Abstract
There are well-documented associations between posttraumatic stress disorder (PTSD) symptoms and intimate relationship impairments, including dysfunctional communication at times of relationship conflict. To date, the extant research on the associations between PTSD symptom severity and conflict communication has been cross-sectional and focused on military and veteran couples. No published work has evaluated the extent to which PTSD symptom severity and communication at times of relationship conflict influence each other over time or in civilian samples. The current study examined the prospective bidirectional associations between PTSD symptom severity and dyadic conflict communication in a sample of 114 severe motor vehicle accident (MVA) survivors in a committed intimate relationship at the time of the accident. PTSD symptom severity and dyadic conflict communication were assessed at 4 and 16 weeks post-MVA, and prospective associations were examined using path analysis. Total PTSD symptom severity at 4 weeks prospectively predicted greater dysfunctional communication at 16 weeks post-MVA but not vice versa. Examination at the level of PTSD symptom clusters revealed that effortful avoidance at 4 weeks prospectively predicted greater dysfunctional communication at 16 weeks, whereas dysfunctional communication 4 weeks after the MVA predicted more severe emotional numbing at 16 weeks. Findings highlight the role of PTSD symptoms in contributing to dysfunctional communication and the importance of considering PTSD symptom clusters separately when investigating the dynamic interplay between PTSD symptoms and relationship functioning over time, particularly during the early posttrauma period. Clinical implications for the prevention of chronic PTSD and associated relationship problems are discussed.
Keywords: PTSD, PTSD symptom clusters, motor vehicle accident, couple, communication
Numerous studies have established the association between posttraumatic stress disorder (PTSD) and intimate relationship impairments, including intimate partner aggression, partner distress, and caregiver burden (e.g., Lambert, Engh, Hasbun, & Holzer, 2012; Miller et al., 2013; Taft, Watkins, Stafford, Street, & Monson, 2011). Research also documents an association between PTSD symptoms and dysfunctional communication between partners at times of relationship conflict (e.g., Miller et al., 2013). However, little is known about how PTSD symptoms and couples’ conflict communication influence each other over time or in the immediate wake of trauma exposure. A better understanding of the bidirectional associations between PTSD symptoms and modifiable couple interactional processes, for prevention and early intervention efforts focused on couples in which one member has experienced a traumatic event. Thus, the goal of the present study was to test two theoretical models of the prospective associations between PTSD symptoms and dysfunctional couple conflict communication, the first of which postulates that dysfunctional communication predicts PTSD symptom severity (social causation) and the second of which postulates that PTSD symptoms predict dysfunctional communication (social selection).
How couples communicate during times of conflict is associated with relationship satisfaction and quality among couples in general (Christensen & Heavey, 1990; Gottman, 1994; Heyman, 2001; Snyder, Heyman, & Haynes, 2005) and among couples with PTSD, in particular. For example, Allen, Rhoades, Stanley, and Markman (2010) examined the cross-sectional associations between PTSD symptoms and negative communication among recently deployed active duty male service members with female civilian wives. Service members’ PTSD symptoms were associated with higher levels of negative communication for both service members and wives, and negative communication partially mediated the association between service members’ PTSD symptoms and both partners’ relationship satisfaction. Studies with veteran samples have yielded similar findings (e.g., Caska et al., 2014; Cook, Riggs, Thompson, Coyne & Sheikh, 2004; Miller et al., 2013). For example, Miller and colleagues (2013) noted that the severity of the veterans’ and partners’ clinician-assessed PTSD symptoms were each associated with more frequent displays of observer-rated negative behaviors (i.e., hostility and psychological abuse) and fewer expressions of positive behaviors (i.e., acceptance and humor) during couple conflict discussions. Cook et al. (2004) examined the associations between PTSD symptoms and couple conflict communication in a sample of World War II ex-prisoners of war. They reported that each of the four PTSD symptom clusters (reexperiencing, hyperarousal, effortful avoidance, and emotional numbing) was significantly associated with unproductive communication at times of relationship conflict. Follow-up tests revealed that, after controlling for the other symptom clusters, only the emotional numbing cluster was uniquely associated with dysfunctional communication, highlighting the salience of this symptom cluster with regard to conflict communication.
Taken together, these studies indicate that chronic PTSD symptoms are positively associated with ineffective or unproductive communication during times of conflict. However, much of this work has been conducted with male military or veteran samples that were exposed to trauma many years earlier. Related research documents that the interval immediately following trauma exposure is a time when natural recovery processes may be occurring (Riggs, Rothbaum, & Foa, 1995; Rothbaum, Foa, Riggs, & Murdock, 1992). This interval may also be a time when both PTSD symptoms and couples’ interactional processes are more malleable. However, the cross-sectional nature of the extant literature renders it impossible to determine the extent to which PTSD symptom severity drives dysfunctional communication or vice versa. That is, it may be that social and emotional processing deficits related to the disorder (Charuvastra & Cloitre, 2008; Monson, Price, Rodriguez, Ripley, & Warner, 2004) impede the ability to communicate effectively with one’s partner at times of disagreement. Alternatively, dysfunctional conflict communication with one’s partner could interfere with recovery following a trauma. Being in an intimate relationship characterized by (or perceived to be characterized by) high levels of criticism and conflict is thought to serve as a chronic stressor that impedes recovery from psychopathology generally (Hooley, 2007; Masland & Hooley, 2015; Whisman & Baucom, 2012). To the extent that dysfunctional communication is a component of family disharmony, perceived ineffective communication with an intimate partner at times of disagreement may amplify the perception that one is under threat, thereby exacerbating PTSD symptoms following a traumatic event. Thus, more research is needed to disentangle the directionality of these associations. As well, with the exception of Cook et al. (2004), most research on the association between PTSD symptoms and couple conflict communication has not examined associations between specific symptom clusters and dysfunctional conflict communication. Given that emotional numbing has been shown to be uniquely associated with greater dysfunctional communication cross-sectionally (Cook et al., 2004), it is important to determine if this symptom cluster, in particular, affects, or is affected by, dysfunctional couple communication in a prospective design in the early posttrauma period. These data thus have potential to inform opportunities for prevention or early intervention.
Prior studies that have attempted to disentangle the directionality of the associations between PTSD symptoms and intimate functioning more generally have investigated two primary models. One model, referred to as social causation, posits that poorer relationship functioning is an antecedent to mental health problems, including PTSD, particularly during stress; the other model, known as social selection, asserts that PTSD symptoms contribute to interpersonal dysfunction (Kaniasty & Norris, 2008). Studies with both veteran and civilian samples suggest that social causation processes are predominant in the earlier stages of posttrauma recovery (e.g., 6–12 months posttrauma; Fredman et al., 2010; Kaniasty & Norris, 2008), whereas social selection processes are more salient in the later posttrauma period, corresponding with the interval when symptoms become chronic and entrenched (Kaniasty & Norris, 2008; King, Taft, King, Hammond, & Stone, 2006). The conceptual distinction between social causation and social selection models of PTSD has greatly advanced our understanding of the disorder within an interpersonal context. Nonetheless, questions remain about the directionality of associations between interpersonal functioning and PTSD symptoms in the very acute aftermath of trauma exposure (i.e., the first 4 months posttrauma exposure) and at the level of specific symptom clusters.
Cross-sectional research indicates associations between the emotional numbing symptom cluster and myriad intimate relationship impairments, particularly among military/veteran samples with chronic PTSD (Cook et al., 2004; Nunnink, Goldwaser, Afari, Nievergelt, & Baker, 2010; Renshaw, Campbell, Meis, & Erbes, 2014; Riggs, Byrne, Weathers, & Litz, 1998). Extant longitudinal research similarly highlights the salience of the emotional numbing symptom cluster with respect to intimate relationship dysfunction and is consistent with both social selection and social causation models with respect to this symptom cluster, in particular. For example, in a sample of U.S. soldiers who had returned from combat deployment within the prior 6 months, Erbes, Meis, Polusny, and Compton (2011) found that a dysphoria PTSD symptom cluster, which subsumed the emotional numbing symptoms, uniquely predicted relationship adjustment 1 year later. In a second study, the investigators (Erbes, Meis, Polusny, Compton, & Wadsworth, 2012) replicated these findings and observed that relationship adjustment did not predict total symptoms assessed 6–9 months later after controlling for initial PTSD symptom severity. These findings suggest that PTSD symptoms, particularly emotional numbing and other aspects of dysphoria, drive relationship adjustment but not vice versa, once symptoms have become chronic. However, these studies examined the effect of PTSD symptom clusters on subsequent relationship adjustment and not the converse (relationship adjustment on later PTSD symptom cluster severity), leaving an important question in this domain unanswered.
Related studies by Evans and colleagues (Evans, Cowlishaw, Forbes, Parslow, & Lewis, 2010; Evans, Cowlishaw, & Hopwood, 2009) have attempted to more fully explicate the bidirectional and longitudinal associations between individual PTSD symptom clusters and family functioning using large samples of treatment-seeking combat veterans with chronic PTSD (mean time since trauma 26 years) by taking into account both autoregressive (i.e., a variable’s association with itself over time) and cross-lagged (i.e., a variable’s association with another variable across time) associations. The authors observed that family functioning appeared to be a more salient driver of PTSD symptom severity than vice versa with the exception of the avoidance/numbing cluster of symptoms, which had a bidirectional association with family functioning over time. However, the authors did not disaggregate effortful avoidance symptoms of PTSD from emotional numbing symptoms, rendering it difficult to parse which aspect of veterans’ withdrawal symptoms are most closely associated with poorer family functioning over time.
Collectively, these findings suggest that intimate relationship functioning and PTSD symptom clusters are related longitudinally and that symptoms of emotional numbing are particularly interpersonally salient, with potential bidirectional associations with relationship dysfunction over time. However, differences in sample characteristics and time since trauma exposure across studies leave questions about the directionality of these associations. Moreover, as noted by other researchers (e.g., Erbes et al., 2012; Evans et al., 2010; Evans, Cowlishaw, & Hopwood, 2009), the focus on broad indices of couples’ relationship quality (e.g., global relationship adjustment, general family functioning, relationship satisfaction, social support) does not identify couple interactional processes that may be closely associated with particular PTSD symptom clusters and potentially targeted in any interventions. In particular, Evans et al. (2010) suggested that researchers should investigate how couples’ communication relates to PTSD symptoms to more fully explicate the relationship context of PTSD and inform opportunities for targeted intervention.
In light of these considerations, the goal of the present study was to examine the prospective associations between PTSD symptoms and conflict communication to determine (a) whether dysfunctional couple conflict communication predicts total PTSD symptom severity, total PTSD symptom severity predicts dysfunctional couple conflict communication, or both; and (b) whether patterns of association differ across PTSD symptom clusters during the first 4 months after recent exposure to a severe motor vehicle accident (MVA). We hypothesized that, consistent with social causation processes, dysfunctional conflict communication at Time 1 would be positively and significantly associated with total PTSD symptom severity at Time 2 and would uniquely predict Time 2 emotional numbing severity when all symptom clusters were examined simultaneously. We also hypothesized that, in accord with social selection processes, emotional numbing severity at Time 1 would be positively and significantly associated with dysfunctional communication at Time 2.
Method
PARTICIPANTS
The sample consisted of 84 (73.7%) female and 30 (26.3%) male survivors of serious MVAs (N = 114), who ranged in age from 18 to 65 years (M = 38.14, SD = 12.52). Fifty-four (47.4%) participants reported being married, 9 (7.9%) were engaged, 9 (7.9%) were cohabiting, and 42 (36.8%) reported being in dating relationships. The average length of the intimate relationships was 111.40 months (SD = 126.30) with a range spanning from 4 to 552 months, and a median of 54 months, as reported during the initial assessment. With respect to race/ethnicity, 83 (72.8%) participants were Caucasian, 22 (19.3%) were African American, 2 (1.8%) were Hispanic/Latino, and 7 (6.1%) were of another race or ethnicity. The majority of the sample was employed at least part-time (62.3%) and had some college education (76.3%). The average elapsed time since the MVA was 27.63 days (SD = 7.19) at the first assessment (4 weeks post-MVA) and 112 days (SD = 7.0) at the second assessment (16 weeks post-MVA).
MEASURES
PTSD Checklist–Civilian Version (PCL-C)
The PCL-C (Weathers, Litz, Herman, Huska, & Keane, 1993) is a self-report scale designed to assess the severity of the 17 DSM-IV symptoms of PTSD. For the purposes of the current study, participants were asked to rate how much the specific MVA-related posttraumatic symptoms described in the measure had bothered them during the past month on a 5-point scale from 1 (not at all) to 5 (extremely), with total scores ranging from 17 to 85. Blanchard, Jones-Alexander, Buckley, and Forneris (1996) have shown that, among MVA survivors, the PCL-C has excellent internal consistency and concordance with the Clinician Administered PTSD Scale (CAPS; Blake et al., 1995). In the current sample, the PCL-C had excellent internal consistency for total PTSD symptoms (α = .94 at Time 1 and α = .95 at Time 2) and good internal consistency for the four PTSD symptom clusters (i.e., reexperiencing, effortful avoidance, emotional numbing, and hyperarousal), with Cronbach’s alphas ranging from .75 to .95 across assessment points.
Communication Patterns Questionnaire (CPQ)
The CPQ (Christensen, 1988; Christensen & Sullaway, 1984) is a 35-item self-report measure designed to assess an individual’s perceptions of dyadic communication patterns at times of conflict. The CPQ uses a 9-point Likert scale ranging from 1 (very unlikely) to 9 (very likely) in which the respondent indicates whether specific communication patterns occur during three phases of an argument: when a problem arises, during the discussion of the problem, and after the discussion of the problem. The CPQ has three subscales: mutual constructive communication (e.g., “Both spouses suggest possible solutions and compromises”), demand/withdrawal communication (e.g., “Female criticizes while male defends himself”), and mutual avoidance and withholding (e.g., “Both spouses avoid discussing the problem”). It has been shown to have adequate internal consistency as well as adequate validity in its ability to differentiate between distressed versus nondistressed couples (Christensen & Shenk, 1991). It also has good concordance with observational measures of couples’ communication (Hahlweg, Kaiser, Christensen, Fehm-Wolfsdorf, & Groth, 2000). Internal consistency for the CPQ subscales ranged from α = .73 to .83 at Time 1 and from α = .79 to .90 at Time 2.
Ineffective Arguing Inventory (IAI)
The IAI (Kurdeck, 1994) is an eight-item self-report measure that assesses dyadic dysfunctional styles in conflict resolution. The primary focus of the IAI is to measure ineffective arguing (e.g., “Our arguments are left hanging and unresolved”). For each item, respondents are asked to indicate how much the statement fit their relationship on a 5-point scale (1 = strongly agree to 5 = strongly disagree). In a psychometric study of the IAI, Kurdek (1994) reported high internal consistency (Cronbach’s α = .89) and that the measure possessed adequate face validity. Internal consistency for the IAI in the present sample was excellent at Time 1 (α = .91) and Time 2 (α = .95).
PROCEDURE
Prospective participants were identified by reviewing police records (n = 2,373) from local police stations in Buffalo, New York. They were then mailed a letter inviting them to participate within 2 weeks of their MVA. All of those contacted were involved in a serious, injury-related MVA in the month prior to their participation. A serious MVA was defined as one in which the individual sought medical attention within 48 hours of the accident (Blanchard & Hickling, 2004).
Those who responded to the invitation letter were screened by phone to determine inclusion/exclusion criteria. The phone screen was conducted no more than 3 weeks after the accident so that participants could complete the Time 1 packet of questionnaires within the first month post-MVA. To be enrolled in the study, participants also had to be in an exclusive heterosexual intimate relationship (e.g., marriage, serious committed dating, or cohabiting) lasting a minimum of 4 months. An additional inclusion criterion was that individuals’ emotional response during the accident included intense fear, helplessness, or horror (DSM-IV-TR Criterion A2 for PTSD; American Psychiatric Association, 2000), as determined by the Motor Vehicle Accident Interview (Blanchard & Hickling, 2004). Exclusion criteria included (a) not speaking English; (b) current physical and/or emotional abuse; (c) current use and/or treatment for alcohol/drug abuse/dependence; (d) impaired cognitive functioning; (e) delusional/ psychotic thinking; (f) in the process of divorce; (g) not meeting MVA-related Criterion A2 for PTSD; (h) having been intoxicated at the time of the accident; and (i) clear suicidal ideation, intention, and plan requiring immediate psychiatric care. The study was approved by the Institutional Review Board at the State University of New York at Buffalo, and informed consent was obtained from all enrolled participants.
Census data collected at the time indicated that approximately 59.9% of the population in the greater Buffalo, NewYork, area was married (U.S. Census Bureau, 2004), suggesting that approximately 1,421 individuals could have met study criteria based on marital status. However, it is unknown what percentage of the available population was in a committed relationship lasting 4 or more months but were not married. Of those who were mailed a letter inviting them to participate in the study, 199 responded. Thus, the response rate was estimated to be 8–14%.
Based on the phone screen, 47 of 199 individuals were excluded from further participation as a result of not being in a romantic relationship at the time (n = 19), having a relationship lasting less than 4 months (n = 7), not seeking medical attention within 48 hours of the MVA (n = 11), being cognitively impaired (n = 3), having acute psychotic thoughts (n = 3), and/or engaging in heavy alcohol use (n = 4). Participants who met the study inclusion/exclusion criteria based on the phone screen (N = 152) were asked to complete packets of postal surveys at Time 1 (4 weeks post-MVA) and at Time 2 (16 weeks post-MVA). Of the 152 individuals who were mailed questionnaire packets, 114 participants (i.e., 75% of those eligible) returned the packets at Time 1 and provided data for both PTSD symptoms and communication patterns. Of these 114 participants, 11 returned packets at Time 1 but not Time 21 but were retained for all analyses in the current investigation because they did not differ significantly from the 103 participants who contributed data at both time points with respect to total PTSD symptoms, PTSD symptom clusters, or communication variables (ps > .14).
ANALYTIC PLAN
First, bivariate correlations were examined to determine if the measures could be aggregated at each time point to form a composite negative communication variable (CPQ demand–withdraw communication, CPQ mutual avoidance, IAI). Examination of cross-sectional correlations indicated that the three measures were strongly correlated at Time 1 (rs = .59–.69, ps < .001) and Time 2 (rs = .70–.77, ps < .001). The measures were subsequently combined to create a composite negative communication variable for each time point by standardizing each variable and then averaging them. Because the negative communication variable and the CPQ mutual constructive communication variable were also strongly correlated at each time point (−.76 at Time 1 and −.79 at Time 2), we subsequently created a single composite conflict communication variable by standardizing the CPQ mutual constructive communication variable (reverse scored) and averaging it with the negative communication variable, with higher scores reflecting greater dysfunctional conflict communication. We then examined the bivariate correlations among total PTSD symptoms, PTSD symptom clusters, and the composite dysfunctional communication variable to explore the cross-sectional associations among the variables at Time 1 and Time 2.
To examine the prospective associations between Time 1 PTSD symptoms and Time 2 conflict communication and vice versa, we first examined PTSD symptoms at the level of total PTSD symptom severity. In this path analysis, the associations between Time 1 total PTSD severity and Time 2 dysfunctional conflict communication as well as Time 2 total PTSD symptom severity (the autoregressive association), and the associations between Time 1 dysfunctional conflict communication and Time 2 total PTSD symptom severity as well as Time 2 dysfunctional conflict communication (the autoregressive association) were modeled. The covariances between Time 1 total PTSD symptom severity and dysfunctional conflict communication and the residuals of Time 2 total PTSD symptom severity and dysfunctional conflict communication were also included, resulting in a fully saturated model.
To determine which specific symptom clusters(s) were prospectively associated with dysfunctional conflict communication, we also conducted a path model in which all PTSD symptom clusters (i.e., reexperiencing, effortful avoidance, emotional numbing, and hyperarousal) and dysfunctional conflict communication were entered at both time points. As with the previous model, all autoregressive and cross-lagged paths were included, along with the cross-sectional covariances among the PTSD symptom clusters and dysfunctional communication at Time 1 and the covariances of the residuals of each outcome at Time 2. To decrease the number of paths estimated, autoregressive paths were constrained to be equivalent across symptom clusters after it was confirmed that there was no degradation in model fit. We subsequently engaged in model-trimming procedures whereby nonsignificant paths were dropped if doing so did not result in a significant degradation in model fit according to the χ2 difference test to compare nested models. Good overall model fit was interpreted using standard fit indices and cutoff scores recommended by Hu and Bentler (1999): (a) χ2 test of model fit, with small and nonsignificant values; (b) the root mean square error of approximation (RMSEA), with values less than or equal to .06; (c) the standardized root mean square residual (SRMR), with values less than or equal to .08; (d) the comparative fit index (CFI), with values of .95 or greater; and (e) the Tucker-Lewis Index (TLI), with values of .95 or greater.
Path analyses were conducted using Mplus version 7 (Muthén & Muthén, 1998–2012) with robust maximum likelihood (MLR) as the method of estimation to account for the non-normal distributions of the PTSD and communication variables. MLR generates parameter estimates that are standard maximum likelihood estimates but uses standard errors that are robust to non-normality, thereby generating more conservative estimates of p values associated with individual path estimates relative to those generated from full information maximum likelihood estimation.
Exploratory tests of moderation by sex were also conducted to determine whether the longitudinal paths differed as a function of participant sex. This was accomplished by specifying the existence of two groups (0 = male, 1 = female) and constraining all longitudinal paths to be equivalent across groups for each model. The constrained, nested model was subsequently compared with the fully saturated model in which all paths were freely estimated across gender. Because the χ2 difference test comparing the nested model with the constrained longitudinal paths was not significant for either of the path models (ps ≥ .42), the more parsimonious path models in which males and females were considered as one group were retained.
Results
Total PCL-C scores ranged from 17 to 77 at Time 1 and from 17 to 80 at Time 2. Using the recommended cutoff of 44 for a probable diagnosis of PTSD (Blanchard, Jones-Alexander, et al., 1996), 42.1% of participants met diagnostic criteria for PTSD at Time 1 and 24.3% met criteria at Time 2, indicating that this sample exhibited moderate levels of psychopathology across the study period.
The bivariate cross-sectional and longitudinal correlations between PTSD symptoms (at both the total and symptom cluster levels) and dyadic conflict communication styles are presented in Table 1. Cross-sectionally and longitudinally, bivariate correlations between PTSD symptoms and dysfunctional communication ranged from small to medium, with the largest associations observed between dysfunctional communication and emotional numbing.
Table 1.
Bivariate Correlations Among PTSD Symptom Severity and Dysfunctional Conflict Communication at 4 and 16 Weeks
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | M | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 Total | - | 39.43 | 15.51 | ||||||||||
| 2. T1 Reexp | .89** | - | 11.95 | 5.40 | |||||||||
| 3. T1 EA | .82** | .73** | - | 4.46 | 2.25 | ||||||||
| 4. T1 EN | .87** | .65** | .67** | - | 9.84 | 4.64 | |||||||
| 5. T1 HYP | .89** | .69** | .62** | .71** | - | 13.18 | 5.40 | ||||||
| 6. T1 Comm | .31** | .21** | .30** | .42** | .19* | - | .00 | .87 | |||||
| 7. T2 Total | .67** | .59** | .62** | .57** | .57** | .25* | - | 32.37 | 14.77 | ||||
| 8. T2 Reexp | .63** | .62** | .60** | .49** | .50** | .14 | .91** | - | 9.52 | 4.97 | |||
| 9. T2 EA | .60** | .58** | .64** | .48** | .46** | .19 | .83** | .76** | - | 3.80 | 2.19 | ||
| 10. T2 EN | .54** | .42** | .49** | .55** | .44** | .37** | .90** | .70** | .70** | - | 8.42 | 4.40 | |
| 11. T2 HYP | .62** | .50** | .53** | .52** | .61** | .20* | .92* | .76** | .64** | .78** | - | 10.63 | 4.91 |
| 12. T2 Comm | .31** | .21* | .35** | .39** | .21* | .82** | .29** | .20* | .19** | .39** | .23* | .00 | .90 |
Note. T1 = Time 1 (4-weeks post-MVA); T2 = Time 2 (16-weeks post-MVA); PTSD = posttraumatic stress disorder; Total = total PTSD symptoms; Reexp = reexperiencing symptoms; EA = effortful avoidance symptoms; EN = emotional numbing symptoms; HYP = hyperarousal symptoms; Comm = conflict communication composite variable. Ns range from 103 to 114.
p < .05,
p < .01.
LONGITUDINAL ASSOCIATIONS BETWEEN PTSD SYMPTOMS AND CONFLICT COMMUNICATION
Total PTSD Symptoms
As displayed in Figure 1, there were significant autoregressive associations between total PTSD symptom severity at Time 1 and Time 2 and between dysfunctional conflict communication at Time 1 and Time 2. Contrary to expectation, the path from Time 1 dysfunctional conflict communication to Time 2 total PTSD symptoms was not significant, but there was a positive and significant cross-lagged path from Time 1 total PTSD symptom severity to Time 2 dysfunctional conflict communication.
FIGURE 1.
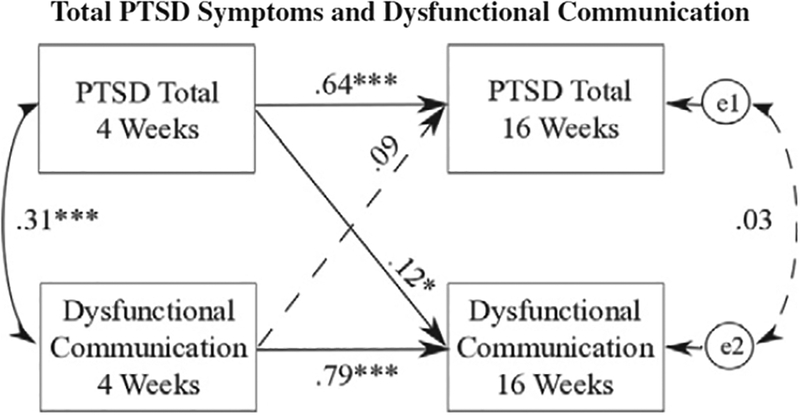
Path model of the prospective predictions of total posttraumatic stress disorder (PTSD) symptoms and dysfunctional communication. * p < .05, *** p < .001.
PTSD Symptom Clusters
Overall, the model provided excellent fit to the data, χ2(21) = 11.70, p = .95; RMSEA = .00; SRMR = .03; TLI = 1.00; CFI = 1.00. As displayed in Figure 2, there were positive and significant autoregressive associations between each symptom cluster at Time 1 and Time 2 and between dysfunctional communication at Time 1 and Time 2. There were also positive and significant cross-lagged paths between Time 1 reexperiencing symptoms and Time 2 effortful avoidance as well as between Time 1 effortful avoidance and each of the other Time 2 symptom clusters (i.e., reexperiencing, emotional numbing, and hyperarousal). Last, and consistent with the focus of the current investigation, there was a positive and significant cross-lagged path from Time 1 effortful avoidance to Time 2 dysfunctional communication as well as a positive and significant cross-lagged path from Time 1 dysfunctional communication to Time 2 emotional numbing.2, 3
FIGURE 2.
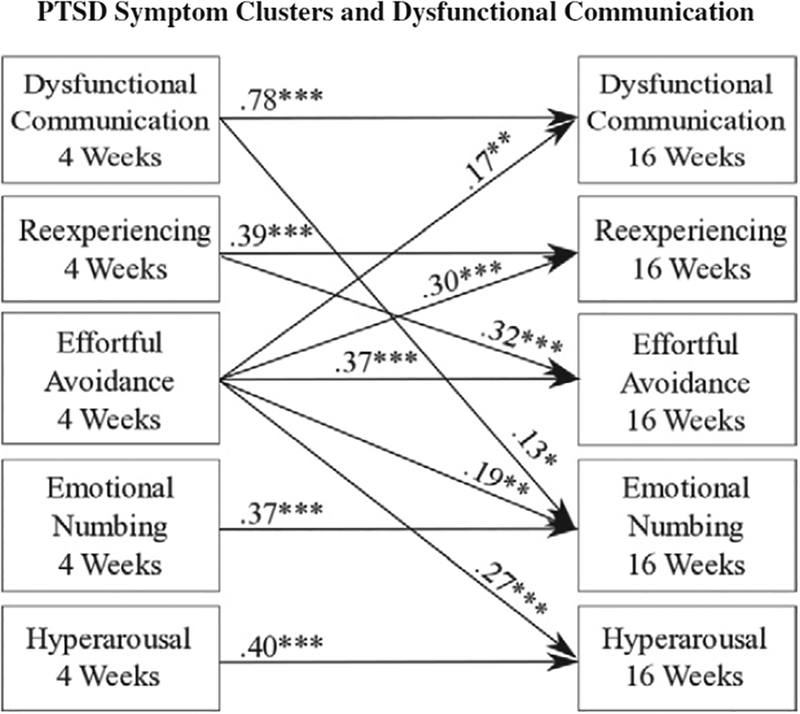
Path model of the prospective predictions of postraumatic stress disorder (PTSD) symptom clusters and dysfunctional communication. Coefficients for the associations among the symptom clusters and dysfunctional communication at Time 1, as well as the covanance of the residuals of the symptom clusters and dysfunctional communication at Time 2 for each of the path models, are available from the first author (S.J.F.) upon request. * p < .05,** p < .01, *** p < .001.
Discussion
The goal of the current investigation was to test two models of the longitudinal associations between dysfunctional conflict communication and PTSD symptom severity in the acute aftermath of a severe MVA. The two models were conceptualized as social causation (i.e., dysfunctional communication predicts greater posttrauma symptom severity) versus social selection (i.e., posttrauma symptom severity predicts greater dysfunctional communication).
Based on prior literature supporting a social causation model of PTSD symptoms in the first 6–12 months posttrauma (e.g., Kaniasty & Norris, 2008), we had hypothesized that dysfunctional communication would predict total PTSD symptoms. Instead, we observed that Time 1 total PTSD symptoms prospectively predicted Time 2 dysfunctional communication, but not vice versa, which is consistent with social selection. It may be that differences in study time frames (e.g., the first 4 months posttrauma in the present study versus 6–12 months in prior studies) account for these differences. Alternatively, the differences in study findings could be due to subtle differences in the interpersonal constructs examined across studies. That is, dysfunctional conflict communication, as studied in the present investigation, may represent an individual’s perception of one behaviorally specific aspect of one’s romantic relationship, whereas one’s report of relationship adjustment and perceived social support received from close others may serve as more global indices of one’s perceptions of relationship functioning.
At the level of PTSD symptom clusters, interesting differences emerged with respect to the directionality of the associations between PTSD symptoms and dysfunctional conflict communication. We found that Time 1 effortful avoidance predicted greater dysfunctional communication at Time 2 but not vice versa, consistent with a social selection interpretation. This suggests that effortful avoidance is the component of total PTSD symptoms that most strongly accounts for the prospective association between total PTSD symptoms and later dysfunctional conflict communication. It may be that, consistent with conceptual models of the interpersonal context of PTSD (Monson, Fredman, & Dekel, 2010), effortful avoidance deprives couples of the opportunity to engage in mutually satisfying behavioral exchanges, which may include communicating constructively at times of relationship conflict. To the extent that a trauma survivor does not engage with one’s partner at times of disagreement due to symptoms of effortful avoidance, the couple is not afforded the opportunity to experience the sense of intimacy and trust that can arise from the successful and productive resolution of disagreements, and conflict is left unresolved.
Whereas social selection processes appear to account for the association between effortful avoidance and dysfunctional conflict communication, social causation processes seem to be at play in the prospective association between emotional numbing and dysfunctional conflict communication such that Time 1 dysfunctional communication positively and prospectively predicted Time 2 emotional numbing symptom severity. These findings suggest that dysfunctional communication proximal to the traumatic event impedes natural recovery by muting emotional processes. The pattern of results regarding the prospective prediction of emotional numbing by dysfunctional communication in this study is similar to that observed by Evans and colleagues (Evans et al., 2009, 2010), who demonstrated that higher levels of family dysfunction at baseline predicted more severe avoidance/numbing symptoms among veterans following treatment for chronic PTSD. These data help to clarify that it may be the emotional numbing symptoms that appear to be particularly responsive to dysfunctional family processes in the form of ineffective and unproductive conflict communication. Taken together with previous research, these findings highlight the critical importance of attending to the emotional climate of the trauma survivor’s intimate relationship during periods when symptoms may be relatively more likely to change (e.g., shortly after trauma exposure and during treatment for PTSD).
There are several clinical implications of these findings. First, early identification and reduction of effortful avoidance symptoms proximal to trauma exposure may have important salutary effects on subsequent dyadic communication and associated intimate relationship functioning. Reduction of effortful avoidance symptoms identified at 1-month posttrauma may also have beneficial implications with respect to PTSD symptoms more broadly, as Time 1 avoidance severity predicted not only Time 2 avoidance severity but also the severity of reexperiencing, numbing, and hyperarousal symptoms. Relatedly, improvements in couples’ dysfunctional important prognostic implications for emotional may have important prognostic implications for emotional numbing, the symptom cluster known to have particularly corrosive effects on intimate relationship adjustment (e.g., Cook et al., 2004; Renshaw et al., 2014; Riggs et al., 1998). The symptom-specific cross-lagged associations with dyadic conflict communication found in the current study suggest that a dyadic approach to recovery following traumatization among couples deemed at high risk, either by virtue of high levels of avoidance symptoms on the part of the trauma survivor and/or high levels of dysfunctional dyadic conflict communication, could be particularly helpful during the early months of recovery from trauma. For example, several existing couple-based interventions for PTSD (e.g., cognitive-behavioral conjoint therapy for PTSD [Monson & Fredman, 2012]; strategic approach therapy [Sautter, Glynn, Cretu, Senturk, & Vaught, 2015; Sautter, Glynn, Thompson, Franklin, & Han, 2009]) seek to simultaneously improve PTSD symptoms and enhance intimate relationship functioning by improving conflict management skills, decreasing effortful avoidance, and enriching emotional expression and dyadic communication and have demonstrated effects on both individual symptom clusters and relationship adjustment (Macdonald, Pukay-Martin, Wagner, Fredman, & Monson, 2016; Monson et al., 2012; Sautter et al., 2009, 2015). Future research that explores the extent to which these treatments may be adapted and delivered, perhaps in abbreviated form, to couples deemed at high risk early in the trauma recovery period could determine the safety and feasibility of conducting dyadic early interventions for trauma survivors and their loved ones.
There are several limitations to the current study. First, there was an exclusive use of self-report measures of PTSD symptoms and conflict communication. Although self-report of PTSD symptoms is the norm in this literature (e.g., Allen et al., 2010; Balderrama-Durbin et al., 2013; Campbell & Renshaw, 2013; Erbes et al., 2011), the use of gold-standard clinician measurement of PTSD symptoms and observer ratings of couples’ communication in future research will help to decrease shared method variance resulting from the reliance on self-report measures. Second and relatedly, there was no partner report of one’s own or the trauma survivor’s PTSD symptoms. In this vein, research indicates there are both actor and partner effects of PTSD on communication (e.g., Miller et al., 2013) and that the longitudinal association between symptoms and family dysfunction may vary as a function of whether the trauma survivor’s perspective versus partner’s perspective on relationship functioning is used (Erbes et al., 2012; Evans et al., 2010). Nonetheless, one’s perceptions of relational communication patterns may, in fact, be more important for PTSD symptoms than actual (e.g., objectively observed) communication patterns. Indeed, in the broader literature on psychopathology in a couple/family context, the extent to which patients perceive family members as behaving negatively toward them is a more robust predictor of symptom severity and treatment outcome than are interview-based ratings of relatives’ emotional attitudes expressed about patients or observer ratings of patient-relative interactions focused on frequency counts of positive and negative behaviors (e.g., Hooley & Teasdale, 1989; see also Fredman, 2010; Masland & Hooley, 2015, for reviews). Future studies that include multimodal assessment of the constructs of PTSD symptoms and couple conflict communication would be helpful in confirming the pattern of findings observed in the present investigation. Third, the current investigation took place over a relatively short time frame (i.e., the first 4 months after trauma exposure). It is possible that the directionality of the associations between PTSD symptom clusters and communication may change over time; employing a longer time frame would be useful in gleaning a more nuanced picture of early adjustment following trauma exposure. Fourth, the response rate in the present sample was low relative to response rates for dyadic research involving public records (e.g., 17%; Davila, Bradbury, Cohan, & Tochluk, 1997). This type of research design could benefit from methodological tools to enhance recruitment rates. As well, we had no measure of couples’ pretrauma conflict communication. Although methodologically challenging, we encourage future research to consider inclusion of a measure of pretrauma conjoint functioning.
Other areas for future directions include examining couples’ communication beyond areas of conflict. For example, it has been shown that, among service members, trauma-related disclosure mediates the cross-sectional association between social support and PTSD symptoms (Balderrama-Durbin et al., 2013) and the longitudinal association between PTSD symptoms, notably emotional numbing, and relationship satisfaction (Campbell & Renshaw, 2013). However, the extent to which disclosure processes operate in civilian samples in the early months after trauma exposure is unknown. Including measures of communication about trauma-related content, in addition to communication at times of conflict, in future research will help to determine whether the pattern of findings observed in the present study is common to all forms of communication or specific to conflict communication. It should also be noted that the majority of the sample was female. Although there were no gender differences observed in the pattern of findings in the present study, females’ behavioral tendency to “tend and befriend” when under stress (e.g., Taylor et al., 2000) may make women particularly attuned to dysfunctional relationship processes, such as communication at times of conflict, and, thus, more susceptible to experience disrupted emotional processing when they perceive difficulties communicating with their partners, particularly after a highly stressful event. Future research that examines these questions in samples that include more male trauma survivors and those who have experienced other index traumas (e.g., combat, robbery) will help elucidate conditions in which gender differences may exist and whether the pattern of findings observed in this sample of MVA survivors generalizes to survivors of other traumatic events. Last, the demographic and symptom characteristics of this sample are similar to those of other samples of MVA survivors who were studied prospectively (e.g., Blanchard, Hickling, et al., 1996); nonetheless, it would be helpful to confirm the pattern of findings in other samples of MVA survivors in future research.
In conclusion, PTSD symptoms—particularly symptoms of effortful avoidance—evident as early as 1 month after a trauma can increase risk for later communication difficulties, whereas dysfunctional communication shortly after traumatization increases risk for more severe emotional numbing symptoms, the PTSD symptom cluster most strongly implicated in impaired intimate relationship functioning. Findings provide additional support for DSM-5’s (American Psychiatric Association, 2013) disaggregating of the avoidance/numbing symptom cluster into effortful avoidance and negative alterations in cognition and mood, and they highlight the importance of considering different types of PTSD symptoms and relationship functioning over time. Early recognition of specific PTSD symptoms and dysfunctional dyadic communication, a modifiable risk factor, could preempt entrenchment of PTSD and associated relationship problems.
Acknowledgments
This research was supported in part by grants from the National Institute of Mental Health to Luana Marques (R36 MH075383 and K23 MH096029–01A1), a grant from the National Center for Advancing Translational Sciences, National Institutes of Health to the Pennsylvania State University (UL1 TR000127), and start-up funds to Steffany J. Fredman at The Pennsylvania State University. We gratefully acknowledge Timothy Brick, Gregory Fosco, Thomas Rodebaugh, and Jeremiah Schumm for their guidance regarding data analysis.
Footnotes
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
This attrition rate of 9.64% is consistent with attrition rates in other studies of MVA survivors (e.g., 8.2% in Blanchard & Hickling, 2004).
A Wald test was conducted to compare the strength of cross-lagged pathways between Time 1 effortful avoidance and Time 2 dysfunctional communication, as well as between Time 1 dysfunctional communication and Time 2 emotional numbing. Results indicated that Time 1 effortful avoidance is more strongly associated with Time 2 dysfunctional communication than Time 1 dysfunctional communication is associated with Time 2 emotional numbing, Wald statistic = 5.028(1), p = .025.
We also estimated a model in which negative and constructive communication were included in the same model at both time points, and results were similar to those observed when a single composite dysfunctional communication variable is used. Specifically, there was a positive and significant cross-lagged path from Time 1 effortful avoidance to Time 2 negative communication and a negative and significant cross-lagged path from Time 1 effortful avoidance to Time 2 constructive communication. There was also a positive and significant cross-lagged path from Time 1 negative communication to Time 2 emotional numbing. No gender differences were found for any of these associations. In addition, there was a positive cross-lagged path from Time 1 negative communication to Time 2 hyperarousal that approached significance at p = .058. However, when we removed that path from the model, overall model fit degraded significantly, Δχ2(1) = 5.1, p = .02, indicating that this path should be retained.
Contributor Information
Steffany J. Fredman, The Pennsylvania State University
J. Gayle Beck, University of Memphis.
Philippe Shnaider, Ryerson University.
Yunying Le, The Pennsylvania State University.
Nicole D. Pukay-Martin, Trauma Recovery Center, Cincinnati VA Medical Center
Kimberly Z. Pentel, University of North Carolina at Chapel Hill
Candice M. Monson, Ryerson University
References
- Allen ES, Rhoades GK, Stanley SM, & Markman HJ (2010). Hitting home: Relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for army couples. Journal of Family Psychology, 24, 280–288. 10.1037/0893-3200.21.4.572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Balderrama-Durbin C, Snyder DK, Cigrang J, Talcott GW, Tatum J, Baker M, … Smith Slep AM (2013). Combat disclosure in intimate relationships: Mediating the impact of partner support on posttraumatic stress. Journal of Family Psychology, 27, 560–568. 10.1037/a0033412 [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8, 75–90. 10.1007/BF02105408 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, & Hickling EJ (2004). After the crash: Psychological assessment and treatment of survivors of motor vehicle accidents (2nd ed.). Washington, DC: American Psychological Association. [Google Scholar]
- Blanchard EB, Hickling EJ, Barton KA, Taylor AE, Loos WR, & Jones-Alexander J (1996). One-year prospective follow-up of motor vehicle accident victims. Behaviour Research and Therapy, 34, 775–786. 10.1016/0005-7967(96)00038-1 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- Campbell SB, & Renshaw KD (2013). PTSD symptoms, disclosure, and relationship distress: Explorations of mediation and associations over time. Journal of Anxiety Disorders, 27, 494–502. 10.1016/j.janxdis.2013.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caska CM, Smith TW, Renshaw KD, Allen SN, Uchino BN, Birmingham W, & Carlisle M (2014). Posttraumatic stress disorder and responses to couple conflict: Implications for cardiovascular risk. Health Psychology, 33, 1273–1280. 10.1037/hea0000133 [DOI] [PubMed] [Google Scholar]
- Charuvastra A, & Cloitre M (2008). Social bonds and posttraumatic stress disorder. Annual Review of Psychology, 59, 301–328. 10.1146/annurev.psych.58.110405.085650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen A (1988). Dysfunctional interaction patterns in couples In Noller P & Fitzpatrick MA (Eds.), Perspectives on marital interaction (pp. 31–52). Clevedon, UK: Multilingual Matters. [Google Scholar]
- Christensen A, & Heavey CL (1990). Gender and social structure in the demand/withdraw pattern of marital conflict. Journal of Personality and Social Psychology, 59, 73–81. 10.1037/0022-3514.59.1.73 [DOI] [PubMed] [Google Scholar]
- Christensen A, & Shenk JL (1991). Communication, conflict, and psychological distance in nondistressed, clinic, and divorcing couples. Journal of Consulting and Clinical Psychology, 59, 458–463. 10.1037/0022-006X.59.3.458 [DOI] [PubMed] [Google Scholar]
- Christensen A, & Sullaway M (1984). Communication patterns questionnaire. Unpublished manuscript, University of California, Los Angeles. [Google Scholar]
- Cook JM, Riggs DS, Thompson R, Coyne JC, & Sheikh JI (2004). Posttraumatic stress disorder and current relationship functioning among World War II ex-prisoners of war. Journal of Family Psychology, 18, 36–45. 10.1037/0893-3200.18.1.36 [DOI] [PubMed] [Google Scholar]
- Davila J, Bradbury TN, Cohan CL, & Tochluk S (1997). Marital functioning and depressive symptoms: Evidence for a stress generation model. Journal of Personality and Social Psychology, 73, 849–861. 10.1037/0022-3514.73.4.849 [DOI] [PubMed] [Google Scholar]
- Erbes CR, Meis LA, Polusny MA, & Compton JS (2011). Couple adjustment and posttraumatic stress disorder symptoms in National Guard veterans of the Iraq war. Journal of Family Psychology, 25, 479–487. 10.1037/a0024007 [DOI] [PubMed] [Google Scholar]
- Erbes CR, Meis LA, Polusny MA, Compton JS, & Wadsworth SM (2012). An examination of PTSD symptoms and relationship functioning in U.S. soldiers of the Iraq war over time. Journal of Traumatic Stress, 25, 187–190. 10.1002/jts.21689 [DOI] [PubMed] [Google Scholar]
- Evans L, Cowlishaw S, Forbes D, Parslow R, & Lewis V (2010). Longitudinal analyses of family functioning in veterans and their partners across treatment. Journal of Consulting and Clinical Psychology, 78, 611–622. 10.1037/a0020457 [DOI] [PubMed] [Google Scholar]
- Evans L, Cowlishaw S, & Hopwood M (2009). Family functioning predicts outcomes for veterans in treatment for chronic posttraumatic stress disorder. Journal of Family Psychology, 23, 531–539. 10.1037/a0015877 [DOI] [PubMed] [Google Scholar]
- Fredman SJ (2010). Couple/family-based assessment strategies for individuals with psychological problems In Hahlweg K, Grawe-Gerber M, & Baucom DH (Eds.), Enhancing couples: The shape of couple therapy to come (pp. 185–198). Göttingen, Germany: Hogrefe. [Google Scholar]
- Fredman SJ, Monson CM, Schumm JA, Adair KC, Taft CT, & Resick PA (2010). Associations among disaster exposure, intimate relationship adjustment, and PTSD symptoms: Can disaster exposure enhance a relationship? Journal of Traumatic Stress, 23, 446–451. 10.1002/jts.20555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM (1994). What predicts divorce? The relationship between marital processes and marital outcomes. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Hahlweg K, Kaiser A, Christensen A, Fehm-Wolfsdorf G, & Groth T (2000). Self-report and observational assessment of couples’ conflict: The concordance between the Communication Patterns Questionnaire and the KPI Observation System. Journal of Marriage and the Family, 62, 61–67. 10.1111/j.1741-3737.2000.00061.x [DOI] [Google Scholar]
- Heyman RE (2001). Observation of couple conflicts: Clinical assessment applications, stubborn truths, and shaky foundations. Psychological Assessment, 13, 5–35. 10.1037/1040-3590.13.1.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooley JM (2007). Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology, 3, 329–352. 10.1146/annurev.clinpsy.2.022305.095236 [DOI] [PubMed] [Google Scholar]
- Hooley JM, & Teasdale JD (1989). Predictors of relapse in unipolar depressives: expressed emotion, marital distress, and perceived criticism. Journal of Abnormal Psychology, 98, 229–235. 10.1037/0021-843X.98.3.229 [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Kaniasty K, & Norris FH (2008). Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. Journal of Traumatic Stress, 21, 274–281. 10.1002/jts.20334 [DOI] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, & Stone E (2006). Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology, 36, 2980–2992. 10.1111/j.0021-9029.2006.00138.x [DOI] [Google Scholar]
- Kurdeck LA (1994). Conflict resolution styles in gay, lesbian, heterosexual nonparent, and heterosexual parent couples. Journal of Marriage and the Family, 56, 705–722. 10.2307/352880 [DOI] [Google Scholar]
- Lambert JE, Engh R, Hasbun A, & Holzer J (2012). Impact of posttraumatic stress disorder on the relationship quality and psychological distress of intimate partners: A meta-analytic review. Journal of Family Psychology, 26, 729–737. 10.1037/a0029341 [DOI] [PubMed] [Google Scholar]
- Macdonald A, Pukay-Martin ND, Wagner A, Fredman SJ, & Monson CM (2016). Cognitive-behavioral conjoint therapy for PTSD improves various PTSD symptoms and trauma-related cognitions: Results from a randomized controlled trial. Journal of Family Psychology, 30, 157–162. 10.1037/fam0000177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masland SR, & Hooley JM (2015). Perceived criticism: A research update for clinical practitioners. Clinical Psychology: Science and Practice, 22, 211–222. 10.1111/cpsp.12110 [DOI] [Google Scholar]
- Miller MW, Wolf EJ, Reardon AF, Harrington KM, Ryabchenko K, Castillo D, … Heyman RE (2013). PTSD and conflict behavior between veterans and their intimate partners. Journal of Anxiety Disorders, 27, 240–251. 10.1016/j.janxdis.2013.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, & Fredman SJ (2012). Cognitive-behavioral conjoint therapy for posttraumatic stress disorder: Harnessing the healing power of relationships. New York, NY: Guilford Press. [Google Scholar]
- Monson CM, Fredman SJ, & Dekel R (2010). Posttraumatic stress disorder in an interpersonal context In Beck JG (Ed.), Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment (pp. 179–208). Washington, DC: American Psychological Association. [Google Scholar]
- Monson CM, Fredman SJ, Macdonald AM, Pukay-Martin ND, Resick PA, & Schnurr PP (2012). Effect of cognitive-behavioral couple therapy for PTSD: A randomized controlled trial. Journal of the American Medical Association, 308, 700–709. 10.1001/jama.2012.9307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson CM, Price JL, Rodriguez BF, Ripley MP, & Warner RA (2004). Emotional deficits in military-related PTSD: An investigation of content and process disturbances. Journal of Traumatic Stress, 17, 275–279. 10.1023/B:JOTS.0000029271.58494.05 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2012). Mplus user’s guide (7th ed.). Los Angeles, CA: Author. [Google Scholar]
- Nunnink SE, Goldwser G, Afari N, Nievergelt CM, & Baker DG (2010). The role of emotional numbing in sexual functioning among veterans of the Iraq and Afghanistan wars. Military Medicine, 175, 424–428. 10.7205/MILMED-D-09-00085 [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Campbell SB, Meis L, & Erbes C (2014). Gender differences in the associations of PTSD symptom clusters with relationship distress in U.S. Vietnam veterans and their partners. Journal of Traumatic Stress, 27, 1–8. 10.1002/jts.21916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggs DS, Byrne CA, Weathers FW, & Litz BT (1998). The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. Journal of Traumatic Stress, 11, 87–101. 10.1023/a:1024409200155 [DOI] [PubMed] [Google Scholar]
- Riggs DS, Rothbaum BO, & Foa EB (1995). A prospective examination of symptoms of posttraumatic stress disorder in victims of nonsexual assault. Journal of Interpersonal Violence, 10, 201–214. 10.1177/0886260595010002005 [DOI] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, & Walsh W (1992). A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic stress, 5, 455–475. 10.1007/BF00977239 [DOI] [Google Scholar]
- Sautter FJ, Glynn SM, Cretu JB, Senturk D, & Vaught AS (2015). Efficacy of structured approach therapy in reducing PTSD in returning veterans: A randomized clinical trial. Psychological Services, 12, 199–212. 10.1037/ser0000032 [DOI] [PubMed] [Google Scholar]
- Sautter FJ, Glynn SM, Thompson KE, Franklin L, & Han X (2009). A couple-based approach to the reduction of PTSD avoidance symptoms: Preliminary findings. Journal of Marital and Family Therapy, 35, 343–349. 10.1111/j.1752-0606.2009.00125.x [DOI] [PubMed] [Google Scholar]
- Snyder DK, Heyman RE, & Haynes SN (2005). Evidence-based approaches to assessing couple distress. Psychological Assessment, 17, 288–307. 10.1037/1040-3590.17.3.288 [DOI] [PubMed] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, & Monson CM (2011). Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology, 79, 22–33. 10.1037/a0022196 [DOI] [PubMed] [Google Scholar]
- Taylor SE, Klein LC, Lewis BP, Gruenewald TL, Gurung RA, & Updegraff JA (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107, 411–429. 10.1037/0033-295x.107.3.411 [DOI] [PubMed] [Google Scholar]
- Census Bureau US. (2004). 2000 Census of Population and Housing: Population and Housing Unit Counts, United States Summary. Washington, DC: Author. [Google Scholar]
- Weathers FW, Litz BT, Herman JA, Huska JA, & Keane TM (1993, October). The PTSD Checklist (PCL): Reliability, validity and diagnostic utility. Paper presented at the 9th annual conference of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Whisman MA, & Baucom DH (2012). Intimate relationships and psychopathology. Clinical Child and Family Psychology Review, 15, 4–13. 10.1007/s10567-011-0107-2 [DOI] [PubMed] [Google Scholar]


