Key Clinical Message
We report the first case of a patient in whom an implantable cardioverter‐defibrillator (ICD) endowed with HeartLogic, a novel algorithm for heart failure (HF) monitoring, was implanted in clinical practice. The good temporal association between HeartLogic index threshold crossings and HF hospitalizations confirms the high sensitivity in detecting gradual worsening of HF.
Keywords: decompensation, heart failure, prediction, remote monitoring
1. INTRODUCTION
In the Multisensor Chronic Evaluation in Ambulatory Heart Failure Patients (MultiSENSE) study,1 a novel algorithm for heart failure (HF) monitoring was established. The HeartLogic (Boston Scientific, St. Paul, Minnesota) index combines data from multiple implantable cardioverter‐defibrillator (ICD)‐based sensors and has proved to be a sensitive and timely predictor of impending HF decompensation. We report the first case of a patient in whom an ICD endowed with HeartLogic was implanted in clinical practice. We report postimplantation data collected from sensors, the combined index, and their association with clinical events during follow‐up.
2. CASE REPORT
On 12 July 2017, a 76‐year‐old man with nonischemic‐dilated cardiomyopathy, 17% ejection fraction, left bundle branch block, and permanent atrial fibrillation was referred to our department, where he underwent implantation of a biventricular ICD for the primary prevention of sudden cardiac death and the delivery of cardiac resynchronization therapy (CRT). The device (model Vigilant, Boston Scientific) and the pacing leads were successfully implanted by means of standard techniques, and the postoperative course was uneventful. On August 7th, the patient was admitted to the hospital for worsening HF; after 5 days, he was discharged in good clinical condition. As rapid ventricular conduction of atrial fibrillation compromised CRT delivery, atrioventricular node modulation was attempted on August 29th. Owing to the recurrence of signs and symptoms of worsening HF, the patient was hospitalized from October 20th to 23rd. After discharge, the patient continued to report fatigue, orthopnea, and dyspnea. Despite multiple drug treatment adjustments made in an outpatient regimen, the patient was hospitalized again on December 11th. Recovery of fast atrioventricular conduction was diagnosed and the percentage of ventricular pacing was reduced. In December 2017, the HeartLogic feature was made available on the LATITUDE (Boston Scientific) remote monitoring platform. Thus, the patient received a communicator for remote monitoring of his implanted device and was instructed on how to use it. Correct setup and system initiation were verified. On the first remote data review, the full report of automatic diagnostics was available (Figure 1), which allowed us to assess the association between sensor data collected since implantation and the clinical events that had occurred. The HeartLogic algorithm combines data from multiple sensors: accelerometer‐based first and third heart sounds, intrathoracic impedance, respiration rate, the ratio of respiration rate to tidal volume, heart rate, and patient activity. The trends are combined into a composite index, which is updated daily. Owing to initialization, the HeartLogic index is not available until 30 days after data collection begins. An alert is issued when the index crosses a programmable threshold (nominal value 16). When the index enters into an alert state (gray area in Figure 1), the threshold is set automatically to a recovery value, which is less than the programmed threshold, to ensure full normalization of values before exiting the alert state.
Figure 1.
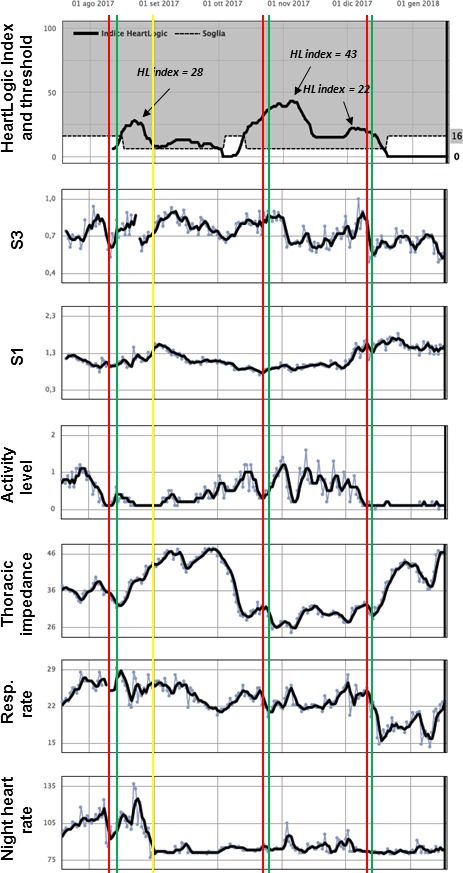
Report of automatic diagnostics available for review through the LATITUDE remote monitoring platform. Red bars: HF admissions; Green bars: Hospital discharge; Yellow bar: Date of the atrioventricular node modulation attempt
In the present case, the retrospective, and consequently blinded, analysis of HeartLogic index data revealed an association between the occurrence of HF events and the presence of threshold crossings and peaking index values. Specifically, the HeartLogic index crossed the threshold at the time of the first hospitalization and 1 week before the second. Moreover, although the index was already above the recovery threshold, it rose further at the time of the worsening of conditions that led to the last admission in December. Analysis of single sensor data showed an increase in third heart sound amplitude before all HF events, together with high values of respiratory rate and, for the first and third HF event, progressively decreasing activity levels. A marked decrease in thoracic impedance seemed to precede only the second HF event.
3. DISCUSSION
In the present report, we describe the first case of HeartLogic utilization in clinical practice. The good temporal association between HeartLogic index threshold crossings and HF hospitalizations seems to confirm the high sensitivity in detecting gradual worsening of HF demonstrated in the validation phase of the MultiSENSE study.1 The algorithm displayed sensitivity of 70%, with a median alert window of 34 days before the HF events and an unexplained alert rate of 1.47 per patient‐year at the nominal threshold.
In our example, the HeartLogic index increased above 16 in advance of the second and third hospital admissions, while in the case of the first admission it reached the threshold value when the patient was already in hospital. This can be ascribed to the postimplantation initialization phase, which expired only when the patient had been admitted to the hospital. Once active, the index increased and reached the alert state. Interestingly, a decrease in thoracic impedance, that is a sign of fluid overload, was seen to precede only one HF event. This result seems to confirm the observed low sensitivity of impedance‐derived fluid indices in the early period after implantation.2 Indeed, during that period, many patients are not clinically stable and there is a risk of incorrectly setting a reference impedance at the time of hypervolemia.2 In addition, a concurrent increase in thoracic impedance has been shown to result from postimplantation pocket healing and CRT‐induced ventricular volume changes,3 and this makes diagnostic systems based only on impedance measurement less sensitive to possible pulmonary fluid accumulation.
The sensitivity of the HeartLogic index, as well as the early warning system, can be adjusted by adequately setting the threshold value, which is set, by default, to 16. It is interesting that, during the periods between the HF events, the index did not fully recover and the alert state persisted. This is consistent with the difficulty of stabilizing the patient's condition (eg atrioventricular node modulation, drug treatment adjustments).
Among the sensed parameters that contribute to the calculation of the HeartLogic index, accelerometer‐based heart sounds seemed to correlate well with HF status. Specifically, the third heart sound is detected in order to provide an objective measure of elevated filling pressure, while the first heart sound is taken as a surrogate for left ventricular contractility, as it has been shown to correlate with the maximum pressure derivative.4 In agreement with previous studies,5 we also observed higher values of respiratory rate at the time of HF events. Moreover, the continuous measurement of resting heart rate, in addition to its contribution to HeartLogic index calculation, allowed us to detect the recovery of fast atrioventricular conduction, therefore suggesting the need to implement new solutions in order to control the rate and ensure biventricular pacing delivery.
This first description of remote monitoring of an HF patient by means of HeartLogic seems to confirm the capability of the algorithm to detect gradual worsening of HF. Single sensor data may, however, provide discordant information, and this highlights the importance of the automatic simultaneous analysis of multiple data.
AUTHORSHIP
LS, VS, and KM: wrote the paper. ML and ND: provided critical feedback. GM, MC, and SV: aided in interpreting device data and in reporting algorithm details. FA: supervised the work. All authors discussed the results and commented on the manuscript.
CONFLICT OF INTEREST
G. Mangone, M. Campari, S. Valsecchi are employees of Boston Scientific. The other authors report no conflicts.
Santini L, Mahfouz K, Schirripa V, et al. Preliminary experience with a novel Multisensor algorithm for heart failure monitoring: The HeartLogic index. Clin Case Rep. 2018;6:1317−1320. https://doi.org/10.1002/ccr3.1573
REFERENCES
- 1. Boehmer JP, Hariharan R, Devecchi FG, et al. A Multisensor algorithm predicts heart failure events in patients with implanted devices: results from the MultiSENSE study. JACC Heart Fail. 2017;5:216‐225. [DOI] [PubMed] [Google Scholar]
- 2. Conraads VM, Tavazzi L, Santini M, et al. Sensitivity and positive predictive value of implantable intrathoracic impedance monitoring as a predictor of heart failure hospitalizations: the SENSE‐HF trial. Eur Heart J. 2011;32:2266‐2273. [DOI] [PubMed] [Google Scholar]
- 3. Maines M, Landolina M, Lunati M, et al. Intrathoracic and ventricular impedances are associated with changes in ventricular volume in patients receiving defibrillators for CRT. Pacing Clin Electrophysiol. 2010;33:64‐73. [DOI] [PubMed] [Google Scholar]
- 4. Thakur PH, An Q, Swanson L, Zhang Y, Gardner RS. Haemodynamic monitoring of cardiac status using heart sounds from an implanted cardiac device. ESC Heart Fail. 2017;4:605‐613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Forleo GB, Santini L, Campoli M, et al. Long‐term monitoring of respiratory rate in patients with heart failure: the Multiparametric Heart Failure Evaluation in Implantable Cardioverter‐Defibrillator Patients (MULTITUDE‐HF) study. J Interv Card Electrophysiol. 2015;43:135‐144. [DOI] [PubMed] [Google Scholar]


