Abstract
Background:
Undescended testes, which are defined as the failure of testes to descend to scrotum, are the most common developmental defect in male infants. Indirect evaluation of histologic damage can be performed with the help of palpation during operation. Hard texture of testes tissue is likely related with histological damage. Real-time elastography is an emerging technology of ultrasonic imaging of soft tissue strain and elasticity, it aims at providing information regarding the mechanical properties of tissues, such as their hardness or stiffness. This study aim was to investigate the changes in strain and elasticity of testes tissue by using elastography technique.
Materials and methods:
A total of 32 patients, who had undescended testes were included in this study. Only two patients had bilateral undescended testes, other patients had unilateral. The age of the patients were recorded according to the time of ultrasonographic (USG) examination. The undescended testes was displayed in the elastographic box with the neighbouring subcutaneous fat tissues. The strain ratios were measured as the ratios of the elasticities of the subcutaneous fat tissue to the elasticities of the undescended testes.
Results:
A total of 32 patients with 34 testes were included in the study. The mean age of the patients with undescended testes was 32.6 months (range 7–60 months). The mean strain ratios were 0.67 (range 0.12–1.41) for the undescended testes and there were no significant differences in undescended testes strain ratios related to patient age (p = 0.453).
Conclusion:
This preliminary study showed that there were no significant fibrosis which can be demonstrated with elastosonography before the age of 5 years old. Additional studies with his-topathological results are needed to identify sensitivity and specificity of elastosonography in undescended testis and in planning optimal operation time for these patients.
Keywords: elastosonography, fibrosis, undescended testis
Introduction
Undescended testes (UDT), which are defined as the failure of testes to descend to scrotum, are the most common developmental defect in male infants. It is recorded in 30% of preterm infants compared with 3% of term infants [1]. The failure of the testicular descent can occur anywhere along the pathway. Previous studies have shown that ultrasound (USG) is the best imaging method to localize nonpalpable testes and it has advantages of being noninvasive and without radiation exposure [2,3,4]. Most UDT will descend spontaneously with age, but surgery is the most accepted treatment for those testes that remain unde-scended after 9 months of age [5,6]. Histological changes in UDT may not be reversed by orchiopexy and result in infertility or cancer [7,8], Therefore, UDT requires early recognition due to the associated reduction in fertility and increased risk of malignancy [9]. Testicular biopsy is the gold-standard to show histological changes [10] but surgeons generally avoided biopsy in children, because of its safety risks [11,12]. Indirect estimation of histological changes can be made preoperatively by measuring testis volume using USG and intraoperative evaluation of testis hardness can be measured by palpation. Real-time elasto-sonography (EUS) is an emerging technology of USG imaging of soft tissue strain and elasticity which aims at providing information regarding the mechanical properties of tissues, such as their hardness or stiffness.
The aim of this study was to investigate the strain and elasticity changes of inguinal canal located UDT according to patient age by using EUS.
Materials and methods
All children with UDT who had USG between January 2015 and December 2015 in our radiology department were included in this study. The diagnosis of UDT and normal testis was determined with physical examination by experienced pediatrists on the week of USG. We excluded children with testicular mass, inguinal hernia, epididymo-orchitis, previous hormone treatment history, or other inflammatory lesion that could affect the testis elasticity.
The EUS examinations were performed by a radiologist with 15 years experience. The examinations were performed using a sonographic scanner (Aplio 500, Toshiba Medical Systems Corporation, Tokyo, Japan) with a 15-MHz linear probe on which real-time tissue elastography software had been installed. The B-mode USG and EUS were performed with patients lying in the supine position. Age at the time of USG was recorded. After detecting UDT, volumes of both testes were calculated by using the maximum length, width, and height measures obtained from the USG. The EUS was performed by applying slight compression to the testis with the ultrasound probe. The pressures and speeds of the manual compressions were adjusted to view the subcutaneous fat tissue as a mix of red and green. Both the B-mode and elastographic images were displayed on the screen during the EUS. The UDT was displayed in the elastographic box with the neighbouring subcutaneous fat tissues in all patients. At least five bars of the indicator should be active to indicate optimal compression. The strain ratios were calculated by measuring the ratios of elasticities of subcutaneous fat tissue to elasticities of UDT tissue. The diameter of the region of interest (ROI) was taken as the centre of the UDT (Figure 1). The strain ratio was automatically calculated by the USG device. Informed consent was taken from the participant’s family.
Figure 1.
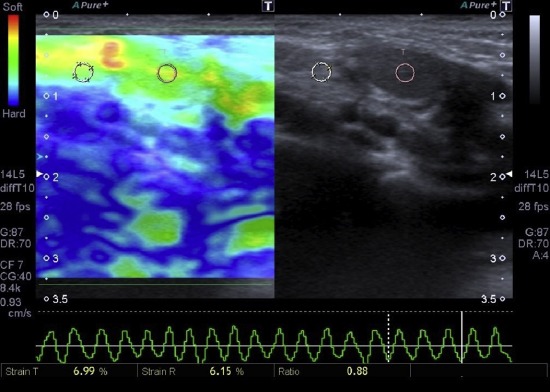
Strain elastosonographic image of 8-month-old boy with undescended testis. The strain ratio between testis and neighboring adipose tissue is 0.88, when the region of interest was placed.
Statistical analysis
All statistical analyses were performed using SPSS software, version 18.0 (SPSS Inc. Chicago, IL, USA). Descriptive data were given as means and standard deviations. Correlation between age (month) and strain ratio value was assessed with the Pearson coefficient for normally distributed data. A p value < 0.05 was considered statistically significant.
Results
A total of 32 patients with 34 testes (30 palpable, 4 non-palpable) were included in the study. Two patients had bilateral and the others unilateral UDT. None of these testes were retractile. The mean age of the patients with UDT was 32.65 months (range 7–60 months). In unilateral cases the right side [n = 16 (53%)] was the most affected side compared with the left side [n = 14 (47%)]. Upon USG, testis volume (p = 0.199) was not statistically different between UDT and normal testis. The mean volume for UDT was 0.39 mm3, the mean volume of the normal testes was 0.40 mm3. The mean strain ratios were 0.67 (range 0.12–1.41) for the UDT and there were no significant differences between undescended testes strain ratios belonging to patient age (month) (p= 0.453).
Discussion
In this study, there was no significant differences in testicular volume between undescended and normal testis. Also there were no statistically difference detected in undescended testes strain ratios belonging to patient age (month).
UDT is simply defined as the absence of testes in the scrotum. Significant histological changes in patients with UDT were shown [13]. Furthermore, several studies noted testicular fibrosis in adults with a history of cryptorchidism [14,15]. It would not be surprising to see fibrosis in an abnormal testis. Although fibrosis can be evaluated easily in histological sections of UDT, surgeons generally avoided biopsy in children, because of its safety risks.
Current urology guidelines state that USG, computerised tomography (CT), and magnetic resonance imaging (MRI) do not provide any additional information to the physical examination of palpable testes [16]. However, USG is the most widely used imaging modality to evaluate UDT because of its easy availability and noninvasiveness. Over the past few decades, USG technology has advanced with newer transducers having a greater resolution power to distinguish testes from adjacent tissues [17]. The EUS allows the assessment of tissue elastic properties, by using different techniques including strain EUS, shear wave EUS, and acoustic radiation force EUS. Assessment of UDT with EUS was first studied by Agladioglu et al [18]; in this study strain EUS technique was used to differentiate UDT from reactive lymph nodes. As in our study, in Agladioglu’s, the strain ratios were measured between subcutaneous fat tissue and UDT. In Agladioglu’s study, 0.25 (range 0.11–0.45) was found as the mean strain ratio for UDT. The difference strain ratios between their study and this current study may be due to the heterogenity of patient’s age in this study. Another study by Hattapoglu et al [19] demonstrated the difference in stiffness between scrotally placed testes and UDT by using shear wave EUS technique. They evaluated UDT in postoperative period. Both studies reviewed the usability and effectiveness of EUS in UDT. But in literature there were no data regarding the relation between the testis strain or elasticity and patient age.
In literature there are no data regarding the optimal age for orchiopexy although many recent findings suggest that early intervention (< 1 years of age) is most beneficial. Given the high rate of spontaneous descent during the first months of life, surgery of UDT diagnosed at birth should probably not be performed before 6 months of age [20]. Operation in bilateral UDT led to a normal sperm count in 76% of the men if surgery was performed between 10 months and 3 years of age, compared with 26% (9–51%) following surgery between 4 years and 14 years of age [21,22]. Operation at an early age will also decrease the risk of testicular cancer [20]. A review of pertinent studies revealed that men with a history of UDT had a 1.5–7.5-fold higher risk of testicular carcinoma in comparison to the normal population. When orchidopexy is not performed until the age of 10 years or later, this risk is elevated 2.9–32-fold [23].
Limitations of our study are as followed: (1) small number of patient group; (2) no patients over 60 months of age; (3) no histopathological correlation; (4) location of UDT were only in inguinal canal; (5) using operator-depended semiqualitative EUS technique (strain EUS); and (6) obtaining distorted strain ratio measurements because of mobile UDT located in the inguinal canal.
According to this study, although EUS is useful and reliable for assessing tissue fibrosis and elasticity, there were no significant fibrosis in UDT that was reflected to strain EUS before 5 years of age. Additional studies that include a large number of patients with histopathological correlation and using quantitative EUS techniques such as shear wave elastography are essential to detect UDT tissue elasticity according to patient age. As with additional studies, EUS can be a useful imaging modality for planning the optimal operation time in patients with UDT.
Acknowledgments
Thanks for providing language help and writing assistance to Dr Mustafa Gök.
Footnotes
Conflicts of interest: The author has no conflict of interest to declare.
References
- [1].John Radcliffe Hospital Cryptorchidism Study Group. Crypt-orchidism: a prospective study of 7500 consecutive male births, 1984–8. Arch Dis Child. 1992;67:892–9. doi: 10.1136/adc.67.7.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Christensen JD, Dogra VS. The undescended testis. Semin Ultrasound CT MR. 2007;28:307–16. doi: 10.1053/j.sult.2007.05.007. [DOI] [PubMed] [Google Scholar]
- [3].Tasian GE, Copp HL. Diagnostic performance of ultrasound in nonpalpable cryptorchidism: a systematic review and meta-analysis. Pediatrics. 2011;127:119–28. doi: 10.1542/peds.2010-1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Tasian GE, Copp HL, Baskin LS. Diagnostic imaging in crypt-orchidism: utility, indications, and effectiveness. J Pediatr Surg. 2011;46:2406–13. doi: 10.1016/j.jpedsurg.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hutson JM, Hasthorpe S. Abnormalities of testicular descent. Cell Tissue Res. 2005;322:155–8. doi: 10.1007/s00441-005-1126-4. [DOI] [PubMed] [Google Scholar]
- [6].Gill B, Kogan S. Cryptorchidism. Current concepts. Pediatr Clin North Am. 1997;44:1211–27. doi: 10.1016/s0031-3955(05)70554-x. [DOI] [PubMed] [Google Scholar]
- [7].Comploj E, Pycha A. Diagnosis and management of cryptor-chidism. Eur Urol Suppl. 2012;11:2–9. [Google Scholar]
- [8].Hadziselimovic F. Cryptorchidism, its impact on male fertility. Eur Urol. 2002;41:121–3. doi: 10.1016/s0302-2838(01)00040-9. [DOI] [PubMed] [Google Scholar]
- [9].Esposito C, Escolino M, Savanelli A, et al. Ultrasonography is unnecessary and misleading in evaluating boys with a non-palpable testis and can be a cause of a legal process. Med Sci Law. 2013;53:247–8. doi: 10.1177/0025802413481013. [DOI] [PubMed] [Google Scholar]
- [10].Patel RP, Kolon TF, Huff DS, et al. Testicular microlithiasis and antisperm antibodies following testicular biopsy in boys with cryptorchidism. J Urol. 2005;174:2008–10. doi: 10.1097/01.ju.0000176480.93985.37. [DOI] [PubMed] [Google Scholar]
- [11].Schlegel PN, Su L. Physiological consequences of testicular sperm extraction. Hum Reprod. 1997;12:1688–92. doi: 10.1093/humrep/12.8.1688. [DOI] [PubMed] [Google Scholar]
- [12].Swerdlow AJ, Higgins CD, Pike MC. Risk of testicular cancer in cohort of boys with cryptorchidism. BMJ. 1997;314:1507–11. doi: 10.1136/bmj.314.7093.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Suskind A, Hayner-Buchan A, Feustel P, et al. Fibrosis correlates with detailed histological analysis of human unde-scended testes. BJU Int. 2008;101:1441–5. doi: 10.1111/j.1464-410X.2007.07406.x. [DOI] [PubMed] [Google Scholar]
- [14].Amat P, Paniagua R, Montero J. Seminiferous tubule degeneration in human cryptorchid testes. J Androl. 1985;6:1–9. doi: 10.1002/j.1939-4640.1985.tb00810.x. [DOI] [PubMed] [Google Scholar]
- [15].Gotoh M, Miyake K, Mitsuya H. A study on cryptorchidism. II. Light and electron microscopic study of the seminiferous tubular wall in the testes of cryptorchid patients. Hinyokika Kiyo. 1984;30:349–62. [PubMed] [Google Scholar]
- [16].Haid B. Undescended testis: current treatment guidelines. Urologe. A2016;55:10–8. doi: 10.1007/s00120-015-0002-4. [DOI] [PubMed] [Google Scholar]
- [17].Tasian GE, Yiee JH, Copp HL. Imaging use and cryptorchidism: determinants of practice patterns. J Urol. 2011;185:1882–7. doi: 10.1016/j.juro.2010.12.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Agladioglu K, Herek D, Herek O, et al. Can ultrasound elas-tography be used as a new technique in the differentiation of undescended testes and reactive lymph nodes in children? Clin Radiol. 2015;70:1269–75. doi: 10.1016/j.crad.2015.06.099. [DOI] [PubMed] [Google Scholar]
- [19].Hattapoglu S, Göya C, Arslan S, et al. Evaluation of postoperative undescended testicles using point shear wave elastography in children. Ultrasonics. 2016;72:191–4. doi: 10.1016/j.ultras.2016.08.012. [DOI] [PubMed] [Google Scholar]
- [20].Ritzen EM, Bergh A, Bjerknes R, et al. Nordic consensus on treatment of undescended testes. Acta Paediatr. 2007;96:638–43. doi: 10.1111/j.1651-2227.2006.00159.x. [DOI] [PubMed] [Google Scholar]
- [21].Taskinen S, Hovatta O, Wikstrom S. Early treatment of cryptorchidism, semen quality and testicular endocrinology. J Urol. 1996;156:82–4. [PubMed] [Google Scholar]
- [22].Engeler DS, Hosli PO, John H, et al. Early orchiopexy: prepu-bertal intratubular germ cell neoplasia and fertility outcome. Urology. 2000;56:144–8. doi: 10.1016/s0090-4295(00)00560-4. [DOI] [PubMed] [Google Scholar]
- [23].Chan E, Wayne C, Nasr A. Ideal timing of orchiopexy: a systematic review. Pediatr Surg Int. 2014;30:87–97. doi: 10.1007/s00383-013-3429-y. [DOI] [PubMed] [Google Scholar]


