Abstract
Medical Doppler ultrasound is usually utilized in the clinical adjusting to evaluate and estimate blood flow in both the major (large) and the minor (tiny) vessels of the body. The normal and abnormal sign waveforms can be shown by spectral Doppler technique. The sign waveform is individual to each vessel. Thus, it is significant for the operator and the clinicians to understand the normal and abnormal diagnostic in a spectral Doppler show. The aim of this review is to explain the physical principles behind the medical Doppler ultrasound, also, to use some of the mathematical formulas utilized in the medical Doppler ultrasound examination. Furthermore, we discussed the color and spectral flow model of Doppler ultrasound. Finally, we explained spectral Doppler sign waveforms to show both the normal and abnormal signs waveforms that are individual to the common carotid artery, because these signs are important for both the radiologist and sonographer to perceive both the normal and abnormal in a spectral Doppler show.
Keywords: Doppler ultrasound terminology, sonography, physics of ultrasound, spectral Doppler of common carotid artery
INTRODUCTION
Ultrasound is the term that describes the sound signal wave's pulse frequencies above the domain of real human hearing, and their publishing (propagation) in a medium. Diagnostic ultrasound in the medical field is a form that utilizing ultrasound power and acoustic features of the organs of human body or phantoms to produce an image from constant and moving tissue.[1] The usage of ultrasound into medical imaging field dates back more than 55 years and it launched was first with a therapeutic field rather than the diagnostic field.[2] The first article on medical imaging ultrasound was published in 1942 by Dr. Dussik at University of Vienna. This article displayed the transmission ultrasound of brain and many of researches done for medical ultrasound field.[3]
The sound is a mechanical power (energy) which travel or propagate during flexible (elastic) continuous medium by the rarefaction and compression of elements that compose it. Rarefaction is an area where the elements furthest from each other, whereas the compression is an area where the elements are closest together. The energy (power) traveling occurs when the signal wave front in the direction of power propagate, called as a longitudinal wave. The distance between both of rarefaction and compression or between each two spots which regenerate on the sinusoidal signal wave known as the wavelength (λ). In contrast, the quantity of times the signal wave fluctuates (oscillates) during a cycle count each second known as the frequency (f).[1] When the frequency exceeds 20KHz, the human cannot hear it, and this process called ultrasound.[4] The speed of sound relies on both the compressibility and density of the medium and variates largely with materials variation.[5] The relationship between the wavelength (λ), frequency (f), and the velocity (c) given by this formula (2):
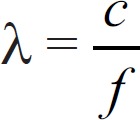 (1)
(1)
The probe or the transducer is a necessary component in an ultrasound system. The transducer has an ingredient that has the ability to produce ultrasound signal waves, and these signals occur when the electric current passes through the probe ingredient. This process called piezoelectric (PE) influence. Furthermore, the main function of the probe is sending ultrasound energy into body organs or into samples and then receiving the reflected signal echoes that may be processed via ultrasound unit into images displayed on a screen monitor. When a voltage utilized by PE element, this will produce a pressure signal wave. The ingredient utilized as a PE element made of crystal, like plastic and lead zirconate titanate which is the most common ingredient to be used basic components of an ultrasound probe are shown in Figure 1 In addition to the crystal which was described before, both of backing and matching materials are very significant components of the system. Matching layer is item situated between the PE material and the phantom sample or the patient. The acoustic resistance in matching layer is coming between PE material and the skin or the surface of the phantom sample, this help to produce a reflection of ultrasound power, then permits for larger energy of ultrasound to transporting through the tissues or blood vessels to produce images.[6] However, backing material, also called damping material, is placed behind the PE ingredient to reduce the pulse period. When the pulse period reduces, it becomes shortened, and this help to improve broadens bandwidth and resolution. The broadens bandwidth technique permits the probe to have a wide range of frequencies.[7] Choosing probes depend on the organ (structure) being tested and on the size of patient or phantom. Generally, the highest probable frequency should be applied because it will increase the resolution, while the lower frequency decrease the resolution and lead to increases the penetration.[8] However, linear probe with a frequency of more than 5 MHz is required in Doppler image scanning.[9,10,11,12,13]
Figure 1.
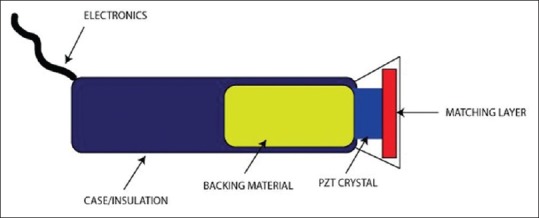
Basic components of ultrasound probe (transducer)
The ultrasound beam travels like a longitudinal signal wave from the probe surface area into the medium, and displays two beam models: a diverging beam (far field) and a converging beam (near field). However, both the frequency of emitted sound and probe diameter were determine the near-field length in unfocused single element probe.
The Doppler effect of sound is sometimes the common case in our lives. For instance, consider understanding and realizing the influence of the sound on the hearing, like a vehicle approaching and then go away from a listener. The pitch of sound increases when the car approaches then suddenly sound pitch decrease as the car moves away from the listener. The rising frequency or pitch of the sound waves displays the constant frequencies from the hear add to the known rise in frequencies from the velocity of the vehicle in motion toward the listener. When both the vehicle and listener are constant, the wave pulse frequency of the vehicle at eardrums is stationary. This principle of car and listener is identical to the principle of B-mode in an ultrasound system. In B-mode, both the source (probe) of the ultrasound pulse frequency and target tissue are nearly constant. Thus, the frequency pitch of the transmitting ultrasound pulse waves and also the frequency pitch of the returning signals echoes are identical.[14,15] No proportional motion from pulse to pulse when the flow is vertical (perpendicular) on the beam. Thus, the Doppler signal size based on many factors. The first one is, blood speed: as speed increases, the Doppler frequency also increases. Second, ultrasound frequency: rising ultrasound frequency will produce high Doppler frequency. Like in B-mode, when the ultrasound frequencies decrease, the penetration will improve. Finally, the angle of insonation: when the beam of ultrasound has much aligned toward the direction of the flow, the Doppler frequency will rise (the angle of insonation between the medical ultrasound beam and the blood flow direction becomes smaller).
Doppler ultrasound supply is an instrument, which it is using for measuring the blood speed and flow, also it is utilized in the research field and clinical field investigations to quantify the range and influence of arterial disease.[13] In Doppler imaging of the blood, the constant object usually is the probe, and the shifting reflectors that produce the returning signal echoes are originally the red cells.[15,16] The Doppler shift frequency or the Doppler-shift is known as the variation between the frequencies of transmitted and received of ultrasound waves echoes.[17] For example, moving of red blood cells at a velocity of 1 m/sec toward the vibration pulses transmitted by an ultrasound probe. 5 MHz is the ultrasound pulse frequency of the probe, 5 MHz is equal to 5 × 106 Hz. By applying the Doppler shift formula (see equation 2). The Doppler-shift is positive and is approximately 6490 Hz.[14] As in the former example, the Doppler-shift frequencies is in the field of human's audible frequencies and thus can be heard when operated through the speaker. However, the capacity of the ear to interpret signals is special as proof from the capacity to recognize one person's sound from another person's. Hearing sound constant to be utilized by expert operators in electronic analyses and shows.[18]
ΔFT=(2fo v cosθ/c) (2)
Where,
ΔFT: Shift Frequency or Doppler Frequency;
fo: Ultrasound probe Frequency (Hz);
V: The blood velocity;
Cosθ: Cosine Angle of the Insonation;
C: Speed Sound in Soft Tissue which is equal to1540 m/s.
When the velocity of sound of source (blood) is zero and the frequency of observer (probe or transducer) is constant, there is no Doppler shift in this case, or it is equal to zero and the wave pulse will be concentric in the center Vsource(blood)= 0. However, when the wave pulses transmitted through the motion between the blood and the probe, the wave pulse will be front of concentric and stay no longer, and the Doppler shift increase when the blood move approaches the transducer, and decrease when moving away from the transducer Vsource (blood)< Vsound. When the velocity of blood and probe are identical, the peak of transmitted signal wave reaches the probe with blood together Vsource(blood)= Vsound. Finally, the transmitted signal wave arrive to the probe after passing the blood at supersonic speed Vsource (blood)> Vsound [Figure 2].[15]
Figure 2.
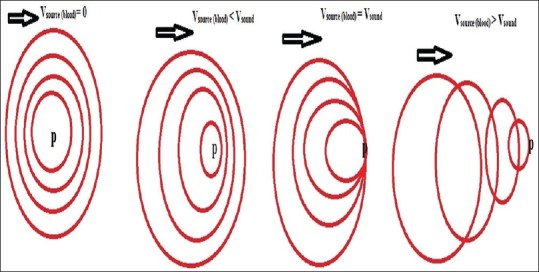
Group of images explaining the Doppler Effect
There are three essential levels of Doppler ultrasound that can be carried out, with any level adding data to the previous level. The initial level is the conventional scale mode or B-mode gray-scale scanning, in this level, no Doppler effect is used. The second one level adjusts a color Doppler examination region of interest (ROI). This level produces an image that displays the blood flow in the vessels. The final level adjusts a small examination area, named a sample volume or gate, along with a vessel of interest.[19]
TECHNICAL OBSERVANCE AND INFORMATION INTERPRETATION
Normal protocols contain common carotid artery (CCA) and Doppler ultrasound examination with a good-resolution linear array probe (5–15 MHz). Three manners should be utilized: B-mode gray imaging, color Doppler flow, and duplex imaging.
B-mode ultrasound imaging of blood flow
A gray-scale of an ultrasound image with two dimensions is called B-mode ultrasound image, and representing the boundaries of both organ and tissue in a slice over the body.[17] B-mode represent the brightness-mode due to all pixels in the image are strength power adjusted, that means the brightness-mode of each pixel is relative to the power strength of the ultrasound reflected from the identical structure within the organ body. In the field of medical ultrasound, B-mode imaging is emitting into the body in a group of short pulses usually 0.2 μs through duration period. However, to specify the diameter of a sample in B-mode ultrasound image, using the calipers which appear on the control panel of the ultrasound device. The depth of a reflecting sample can be studied by calculating the time trip between the sending of the ultrasound pulse and the receiving of the reflected signal wave.[20]
Color ultrasound Doppler imaging of blood
There are two ways for color ultrasonic imaging estimation: pulse wave (spectral Doppler) and color-flow modes. The spectral mode testing the blood speeds of particular arteries. Whereas, color-flow mode utilize color-Doppler signals overlie on a B-mode scan image of the artery to evaluate its vascularity. Both ways depend on the Doppler-shift frequencies. Thus, when the signal wave of blood cells (source) is constant or moving in a parallel direction to the probe, there is no variation between transmitted and receiving frequencies, and in this case, the color Doppler signals undiscovered. The positive Doppler frequency occurs when the source flow approaches toward the probe and the receiving signal frequency wave is higher than the emitting frequency. While, a negative Doppler signal frequency occurs when the blood cells move away from the probe, or, in other words, when the frequency of the emitting signal is higher than returning frequency.[14,15,21,22]
In the traditional Doppler spectral mode, an ultrasound probe array is worked to emit by an emitting ultrasound burst which is frequently fire at pulse repetition frequency (PRF), this PRF is usually in the unit of kilohertz range. However, the return back radiofrequency (RF) signals is discovered by the probe components and then formed into a receive signal beam by a beam former. In a modern (digital) system, the combined RF signal from each firing is demodulated by a demodulator into both its in-phase and quadrature (I/Q) elements. The (I/Q) elements were inserted (combined) over a particular time interval and then sampled. The combined interval and emitted burst length known as the length of sample or sample length or sample volume which determined by the user on the ultrasound device. The sample length pointer consists of parallel lines on both parts of the sample or arterial axis line. The sample length should be positioned within an arterial lumen, and the scale of the sample length size is typically between 0.33 and 0.5 mm of the luminal diameter.[23,24] This process effectively produces the Doppler signal backscatter from the sample length which should be low and <2.5 mm.[25] Then, the Doppler signal is cross over a wall filter which is should be low,[25] and its main function is to reject any noise in the signal caused by low frequency identical to constant or very slow-moving tissue, inclusive a part of the vessel wall (s).[12,23] The filtered products are then come into a spectrum.
As we mentioned before, that there are two ways for color ultrasonic imaging estimation. First, in spectral Doppler mode, the spectral sends beams pulsed ultrasound into the blood flow with a particular PRF. The PRF is usually between 64 and 128 A-lines, it resulted from sending and receiving ultrasound beams pulses in a particular direction. To measure the speed of blood flow at a particular depth, the A-lines represent the time-gated to take signals from a wanted depth. The diversities of blood flow speed are displayed as a graphical signal wave shape or image resulted by moving blood called spectrum. The spectrum appears on the spectrum window which represents the mix of Doppler frequencies existing in a particular sample of a vessel during a short period and displaying the normal flow of blood at a regular velocity[17] [Figure 3]. When the arteries are normal, the flow acceleration in systole is fast, thus, the peak speed arrives within a few hundredths of a second after the contraction stage of ventricular chamber begins. Furthermore, blood in the middle of the artery shifts quicker than blood at the peripheral side, which is known as laminar flow. The erythrocytes move at an identical speed when the flow is laminar.[23] This spectrum supplies three functions, time-average maximum velocities (TAMV or mean velocity [Vm]), maximum velocities values as peak systolic velocity (PSV or Vp), and end-diastolic velocity (EDV or Vd). Initially, the PSV is the highest spot along the length region of the spectrum, whereas EDV is the finish spot of the cardiac cycle. TAMV is the highest average speed values. Pulsatile index (PI) and resistance index (RI) are calculated using the proportion of the three velocities measurements (TAMV, PSV, and EDV) (see equation 3 and 4).[23] To make an accurate spectral graphic in real human and animal, it is critical to put the sample gate (sample length) Doppler into an artery. Ordinarily, this may be difficult considering the vessels diameters and the human or animal mobility. however, when the phantom used instead of a real human or animal, the trustful of spectral graphic increased because the phantom is fixed and not moveable.[15,26] In addition, the direction of blood flow is related to the place of the spectrum in relation to the baseline of the screen, signal shapes above and under the baseline, respectively, represented that the blood cells moving toward and away from the probe. However, adjustment of the Doppler angle is required to measure blood speeds. Doppler angle is the angle of crossing of the ultrasonic signal pulse with the direction of moving blood cells. To make a precise spectrum a Doppler angle of the range between 30° and 60° is required[9] because the function of cos angle has curve above these angles and there is risk of errors and low accuracy in angle correction.[17,27] When the Doppler angle is 0°, the top Doppler shift will be done since the cosine of 0° is 1. On the other hand, when the Doppler angle is 90°, no Doppler shift (no flow) will be listed, since the cosine of 90° is 0.[27] It has been displayed that the peak systolic speed values can change with the Doppler angle applied. Generally, smaller angles will produce lower speeds.[28]
Figure 3.
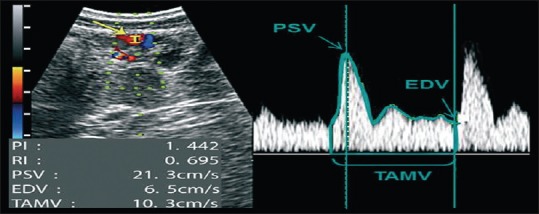
Spectral Doppler evaluation of uterine artery
PI = (PSV/EDV)/TAMV (3)
RI = (PSV/EDV)/PSV (4)
Second, color-flow mode, which provides a direct qualitative estimation of the blood flow to various tissues and organs. The vascularity of the sample is evaluated subjectively taking into account the extension of the sample (artery) with color pixels through a continuous real-time test. Compared with the spectral mode, color-flow mode is faster, simpler, and more effective way for evaluation than the spectral mode. The modern Doppler devices show two various modes of color-flow scanning: color-flow and power-flow modes. The conventional color-flow mode utilizes two special colors (Red and Blue). Generally, the difference between red and blue colors, used to appear the vascular blood perfusion of the sample (artery). Furthermore, indicate the direction of the blood relation to the probe. By convection way, red color specks represent blood flow moving toward to the probe, whereas blue color specks indicate red blood cells moving away from the transducer. However, in power-Doppler flow mode, the motion of blood flow is graduated utilizing a single color, which differs according to the strength of the Doppler signals. Power-Doppler imaging has major sensitivity to slow (weak) blood flow, and the power-Doppler mode is not related to the Doppler angle. Thus, power Doppler mode can betterment the estimation of vessels with tiny (small) diameters and weak blood flow.[14,15,29] However, color gain indicates the amplification of information flow to improve the photograph of flow.[14] Color gain (the “gain” knob on the ultrasound device) should be highly adjusted without showing background color noise. The color speed (velocity) is the scale of flow speeds that are depicted in color Doppler ultrasound technique.[23] If the speed scale (the “scale” knob on the ultrasound technique) adjusting is lesser than the flow speed of the artery, aliasing artifacts will exist. The sonographer can reveal the color flow within an arterial lumen by rising the gain or reducing the scale. In addition, when the gain decreases, the color flow artifacts will decrease.[12]
Duplex imaging
Duplex imaging gathers both the B-mode and pulsed signal wave Doppler (spectral Doppler).[9] The probe is identical to a B-mode imaging probe but with a little group of the probe elements applied to send and discover pulsed Doppler signals. The residual elements utilize the B-mode imaging. This mechanism lets the blood vessel to be scanned and the depth of sample is adjusted by an option on-monitor screen cursor called the “Doppler gate.” The Doppler gate width can be changed to alter the depth range.[30] A second mark (cursor) on screen monitor is referred to the “angle.” The Doppler gate with this angle can be aligned with the direction of the vessel to produce a calculation of the insonation angle with the blood flow thus that speed of blood flow can also be calculated through applying the Doppler formula. Duplex Doppler scanning technique also helps to measure the volume flow which is performed through measuring the lumen diameter on the B-mode image, the highest flow in systole stage, and calculation of the cross-sectional region. When the four cardiac cycles or gear pump in flow phantom are completed, the average flow velocity can be calculated by Doppler spectrum. The device then calculates the volume flow automatically.[17,31] However, the expression is generally utilized by indicating clinicians when ordering a scanning with the spectral Doppler effect, which mechanically would be further precisely termed as a triplex Doppler since it includes all of gray-scale (B-scan), color Doppler, and spectral Doppler.[32]
MOST SIGNIFICANT COMMON INFORMATION THAT OBTAINED BY DOPPLER ULTRASOUND TECHNIQUE
Pulsed wave Doppler systems imaging
Pulsed wave (PW) Doppler imaging has the ability of measuring tissue and blood speed from a limited sample volume, range of the time should be known from the probe face. Hence, the additional information regarding the position of the blood scattered which is the main feature of pulsed systems over continuous wave systems. As those PW systems can do this, the pulse of ultrasound is transferred in low bursts, like the traditional B-mode imaging, and the system then converts to receive mode. The distance resulted from switches and converts is the time between the transmitted and received echo with knowing the speed of sound. The main disadvantage that appear with PW Doppler, that the PW Doppler is an inherent, and is not a product of discretization for digital analysis.[27,33] Since only continuous waves are the goal to Doppler shifts, the pulsed wave cannot measure frequency shift via Doppler technique. Hence, PW systems send many of sequential impulses and the alteration of time (or phase) in the received signals is applied to estimate the Doppler frequency. Usually, 8–32 pulses are emitted; the tradeoff is between precision (more pulses allow more credible estimate allowed by more pulses) and temporal resolution (it takes longer time to emit extra pulses).[34]
Determination the speed of blood flow
The mathematic equations for alteration from both the Doppler frequency and the angle of blood flow speed in the tiny sample volume specified by the sample length are considered as a case for debate of the physics principle of medical ultrasound.[35] The top border of the speed range is adjusted by the sonographer or operator, to reduce artifacts and to improve the signal show. The changes in both Doppler-shift (effect) frequencies and pulse signal wave amplitudes are presented in the shape of a sine pulse wave, this signal waveform refers to a cardiac cycle. Some equipment automatically marks the line of the specified cardiac cycle utilizing built-in algorithms, also in some equipment, the cardiac cycle is marked manually. PSV or PV is the highest spot over the length region of the spectrum, whereas EDV or EV is the finish spot of the cardiac (heart) cycle. TAMV or TV is the highest speed values average of the peak. These measurement values are calculated from suitable points or spots of the spectrum and offered numerically (as a numbers or digits) on the monitor of most equipment. The pulsatility can be low when the Doppler wave appear with a wide systolic outline and gradually reduce toward the direction of the end-diastolic profile. This wave signal refer to that the vessels provide a vascular bottom that have very low resistance.[18] High-pulsatility or high marginal resistance appears when the Doppler wave signal with sharp (severe) peak systolic outline profile and an inverted or lost diastolic profile.[36] Moderate-pulsatility Doppler's shape almost occurs between the low- and high-resistance models. The region under the profile of the greater amounts of the spectral show is refer to the window [Figure 3]. The information which appears on the window border is an index of several simultaneous Doppler frequency shifts of the signal and happens when a lot of the width range of the artery is taken for analysis, or the blood flow is confused. However, if the blood flow in the vessel is influenced by any turbulence, so the Doppler spectral fills in overall the window border and may overtake the fill value in border which is generating from the laminar flow.[36] Flow trouble or the flow in several directions produces in a vast range of the Doppler frequency shifts.[14,35]
Doppler indices (peak systolic velocity, end diastolic velocity and time-average maximum velocities) of blood
Blood flow in the vessel is influenced by two main factors, first one is the resistance given by the wall of vessel and second one is the pressure variation (blood vessel elasticity) between the ends of the vessel. While the first agent is specified by heart function and then, the proportional place of the artery vessel in the cardiac circulatory system, the second factor based on the main physiologic state of the artery vessel and the desire for the blood. Thus, any normal artery vessel in the human organs has a special flow model that is appear in Doppler spectral waveforms acquired with the medical Doppler ultrasonography (US), and hence, this indicate to both the physiologic and the anatomic need of the vessel. There are two main equations for calculating the PI and the RI from appeared spectral (See equations 1 and 2). Both the pulsatility index and the resistive index provide input about both the resistance and blood vessel elasticity or blood flow that has no ability to be acquired from measurements value of the velocity alone. The influences of difference in artery vessel angulation and diameter are not taken into account in the calculation of these indices. In other words, the PI and the RI calculation method are not affected by the angle of Doppler flow. The PI and RI can be applied to represent both the elasticity and resistance of downstream blood vessel. The best way to calculate the PI is through subtracting the end diastolic velocity EDV from the peak flow velocity PSV, then dividing by the Vm calculated; while the RI is calculated utilizing the peak systolic velocity as the denominator or divisor.[17,19,36,37,38] Measurements of PSV, ESV, and systolic-diastolic S; D or S/D velocity ratio are significant since the peak systolic velocity is the primary Doppler parameter to be abnormal in stenosis.[17]
The alternative choices of Doppler speed measurements are the Doppler indices. They are particularly valuable when sampling tiny, tortuous vessels and not straight part to evaluate the Doppler angle. Indices are proportions of speed measurements and thus are separate from the Doppler angle. Furthermore, the Doppler indices are explainable and able to be related to the hemodynamic, proximal (downstream) to the degree of the arterial examination. They provide both of the researcher and the clinician with conclusions and deductions on an obstacle proximal to sampled zone and on size of distal artery perfusion of a tissue or organ provided by the artery vessel. On this basis, indices functions can be deemed, that it is able to determine flow volume and the blood speed in the providing artery. Thus, the Doppler indices are calculated and then offered numerically through the device [Figure 3]. They are calculated and computed from three values for PSV, EDV, and TAMV, as resulted from the spectrum power. The relationship between the RI and both soft tissues in the body and the range of vascular artery perfusion are inversely related. Hence, when the resistance increase, or RI increase, the perfusion will decrease. Furthermore, the relationship between the pulsatility index (PI) and the perfusion is also inversely related.[14] Knowing of peak systolic velocity threshold is the greatest significant factor for vascular stenosis diseases.[39,40,41,42]
Blood flow detection, direction, and velocity profile
Although that the Doppler shift frequency evaluated, but this does not immediately measure the blood speed. A vast range of hemodynamic data can be generated by Doppler spectral ultrasound. Such as, existent of the blood flow, the trend of flow, and speed of flow. First, flow detection. Determination of the existence of blood flow is one of the most utilizes of medical Doppler ultrasound. The detection of presence of blood flow via two-dimensional color flow map with duplex Doppler. However, caution should be taken into account when interpreting failure to discover the Doppler frequency shift as in these situations the flow may be existent but not within the sensitivity range of Doppler device. Second, flow direction. The demodulation of the mechanism allows locating the flow direction. Two types of flow direction, forward and backward or reverse, which are shown on the opposite part (side) of zero baseline. The flow direction of the blood in the vessels provides both clinicians and researchers with important hemodynamic data and information. The direction of the blood flow registered via Doppler flow scanning may differ with considering the place of the medical ultrasound probe and angle of the transmitted ultrasound beam. The blood flow direction is known as antegrade (flow would be in toward direction) when the flow direct with normal circulation and the spectral waveforms above the baseline, while the retrograde (flow of blood would be in the adverse direction) when it is against normal circulation and the spectral waveforms below the baseline. In addition, both the antegrade and the retrograde may be away or toward the probe.[19,36] Finally, flow velocity profile. The Doppler spectral form range may refer to the flow velocity profile, so the spectral can be broadening when the spectral range is broad or wide, but the spectral can be narrowing when the spectral range is thin or slim.[43,44]
When the spectral narrowing this typically refer to a plug or flat blood velocity since the blood is moving at identical speed, this case also usually can be shown in large vessels. In addition, the spectral narrowing is noticeable when the size or volume of sample is less than the lumen. In contrast, the spectral broadening is observed with parabolic flow where the blood flows at a wide range of velocity and make a broad range of Doppler shift.[43] However, the main functions of Doppler device parameter it were concluded in Table 1.
Table 1.
Main functions of Doppler device parameter
| Name of Doppler device parameter | Main functions |
|---|---|
| Mean velocity evaluation | This exam supply evaluation of the precision of the Doppler system’s evaluate of the mean Doppler scattered speed. In addition to the precision of the colour Doppler evaluate of the mean scattered speed |
| Range gate | Helps reveal blood flow signal wave |
| Sample volume or sample length | This exam evaluate the sensitivity of range gate to make sure if it is extreme sensitive at the centre position of the gate |
| Maximum velocity precision | This exam supply evaluation of the precision of the Doppler system’s evaluate of the maximum Doppler scattered speed. In addition to the precision of the reveal the degree of arterial narrowing or stenosis |
| Lowest detectable speed | This exam supply evaluation of the lowest speed that it is likely to show unambiguously |
| Highest detectable speed | This exam supply evaluation of the highest speed that it is likely to show unambiguously on both the colour Doppler image or on the PW Doppler spectrum. The highest speed with some diseases or stenosis may be reach up to 500-600 cm/s and can show this speed on the spectrum without aliasing |
| Spectral broadening | This exsam supply evaluation of the spectral Doppler broadening which cause by range of angles |
| Flow direction | This exam supply ability of the differentiate between flow towards and away from the probe |
| Angle correction | This exam supply ability to measures the accuracy of the angle correction the device |
| Wall filter | This exam remove intense signals from the vessel wall motion |
Source from: Browne, J.E., A review of Doppler ultrasound quality assurance protocols and test devices. Physica Medica, 2014. 30(7): p. 742-751. PW: Pulsed wave
Pulse repetition frequency in medical Doppler ultrasound
Frequency of ultrasound signal waves may be constant for sole-frequency probes and may be planned by the user for several frequency probes. The energy of the signal waves transmitted from the probe as well may be planned by the user to change the scanner sensibility in some styles, this control or plan process is called the voltage amplitude, output, or acoustic power different models. When the power increases, the signals'waves become weak, and this makes assessing signals'waves. The probe sends ultrasound signal waves in the form of pulses to let the time for receiving of the echo that return before another wave pulse is emitted. In most equipment, the Doppler PRF is monitored by rising or reducing the field range of speeds to be sampled. When the significant vessels of study are close to the probe or the blood flow is high, so the setting of high PRF is required. In contrast, when the significant vessels of study are far away from the probe or the blood flow of vessels is slow, the setting of low PRF is required.[14,45]
Aliasing artefact
Aliasing artifact is an inexact show of spectral and color Doppler speed and takes place when the speed range exceeds the scale ready to show it. The highest speed scale is restricted by the number of US signal pulses per second that can be emitted and received by the probe. Precise description of frequency shifts demands a scale that is two times as big as the maximum shift (called as the Nyquist limit, when the speed of blood flow exceeds 1/2 the PRF).[46] If the scale is so tiny, big shifts exceed the ready range and are shown as several tiny shifts. For spectral flow across the probe, the speed peak is cut off at the upper part of the scale and the lost part is written from the lowest part of the scale back toward the upper. The idea of a solution to spectral aliasing artefact is to decline the baseline or raising the speed scale, or reducing the Doppler frequency shift by raising the Doppler angle insonation.[46,47]
Phasicity against phase quantification
The Doppler spectral waveform has phasicity, which is made by the cardiac cycle that produce both the velocity and acceleration as a phasic blood flow, then the blood flow of samples shows as a phasic waveform. However, there are four types of phasicity. nonphasic waveform, which occurs when there is a constant flow or no acceleration or velocity, and the pulse waveform is smooth and flat in shape. Aphasic waveform, which occurs when there is no velocity, no phase, and no flow. Phasic waveform, which occurs when there is moderate ripple (superficial slopes and a tiny vertical range between inflections). Finally, “pulsatile” waveform, which occurs when there is clear ripple (steep or decline slopes and a wide or broad vertical range that placed between inflections) [Figure 4].[19] However, conventionally, radiologists have explained phases in word of acceleration alterations or inflection spots, relied on the notice that inflection spots produce audible (heard) sounds at medical Doppler ultrasound. According to this method, the flow manner is qualified as “monophasic” when there is a low pulsatility waveforms and it is flow usually in forward direction, “biphasic” when there are two sounds heard through each cycle or medium pulsatility Doppler waveforms are distinguished by both sharp and tall systolic peaks with direct forward flow throughout the diastole, and as “triphasic” when there is three sounds are heard through each cycle or high great pulsatility Doppler waveforms that have narrow, long, and sharp systolic peaks, a short flow reversal (under baseline) and a forward flow phase.[17,48]
Figure 4.
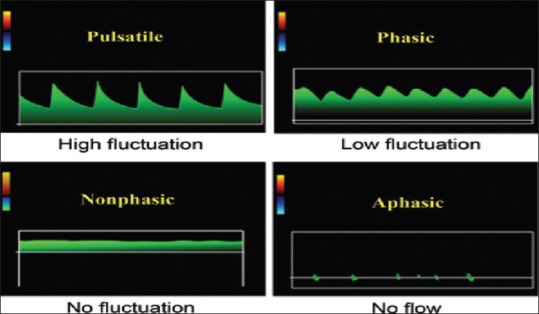
Phasicity, graphs clarify the different waveforms. The expressions terms utilized to describe the grade of waveform ripple empirically describe the speed and acceleration features of the waveform. Keep in mind that all of pulsatile, phasic and nonphasic flow waveforms all of them have Phasicity [19]
COMMON CAROTID ARTERY DOPPLER ULTRASOUND
Indications for common carotid artery sonographic examination
People who elected for estimation of CCA stenosis can be divided into two main groups: symptomatic group (which is consist of patients with neurologic incidents such as, patients with transient ischemic attack, amaurosis fugax, and a minor stroke) and asymptomatic group (which contains patients with cervical bruit, endarterectomy, and neck mass).[49,50,51,52] Concerning CCA sonography for examination before major cardiovascular operation, in a modern study which done by Ascher et al.[53] on several numbers of patients who subjected to open heart operation and pre surgery CCA duplex sonography, that the most important risk factor of CCA disease is the patient age. They decided that CCA examination before coronary artery surgery (open heart) should be fully recommended for all older patients (more than 60 years), but for younger patients (<60 years) with two or extra major risk factors: diabetes, smoking, and hypertension.
Spectral analysis of common carotid artery
The spectral shows in CCA that the system is examined cm/s instead of kHz frequency shift.[54] Measurements of velocities should be applied exclusively through testing of the CCA for several reasons: First one, speed values are naturally more precise than frequency shift measurements, due to the “Doppler angle” between the probe line and the flow direction should be known to change frequency shift to velocity. The Doppler shift differences in direct relationship to the Doppler angle, since the Doppler angle is unsteady due to period-to-period difference in the alignment of the medical Doppler probe proportion to the artery vessel lumen. For this reason, measurements of Doppler frequency or Doppler shift may change from site-to-site in the vessels with a regular flow. Second one, speeds (velocities) measurements are global standardization of flow parameters.
The blood flow of CCA is distinguished by low flow resistance because around 70% of blood flow in CCA is transmitted to the internal carotid circulation. If there is an obstruction in CCA, so the waveform supposed to be high pulsatility and an amplitude of waveform will reduce because of decreasing of blood flow inside the CCA. The best and simplest successful method to interpret and explain CCA pulsatility is to match visually the pulse waveforms registered on the screen monitor. In normal CCA, the flow shapes should be uniformly and should have flow over diastole. However, when the occlusion or the obstruction exists, the asymmetrical flow in diastole will appear.[55] The flow velocity through the artery will increase if there is no obstruction in CCA and the pulsatility is high. In this case, high resistance features will appear symmetrically or uniformly in the CCA waveforms; moreover, with infrequent exceptions, the diastolic of the blood flow will stay above (over) the zero baseline.
The domain, site, anatomy, and characteristics of the CCA should be recorded first with gray-scale imaging using B-mode.[17] Using color Doppler imaging is necessary to discover the regions of defect blood flow which need Doppler spectral analysis. The speed of blood flow through the proximal, mid, and distal CCA should be measured, and spectral Doppler analysis of the PW should be carried out.[56] The physical challenges will be minimal since we are dealing with phantom or with the fixed sample.[57] duplex Doppler scanning technique in CCA also helps to measure the volume flow which is performed through measuring the lumen diameter on the B-mode image, the highest flow in systole stage, and calculation of the cross-sectional region. When the four cardiac cycles or gear pump which take place instead of heart inflow phantom are completed, the average flow velocity is calculated by Doppler spectrum. The device then calculates the volume flow automatically.
The Doppler angle of CCA should be <60°,[17,58] because if the angle of CCA is more than 60°. The measurements are less likely to be precise.[9] In other words, to recognize why the Doppler angle should be lower than 60°, one needs to understand how the Doppler angle is utilized in the calculation of blood flow velocity. When the Doppler angle increases from 0° to 60°, Cos angle decreases from 1 to 0.5; while, when the Doppler angle increases from 60° to 90°, Cos angle decreases from 0.5 to 0.[19] The best angle of effectiveness is in range 45° ± 4°. Regular utilize of an appropriate Doppler angle of effectiveness for speed measurements in the CCA decreases errors in speed measurements regarding the difference in the Doppler angle. The most popular error resulted by the operator is that improper alignment of the spectral Doppler angle of effectiveness with the trend of the blood flow.[57]
The best place of the sample length (sample volume box) or (sample gate) in normal CCA artery vessel is in the middle of the lumen in parallel direct to the artery vessel wall, while in an abnormal CCA it should be in parallel form to the trend of the blood flow. The sample length should be located away from the vessel wall, to avoid the artificial spectral broadening. The broadening of spectral Doppler results from several factors such as trouble in the blood flow, increase in Doppler angle, increase in sample length (volume) box more than 3.5 mm, high PW Doppler gain adjusting and sample length (volume) box located near to the vessel wall.[19,59] The size of the sample length (volume) box is usually preserved between 2 and 3 mm. The Doppler signal will be lost when the sample length is too small (1.5 mm). However, the degree or level of spectral Doppler broadening is relating to the intensity of blood flow trouble and extent of the stenosis.[17,44,57,60] Information or data for the spectral waveform is gained from a tiny (typically from 2 to 4 mm) sample length that is positioned in the center of the artery vessel by the operator.[19]
The color box (also called as the Doppler sampling window) is sited above the artery vessel to be interrogated. Moreover, the volume of the color window set to contain all ROI. Modification of the Doppler angle of effectiveness can be obtained by altering pre-set color box Doppler angles from all directions like left to center or right, also angling the probe to make sure that the spectral angle of effectiveness is lower than 60°. While the scale of color velocity (speed) is the most significant factor of the CCA ultrasound color Doppler setup.[17] The scale of color velocity is a sonographer-determined domain of velocities which needs adjustment, similar to the window border and degree of a gray-scale image. Since it is not equivalent to the PRF, and hence, the relationship between the PRF and the velocity scale is a proportional relationship. There is an inverse relationship between the PRF and the period between emitted pulses, so when low color speed scale is applied, the image frame rate may look like slow.[37,61] When the color velocity scale is adjusted below the level of the Vm of the blood flow, the aliasing artefact during the artery vessel lumen will appear.[62] In contrast, when the color velocity scale is adjusted sufficiently higher than the Vm of blood flow, the aliasing artefact will disappear, but the stenosis missed. The area or ROI should be re-estimated by applying very low color velocity adjusting (15 cm/s) to improve discover of the trickle flow. In a normal CCA ultrasound scanning, the scale of color velocity should be adjusted at a range of 30–40 cm/s.[57] However, the control of color or Doppler gain must be adjusted so that color only attains the intimal surface of artery vessel. When the color gain adjusting is very low, the small flow may go undiscovered. When a high color gain adjusting is used, “bleeding” of the color that covers the vessel wall and surrounding the tissues may restrict the vision of the vessel plaque surface then may make an incorrect arrangement or position of the Doppler angle modification with the direction of the blood flow through the scanning of a PW Doppler.[28] The thickness of the intima (innermost coating or membrane) of vessels should at all times be carried out on a gray-scale image.[57]
The thickness of the intima-media of the CCA is a measurable indicator of the existence of some abnormalities. The longitudinal vision of the normal CCA wall shows two almost parallel echogenic lines; both the inner (internal) and the outer (external) lines. The internal line shows the interface of the lumen-intima, while the external line shows the interface of the media-adventitia. The collective thickness of intima and media is the distance between them.[63] The reflections of the lumen-intima should be thin, fine, straight, and parallel to the adventitial layer.[64] The measurement of the intima-media thickness of the CCA necessary to know if the presence of stroke or atherosclerosis.[62,65,66] Measurements of intima-media thickness should be acquired from a gray-scale image, but not from a color Doppler image. Thus, we advise applying of the linear probe with higher-frequency more than 7 MHz with structure and consistent imaging to minimize the near-field artefacts.[67] High values of the intima-media thickness have also resulted in a physiological influence of aging.[68] The normal value of intima-media thickness is <1 mm.
The study of the plaque forms or morphology, like the surface exterior, the existence of ulceration, echogenicity of the plaque, also the existence of the plaque and the stenosis, is significant for estimating future of the cardiovascular events.[69] Generally, it is highly recommended to make the depiction of the plaque form from a grayscale image through CCA Doppler US examination. The description should contain surface exterior, the existence of ulceration, echogenicity of the plaque, also the existence of plaque and stenosis. On B-mode imaging, the echogenicity of the plaque supports to grade them as low, medium, or highly echogenic, and in that way determined the kind of the plaque. To distinguish a calcified from non-calcified plaques by its appearances as homogeneous or heterogeneous appearances.[17] There are three descriptions of the echogenicity of the plaque: first, one is echogenic plaque and second is isoechoic plaque and Finally, echo lucent plaque, or heterogeneous plaque. When the echogenicity of the plaque is similar to the intima-media complex, thus the plaque morphology is an isoechoic plaque. When the echogenicity at the surface of the plaque with depression by more than 2 mm so the plaque has ulceration.[62]
Normal velocity of blood in the CCA is typically between 25-45 cm/s. Thus, high blood flow (>135 cm/s) in CCA caused by high cardiac output or high velocities flow by a gear pump. The systolic peak must be measured after a uniform beat. Measurements of PSV, ESV, and systolic-diastolic S; D or S/D velocity ratio are significant since the peak systolic velocity is the primary Doppler parameter to be abnormal in stenosis.[17] A normal PSV range in CCA should be nearly 60–100 cm/s or 78–118 cm/s or <125 cm/s, above this range there may be some stenosis or obstruction occur.[9,38,70] A normal EDV range in CCA should be nearly between 20 and 32 cm/sec, the RI between 0.72 and 0.84 cm/s, and PI 0.98–1.94 cm/s.[38,71] The ordinary normal speed (velocity) of the CCA is between 30 and 40 cm/s (30–40 cm/s).[62] Usually, a PI realized as very high resistance, moderately high resistance, then high resistance, low resistance, and very low resistance when PI >2, between 1.7 and 1.9, between 1.2 and 1.6, between 0.6 and 1.1, and <0.6, respectively.[36] In other words, the waveform of the high speed of end-diastolic blood flow that indicates an extra steady blood supply over an entire cardiac cycle and lower resistance in the downstream vasculature, when a PI <1.2 and a diastolic/systolic ratio >25% shows low resistance in the downstream vasculature. Moreover, when a PI <0.6 and a diastolic/systolic ratio >50% (>2.0) shows very low resistance. However, the waveform of low speed of end-diastolic blood flow that indicates higher resistance in the downstream vasculature. When an RI in the range >0.7 or PI in the range >1.2 indicates to as a high resistance waveform.[36] Normally, the waveforms of the CCA supposed to be low resistance RIs ranging from 0.55 to 0.7 due to overbalance of carotid flow going into the internal carotid artery.[32] In addition, the systolic peaks (PSV) of the CCA is moderately broad, also the quantity of flow throughout diastole is moderate too.[63]
Limitations of detection of carotid artery stenosis using spectral Doppler ultrasonography
Tortuosity of carotid artery due to minor coiling and twisting to aggregation may transfer a high peak velocity in the carotid artery. For instance, the loss of plaques like an origin of raised velocities should be certain on both the gray and color flow scale imaging. Furthermore, the plaques that calcified in a heavy form may work as a barrier to the medical Doppler ultrasound waves, also, it may lead to posterior acoustic shadowing. Thus, this acoustic shadow allows the concerned segment unable to be reached to gray scale and medical Doppler ultrasound examination. In the existence of a peripheral calcified plaque, the flow styles directly distal to the trauma or the lesion must be noticed: perceivable stenosis should be excluded when the blood flow stays normal or moderately troubled.[72] The peak systolic velocity values of the carotid artery are less credible when differences in cardiovascular physiologic cases are existing, like low or high cardiac output, aortic artery abnormalities and hypertension.[73]
CONCLUSION
Recently, spectral Doppler medical ultrasound has grown to be a full portion of diagnostics across a diversity of medical specialties. Spectral Doppler ultrasound was utilized to separate normal blood flow from abnormal blood flow in almost all parts of the body. However, each artery or vessel into the body has its own individual normal sign waveform that distinguishes it from pathologic sign waveform. Thus, it is very significant to know both the normal and abnormal sign waveforms when estimating for malformation with Doppler ultrasound. Moreover, duplex and color Doppler ultrasound are the initial imaging testing done for the diagnosis the stenosis in the CCA with respect to cost-effectiveness and its dual capacity to estimate the hemodynamic and morphologic abnormalities. A united protocol of testing, experience among sonographer, specialists of diagnostic imaging, and quality assurance are very important to guarantee reliable results. In spite of duplex imaging cannot exactly realizes the percentage of stenosis diameter, some of stenosis diameters able to be achieved with known diagnostic strata. However, diagnosis the CCA by Doppler ultrasound is more effective, less cost, and less harmful than computed tomographic angiography, and magnetic resonance angiography.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This research study was supported by Prof. Dr. Mohammad Zubir Matjafri. We thank our colleagues from (Universiti Sains Malaysia, Medical Physics and Radiation Science department) who provided insight and expertise that greatly assisted the research, although they may not agree with all of the interpretations of this paper.
REFERENCES
- 1.Bushberg JT, Boone JM. University of California-Davis: Lippincott Williams & Wilkins; 2011. The Essential Physics of Medical Imaging. [Google Scholar]
- 2.Jensen JA. Medical ultrasound imaging. Prog Biophys Mol Biol. 2007;93:153–65. doi: 10.1016/j.pbiomolbio.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 3.Brant WE, Helms CA. Fundamentals of Diagnostic Radiology. University of Virginian: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 4.Colquhoun K, Alam A, Wilson D. Basic science: Ultrasound. Curr Orthop. 2005;19:27–33. [Google Scholar]
- 5.Lutz H, Buscarini E. Manual of Diagnostic Ultrasound. Vol. 2. Slovenia: World Health Organization; 2013. [Google Scholar]
- 6.Jakowski JD. The basics of sonography and ultrasound terminology. Pathol Case Rev. 2013;18:5–11. [Google Scholar]
- 7.Fischetti AJ, Scott RC. Basic ultrasound beam formation and instrumentation. Clin Tech Small Anim Pract. 2007;22:90–2. doi: 10.1053/j.ctsap.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Sanders RC, Winter TC. Lippincott Williams & Wilkins; 2007. Clinical sonography: A practical guide. [Google Scholar]
- 9.Gerhard-Herman M, Gardin JM, Jaff M, Mohler E, Roman M, Naqvi TZ, et al. Guidelines for noninvasive vascular laboratory testing: A report from the American Society of Echocardiography and the Society for Vascular Medicine and Biology. Vasc Med. 2006;11:183–200. doi: 10.1177/1358863x06070516. [DOI] [PubMed] [Google Scholar]
- 10.Zhou X, Kenwright DA, Wang S, Hossack JA, Hoskins PR. Fabrication of two flow phantoms for Doppler ultrasound imaging. IEEE Trans Ultrason Ferroelectr Freq Control. 2017;64:53–65. doi: 10.1109/TUFFC.2016.2634919. [DOI] [PubMed] [Google Scholar]
- 11.Ramnarine KV, Anderson T, Hoskins PR. Construction and geometric stability of physiological flow rate wall-less stenosis phantoms. Ultrasound Med Biol. 2001;27:245–50. doi: 10.1016/s0301-5629(00)00304-5. [DOI] [PubMed] [Google Scholar]
- 12.Hwang JY. Doppler ultrasonography of the lower extremity arteries: Anatomy and scanning guidelines. Ultrasonography. 2017;36:111–9. doi: 10.14366/usg.16054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kenwright DA, Anderson T, Moran CM, Hoskins PR. Assessment of spectral Doppler for an array-based preclinical ultrasound scanner using a rotating phantom. Ultrasound Med Biol. 2015;41:2232–9. doi: 10.1016/j.ultrasmedbio.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ginther O, Utt MD. Doppler ultrasound in equine reproduction: Principles, techniques, and potential. J Equine Vet Sci. 2004;24:516–26. [Google Scholar]
- 15.Ferreira JC, Ignácio FS, Meira CD. Doppler ultrasonography principles and methods of evaluation of the reproductive tract in mares. Acta Sci Vet. 2011;11:1125–23. [Google Scholar]
- 16.Hangiandreou NJ. AAPM/RSNA physics tutorial for residents. Topics in US: B-mode US: Basic concepts and new technology. Radiographics. 2003;23:1019–33. doi: 10.1148/rg.234035034. [DOI] [PubMed] [Google Scholar]
- 17.Mehra S. Role of Duplex Doppler sonography in arterial stenoses. J Indian Acad Clin Med. 2010;11:294–9. [Google Scholar]
- 18.Pellerito J, Polak JF. Manhasset, New York: Elsevier Health Sciences; 2012. Introduction to Vascular Ultrasonography. [Google Scholar]
- 19.McNaughton DA, Abu-Yousef MM. Doppler US of the liver made simple. Radiographics. 2011;31:161–88. doi: 10.1148/rg.311105093. [DOI] [PubMed] [Google Scholar]
- 20.Martin K. Edinburg University: 2010. Introduction to B-mode imaging Diagnostic Ultrasound: Physics and Equipment; pp. 1–22. [Google Scholar]
- 21.Sound SO. Introduction to vascular ultrasonography Physics and Instrumentation in Doppler and B-Mode Ultrasonography. James A Zagzebski. 2012;1550:20. [Google Scholar]
- 22.Zagzebski J. Philadelphia, PA: WB Saunders Co; 1992. s and instrumentation in Doppler and B-mode ultrasonography Introduction to Vascular Ultrasonography; pp. 19–43. [Google Scholar]
- 23.Kruskal JB, Newman PA, Sammons LG, Kane RA. Optimizing Doppler and color flow US: Application to hepatic sonography. Radiographics. 2004;24:657–75. doi: 10.1148/rg.243035139. [DOI] [PubMed] [Google Scholar]
- 24.Knox RA, Phillips DJ, Breslau PJ, Lawrence R, Primozich J, Strandnes DE., Jr Empirical findings relating sample volume size to diagnostic accuracy in pulsed Doppler cerebrovascular studies. J Clin Ultrasound. 1982;10:227–32. doi: 10.1002/jcu.1870100505. [DOI] [PubMed] [Google Scholar]
- 25.Zhou X, Xia C, Khan F, Corner GA, Huang Z, Hoskins PR, et al. Investigation of ultrasound-measured flow rate and wall shear rate in wrist arteries using flow phantoms. Ultrasound Med Biol. 2016;42:815–23. doi: 10.1016/j.ultrasmedbio.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 26.Ginther O. Cross Plains, WI: Equiservices Publishing; 2007. Ultrasonic Imaging and Animal Reproduction: Color-Doppler Ultrasonography Book 4. [Google Scholar]
- 27.Uppal T, Mogra R. RBC motion and the basis of ultrasound Doppler instrumentation. Australas J Ultrasound Med. 2010;13:32–4. doi: 10.1002/j.2205-0140.2010.tb00216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oates CP, Naylor AR, Hartshorne T, Charles SM, Fail T, Humphries K, et al. Joint recommendations for reporting carotid ultrasound investigations in the United Kingdom. Eur J Vasc Endovasc Surg. 2009;37:251–61. doi: 10.1016/j.ejvs.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 29.Ferreira JC, Gastal EL, Ginther OJ. Uterine blood flow and perfusion in mares with uterine cysts: Effect of the size of the cystic area and age. Reproduction. 2008;135:541–50. doi: 10.1530/REP-07-0447. [DOI] [PubMed] [Google Scholar]
- 30.Lunt MJ. Review of duplex and colour Doppler imaging of lower-limb arteries and veins. J Tissue Viability. 1999;9:45–55. doi: 10.1016/s0965-206x(99)80013-8. [DOI] [PubMed] [Google Scholar]
- 31.Hoskins PR. Measurement of arterial blood flow by Doppler ultrasound. Clin Phys Physiol Meas. 1990;11:1–26. doi: 10.1088/0143-0815/11/1/001. [DOI] [PubMed] [Google Scholar]
- 32.Rohren EM, Kliewer MA, Carroll BA, Hertzberg BS. A spectrum of Doppler waveforms in the carotid and vertebral arteries. AJR Am J Roentgenol. 2003;181:1695–704. doi: 10.2214/ajr.181.6.1811695. [DOI] [PubMed] [Google Scholar]
- 33.Gudmundson E, Jakobsson A, Gran F. IEEE. 2012. Overcoming the Nyquist Limit in Blood Flow Velocity Estimation. In: Ultrasonics Symposium (IUS), 2012 IEEE International. [Google Scholar]
- 34.Fredriksen TD, Ekroll IK, Lovstakken L, Torp H. 2-D tracking Doppler: A new method to limit spectral broadening in pulsed wave Doppler. IEEE Trans Ultrason Ferroelectr Freq Control. 2013;60:1896–905. doi: 10.1109/TUFFC.2013.2774. [DOI] [PubMed] [Google Scholar]
- 35.Kurjak A, Kupesic S, Breyer B, Sparac V, Jukic S. The assessment of ovarian tumor angiogenesis: What does three-dimensional power Doppler add? Ultrasound Obstet Gynecol. 1998;12:136–46. doi: 10.1046/j.1469-0705.1998.12020136.x. [DOI] [PubMed] [Google Scholar]
- 36.Chen SY, Hsu HY. Analysis of Doppler blood flow waveform of cerebral arteries and common abnormal findings. J Med Ultrasound. 2014;22:3–6. [Google Scholar]
- 37.Nelson TR, Pretorius DH. The Doppler signal: Where does it come from and what does it mean? AJR Am J Roentgenol. 1988;151:439–47. doi: 10.2214/ajr.151.3.439. [DOI] [PubMed] [Google Scholar]
- 38.Chavhan GB, Parra DA, Mann A, Navarro OM. Normal Doppler spectral waveforms of major pediatric vessels: Specific patterns. Radiographics. 2008;28:691–706. doi: 10.1148/rg.283075095. [DOI] [PubMed] [Google Scholar]
- 39.Jung J, Chang J, Oh S, Choi M. Spectral Doppler ultrasound in the major arteries of normal conscious immature micropigs. J Vet Sci. 2010;11:155–9. doi: 10.4142/jvs.2010.11.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Blohmé L, Pagani M, Parra-Hoyos H, Olofsson P, Takolander R, Swedenborg J, et al. Changes in middle cerebral artery flow velocity and pulsatility index after carotid endarterectomy. Eur J Vasc Surg. 1991;5:659–63. doi: 10.1016/s0950-821x(05)80902-8. [DOI] [PubMed] [Google Scholar]
- 41.Cooperberg E. Ultrasound Doppler spectral analysis in the diagnosis of occlusive lesions of the carotid arteries. Ultrasound Med Biol. 1992;18:421–5. doi: 10.1016/0301-5629(92)90050-k. [DOI] [PubMed] [Google Scholar]
- 42.Robinson ML, Sacks D, Perlmutter GS, Marinelli DL. Diagnostic criteria for carotid duplex sonography. AJR Am J Roentgenol. 1988;151:1045–9. doi: 10.2214/ajr.151.5.1045. [DOI] [PubMed] [Google Scholar]
- 43.Maulik D. Springer Protocols Malaysia Consortium. Springer; 2005. Spectral Doppler sonography: Waveform analysis and hemodynamic interpretation. In: Doppler Ultrasound in Obstetrics and Gynecology; pp. 35–56. [Google Scholar]
- 44.Scheinfeld MH, Bilali A, Koenigsberg M. Understanding the spectral Doppler waveform of the hepatic veins in health and disease. Radiographics. 2009;29:2081–98. doi: 10.1148/rg.297095715. [DOI] [PubMed] [Google Scholar]
- 45.Quiñones MA, Otto CM, Stoddard M, Waggoner A, Zoghbi WA. Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. Recommendations for quantification of Doppler echocardiography: A report from the Doppler quantification task force of the nomenclature and standards committee of the American Society of Echocardiography. J Am Soc Echocardiogr. 2002;15:167–84. doi: 10.1067/mje.2002.120202. [DOI] [PubMed] [Google Scholar]
- 46.Taylor KJ, Holland S, Doppler US. Part I. Basic principles, instrumentation, and pitfalls. Radiology. 1990;174:297–307. doi: 10.1148/radiology.174.2.2404309. [DOI] [PubMed] [Google Scholar]
- 47.Rubens DJ, Bhatt S, Nedelka S, Cullinan J. Doppler artifacts and pitfalls. Radiologic Clinics. 2006;44:805–35. doi: 10.1016/j.rcl.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 48.Lim AK, Patel N, Eckersley RJ, Kuo YT, Goldin RD, Thomas HC, et al. Can Doppler sonography grade the severity of hepatitis C-related liver disease? AJR Am J Roentgenol. 2005;184:1848–53. doi: 10.2214/ajr.184.6.01841848. [DOI] [PubMed] [Google Scholar]
- 49.North American Symptomatic Carotid Endarterectomy Trial Collaborators, Barnett HJ, Taylor DW, Haynes RB, Sackett DL, Peerless SJ, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–53. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 50.Warlow C. MRC European Carotid Surgery Trial: Interim results for symptomatic patients with severe (70-99%) or with mild (0-29%) carotid stenosis. Lancet. 1991;337:1235–43. [PubMed] [Google Scholar]
- 51.European Carotid Surgery Trialists'Collaborative Group. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: Final results of the MRC European Carotid Surgery Trial (ECST) Lancet. 1998;351:1379–87. [PubMed] [Google Scholar]
- 52.Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339:1415–25. doi: 10.1056/NEJM199811123392002. [DOI] [PubMed] [Google Scholar]
- 53.Ascher E, Hingorani A, Yorkovich W, Ramsey PJ, Salles-Cunha S. Routine preoperative carotid duplex scanning in patients undergoing open heart surgery: Is it worthwhile? Ann Vasc Surg. 2001;15:669–78. doi: 10.1007/s10016-001-0088-6. [DOI] [PubMed] [Google Scholar]
- 54.Forster FK, Chikos PM, Frazier JS. Geometric modeling of the carotid bifurcation in humans: Implications in ultrasonic Doppler and radiologic investigations. J Clin Ultrasound. 1985;13:385–90. doi: 10.1002/jcu.1870130603. [DOI] [PubMed] [Google Scholar]
- 55.Zwiebel WJ. Spectrum analysis in carotid sonography. Ultrasound Med Biol. 1987;13:625–36. doi: 10.1016/0301-5629(87)90060-3. [DOI] [PubMed] [Google Scholar]
- 56.Grant E, Barr L, Borgstede J. Reston, VA: American College of Radiology; 2002. ACR Guideline for the Performance of an Ultrasound Examination of the Extracranial Cerebrovascular System; pp. 577–80. [Google Scholar]
- 57.Tahmasebpour HR, Buckley AR, Cooperberg PL, Fix CH. Sonographic examination of the carotid arteries. Radiographics. 2005;25:1561–75. doi: 10.1148/rg.256045013. [DOI] [PubMed] [Google Scholar]
- 58.Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI, et al. Carotid artery stenosis: Gray-scale and Doppler US diagnosis – Society of radiologists in ultrasound consensus conference. Radiology. 2003;229:340–6. doi: 10.1148/radiol.2292030516. [DOI] [PubMed] [Google Scholar]
- 59.Hoskins PR. Ultrasound techniques for measurement of blood flow and tissue motion. Biorheology. 2002;39:451–9. [PubMed] [Google Scholar]
- 60.Maulik D, Zalud I. Winthrop University Hospital: Springer; 2005. Doppler Ultrasound in Obstetrics and Gynecology. [Google Scholar]
- 61.Bluth EI, Stavros AT, Marich KW, Wetzner SM, Aufrichtig D, Baker JD, et al. Carotid duplex sonography: A multicenter recommendation for standardized imaging and Doppler criteria. Radiographics. 1988;8:487–506. doi: 10.1148/radiographics.8.3.3289100. [DOI] [PubMed] [Google Scholar]
- 62.Lee W. General principles of carotid Doppler ultrasonography. Ultrasonography. 2014;33:11–7. doi: 10.14366/usg.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Garg S, Kashikar SV, Phatak S. Colour Doppler evaluation of extracranial carotid arteries: A Clinical and radiological correlation. J Clin Diagn Res. 2016;10:TC06–10. doi: 10.7860/JCDR/2016/15426.7130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rajagopal K, Lakhkar BN, Banavali S, Singh NK. Pictorial essay: Color duplex evaluation of carotid occlusive lesions. Indian Journal of Radiology and Imaging. 2000;10:221. [Google Scholar]
- 65.O'Leary DH, Polak JF. Intima-media thickness: A tool for atherosclerosis imaging and event prediction. Am J Cardiol. 2002;90:18L–21L. doi: 10.1016/s0002-9149(02)02957-0. [DOI] [PubMed] [Google Scholar]
- 66.Baldassarre D, Amato M, Bondioli A, Sirtori CR, Tremoli E. Carotid artery intima-media thickness measured by ultrasonography in normal clinical practice correlates well with atherosclerosis risk factors. Stroke. 2000;31:2426–30. doi: 10.1161/01.str.31.10.2426. [DOI] [PubMed] [Google Scholar]
- 67.Kofoed SC, Grønholdt ML, Wilhjelm JE, Bismuth J, Sillesen H. Real-time spatial compound imaging improves reproducibility in the evaluation of atherosclerotic carotid plaques. Ultrasound Med Biol. 2001;27:1311–7. doi: 10.1016/s0301-5629(01)00430-6. [DOI] [PubMed] [Google Scholar]
- 68.Homma S, Hirose N, Ishida H, Ishii T, Araki G. Carotid plaque and intima-media thickness assessed by b-mode ultrasonography in subjects ranging from young adults to centenarians. Stroke. 2001;32:830–5. doi: 10.1161/01.str.32.4.830. [DOI] [PubMed] [Google Scholar]
- 69.Park AE, McCarthy WJ, Pearce WH, Matsumura JS, Yao JS. Carotid plaque morphology correlates with presenting symptomatology. J Vasc Surg. 1998;27:872–8. doi: 10.1016/s0741-5214(98)70267-8. [DOI] [PubMed] [Google Scholar]
- 70.Slovut DP, Romero JM, Hannon KM, Dick J, Jaff MR. Detection of common carotid artery stenosis using duplex ultrasonography: A validation study with computed tomographic angiography. J Vasc Surg. 2010;51:65–70. doi: 10.1016/j.jvs.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 71.Mikkonen RH, Kreula JM, Virkkunen PJ. Peak systolic velocity, resistance index and pulsatility index. Variations in measuring a pre-recorded videotape. Acta Radiol. 1997;38:598–602. doi: 10.1080/02841859709174392. [DOI] [PubMed] [Google Scholar]
- 72.Cranley JJ, Johnson G. Duplex scanning in vascular disorders. J Vasc Surg. 1991;13:463–4. [Google Scholar]
- 73.AbuRahma AF, Richmond BK, Robinson PA, Khan S, Pollack JA, Alberts S, et al. Effect of contralateral severe stenosis or carotid occlusion on duplex criteria of ipsilateral stenoses: Comparative study of various duplex parameters. J Vasc Surg. 1995;22:751–61. doi: 10.1016/s0741-5214(95)70066-8. [DOI] [PubMed] [Google Scholar]


