naso-orbito-ethmoidal fracture and nasal fracture were also addressed.
Conclusion
Tension pneumocephalus is a surgical emergency. Prompt identification of the changing neurological status of the patient and decompressing the raising intracranial pressure through appropriate approach are mandatory to save life. In this case, the acute signs of raising intracranial pressure were identified and timely addressed surgically along with the maxillofacial injury management. This restored the neurological status of the individual as well as his facial form and function.
References
- 1.Wolff E. Air accumulation in the right lateral ventricle of the brain (Pneumocephalus. Münch Med Wochenschr. 1914;61:899–902. [Google Scholar]
- 2.Ishiwata Y, Fujitsu K, Sekino T, Fujino H, Kubokura T, Tsubone K, Kuwabara T. Subdural tension pneumocephalus following surgery for chronic subdural hematoma. J Neurosurg. 1988;68:58–61. doi: 10.3171/jns.1988.68.1.0058. [DOI] [PubMed] [Google Scholar]
- 3.Michel SJ. The Mount Fuji Sign. Radiology. 2004;232:449–450. doi: 10.1148/radiol.2322021556. [DOI] [PubMed] [Google Scholar]
- 4.Bjerrum S, Rosendal F. A rare case of tension pneumocephalus after head trauma. Int J Surg Case Rep. 2015;6:300–302. doi: 10.1016/j.ijscr.2014.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Por YC, Barcelo CR, Salyer KE. Extradural tension pneumocephalus after posterior cranial vault remodelling for ventriculo-peritoneal shunt-induced craniosynostosis. J Craniofac Surg. 2005;16:504–508. doi: 10.1097/01.scs.0000171970.14185.38. [DOI] [PubMed] [Google Scholar]
- 6.Monajati A, Cotanch WW. Subdural tension pneumocephalus following surgery. J Comput Assist Tomogr. 1982;6:902–906. doi: 10.1097/00004728-198210000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Markham JW. The clinical features of pneumocephalus based on survey of 284 cases with report of additional 11 cases. Acta Neurochir. 1967;60:1–78. doi: 10.1007/BF01401900. [DOI] [PubMed] [Google Scholar]
- 8.Cartwright MJ, Eisenberg MB. Tension pneumocephalus associated with rupture of a middle fossa encephalocele. J Neurosurg. 1992;76:292–295. doi: 10.3171/jns.1992.76.2.0292. [DOI] [PubMed] [Google Scholar]
- 9.Aoyama I, Kondo A, Nin K, Shimotake K. Pneumocephalus associated with benign brain tumor: report of two cases. Surg Neurol. 1991;36:32–36. doi: 10.1016/0090-3019(91)90129-W. [DOI] [PubMed] [Google Scholar]
- 10.Haran RP, Chandy MJ. Symptomatic pneumocephalus after transsphenoidal surgery. Surg Neurol. 1997;48:575–578. doi: 10.1016/S0090-3019(96)00420-X. [DOI] [PubMed] [Google Scholar]
- 11.Klopfenstein CE, Forster A, Suter PM. Pneumocephalus. A complication of continuous positive airway pressure after trauma. Chest. 1980;78:656–657. doi: 10.1378/chest.78.4.656. [DOI] [PubMed] [Google Scholar]
- 12.McIntosh BC, Strugar J, Narayan D. Traumatic frontal bone fracture resulting in intracerebral pneumocephalus. J Craniofac Surg. 2005;16:461–463. doi: 10.1097/01.SCS.0000157249.31826.B7. [DOI] [PubMed] [Google Scholar]
- 13.Zasler ND. Posttraumatic tension pneumocephalus. J Head Trauma Rehabil. 1999;14:81–84. doi: 10.1097/00001199-199902000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Klein MA, Kelly JK, Jacobs IG. Diffuse pneumocephalus from Clostridium perfringens meningitis: CT findings. AJNR. 1989;10:447. [PMC free article] [PubMed] [Google Scholar]
- 15.Bunc G, Roskar Z, Vorsic M. Pneumocephalus secondary to a neck stab wound without neurologic injury in a 13-year-old girl. Pediatr Neurosurg. 2001;34:239–241. doi: 10.1159/000056029. [DOI] [PubMed] [Google Scholar]
- 16.Kulkarni MS, Baum CR. Traumatic pneumocephalus. Clin Pediatr Emerg Med. 1999;1:70–73. doi: 10.1016/S1522-8401(99)90010-1. [DOI] [Google Scholar]
- 17.Satapathy GC, Dash HH. Tension pneumocephalus after neurosurgery in the supine position. Br J Anaesth. 2000;84:115–117. doi: 10.1093/oxfordjournals.bja.a013368. [DOI] [PubMed] [Google Scholar]
- 18.Cobba ARM, Caroline K, Timothy LW. Pneumocephalus—late cause of neurological deterioration after craniomaxillofacial trauma. Br J Oral Maxillofac Surg. 2013;51:e188–e189. doi: 10.1016/j.bjoms.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 19.Pillai P, Sharma R, Larami M, et al. Traumatic tension pneumocephalus: two cases and comprehensive review of literature. Opus 12 Sci. 2010;4(1):6–11. doi: 10.4103/IJCIIS.IJCIIS_8_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien) 1967;16:1–78. doi: 10.1007/BF01401900. [DOI] [PubMed] [Google Scholar]
- 21.Vitali AM, le Roux AA. Tension pneumocephalus as a complication of intracranial pressure monitoring: a case report. Ind J Neurotrauma. 2007;4:115–118. doi: 10.1016/S0973-0508(07)80025-6. [DOI] [Google Scholar]
- 22.Lin MB, Cheah FK, Ng SE, Yeo TT. Tension pneumocephalus and pneumorachis secondary to subarachnoid pleural fistula. Br J Radiol. 2000;73:325–327. doi: 10.1259/bjr.73.867.10817052. [DOI] [PubMed] [Google Scholar]
- 23.Schirmer CM, Heilman CB, Bhardwaj A. Pneumocephalus: case illustrations and review. Neurocrit Care. 2010;13(1):152–158. doi: 10.1007/s12028-010-9363-0. [DOI] [PubMed] [Google Scholar]
- 24.Gore PA, Maan H, Chang S, Pitt AM, Spetzler RF, Nakaji P. Normobaric Oxygen therapy strategies in the treatment of post craniotomy pneumo-cephalus. J Neurosurg. 2008;108:926–929. doi: 10.3171/JNS/2008/108/5/0926. [DOI] [PubMed] [Google Scholar]
- 25.Arbit E, Shah J, Bedford R, Carlon G. Tension pneumocephalus: treatment with controlled decompression via a closed water-seal drainage system. Case report. J Neurosurg. 1991;74:139–142. doi: 10.3171/jns.1991.74.1.0139. [DOI] [PubMed] [Google Scholar]


