Abstract
Background
Moderate to vigorous endurance and strength-training exercise was suggested as a treatment option for major depression. However, there is little evidence to support this suggestion in adolescent patients. The present study investigates the effects of a whole-body vibration strength-training intervention on symptoms in medication-naïve adolescent inpatients experiencing a major depressive episode. Potential underlying endocrinological and neurobiological mechanisms are explored.
Methods/design
A double-blinded randomized controlled trial is conducted at the University Hospital of Cologne in Germany, comparing a 6-week, whole-body vibration strength-training with a 6-week placebo-intervention, as add-on therapy to inpatient treatment as usual. Forty-one subjects (13–18 years of age) will be included in each of the two groups. The study is powered to detect (α = .05, β = .2) a medium effect size difference between the two groups (d = .5) in terms of patients’ change in the Children’s Depression Rating Scale raw-score, from baseline until the end of the intervention. As secondary endpoints, the effects of exercise treatment on patients’ cortisol awakening response as well as on brain-derived neurotrophic factor, insulin-like growth factor 1 and inflammatory markers (tumor necrosis factor-alpha, interleukin-6 and C-reactive protein) serum levels will be assessed.
Discussion
This study will provide evidence on the effectiveness of whole-body vibration strength-training as an add-on therapy in adolescent inpatients experiencing a major depressive episode. After completion of data collection, the present study will be the largest randomized controlled trial so far to investigate the effectiveness of an exercise intervention in inpatient adolescents suffering from a major depressive episode. Moreover, the present study may help to determine the underlying mechanisms of potential anti-depressant effects of exercise in depressed adolescent inpatients.
Trial registration
DRKS.de, German Clinical Trials Register (DRKS), Identifier: DRKS00011772. Registered on 20 March 2017.
Electronic supplementary material
The online version of this article (10.1186/s13063-018-2747-8) contains supplementary material, which is available to authorized users.
Keywords: Exercise, Whole-body vibration, Major depression, Adolescence, Cortisol, Neurotrophins, Inflammatory markers
Background
Depression is one of the most common psychiatric diagnoses among adolescents [1, 2]. Prevalence rates of between 3 and 6% for meeting full criteria of major depressive disorder are reported [3–5]. Adolescent depression is particularly malignant. It increases the likelihood of recurrence and chronicity in adulthood [6, 7]. It is frequently accompanied by a wide range of psychiatric and somatic comorbidities [8–11] and typically leads to substantial impairment in social [12] and cognitive functioning [13], as well as in scholastic and vocational performances [13, 14]. The increased risk for suicide makes depression the third leading cause of death among adolescents worldwide [15].
In most countries, clinical guidelines recognize cognitive behavioral therapy and pharmacotherapy with the selective serotonin re-uptake inhibitor fluoxetine, or the combination of both, as evidence-based treatment options for adolescent depression [16–20]. However, cognitive behavioral therapy can be inaccessible and expensive [21, 22], whereas a clear advantage of pharmacotherapy for children and adolescents was recently questioned [23]. Pharmacotherapy entails possible side-effects [24]. Fluoxetine and venlafaxine were shown to be associated with an elevated risk of suicidal ideation and behavior (suicidality) in adolescents [25, 26]. Accordingly, alternative treatment approaches for adolescent depression are required. Recently, there has been a growing interest in physical activity as an alternative treatment option for depression. In adults suffering from a major depressive episode, a recent meta-analysis of 35 randomized controlled trials showed a moderate clinical effect of exercise treatments on depression symptoms [27]. Trials investigating the benefits of exercise interventions in adolescents experiencing a major depressive episode are rare [28], but first evidence is promising [29–31].
In a recent pilot study, our group showed comparable anti-depressant effects of a whole-body vibration strength-training (WBV-training) to an ergometer training intervention on a stationary cycle in adolescent stationary patients, when compared to treatment as usual (TAU). However, WBV-training was better accepted and patients reported higher motivation to maintain physical activity after discharge from the clinic compared to ergometer training [31]. Based on these findings, the present study continues to investigate WBV-training as a potential add-on therapy for adolescents suffering from a major depressive episode. The main objective of the present study is to replicate the anti-depressant effects of the 6-week WBV-training on depression symptoms in adolescent inpatients while also improving methodological shortcomings of our previous pilot study. Unlike in our pilot study, WBV-training is not tested against TAU, but against a placebo control group intervention (PCG-intervention) (supervised myofascial release training + TAU) providing a comparable amount of psychosocial stimulation. Moreover, in the present study, allocation to treatment groups is completely randomized. The severity of depression symptoms is not exclusively assessed by self-report, but also by blinded clinician rating. The statistical test power will be increased.
Several endocrinological and neurobiological adaptations to physical activity have been proposed to explain the anti-depressant effect of exercise interventions [32]. Emphasis is put on the positive effect of exercise on the hypothalamic-pituitary-adrenal axis (HPA axis) [33, 34], on neurotrophin [34, 35] and growth factor expression [36], as well as on inflammatory markers [34, 37, 38]. Changes in these parameters are supposed to promote beneficial structural and functional changes of the central nervous system via different pathways [39, 40], resulting in improvement of depression symptoms [34, 41]. However, existing research has been conducted almost exclusively in adults. Therefore, the secondary objective of the present study is to investigate endocrinological and neurobiological adaptations to the 6-week WBV-training. The effect of the WBV-training on HPA axis activity is assessed by measuring patients’ salivary cortisol awakening response [42]. WBV-training-induced changes in brain-derived neurotrophic factor (BDNF), insulin-like growth factor 1 and inflammatory markers (tumor necrosis factor-alpha, interleukin-6 and C-reactive protein (CRP)) serum levels are explored.
Methods/design
The present study is designed as a longitudinal interventional study with two randomized treatment groups whose members will engage for 6 weeks in physical activity as add-on therapy to TAU (parallel-group, double-blinded, randomized controlled trial). The pre-specified objectives and hypotheses are listed in Table 1. The study flowchart is shown in Fig. 1. The study protocol was approved by the Ethics Committee of the University Hospital of Cologne (Germany) and is registered at the World Health Organization trial register (Identifier: DRKS00011772, see also Additional file 1). Any modifications to the protocol which may impact on the conduct of the study, potential benefit of the patient or may affect patient safety, including changes of study objectives, study design, patient population, sample sizes, study procedures, or significant administrative aspects will require a formal amendment by the ethics commission. The study conforms to the Declaration of Helsinki.
Table 1.
Objectives and hypotheses of the study
| Objectives | Hypotheses |
|---|---|
| Main objective • To evaluate the effect of a 6-week whole-body vibration-training vs. placebo on clinician-rated severity of depression symptoms in adolescent inpatients experiencing a major depressive episode |
Main hypothesis • In adolescent inpatients experiencing a major depressive episode, the change in the Children’s Depression Rating Scale-Revised raw-scores from baseline to completion of the 6-week intervention differs significantly between the whole-body vibration strength-training group and the control group (hypothesis A) |
| Secondary objectives • To evaluate the effect of a 6-week whole-body vibration-training vs. placebo on hypothalamic-pituitary-adrenal axis dysregulation in adolescent inpatients experiencing a major depressive episode |
Secondary hypotheses • In adolescent inpatients experiencing a major depressive episode, the change in cortisol awakening response from baseline to completion of the 6-week intervention differs significantly between the whole-body vibration-training group and the control group (hypothesis B) |
| • To evaluate the effect of a 6-week whole-body vibration-training vs. placebo on neurotrophin and growth factor expression in adolescent inpatients experiencing a major depressive episode | • In adolescent inpatients experiencing a major depressive episode, the change of brain-derived neurotrophic factor and insulin-like growth factor 1 serum levels from baseline to completion of the 6-week intervention/to 8 weeks’ follow-up differs significantly between the whole-body vibration-training group and the control group (hypothesis C) |
| • To evaluate the effect of a 6-week whole-body vibration-training vs. placebo on inflammatory-marker expression in adolescent inpatients experiencing a major depressive episode | • In adolescent inpatients experiencing a major depressive episode, the change in tumor necrosis factor-alpha, interleukin-6, C-reactive protein serum levels from baseline to completion of the 6-week intervention/to 8 weeks’ follow-up differs significantly between the whole-body vibration-training group and the control group (hypothesis D) |
| • To evaluate the effect of a 6-week whole-body vibration-training vs. placebo on self-perceived severity of depression symptoms in adolescent inpatients experiencing a major depressive episode | • In adolescent inpatients experiencing a major depressive episode, the change of Beck’s Depression Inventory-second edition raw-scores from baseline to completion of the 6-week intervention/to 8 weeks’ follow-up/to 20 weeks’ follow up differs significantly between the whole-body vibration-training group and the control group (hypothesis E) |
| • To evaluate the sustainability of the effect of the 6-week whole-body vibration-training vs. placebo on clinician rated severity of depression symptoms in adolescent inpatients experiencing a major depressive episode | • In adolescent inpatients experiencing a major depressive episode, the change of Children’s Depression Rating Scale-Revised raw-scores from baseline to 8 weeks’ follow-up/to 20 weeks’ follow-up differs significantly between the whole-body vibration-training and the control group (hypothesis F) |
Fig. 1.
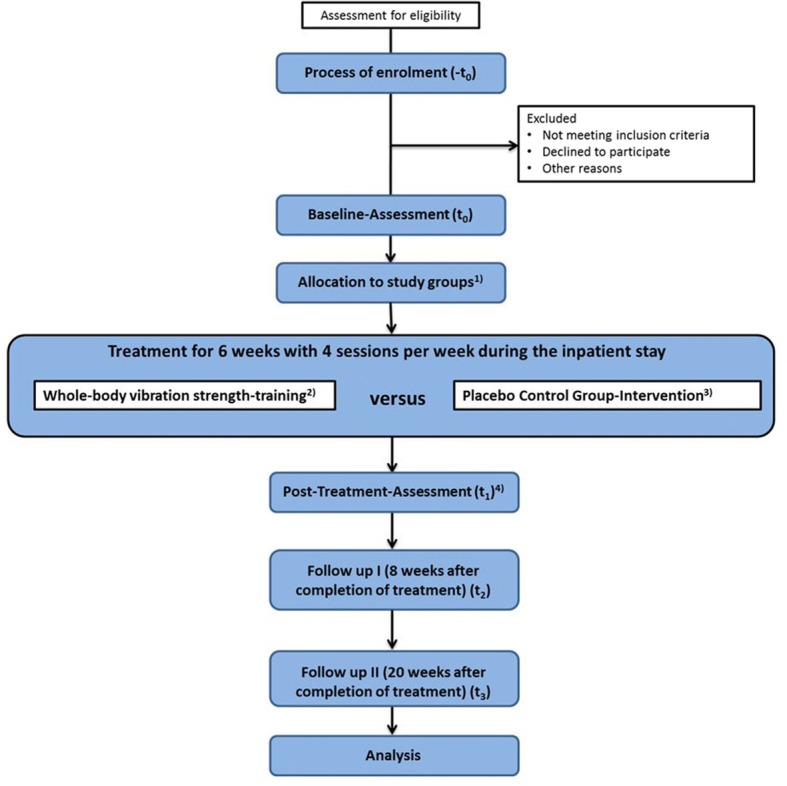
Flowchart of the trial. (1) A stratified block randomization with permuted block length is conducted to allocate patients into treatment groups. The stratification factor is patients’ gender (male vs. female); (2) Participants allocated to the whole-body vibration strength-training perform static and dynamic exercises on a Whole Body Vibration Plate; (3) Participants allocated to the Placebo Control Group receive a supervised myofascial release training program hardly inducing any muscular effort and cardiovascular stimulation; (4) Post-Treatment Assessment (t1) is conducted after completion of the 6-week exercise-treatment phase
Study population and recruitment
Participants are recruited from the adolescent psychiatric wards of the Department of Child and Adolescent Psychiatry and Psychotherapy at the University Hospital of Cologne, Germany. On admission to the inpatient treatment, adolescents and their parents (or other caregivers) are contacted by the study coordinator and informed about the program. If interest in participation is expressed, patients will be screened for eligibility. Inclusion and exclusion criteria of the study are listed in Table 2. Patients are included in the study only after they and their parents (or other caregivers) give written informed consent. The participants are included chronologically.
Table 2.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| • 13–18 years of age • Undergoing inpatient psychiatric treatment • Within the first 3 weeks of inpatient treatment • Meeting DSM-V and ICD-10 criteria of non-psychotic major depressive disorder assessed by clinician rating with the structured clinical interview ‘Schedule for Affective Disorders and Schizophrenia adapted for school-aged children (present and life-time)’ • Baseline raw-score of at least 40 points in the Children’s Depression Rating Scale-Revised |
• Comorbid schizophrenia, personality disorder, autism spectrum disorder, schizoaffective disorder, acute or past psychotic events • Acute suicidality • Current substance abuse • Permanent medication with inherent psychotropic effects including fluoxetine • Non-substituted hypothyroidism • Addison’s disease • Body Mass Index less than 16 kg/m2 • Any contraindication that prevents participation in the exercise intervention • Insufficient knowledge of the German language • Intelligence quotient less than 70 |
DSM-V Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, ICD-10 10th revision of the International Statistical Classification of Diseases and Related Health Problems
Randomization and blinding
Eligible patients are randomized to one of two treatments (see “Groups and treatments” section below). A stratified block randomization with permuted block length is conducted. The stratification factor is patients’ gender (male vs. female). Randomization of treatment groups is implemented based on sealed, opaque envelopes by the Institute of Medical Statistics and Computational Biology of the University of Cologne.
The present study is a double-blinded trial. Prior to participation, patients will be informed that two physical activity interventions (whole-body vibration strength-training/myofascial release training) will be compared regarding their effect on severity of depression symptoms in adolescent inpatients. Accordingly, patients do not know the specific hypotheses of the trial. They will not know if they are allocated to the experimental or to the control group and, therefore, can be considered blinded. Moreover, experimental testing procedures will be carried out by specially trained experimental staff that will also be blinded regarding the allocation of participants to the specific experimental group.
Groups and treatments
WBV-training and PCG-intervention are conducted at the Department of Child and Adolescent Psychiatry and Psychotherapy at the University Hospital of Cologne. The participants of both intervention groups exercise four times per week for 6 weeks during their inpatient stay. Each session lasts approximately 30 min. The intervention sessions are carried out individually or in small groups with up to four participants. Training sessions are always instructed by specially trained study staff. In the following, WBV-training and PCG intervention will be described in detail:
Whole-body vibration strength-training
Participants perform static and dynamic exercises on the Galileo® Whole Body Vibration Plate Med M (Novotec Medical GmbH, Pforzheim, Germany). The training sessions consist of six standardized exercises: squats, lunges, upper-body rotation against resistance, butterfly reverse against resistance, standing in partial squatting position, rocking the feet between the ball and heel. Resistance is applied using a latex resistance band (TheraBand, Akron, OH, USA). Each exercise is performed for 2 min. at 24 Hz and standing with feet parallel on the vibration plate, feet hip width apart. Between each exercise, participants stay active conducting low-intense shoulder and hip mobilization exercises for 2 min. After completion of four training sessions, vibration frequency is increased to 26 Hz. After completion of 12 trainings, the time of each exercise is increased to 3 min with 3-min. active rest intervals between the exercises.
Placebo control group intervention
Patients allocated to the PCG-training receive a supervised myofascial release training program. The training sessions consist of seven standardized exercises using a foam roll (Blackroll, Bottighofen, Switzerland): self-massage of the soles of the feet (one leg stand), of the calves (lying in dorsal position), of the hamstrings (lying in dorsal position), of the thighs (manually while lying in dorsal position), of the neck (lying in dorsal position), of the lower and upper back (leaning backwards against a wall in standing position), as well as self-massage of the upper arm and shoulder (leaning sideways against a wall in standing position). Each exercise is repeated 10 times on each side of the body. Between each exercise, participants do low-intensity shoulder and hip mobilization exercises for 2 min. The PCG-intervention was designed to provide an amount of psychosocial stimulation comparable to the WBV-training. All myofascial release exercises are instructed and patients are corrected, if necessary. However, unlike the WBV-training, myofascial release training sessions applied to the PCG hardly induce any muscular effort and cardiovascular stimulation.
Contraindications for participation in a training session in the WBV-training and in the PCG-intervention are acute suicidality, injuries, infections, or fever. To increase adherence to the training, participants are picked up from the ward by study staff. Treatment participation and comments on each session will be recorded.
The WBV-training and PCG-intervention are conducted simultaneously with the patients’ TAU at the Department of Child and Adolescent Psychiatry and Psychotherapy at the University Hospital of Cologne. TAU is carried out by a multidisciplinary team, consisting of psychiatrists, psychotherapists, music therapists, art therapists, pedagogs and social workers. Patients receive psychotherapy in the form of individual sessions one to two times per week. Families are closely involved in the patients’ therapy process. Every 4 weeks, systemic family therapy sessions are conducted. In addition, patients participate in individual and group music-therapy and art-therapy sessions. Counseling by the social services is conducted once or twice during inpatient stay.
Data collection and timeline
Data are collected during the process of enrollment (− t0), at baseline (t0), after completion of the 6-week intervention (t1), 8 weeks after completion of the 6-week intervention (follow-up I, t2), as well as 20 weeks after completion of the 6-week intervention (follow-up II, t3). At –t0, patients’ demographic (age, sex, education, socioeconomic status) and anthropometric data (weight, height, Body Mass Index (BMI)), as well as past medical history and current medication, are collected. To determine patients’ eligibility for study participation before allocation to treatment groups, the primary outcome measure of the planned study (the Children’s Depression Rating Scale-Revised (CDRS-R)) is also assessed at − t0. A raw-score of 40 or more points in the CDRS-R must be present to take part in the study [43] (compare Table 2). Baseline measurement takes place 1–3 days after enrollment. At t0, all secondary outcome measures of the study (see “Secondary endpoints” section below), as well as potential confounding factors (see “Potential confounding factors” section below), are protocolled. At t1, the primary outcome measure and all secondary outcome measures are assessed. The t1 measurement takes place 1–3 days after completion of the 6-week exercise-treatment phase. At t2, the primary outcome measure and all secondary outcome measures of the study, except cortisol awakening response, are assessed. Finally, at t3, only the CDRS-R and the Beck’s Depression Inventory -second edition (BDI-II) are applied. Time accuracy of both follow-up intervals lies within a range of ± 3 days. The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) study schedule of enrollment, interventions and assessments is provided in Fig. 2. The SPIRIT Checklist [44] is provided as Additional file 2 to this publication.
Fig. 2.
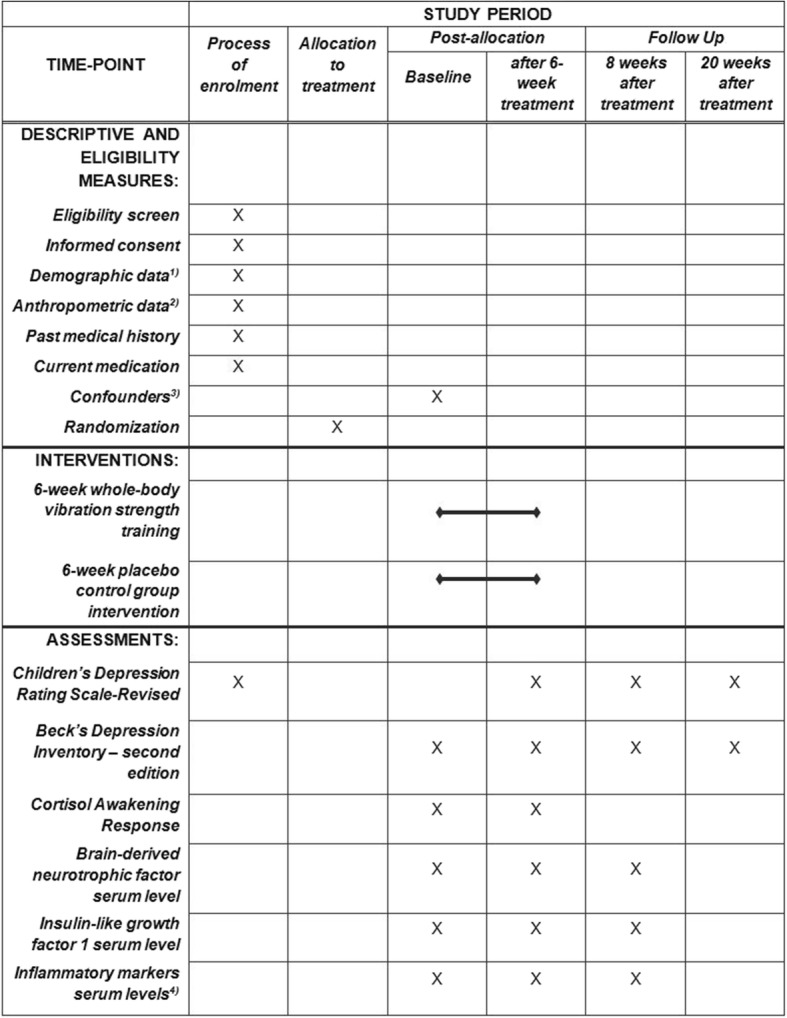
The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) schedule of enrollment, interventions and assessments. (1) Demographic data will be assessed: age, sex and education; (2) Anthropometric data will be assessed: height, weight and BMI; (3)Potential confounding factors will be assessed: current psychiatric comorbidities, as well as patients’ history of mental disorders (Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version adapted for school-aged children, Diagnostic System for Mental Disorders in Childhood and Adolescence), emotional and/or behavioral problems (Child Behavior Checklist/4–18, Youth Self-Report/11–18) and socioeconomic status (modified questionnaire from Trinkl and colleagues [51]); (4) Inflammatory markers will be assessed: tumor necrosis factor-alpha, interleukin-6 and C-reactive protein are assessed
Primary endpoint
The primary endpoint of the present study is patients’ change of severity of depression symptoms from baseline until the end of the 6-week intervention. Patients’ severity of depression symptoms is measured by the CDRS-R. In the context of clinical trials, the CDRS-R is one of the most frequently used clinician ratings for the assessment of depressive symptomatology in adolescents [45]. The CDRS-R is a semi-structured interview consisting of 17 items that are rated between 1 (“no difficulties”) and 5 or 7 points (“clinically significant difficulties”). Usually, a raw-score of 40 points is used as a cut-off for depressive symptomatology and higher raw-scores are interpreted as more severe depression symptoms [43]. For CDRS-R application in adolescents, excellent internal consistency and good convergent validity have been reported [45].
Secondary endpoints
The following secondary endpoints are assessed in the present study:
Hypothalamic-pituitary-adrenal axis activity
HPA axis activity is assessed by measuring patients’ cortisol awakening response. Saliva samples are collected after forced awakening at 7.00 and at 7.30 a.m. on two consecutive weekdays at t0 and at t1. Patients are asked to remain in bed without going back to sleep and to refrain from drinking and eating during the 30-min sampling period. In case of non-adherence (i.e., awakening before forced waking, rising before the second sample is collected, eating, or drinking), the procedure is repeated on the following day. Saliva is collected using Salivette collection devices (Sarstedt, Nümbrecht, Germany). Saliva samples are frozen and stored at − 20 °C until analysis. After thawing, salivettes are centrifuged at 3000 rpm for 5 min. Salivary cortisol concentrations are measured using commercially available chemiluminescence immunoassay with high sensitivity (IBL International, Hamburg, Germany). The intra- and interassay coefficients for cortisol are required to be below 8%. To measure HPA axis activity, mean salivary cortisol concentration and the increase between baseline and the 30-min samples are determined.
Serum brain-derived neurotrophic factor, insulin-like growth factor 1 and inflammatory-marker levels
Drawing of 8.5 ml venous blood from sedentary patients is performed at t0, t1 and t2. Samples for BDNF, cytokine (insulin-like growth factor-1, tumor necrosis factor-alpha, interleukin-6) and CRP analysis will be taken from a peripheral vein of the arm and collected in serum gel tubes (S-Monovette® Serum, Sarstedt, Nümbrecht, Germany). After complete coagulation at 4 °C, samples will be centrifuged for 10 min. at 1000 g and 4 °C. The serum will be prepared and aliquoted within 24 h after blood drawing. Duplicate samples will be stored at − 80 °C until analyzed when samples of all included participants are collected. Serum levels of BDNF and cytokines are assessed at t0, t1 and t2. BDNF and cytokines will be measured in duplicates in a multiplex analyzer (Bio-Plex 200®, Bio-Rad Laboratories) according to the manufacturer’s instructions. Sera will be thawed, centrifuged for 10 min. at 10,000 g and 4 °C and diluted in sample diluent (1:4). By using the median of the fluorescence intensity and the standard curve, the absolute concentration of BDNF and the cytokines (pg/ml) will be calculated (Bio-Plex Manager 6.1, Bio-Rad Laboratories). For determination of CRP, the blood will be drawn as described above in lithium-heparin tubes (S-Monovette®, lithium-heparin, Sarstedt, Nümbrecht, Germany). It will be centrifuged for 10 min. at 4000 g and 21 °C. Plasma will be aliquoted within 3 h after blood drawing and used fresh. The CRP level will be determined via latex agglutination assay according to the manufacturer’s instructions (C-Reactive Protein Gen.3, cobas®, Roche Diagnostics, Basel, Switzerland). Briefly, plasma will be diluted 1:100 and added on a slide, which is pre-coated with antibodies to monoclonal anti-human CRP and latex reagent. After 2 min incubation, clear agglutination will be observed on the slide and it will be examined turbidimetrically using the analytic system cobas® C702 (Roche Diagnostics). CRP values below 3 mg/l are considered clinically irrelevant and will be adjusted to 0 mg/l.
Self-rated severity of adolescent patients’ depression symptoms
For the self-rating procedure, the German version of the BDI-II [46] is applied. The BDI-II was developed as an indicator of the presence and severity of depression in psychiatric patients from 13 years of age onwards. Twenty-one symptoms are rated by the patient from 0 to 3, with higher scores indicating more severe occurrence of the particular symptom. Accordingly, the sum score ranges from 0 to 63, with higher scores indicating more severe depressive symptomatology. The BDI-II is sensitive for changes in severity of depressive symptomatology. Excellent indices of reliability, as well as good discriminant and convergent validity, have been reported in adolescent psychiatric inpatients [47].
Sustainability of effects of whole-body vibration strength-training on severity of depression symptoms
CDRS-R is additionally applied 8 and 20 weeks after completion of the treatment to assess sustainability of potential effects of WBV-training compared to placebo.
The “Balancing Vibrations Study” also comprises magnetic resonance imaging, as well as combined transcranial magnetic stimulation and electroencephalographic recordings. For clarity, the more complex protocols and hypotheses, regarding these neuroimaging/neurophysiological parameters, will be illustrated separately and reported elsewhere.
Potential confounding factors
Several additional factors, potentially impacting the primary outcome of the study (severity of depression symptoms), are assessed at t0. To confirm depression diagnosis and to capture current psychiatric comorbidities, as well as patients’ history of mental disorders, the “Schedule for Affective Disorders and Schizophrenia – Present and Lifetime Version adapted for school-aged children” [48] and the “Diagnostic System for Mental Disorders in Childhood and Adolescence” [49] are applied. For assessment of emotional and/or behavioral problems, the “Child Behavior Checklist/4–18,” as well as the “Youth Self-Report/11–18” of the Achenbach System of Empirically Based Assessment, are used [50]. The patients’ socioeconomic status is assessed with a modified questionnaire developed by Trinkl and colleagues [51].
Adverse events and compliance assessment
Adverse events and serious adverse events, which are related to the interventions, are assessed by the clinicians. During our pilot study, neither adverse events nor severe adverse events occurred [31]. Compliance to WBV-training and PCG-intervention is protocolled by scientific staff. It was pre-defined that patients need to participate in 20 sessions for complete compliance. This was shown feasible in our pilot study [31].
The Department of Child and Adolescent Psychiatry and Psychotherapy at the University Hospital of Cologne has insurance to cover for non-negligent harm associated with the protocol. This will include cover for additional health care, compensation, or damages. Incidences judged to arise from negligence (including those due to major protocol violations) will not be covered by study insurance policies.
Data management and confidentiality
All data will be entered electronically by two independent student assistants. Any deviations will be clarified and corrected. Original study forms will be kept on file. All study-related information is stored in a secure and accessible place and manner. All participant information will be stored and locked in file cabinets in areas with limited access. Participant files will be kept in storage for a period of 3 years after completion of the study. Blood samples will be disposed after analyses.
All laboratory samples, reports, data collection, process and administrative forms will be identified by a coded identification number, to maintain participant confidentiality. All records that contain names or other personal identifiers, such as locator forms and informed consent forms, will be stored separately from study records, which are also identified by code numbers. All local databases will be secured with password-protected access systems. Forms, lists, logbooks, appointment books and any other listings that link participant identification numbers to other identifying information will be stored in a separate, locked file in an area with limited access.
Sample size calculation
Sample size calculation was done for the effect of experimental treatment (WBV-training vs. PCG intervention) on the primary endpoint (severity of depression symptoms) measured by CDRS-R raw-scores in an analysis of covariance (ANCOVA) model using G*Power 3.1.9.2 software [52]. It was hypothesized that changes in the CDRS-R raw-scores from baseline to completion of the 6-week intervention differ significantly between the WBV-training group and the PCG-training group. As clinically relevant effect size, a medium effect of d = .5 was defined. Alpha was set at 5%. Test power (1 − β) was set at 80%. Participants’ CDRS-R scores at baseline will be included in the model as covariate. Required sample size in such an ANCOVA model can be calculated as (1 − ρ2) × n, with ρ representing the correlation between participants’ baseline and post-treatment outcome scores, and n representing the sample size that would have been required if a t test of post-treatment outcome scores was applied [53]. Based on the results of our pilot study, we estimated the correlation between patients’ severity of depression symptoms at baseline and at post treatment with ρ = .6. Under the presuppositions made, sample size calculation showed that 41 patients in each group (N = 82) would be required. We accounted for a 15% dropout rate, leading to a total sample size of N = 94 patients.
Statistical analysis
An intention-to-treat analysis will be performed. We will also assess the effect of the complete treatment in a per-protocol analysis. To determine the effects of between-subjects factor “treatment,” within-subjects factor “measurement time point” and their interaction on primary and secondary outcomes, separate 2 × 3 (hypothesis A, E, F)/2 × 2 (hypothesis C, D) mixed ANCOVAs will be conducted. For secondary outcome “HPA axis activity” (hypothesis B) separate 1-factor ANCOVA will be conducted. As covariate, patients’ baseline scores of each specific parameter will be used. A significant main effect of within-subjects factor measurement time point will be further investigated through post hoc pairwise comparisons. Simple effects analyses will be conducted to determine potential group differences at each time point. Due to the exploratory character of the secondary hypotheses, alpha error adjustment will not be applied.
ANCOVA assumptions will be explored. In case of violations of normality assumption, appropriate non-parametric procedures will be used. In case of violations of ANCOVA assumptions of homogeneous variances for between-subjects factor levels and sphericity for variances of differences between categories of within-subjects factor, the F-test will be adjusted. Eta-squared values will be reported as effect size estimates for explained variance, and Cohen’s d values will be reported for post hoc pairwise comparisons.
Statistical analysis will be performed by a statistician, blinded to treatment groups. Statistical analyses will be conducted using SPSS 25® (IBM®, Armonk, NY, USA). A result will be considered significant at a p value equal to or less than .05.
Discussion
Research on the anti-depressant effects of physical activity in clinically depressed adolescent patients is rare. Apart from our previously published pilot study [31], to the best of our knowledge, only two small trials examined the effects of exercise interventions in clinically depressed adolescent patients [29, 30]. The latter two studies exclusively included ambulatory patients. Our pilot study was the first to investigate the anti-depressant effects of an exercise intervention on depression symptoms in adolescents in an inpatient setting. The first results are promising. Anti-depressant effects, comparable to those reported in clinically-depressed adults [27], were shown. However, methodological shortcomings; e.g., small sample sizes, incomplete randomization, lack of placebo treatment in the control group, and only self-report of depressive symptoms, reduce the validity of the existing results. To incorporate physical activity into treatment of adolescent depression, more clinical randomized controlled trials at a high methodological level are needed. After completion of data collection, the present study will be the largest randomized controlled trial so far to investigate add-on exercise therapy in inpatient adolescents experiencing a major depressive episode.
Beyond the investigation of anti-depressant effects of WBV-training on clinical depression symptoms in adolescent inpatients, the present study explores potential underlying physiological mechanisms. To reliably attribute changes in clinical depression symptoms, after an exercise intervention to physiological adaptations to the physical activity, exercise treatment and control group treatment must fulfill the ceteris paribus clause. This means that the exercise group and the control group should be equal regarding all factors except for the critical ingredient (here: the physical exertion) [54, 55]. The present study compares the effects of WBV-training, not just against TAU, but against a placebo control group. WBV-training and PCG-training are both supervised and, therefore, exhibit a comparable amount of social attention to the patients. Accordingly, it will be possible to disentangle the effects of physiological factors from the potential effects of psychosocial factors related to the experimental treatment on patients’ depression symptoms. Thus, placebo and Hawthorne effects can be avoided.
The knowledge about the endocrinological and neurobiological mechanisms potentially underlying the anti-depressant effects of exercise is still in its infancy. Moreover, existing research has been conducted almost exclusively in adults. Our study will contribute to filling this knowledge gap. The present study investigates the effects of WBV-training on HPA axis activity, neurotrophin expression and inflammatory-marker expression. Hyperactivity of the HPA axis in major depression is one of the most consistent and robust biological findings in psychiatry. Hyperactivity of the HPA axis results in hypercortisolemia [56]. Continuously increased levels of cerebral cortisol lead to increased brain inflammation [57]. The anti-inflammatory effect of acute cortisol secretion changes with chronic exposure to a pro-inflammatory effect [58, 59]. Chronic glucocorticoid exposure and increased levels of CRP and pro-inflammatory cytokines, such as tumor necrosis factor-alpha and interleukin-6, within the central nervous system are associated with reduced levels of neurotrophins, like BDNF [60]. First evidence indicates that exercise positively influences cortisol levels in depressed adolescents [37], but further research is required. In adults exhibiting depression symptoms, neuroimmunomodulatory effects [61] and increases in neurotrophins due to exercise training have been reported [62]. It remains unclear if WBV-training in clinically depressed adolescents has similar molecular effects.
Trial status
The recruitment of the patients started on 1 August 2017 and is still ongoing. Recruitment is expected to be completed by 31 July 2020. The data analysis and the writing of scientific manuscripts will be carried out after completion of recruitment.
Additional files
All Items from the World Health Trial Registration Data Set. (PDF 80 kb)
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 Checklist. (PDF 129 kb)
Acknowledgements
The authors thank Prof. Clemens Kirschbaum (Ph.D.) and Mrs. Sarah Brand for their support in the description of the HPA axis activity assessment, and Mrs. Rozeta Levkovska for her proof-reading.
Funding
This work received funding from the Marga and Walter Boll-Stiftung (project number: 210–07.2-11). The Marga and Walter Boll-Stiftung is located at Marie-Curie-Straße 8, 50170 Kerpen, Germany and can be contacted via phone (+ 49 2273 99 17 512), or email (info@bollstiftung.de). The funding source had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, nor in the decision for publication of the results.
Availability of data and materials
The data sets of this study will be made available by the corresponding author on reasonable request.
Abbreviations
- ANCOVA
Analysis of covariance
- BDI-II
Beck’s Depression Inventory-second edition
- BDNF
Brain-derived neurotrophic factor
- CDRS-R
Children’s Depression Rating Scale-Revised
- CRP
C-reactive protein
- DRKS
German Clinical Trials Register
- HPA axis
Hypothalamic-pituitary-adrenal axis
- PCG-intervention
Placebo control group intervention
- SPIRIT
Standard Protocol Items: Recommendations for Interventional Trials
- t0
Baseline measurement
- − t0
Time point of enrollment
- t1
After completion of the 6-week intervention
- t2
8 weeks after completion of the 6-week intervention; follow-up I
- t3
20 weeks after completion of the 6-week intervention; follow-up II
- TAU
Treatment as usual
- WBV-training
Whole-body vibration training
Authors’ contributions
MO, NG, HLW and SB are responsible for the development of the trial. MO and JLG have implemented the trial and are trial managers. MO wrote the manuscript for the study protocol. OF, AM, EM and SB contributed to the manuscript development and provided clinical expertise. MO is responsible for designing statistical procedures. AZ contributed to the description of the treatments. EM will perform the cytokine analyses. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethical approval has been obtained from the Ethics Committee of the University Hospital of Cologne, Germany (reference number 15–426). The trial was registered at drks.de (ID: DRKS00011772) prior to starting recruitment. Patients are being informed about the risks and possible benefits of the study. Participation in this study is voluntary. Written informed consent is being obtained from all patients.
Consent for publication
All participants give consent to the publication of the results and receive adequate anonymization. All data will be analyzed with confidentiality. This information is included in the written informed consent.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s13063-018-2747-8) contains supplementary material, which is available to authorized users.
Contributor Information
Max Oberste, Phone: +49 (0) 221 478 76909, Email: max.oberste-frielinghaus@uk-koeln.de.
Nicola Großheinrich, Email: n.grossheinrich@katho-nrw.de.
Heidrun-Lioba Wunram, Email: heidrun-lioba.wunram@uk-koeln.de.
Johannes Levin Graf, Email: levingraf@posteo.de.
Alischa Ziemendorff, Email: alischa.ziemendorff@uk-koeln.de.
Axel Meinhardt, Email: axel.meinhardt@uk-koeln.de.
Oliver Fricke, Email: o.fricke@gemeinschaftskrankenhaus.de.
Esther Mahabir, Email: esther.mahabir-brenner@uni-koeln.de.
Stephan Bender, Email: stephan.bender@uk-koeln.de.
References
- 1.Satcher DS. Executive summary: a report of the Surgeon General on mental health. Public Health Rep. 2000;115:89–101. doi: 10.1093/phr/115.1.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bettge S, Wille N, Barkmann C, Schulte-Markwort M, Ravens-Sieberer U. Depressive symptoms of children and adolescents in a German representative sample: results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17(Suppl 1):71–81. doi: 10.1007/s00787-008-1008-x. [DOI] [PubMed] [Google Scholar]
- 3.Bhatia SK, Bhatia SC. Childhood and adolescent depression. Am Fam Physician. 2007;75:10–15. [PubMed] [Google Scholar]
- 4.Jane Costello E, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry Allied Discip. 2006;47:1263–1271. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- 5.Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44:972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 6.Cook MN, Peterson J, Sheldon C. Adolescent depression: an update and guide to clinical decision making. Psychiatry (Edgmont). 2009;6:17–31. http://www.ncbi.nlm.nih.gov/pubmed/19855857. http://www.pubmedcentral.nih.gov/articlerendr.fcgi?artid=PMC2766285. Accessed 21 Jan 2018. [PMC free article] [PubMed]
- 7.Costello EJ, Pine DS, Hammen C, March JS, Plotsky PM, Weissman MM, et al. Development and natural history of mood disorders. Biol Psychiatry. 2002;52:529–542. doi: 10.1016/S0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- 8.Brady EU, Kendall PC. Comorbidity of anxiety and depression in children and adolescents. Psychol Bull. 1992;111:244–255. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- 9.Small DM, Simons AD, Yovanoff P, Silva SG, Lewis CC, Murakami JL, et al. Depressed adolescents and comorbid psychiatric disorders: are there differences in the presentation of depression? J Abnorm Child Psychol. 2008;36:1015–1028. doi: 10.1007/s10802-008-9237-5. [DOI] [PubMed] [Google Scholar]
- 10.Keenan-Miller D, Hammen CL, Brennan PA. Health outcomes related to early adolescent depression. J Adolesc Health. 2007;41:256–262. doi: 10.1016/j.jadohealth.2007.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hasler G, Pine DS, Kleinbaum DG, Gamma A, Luckenbaugh D, Ajdacic V, et al. Depressive symptoms during childhood and adult obesity: the Zurich cohort study. Mol Psychiatry. 2005;10:842–850. doi: 10.1038/sj.mp.4001671. [DOI] [PubMed] [Google Scholar]
- 12.Guberman C, Manassis K. Symptomatology and family functioning in children and adolescents with comorbid anxiety and depression. J Can Acad Child Adolesc Psychiatry. 2011;20:186–95. http://www.ncbi.nlm.nih.gov/pubmed/21804847. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC143694/pdf/ccap20_3p186.pdf. Accessed 5 Feb 2018. [PMC free article] [PubMed]
- 13.Lundy SM, Silva GE, Kaemingk KL, Goodwin JL, Quan SF. NIH Public Access. 2010. pp. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLeod JD, Uemura R, Rohrman S. Adolescent mental health, behavior problems, and academic achievement. J Health Soc Behav. 2012;1845:482–492. doi: 10.1177/0022146512462888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization The world health report 2001. Soc Psychiatry Psychiatr Epidemiol. 2001;36:473–474. doi: 10.1007/s001270170010. [DOI] [PubMed] [Google Scholar]
- 16.Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Hughes CW, Carmody T, et al. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch Gen Psychiatry. 1997;54:1031. doi: 10.1001/archpsyc.1997.01830230069010. [DOI] [PubMed] [Google Scholar]
- 17.Emslie GJ, Heiligenstein JH, Wagner K, Hoog SL, Ernest DE, Brown E, Nilsson M, et al. Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial. J Am Acad Child Adolesc Psychiatry. 2002;41:1205–1215. doi: 10.1097/00004583-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Dolle K, Schulte-Körne G. The treatment of depressive disorders in children and adolescents. Dtsch Arztebl Int. 2013;110:854–860. doi: 10.3238/arztebl.2013.0854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.March J, Silva S, Curry J, Wells K, Faribank J, Burns B, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression. JAMA. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 20.March J, Silva S, Vitello B, TADS Team The treatment for adolescents with depression study (TADS) J Am Acad Child Adolesc Psychiatry. 2006;45:1393–1403. doi: 10.1097/01.chi.0000237709.35637.c0. [DOI] [PubMed] [Google Scholar]
- 21.Biddle S, Fox KR, Boutcher SH, Stephen H. Physical activity and psychological well-being. London and New York: Routledge; 2000.
- 22.Asarnow J, Emslie G, Clarke G, Wagner K, Sprito A. Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48:330–339. doi: 10.1097/CHI.0b013e3181977476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cipriani A, Zhou X, Del Giovane C, Hetrick SE, Qin B, Whittington C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet. 2016;388:881–890. doi: 10.1016/S0140-6736(16)30385-3. [DOI] [PubMed] [Google Scholar]
- 24.Pinna G. Fluoxetine: pharmacology, mechanisms of action and potential side effects. 2015. [Google Scholar]
- 25.Bridge JA, Iyengar S, Salary CB, Barbe RP, Birmaher B, Pincus HA, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment. JAMA. 2007;297:1683. doi: 10.1001/jama.297.15.1683. [DOI] [PubMed] [Google Scholar]
- 26.Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry. 2006;63:332. doi: 10.1001/archpsyc.63.3.332. [DOI] [PubMed] [Google Scholar]
- 27.Cooney G, Dwan K, Greig C, Lawlor D, Rimer J, Waugh F, et al. Exercise for depression (review) summary of findings for the main comparison. Cochrane Database Syst Rev. 2013;9:CD004366. doi: 10.1002/14651858.CD004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larun L, Nordheim LV, Ekeland E, Hagen KB, Heian F. Exercise in prevention and treatment of anxiety and depression among children and young people. Cochrane Database Syst Rev. 2006:CD004691. 10.1002/14651858.CD004691.pub2. [DOI] [PubMed]
- 29.Hughes C, Barnes S, Barnes C, Defina L, Nakonezy P, Emslie G. Depressed adolescents treated with exercise (DATE): a pilot randomized controlled trial to test feasibility and establish preliminary effect sizes. Ment Health Phys Act. 2014;6:1–32. doi: 10.1016/j.mhpa.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dopp RR, Mooney AJ, Armitage R, King C. Exercise for adolescents with depressive disorders: a feasibility study. Depress Res Treat. 2012;2012:1–9. doi: 10.1155/2012/257472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wunram HL, Hamacher S, Hellmich M, Volk M, Jänicke F, Reinhard F, et al. Whole body vibration added to treatment as usual is effective in adolescents with depression: a partly randomized, three-armed clinical trial in inpatients. Eur Child Adolesc Psychiatry. 2017:1–18. 10.1007/s00787-017-1071-2. [DOI] [PubMed]
- 32.Buckworth J, Buckworth J. Exercise psychology: Human Kinetics. Champaign; 2013.
- 33.Wittert GA, Livesey JH, Espiner EA, Donald RA. Adaptation of the hypothalamopituitary adrenal axis to chronic exercise stress in humans. Med Sci Sports Exerc. 1996;28:1015–1019. doi: 10.1097/00005768-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41:15–28. doi: 10.2190/PM.41.1.c. [DOI] [PubMed] [Google Scholar]
- 35.Dishman RK. The new emergence of exercise neurobiology. Scand J Med Sci Sports. 2006;16:379–380. doi: 10.1111/j.1600-0838.2006.00609.x. [DOI] [PubMed] [Google Scholar]
- 36.Krogh J, Rostrup E, Thomsen C, Elfving B, Videbech P, Nordentoft M. The effect of exercise on hippocampal volume and neurotrophines in patients with major depression-a randomized clinical trial. J Affect Disord. 2014;165:24–30. doi: 10.1016/j.jad.2014.04.041. [DOI] [PubMed] [Google Scholar]
- 37.Nabkasorn C, Miyai N, Sootmongkol A, Junprasert S, Yamamoto H, Arita M, et al. Effects of physical exercise on depression, neuroendocrine stress hormones and physiological fitness in adolescent females with depressive symptoms. Eur J Pub Health. 2006;16:179–184. doi: 10.1093/eurpub/cki159. [DOI] [PubMed] [Google Scholar]
- 38.Byrne ML, O’Brien-Simpson NM, Reynolds EC, Walsh KA, Laughton K, Waloszek JM, et al. Acute phase protein and cytokine levels in serum and saliva: a comparison of detectable levels and correlations in a depressed and healthy adolescent sample. Brain Behav Immun. 2013;34:164–175. doi: 10.1016/j.bbi.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 39.Zimmer P, Oberste M, Bloch W. Einfluss von Sport auf das zentrale Nervensystem—Molekulare und zelluläre wirkmechanismen. Dtsch Z Sportmed. 2015;66:42–49. doi: 10.5960/dzsm.2015.164. [DOI] [Google Scholar]
- 40.Mattson MP. Lifelong brain health is a lifelong challenge: from evolutionary principles to empirical evidence. Ageing Res Rev. 2015;20:37–45. doi: 10.1016/j.arr.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Knapen J, Vancampfort D. Evidence for exercise therapy in the treatment of depression and anxiety. Int J Psychosoc Rehabil. 2013;17(2):75–87. http://www.psychosocial.com/IJPR_17/Evidence_for_Exercise_Therapy_Knapen.html. Accessed 12 Feb 2018.
- 42.Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): facts and future directions. Int J Psychophysiol. 2009;72:67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 43.Plener PL, Grieb J, Spröber N, Straub J, Schneider A, Keller F, et al. Convergence of Children’s Depression Rating Scale-revised scores and clinical diagnosis in rating adolescent depressive symptomatology. Ment Illn. 2012;4:29–31. doi: 10.4081/mi.2012.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chan AW, Tetzlaff JM, Götzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:1–42. doi: 10.1136/bmj.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mayes TL, Bernstein IH, Haley CL, Kennard BD, Emslie GJ. Psychometric properties of the children’s Depression Rating Scale–revised in adolescents. J Child Adolesc Psychopharmacol. 2010;20:513–516. doi: 10.1089/cap.2010.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hautzinger M, Keller F, Kühner C. Das Beck Depressionsinventar II. Deutsche Bearbeitung und Handbuch zum BDI-II. München: Pearson; 2006.
- 47.Osman A, Kopper BA, Barrios F, Gutierrez PM, Bagge CL. Reliability and validity of the Beck Depression Inventory-II with adolescent psychiatric inpatients. Psychol Assess. 2004;16:120–132. doi: 10.1037/1040-3590.16.2.120. [DOI] [PubMed] [Google Scholar]
- 48.Delmo C, Weiffenbach O, Gabriel M, Stadler C, Poustka F, Bruhl B, et al. Kiddie-Sads-Present and Lifetime Version (K-SADS-PL) Screening Interview Vorwort der amerikanischen Originalversion: Diagnostic Interview Kiddie-Sads-Present and Lifetime Version (K-SADS-PL) 2000. [Google Scholar]
- 49.Döpfner M, Görtz-Dorten A, Lehmkuhl G. DISYPS- II, Diagnostik-System für psychische Störungen im Kindes- und Jugendalter nach ICD-10 und DSM-IV. Bern: Huber; 2008. [Google Scholar]
- 50.Aschenbach T, Rescorla L. Manual for the ASEBA school-age forms and profiles. Burlington: University of Vermont Research Center for Children, Youth and Families; 2001. [Google Scholar]
- 51.Trinkl M, Greimel E, Bartling J, Grünewald B, Schulte-Körne G, Grossheinrich N. Right-lateralization of N2-amplitudes in depressive adolescents: an emotional go/no-go study. J Child Psychol Psychiatry Allied Discip. 2015;56:76–86. doi: 10.1111/jcpp.12282. [DOI] [PubMed] [Google Scholar]
- 52.Faul F, Erdfelder E, Lang A-G, Buchner A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 53.Borm GF, Fransen J, Lemmens WAJG. A simple sample size formula for analysis of covariance in randomized clinical trials. J Clin Epidemiol. 2007;60:1234–1238. doi: 10.1016/j.jclinepi.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 54.Oberste M, Hartig P, Bloch W, Elsner B, Predel H-G, Ernst B, et al. Control group paradigms in studies investigating acute effects of exercise on cognitive performance–an experiment on expectation-driven placebo effects. Front Hum Neurosci. 2017;11 10.3389/fnhum.2017.00600. [DOI] [PMC free article] [PubMed]
- 55.Stothart CR, Simons DJ, Boot WR, Kramer AF. Is the effect of aerobic exercise on cognition a placebo effect? PLoS One. 2014;9:e109557. doi: 10.1371/journal.pone.0109557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mello AF, Juruena MR, Pariante CM, Audrey R, Price LH, Carpenter LL, et al. Depression and stress: is there an endophenotype? Rev Bras Psiquiatr. 2015;29(Supt l):1–12. [DOI] [PMC free article] [PubMed]
- 57.Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.MacPherson A, Dinkel K, Sapolsky R. Glucocorticoids worsen excitotoxin-induced expression of pro-inflammatory cytokines in hippocampal cultures. Exp Neurol. 2005;194:376–383. doi: 10.1016/j.expneurol.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 59.Hu W, Zhang Y, Wu W, Yin Y, Huang D, Wang Y, et al. Chronic glucocorticoids exposure enhances neurodegeneration in the frontal cortex and hippocampus via NLRP-1 inflammasome activation in male mice. Brain Behav Immun. 2016;52:58–70. doi: 10.1016/j.bbi.2015.09.019. [DOI] [PubMed] [Google Scholar]
- 60.Mondelli V, Cattaneo A, Murri MB, Papadopoulos AS, Aitchison KJ, Europe PMC Funders Group. Stress and inflammation reduce BDNF expression in first-episode psychosis: a pathway to smaller hippocampal volume. J Clin Psychiatry. 2014;72:1677–84. [DOI] [PMC free article] [PubMed]
- 61.Eyre HA, Papps E, Baune BT. Treating depression and depression-like behavior with physical activity: an immune perspective. Front Psychiatry. 2013;4:3. doi: 10.3389/fpsyt.2013.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kerling A, Kück M, Tegtbur U, Grams L, Weber-Spickschen S, Hanke A, et al. Exercise increases serum brain-derived neurotrophic factor in patients with major depressive disorder. J Affect Disord. 2017;215:152–155. doi: 10.1016/j.jad.2017.03.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
All Items from the World Health Trial Registration Data Set. (PDF 80 kb)
Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 Checklist. (PDF 129 kb)
Data Availability Statement
The data sets of this study will be made available by the corresponding author on reasonable request.


