Abstract
Aim
Mechanical assist devices are sometimes needed during resuscitation efforts of patients with prolonged cardiac arrest. Two such devices, the AutoPulse and the LUCAS, have different mechanisms of action. We propose that the effectiveness of mechanical assist devices is somewhat dependent on the configuration and compliance of the patient's chest wall.
Methods
A previous study of patients with out‐of‐hospital cardiac arrest in Arizona reported that survivors were younger and many were observed to have narrow anterior–posterior chest diameters. These observations suggest that the predominant mechanism of blood flow during cardiopulmonary resuscitation of individuals with primary cardiac arrest is influenced by the patient's anterior–posterior chest diameter and compliance. It is proposed that in older individuals with an increased anterior–posterior chest diameter and decreased chest compliance that the AutoPulse, which works by increasing intrathoracic pressures, may be more effective. In contrast, the LUCAS device, which works predominately by compression of the sternum, is probably more effective in patients with narrower anterior–posterior diameters and a more compliant chest.
Results
These hypotheses need to be confirmed by researchers who not only have access to the lateral chest roentgenograms of patients with cardiac arrest, to determine their anterior–posterior chest diameter, but also to the type of mechanical device that was used during resuscitation efforts and their patient's survival. If the observations herein proposed are confirmed, hospitals and paramedics may ideally need to have one of each type of mechanical chest compression unit and select the one to use depending on the patient's age and anterior–posterior chest diameter.
Conclusions
The mechanism of blood flow in patients with cardiac arrest is predominantly secondary to cardiac compression in younger patients with narrow anterior chest diameters and predominately secondary to the thoracic pump mechanism in older patients with emphysema.
Keywords: Cardiac compression, device, resuscitation, straight back syndrome, thoracic pump
Introduction
It has been said that in many arguments or disagreements there is often some truth on each side. And so it is with the controversy over the mechanism of blood flow during chest compressions of patients with cardiac arrest.
Kouwenhoven, Jude and Knickerbocker, in their 1960 classic description of closed chest manual compressions for cardiac arrest secondary to ventricular fibrillation (VF), proposed that forceful rhythmic sternal compressions resulted in cardiac compressions, thereby generating forward blood flow and improving survival.1 In contrast, a quarter of a century later, Weisfeldt, Halperin and their colleagues, also at Johns Hopkins University School of Medicine (Baltimore, MD, USA), made hemodynamic observations in their resuscitation research laboratory leading them to propose that the mechanism of blood flow from chest compressions for primary cardiac arrest was not only the result of physical cardiac compression but also the result of a diffuse increase in intrathoracic pressure.2
Therefore, the initial mechanism of blood flow following promptly initiated chest compressions for primary cardiac arrest is controversial. There are now two major different postulated mechanisms of blood flow secondary to chest compressions in patients with cardiac arrest, “cardiac compression” and “thoracic pump.”
The “cardiac compression” theory of forward blood flow during chest compressions for cardiac arrest presumes that blood is squeezed from the heart into the arterial and pulmonary circulations, with closure of the mitral and tricuspid valves, preventing retrograde blood flow, and opening of the aortic and pulmonary valves in response to forward blood flow. Air is thought to move freely in and out of the lungs, so that the intrathoracic pressures do not significantly rise and the pulmonary circulation is not adversely affected by chest compressions. With the relaxation of chest compression, the heart fills with blood and air passively returns to the lungs.
Discussion
About a quarter of a century ago, while the author was a visiting professor at the Mayo Clinic Medical School (Rochester, MN, USA), Dr. Higano presented a patient who had a cardiac arrest while undergoing trans‐esophageal echocardiography (TEE).3 Fortunately, they continued the TEE recording during the resuscitation efforts that showed with each chest compression there was compression of the ventricles, with closure of the mitral and tricuspid valves and opening of the aortic and pulmonic valves, and with each release of chest compression, the aortic and pulmonic valves closed and the mitral and tricuspid valves opened.3
This TEE in a man with recent onset VF arrest was consistent with resuscitation research findings in animals with induced VF arrest: that cardiac compression was the mechanism of blood flow during chest compressions for recent cardiac arrest (Fig. 1).
Figure 1.
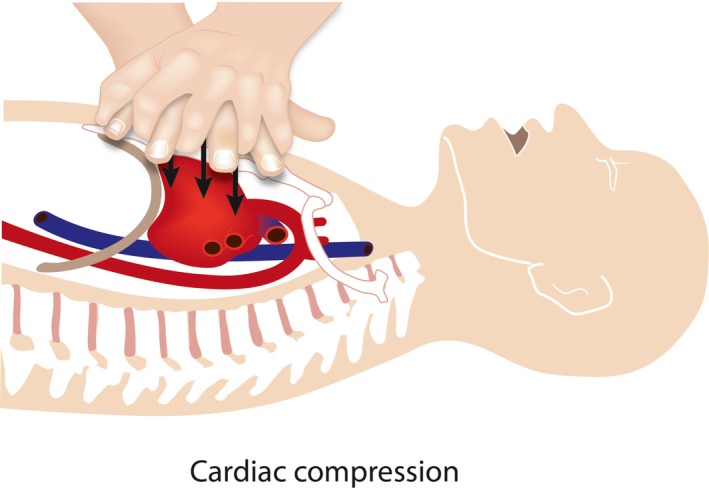
A drawing to depict a person with a narrow anterior–posterior chest diameter, a condition where chest compressions for cardiac arrest would most likely result in cardiac compression as the mechanism of blood flow during chest compressions.
Thoracic pump as the predominant mechanism of blood flow during chest compressions for cardiac arrest
Three decades after Kouwenhoven's initial reports, researchers also at the Johns Hopkins Medical School proposed an alternative theory of forward blood flow during resuscitation efforts for cardiac arrest.4 They proposed that chest compressions for primary cardiac arrest caused a rise in the intrathoracic pressure, which is transmitted to the intrathoracic vascular, producing forward blood flow.4 These academic resuscitation researchers proposed that with each chest compression the intrathoracic pressure rises because of the collapse of the airways; the thoracic pump theory. This theory presumes that the rise in the intrathoracic pressures results in collapse of the pulmonary airways, thereby reducing the movement of air out of the lungs and reducing the size of the intrathoracic structures, but not necessary equally.4 The collapse of venous structures at the thoracic inlet was postulated to prevent retrograde venous blood flow and with each relaxation of chest compressions, the intrathoracic pressure falls with return of venous blood.2, 4
These then new findings from the cardiopulmonary resuscitation (CPR) research group of Hopkins led to their initial recommendation of a manual chest compression rate of 60/min with a distinct pause at maximal chest compression.2 This concept was foreign to our resuscitation research group, as well as to resuscitation researchers in the Department of Surgery and Physiology at Duke University Medical Center (Durham, NC, USA), leading us to cooperate in a study to compare the survival of animals with VF arrest treated with manual chest compression rates of 60/min versus 120/min.5 “We found that when compared with the compression rate of 60/min, a compression rate of 120/min produced more successfully defibrillated animals; 12/13 of animals receiving compressions at 120/min versus 2/13 at a chest compression rate of 60/min P < 0.002”.5 “And more 24 h survivors (8/13) at the fast chest compression rate versus 2/13 at 60/min P < 0.03. All 24 h survivors were conscious and able to sit, stand, and drink normally”.5
Thoracic pump theory led to the development of the AutoPulse
Halperin and associates’ new concept of the mechanism of blood flow during chest compressions for cardiac arrest led them to develop the AutoPulse (Seattle, WA, USA), a mechanical device for CPR that not only compresses the chest but also increases the intrathoracic pressure, the so‐called thoracic pump theory.6 The commercially available AutoPulse has a backboard and a broad cloth band that is to be placed across the chest of the patient with cardiac arrest. According to the developers of the AutoPulse, it was designed to treat patients with cardiac arrest by periodically increasing the patient's intrathoracic pressure rather than physically compressing the heart.6 The programed rate of chest compressions by the AutoPulse is 80/min.6
Cardiac compression theory led to the development of mechanical chest compression devices
A currently popular commercially available mechanical chest compression device designed for cardiac compression during closed chest CPR is the Lund University Cardiac Assist System or “LUCAS” (http://www.lucascpr.com/en/lucas_cpr/lucas_cpr). Detailed information and references are available from Physio Control online. The LUCAS cardiac assist system is designed to assist paramedic and medical responders during prolonged resuscitation efforts and thereby help to improve outcomes of sudden cardiac arrest victims.
The LUCAS 2 (Jolife, Lund, Sweden) device has a piston mounted on a frame that can be placed above the patient's chest. The piston is driven up and down by a power source such as compressed air or oxygen, thereby functioning similar to manual chest compressions and releases. The LUCAS originally functioned not only as a device for mechanical chest compressions, but also for active chest decompression because of cup‐like pliable material on the piston designed to facilitate active decompression during the release phase of chest compression. Evidently, to get the device approved in the USA, the manufacturer of the LUCAS had to alter the device so that it did not have active decompression throughout the entire release phase of chest compression.
Randomized trials failed to show that mechanical devices were superior to manual chest compressions
There have been a number of randomized controlled trials of mechanical chest compression devices used during resuscitation of patients with out‐of‐hospital cardiac arrest (OHCA). There have also been a number of systematic reviews of studies evaluating the effectiveness of these devices. A 2015 systematic review by Gates and associates evaluated five trials, three reports that utilized the LUCAS or LUCAS‐2 and two that utilized the AutoPulse device.7 These investigators found no significant difference between these mechanical chest compression devices compared to manual chest compression, for survival to discharge or to survival with good neurological outcomes.7 They concluded that, “Existing studies do not suggest that mechanical chest compression devices are superior to manual chest compressions” when used during resuscitation of patients with OHCA.7
There are times when mechanical devices are necessary
It is clear that there are certain clinical situations during resuscitation of patients with cardiac arrest when a mechanical chest compression device may be desirable. These include prolonged resuscitation efforts due to persistent or recurrent cardiac arrest with inadequate number of personnel or during transportation with limited space such as in small helicopters, and in the hospital during cardiac catheterization.
Mechanism of blood flow during chest compressions for primary cardiac arrest is somewhat dependent on the patient's age and chest configuration
In all probability, the major determinants of the mechanism of blood flow in patients with cardiac arrest in response to chest compressions are the configuration and compliance of the arrested patient's thoracic cage. In an analysis of over 3,500 patients with OHCA between 2005 and 2008 in Arizona, survival was most prominent in those who received chest compression only CPR who were younger than 40 years of age.8
This author has noticed that many patients who have survived OHCA have both a relatively narrow anterior–posterior chest diameter, and a relative straight vertebral column, the so‐called “straight back syndrome,” a condition where the anterior‐posterior chest diameter is quite narrow, as shown in Fig. 2.9, 10
Figure 2.
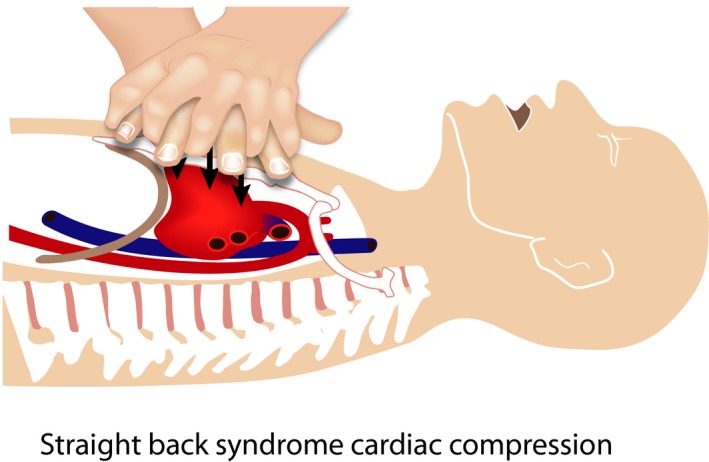
A drawing to depict a person with a very narrow anterior–posterior chest diameter, and a relatively straight vertebral column, the so‐called “straight back syndrome.”
In patients with an average chest configuration and those with so‐called “barrel chests,” secondary to emphysema or other causes, the lateral chest roentgenogram often shows a significant distance between the anterior chest‐wall and the heart (Fig. 3). In such patients it is nearly inconceivable that sternal compressions of the chest during CPR could result in cardiac compression. Rather, the mechanism of blood flow from chest compressions is probably secondary to the rhythmic alterations of the intrathoracic pressure and releases, for example, the “thoracic pump” theory.
Figure 3.
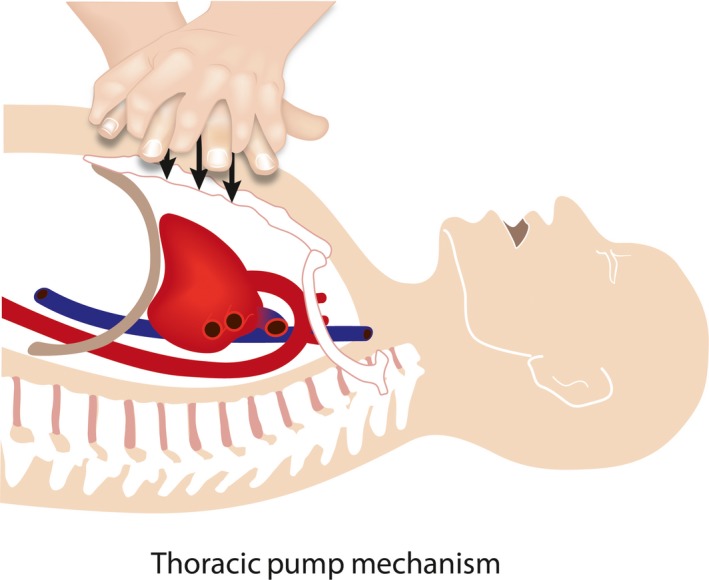
A drawing to depict a person with a large anterior–posterior chest diameter, when chest compressions for cardiac arrest would most likely not result in cardiac compression but rather a rhythmic increase increased in intrathoracic pressures as the mechanism of blood flow during attempted resuscitation for cardiac arrest.
What are these anterior–posterior chest measurements? They are currently unknown! Accordingly, since the author is retired, he encourages resuscitation researchers to correlate the anterior–posterior chest diameters of patients with cardiac arrest with survival and with the type of chest compression technique, including the types of mechanical devices used during the resuscitation efforts.
Do survivors of OHCA have more compliant chest walls?
Another characteristic of survivors of patients with primary (non‐respiratory) OHCA is that they are younger. In an analysis of patients with OHCA in Arizona, before and after the institution of cardiocerebral resuscitation (an approach that included advocating continuous chest compressions) by bystanders of patients with primary cardiac arrest,11, 12 it was found that survival was greater in younger than in older individuals (Fig. 4).8 It was reported that survival of patients with OHCA treated by bystander continuous chest compressions quadrupled in patients younger than 40 years of age, doubled in patients 40–49 years of age, but increased only somewhat in patients over the age of 50 years (Fig. 4).10 Younger patients in all probability have more compliant chests and are also are less likely to have comorbid medical conditions.
Figure 4.
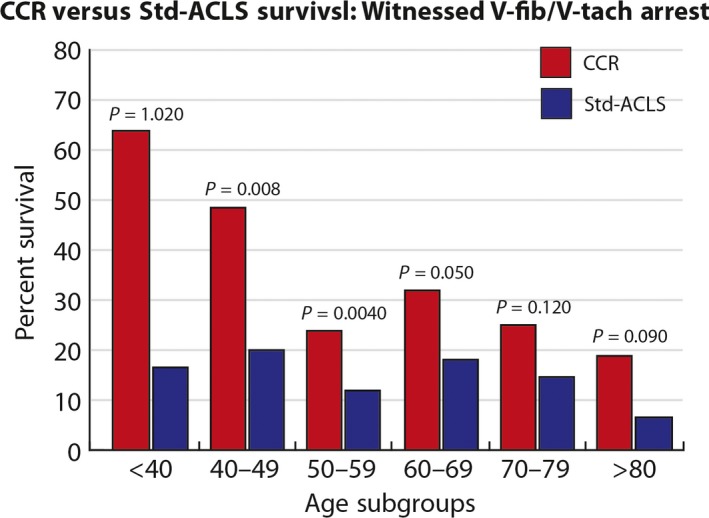
A graph derived from data published by Mosier and associates of patients with witnessed primary out‐of‐hospital cardiac arrest and a shockable rhythm who were treated by cardiocerebral resuscitation (CCR) in Arizona.8, 11, 12 It plots the percent survival of patients versus their age, showing better survival in younger patients. Std‐ACLS, Standard Acute Cardiac Life Support.
Thus, when it comes to the controversy over the mechanism of blood flow during chest compressions for cardiac arrest, there must be “some truths on each side.” The mechanism of blood flow during resuscitation efforts for recent cardiac arrest may well depend on the patient's anterior–posterior chest wall diameter (Figs 1–3), and other factors related to the patient's age (Fig. 4).
Conclusions
The mechanisms of blood flow during chest compressions for primary cardiac arrest may be somewhat determined by the patient's chest wall configuration and age. In those with narrow anterior–posterior chest diameters, especially in younger individuals, the mechanism of blood flow from chest compressions is probably predominantly that of cardiac compression. In older individuals and in those with increased anterior–posterior chest diameters, the mechanism of blood flow during CPR is probably predominantly secondary to increases in intrathoracic pressures. These observations need to be confirmed by researchers in resuscitation science. Finally, these observations call into question the previous assumption that the “straight back syndrome” is a benign condition.
Disclosure
Approval of the research protocol: N/A.
Informed consent: N/A.
Registry and the registration no. of the study/Trial: N/A.
Animal studies: N/A.
Conflict of interest: None declared.
Funding Information
No funding information provided.
References
- 1. Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed‐chest cardiac massage. JAMA 1960; 173: 1064–7. [DOI] [PubMed] [Google Scholar]
- 2. Halperin HR, Guerci AD, Chandra N et al Vest inflation without simultaneous ventilation during cardiac arrest in dogs: improved survival from prolonged cardiopulmonary resuscitation. Circulation 1986; 74: 1407–15. [DOI] [PubMed] [Google Scholar]
- 3. Higano ST, Oh JK, Ewy GA, Seward JB. The mechanism of blood flow during closed chest cardiac massage in humans: transesophageal echocardiographic observations. Mayo Clin. Proc. 1990; 65: 1432–40. [DOI] [PubMed] [Google Scholar]
- 4. Halperin HR, Tsitlik JE, Gelfand M et al A preliminary study of cardiopulmonary resuscitation by circumferential compression of the chest with use of a pneumatic vest. N. Engl. J. Med. 1993; 329: 762–8. [DOI] [PubMed] [Google Scholar]
- 5. Feneley MP, Maier GW, Kern KB et al Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation 1988; 77: 240–50. [DOI] [PubMed] [Google Scholar]
- 6. Halperin HR, Paradis N, Ornato JP et al Cardiopulmonary resuscitation with a novel chest compression device in a porcine model of cardiac arrest: improved hemodynamics and mechanisms. J. Am. Coll. Cardiol. 2004; 44: 2214–20. [DOI] [PubMed] [Google Scholar]
- 7. Gates S, Quinn T, Deakin CD, Blair L, Couper K, Perkins GD. Mechanical chest compression for out of hospital cardiac arrest: systematic review and meta‐analysis. Resuscitation 2015; 94: 91–7. [DOI] [PubMed] [Google Scholar]
- 8. Mosier J, Itty A, Sanders A et al Cardiocerebral Resuscitation is associated with improved survival and neurologic outcome from out‐of‐hospital cardiac arrest in elders. Acad. Emerg. Med. 2010; 17: 269–75. [DOI] [PubMed] [Google Scholar]
- 9. Davies MK, Mackintosh P, Cayton RM, Page AJ, Shiu MF, Littler WA. The straight back syndrome. Q. J. Med. 1980; 49: 443–60. [PubMed] [Google Scholar]
- 10. Deleon AC Jr, Perloff JK, Twigg H, Majd M. The straight back syndrome: clinical cardiovascular manifestations. Circulation 1965; 32: 193–203. [DOI] [PubMed] [Google Scholar]
- 11. Ewy GA. Cardiocerebral resuscitation: the new cardiopulmonary resuscitation. Circulation 2005; 111: 2134–42. [DOI] [PubMed] [Google Scholar]
- 12. Kern KB, Valenzuela TD, Clark LL et al An alternative approach to advancing resuscitation science. Resuscitation 2005; 64: 261–8. [DOI] [PubMed] [Google Scholar]


