Abstract
Background:
Ultrasound has become an increasingly utilized tool for the imaging of the musculoskeletal system, especially for imaging the components of the knee. Even though MRI is touted as being the golden standard for identifying knee pathologies, the use of ultrasound has gained popularity in this field given its ability for rapid diagnosis. This study aims to investigate the efficacy of point-of-care ultrasound (POCUS) to diagnose injuries to the medial knee compartment when compared to magnetic resonance imaging (MRI).
Methods:
This was a prospective, observational study conducted at an orthopedic outpatient clinic. Prospective patients with medial knee pain scheduled for an MRI of the knee were evaluated by POCUS prior to the MRI. Sonographic findings were then compared to MRI results to assess correlation.
Results:
Nine patients were enrolled in the study. Median age was 53 years and eight were male (89%). POCUS demonstrated 100% sensitivity and 50% specificity for medial meniscus tear and 67% sensitivity and 83% specificity for medial collateral ligament (MCL) tear.
Conclusion:
Ultrasound may have a role as the initial rapid imaging modality in patients with suspected medial meniscus or MCL tears as it is highly sensitive, and it may serve as an effective screening tool for patients with both acute and chronic knee pain.
Keywords: Point-of-care-ultrasound (POCUS), Musculoskeletal ultrasound, Medial meniscal injury, Medial collateral ligament injury
Introduction
Magnetic resonance imaging (MRI) has historically been considered to be the golden standard imaging modality to diagnose medial knee injuries. However, there are significant limitations of using MRI, such as the presence of indwelling cardiac pacemakers, metal implants, patient intolerance due to claustrophobia and delay in treatment due to long wait periods [1,2,3]. As a result, recent studies have demonstrated point-of-care ultrasound (POCUS) as an alternative, non-invasive and real-time imaging modality to evaluate the soft tissue pathology of the knee, including injuries to the medial meniscus and medial collateral ligament (MCL) [3,4,5,6,7,8].
One of the most common mechanisms for knee injury is direct trauma, which is commonly seen in athletic injuries [3]. When injury occurs, the superficial MCL is the most commonly damaged ligament of the knee, usually induced by valgus stress, and can occasionally be accompanied by a tear in the medial meniscus [4,9]. While clinical examination is essential in diagnosing tears of the medial compartment of the knee, imaging is often required to make a conclusive diagnosis [3]. An accurate and rapid diagnosis of injury to the MCL or medial meniscus is important to determine the treatment plan and whether surgical intervention will be necessary [2]. While there is literature to support the efficacy of ultrasound in identifying medial knee pathology, there is a paucity of literature that directly compares POCUS to MRI. The primary aim of this study was to determine the accuracy of POCUS in diagnosing medial meniscus and MCL injuries when compared to MRI.
Materials and methods
Study design
This study was a prospective, observational study conducted at an orthopedic outpatient clinic. The study was approved by the site’s Institutional Review Board and was compliant with the Health Insurance Portability and Accountability Act (HIPAA).
Patient recruitment
Prospective patients were identified and enrolled into the study by the lead clinical investigator, a Sports Medicine fellowship-trained family medicine physician. Patients presenting with acute (days), intermittent (months), or chronic (years) pain in the medial compartment of the knee were considered eligible for enrollment. Medial knee pain was based on history and physical exam findings. Inclusion criteria consisted of age 18 years and older, presence of medial knee pain, and plan for an MRI to be obtained of the knee for the first time. Exclusion criteria consisted of age younger than 18 years, knee pain outside the medial compartment, or having previously undergone MRI evaluation of the knee.
Following history and physical examination, patients deemed eligible were approached for inclusion into the study. Patients who were scheduled for an MRI of the knee were invited to participate in the study. A total of nine patients were enrolled in the study. All enrolled patients underwent a POCUS, performed at bedside by the lead investigator upon initial presentation to the clinic. These images were interpreted prior to patients undergoing MRI evaluation. The MRI was at a community imaging facility with 1.5T MRI scanner. The scan protocol consisted of standard MRI sequencing for evaluation of knee pathology, consisting of multi-planar images in all orientations: sagittal, coronal, and axial. Spatial resolution was maximized using small field-of-views (14–16 cm), thin slices (3 mm) and a high matrix size. All MRI studies were read by both an independent, licensed musculoskeletal radiologist and then later by the study’s lead clinical investigator. Lead investigator for the study is a board certified, fellowship trained, primary care sports medicine specialist with seven years of practice experience and one year of ultrasound training. The lead investigator was blinded to the results of the MRI until the ultrasound had been performed and simultaneously read to maintain adequate blinding.
Ultrasound procedure technique
Each ultrasound study was performed using a SonoSite M-turbo machine (FUJIFILM Sonosite Inc, Bothell WA) with a 6–15 MHz linear probe. For examination of the medial knee, the patient was asked to rotate the leg externally while maintaining 20°–30° of knee flexion. The transducer was placed obliquely over the long-axis of the medial collateral ligament (Fig. 1). Care was taken to examine the entire length of the medial collateral ligament (Fig. 2). A normal MCL is seen in a longitudinal plane as a thick hyperechoic and fibrillar structure, extending from the medial femoral condyle to the proximal tibia. If a tear of the MCL was noted, the degree of tear was classified using the following designation: Grade 1 (Mild; stretching of the ligament without discontinuity of the fibers and associated edematous changes), Grade 2 (Moderate; partial disruption of the ligament), Grade 3 (Severe; complete discontinuity of the ligament fibers and/or retraction). The medial joint line was also assessed for joint effusion, bony abnormalities, and medial meniscus pathology. Bony abnormalities assessed included: osteophytic changes, chondrocalcinosis present at the joint line seen as hyperechoic changes with shadowing. The medial meniscus was assessed for tears, noting the potential for a peri-meniscal cyst, meniscal cleft, extrusion, degeneration, and/or calcification (Fig. 3). Meniscal degeneration was noted as a diffuse and ill-defined pattern of hypoechoic changes. Meniscal tearing was noted as a well-defined anechoic or hypoechoic disruption and/or cleft. Meniscal cysts were noted as anechoic or hypoechoic cystic structures found within the substance of the meniscus. Care was taken to not mistake a normal semimembranosus tendon structure for a meniscal cyst. Meniscal extrusion was noted as abnormal displacement of meniscal tissue and associated edema. It was also noted if the patient experienced pain with transducer placement on the medial compartment.
Figure 1.

Evaluation of the medial compartment of the knee using a linear ultrasound probe.
Figure 2.
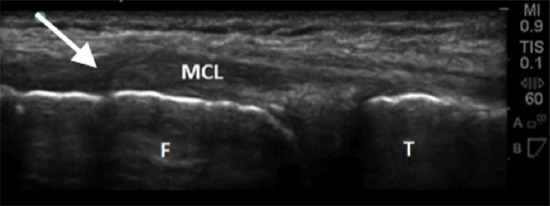
Ultrasound image of proximal MCL tear (arrow), noting ligament tissue disruption with retraction. Both the distal femur (F) and proximal tibia (T) are depicted with the adjoining MCL.
Figure 3.
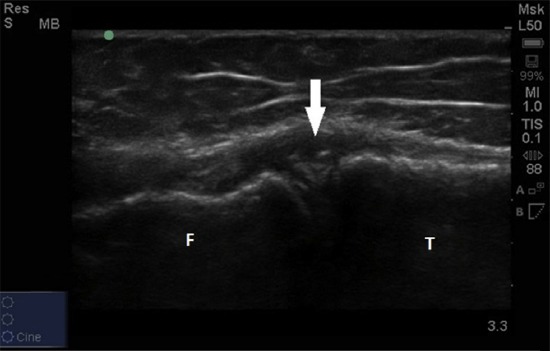
Ultrasound image of medial meniscus tear with fragmentation (arrow). The distal femur (F) and proximal tibia (T) are depicted.
Statistical analysis
Study data was entered in Excel (Microsoft, Redmond WA) and analyzed using Stata statistical software package (version 12.1, Statacorp, College Station TX). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated and reported.
Results
A total of nine patients were enrolled in the study. Median age was 53 years and eight were male (89%). The time to obtain MRI following initial evaluation ranged from three to seventeen days with a median of four days. Mechanism of injury, time from injury to evaluation, clinical presentation and physical exam findings are listed in Table 1.
Table 1.
Summary of initial patient evaluations (n = 9).
| Patient | Mechanism of injury | Time from injury to evaluation | Clinical presentation | Positive physical exam findings | Radiographic findings |
|---|---|---|---|---|---|
| 1 | Twisted on planted foot playing soccer |
2 months | Intermittent pain and soreness with activity |
Limited ROM with extension, increased translation on Lachman, medial joint tenderness, +McMurray |
Mild degenerative changes |
| 2 | Playing basketball, no acute event |
4 months | Persistent, progressive pain in anteromedial patellar compartment and medial knee, feels apprehension with planting and twisting |
Apprehension to full extension, medial joint pain, medial patellar facet pain, +McMurray |
Mild medial joint space sclerosis, prior Osgood-Schlatter diagnosis |
| 3 | Playing football, valgus pressure on medial aspect of knee while crouched down |
14 months | Intermittent knee pain with activity, difficulty with running and climbing stairs |
Tenderness to palpation at climbing stairs medial joint space, increased translation with valgus stress, +McMurray |
No bony abnormalitiess |
| 4 | Collided with a tree while snowboarding |
7 years | Persistent pain, recurrent swelling, limping, decreased ROM |
Decreased ROM at patello- femoral compartment, decreased ROM with extension, slight increased translation with MCL valgus stress, restricted McMurray |
Age appropriate tri- compartmental degenerative changes, and bony ossification at the proximal MCL |
| 5 | Playing basketball, slipped and fell in valgus position |
2 days | Acute pain, swelling in medial compartment, general knee dysfunction |
Localized soft tissue swelling and ecchymosis at medial compartment, increased translation with valgus stress, tenderness over MCL |
No bony abnormalities |
| 6 | Playing basketball, landed from jump and felt knee instability |
4 months | Persistent pain at medial compartment, inability to resume activities |
Mild apprehension on patella testing, mild joint space pain, +Lachman, þanterior drawer, +McMurray |
No bony abnormalities |
| 7 | Snowboarding, hit a rail in mid-air and fell down |
1 month | Persistent medial knee pain, discomfort with activity |
Hesitancy with full flexion, +bounce test at medial compartment, medial joint space pain, +McMurray |
No bony abnormalities |
| 8 | Auto collision with direct impact to medial compartment of s left knee |
2 years | Intermittent pain, difficulty with ambulation, mild swelling |
Medial facet tenderness, apprehension with full flexion, pain at mid and posteromedial joint space,+McMurray |
Mild amount of medial joint space narrowing and sclerosis with small osteophytic changes |
| 9 | Felt sharp pain while running |
1 month | Intermittent pain with activity, increased pain at end of the day |
Medial joint line tenderness, fullness along medial aspect, +McMurray |
No bony abnormalities |
* The McMurray test is a rotational exam that can reveal meniscal tears. The Lachman/anterior drawer test is a clinical exam used to test the stability of the anterior cruciate ligament (ACL). The bounce test evaluates the limitation of knee extension and can possibly reveal meniscal tears. ROM = range of motion; MCL = medial collateral ligament; ACL: anterior cruciate ligament.
Malanga GA, Andrus S, Nadler SF, et al. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil 2003;84(4):592-603.
While the majority of POCUS and MRI findings of medial meniscus and MCL correlated, there were three comparisons without agreement. In two instances, POCUS demonstrated tears (1 medial meniscus, 1 MCL) while MRI did not. In a separate instance, MRI identified an old MCL tear that the ultrasound image did not detect. The complete list of POCUS and MRI findings are listed in Table 2.
Table 2.
Comparison of ultrasound and MRI findings for individual patients.
| Patient | Ultrasound findings | MRI findings | Agreement | Time to MRI from initial evaluation(days) |
|---|---|---|---|---|
| 1 | Mild degenerative medial meniscus tearing Normal MCL |
Bucket handle tear of medial meniscus Normal MCL |
Yes | 5 |
| 2 | Tear of posterior cleft of medial meniscus Normal MCL |
Horizontal tear of peripheral posterior horn and posterior body of medial meniscus Normal MCL |
Yes | 7 |
| 3 | Tear of cleft of medial meniscus Thickening of proximal MCL due to prior tear |
Normal medial meniscus Thickening of proximal MCL due to prior tear |
No | 4 |
| 4 | Small tear of cleft of medial meniscus Proximal MCL thickening and calcific change due to grade I tear |
Complex tear of body and posterior horn of medial posterior horn of medial meniscus with communication to inner free edge to inner free edge to inner Normal MCL |
No | 4 |
| 5 | Normal medial meniscus Proximal grade I MCL tear |
Normal medial meniscus Grade II MCL tear |
Yes | 17 |
| 6 | Small tear of cleft mid- posterior medial meniscus Normal MCL |
Tear of posterior horn medial menisco-capsular Chronic MCL thickening |
No | 3 |
| 7 | Tear of cleft of medial meniscus Normal MCL |
Posterior horn medial meniscus tear Normal MCL |
Yes | 7 |
| 8 | Tear of cleft and posterior horn of medial meniscus Normal MCL |
Tear of posterior horn and mid- zone of medial meniscus Normal MCL |
Yes | 3 |
| 9 | Tear of cleft and posterior horn of medial meniscus Normal MCL |
Complex tear of posterior horn of medial meniscus Normal MCL |
Yes | 3 |
MCL = medial collateral ligament.
Overall, POCUS demonstrated 100% sensitivity and 50% specificity for medial meniscus tear, yielding a positive predictive value (PPV) of 87.5% and a negative predictive value (NPV) of 100%. Ultrasound was also able to show a 67% sensitivity and 83% specificity with a similar PPV of 67% and NPV of 83% for MCL tears. After combining medial meniscus and MCL tears, POCUS had a sensitivity of 90%, specificity of 75% for identifying these injuries.
Discussion
Using ultrasound for the diagnosis of medial knee injuries confers several benefits. It is a non-invasive, cost-efficient bedside procedure that allows for real-time diagnosis and early management of injuries. Ultrasound offers a dynamic assessment of joint pathology, allowing for rapid detection of fractures, structural anomalies, torn ligaments, fluid, infection, and other osteoarthritic injuries [1,10]. This provides a great time benefit to both the patient and the physician. It is an economical imaging modality that is less costly and faster to obtain than an MRI study [11]. The portability of the equipment facilitates bedside scanning without the inconvenience of transporting patients. However, along with these advantages, there are also limitations to using ultrasound. There is a relatively steep learning curve and dependence on the training, skill, and experience of the operator [7]. Given operator-dependence, results may lack standardization in assessing knee pathology. Nonetheless, studies conducted more recently have demonstrated higher sensitivities and specificities of ultrasound in diagnosing medial meniscus tears, which may be attributed in technology and increased operator training [2].
When using ultrasound to visualize a normal medial meniscus, a hyperechoic, homogenous triangle or wedge-shaped structure can be seen [1,7,12,13,14]. Sonographic findings of meniscal tears include a hypoechoic band or stripe that can be seen within the meniscus, resulting in heterogeneity of the meniscus [4,7,8,14]. The size and shape of the hypoechoic band will vary depending on the size, shape, and location of the meniscal tear. It should be noted that the posterior horn is usually larger than the anterior horn, and it is easier to visualize tears in the outer margin of the medial meniscus compared to the inner margin due to it being more superficial [7].
In this study, meniscal horn tears, especially those posteriorly, were identified on ultrasound. However, in one patient (Patient 3), a meniscal tear was seen on ultrasound that did not appear on MRI, thus affecting specificity. These findings are consistent with other studies that have evaluated ultrasound as a diagnostic tool for meniscal injuries. A large study performed by Grifka et al. analyzing 1196 ultrasound images showed an 83% sensitivity and a 90% specificity for medial meniscus tears [15]. This is confirmed with several other studies that find the overall examination sensitivity and specificity to range from 83 to 97.2% and 83 to 100%, respectively [15,16,17]. In addition, negative predictive value for using ultrasound to diagnose these medial meniscal injuries is 94.4% [17]. Another study by Cook et al. showed that the use of ultrasonography proved to be two times more likely to correctly diagnose displaced vertical longitudinal tears, which was confirmed with arthroscopy, when compared to MRI [2]. This study had a sensitivity and specificity of 91.2% and 84.2%, respectively. In our study, use of ultrasound was limited in one patient who had a bucket-handle tear (Patient 1), as the definitive diagnosis was missed using ultrasonography. Bucket handle tears are longitudinal tears separating the inner and outer portion of the meniscus in the anterior–posterior axis. They are difficult to visualize due to their depth as the tear occurs on the inner rim of the medial meniscus [7].
In theory, visualizing the MCL under ultrasound is relatively easy due to its superficial location, spanning from the medial femoral condyle to the medial tibial metaphysis. The MCL has two layers, a superficial and deep layer, with the deep layer being continuous with the medial meniscus. Because of this continuity of the deep layer of the MCL with the medial meniscus, they are often injured together. Both the layers of the MCL are sonographically hyperechoic structures and are separated by a hypoechoic band, consisting of areolar tissue. This gives the MCL a trilaminar structure with the hyperechoic outer parts and a hypo-echoic inner part [7,8,9,18,19]. However, when injured, the trilaminar appearance is often lost and the MCL becomes hypoechoic and heterogenous, thought to be due to edema. The injured MCL also appears thicker when compared to the normal MCL [4,7,8,19]. One study by Kleinbaum et al., which measured normal and abnormal MCL thickness on ultrasound, showed that the average respective thickness of the injured MCL at the proximal and distal attachments was 6.4 and 4.4 mm, while that of the normal MCL was 4.3 and 3.1 mm [9].
Our study had only three patients with potential MCL pathology on MRI, with one having chronic MCL changes that were missed on ultrasound (Patient 6). This suggests the limited role ultrasound may have in evaluating chronic ligamentous injuries. Data on the sensitivity and specificity of ultrasound use in diagnosing MCL tears is not as abundant as in meniscal injuries. A study of 200 patients with primarily traumatic knee injuries and a clinical indication for arthroscopy demonstrated a small proportion with MCL tears [20]. The sensitivity and specificity of using ultrasound to diagnose these tears was 66% and 50%, respectively. Despite the low sensitivity of diagnosing old ligamentous injuries, there is great utility in diagnosing acute injuries immediately as treatment can be initiated sooner. Additionally, when MCL tears are diagnosed, grading of these tears can be up to 94% accurate when using ultrasound [7].
The main limitation of our study was the low number of subjects that were enrolled. Only nine patients over the course of one year were enrolled in this study due to the study setting being an orthopaedic referral center, where patients either have a known existing condition or have received an MRI prior to initial evaluation. However, this was simply an observational pilot study. A larger sample size is needed to be able to establish a true observational study. This can be done by enrolling patients from a wider range of settings, such as emergency departments, prior to referral to an orthopedist. Another limitation, as stated above, is the lack of a standardized protocol to diagnose MCL and medial meniscus tears. This leads to operator-dependence of performing and interpreting the scan, which is subjective and variable. In our study, all scans and their interpretation were solely performed by the lead investigator, eliminating inter-rater variability. There may have been some bias present from the lead investigator given that the patients enrolled were already scheduled for an MRI, indicating either a severe enough or long-standing injury. Thus, perhaps there was an increased amount of time and attention spent scanning with the ultrasound probe looking for pathology, yielding higher quality images. However, for the confines of this study and given the lack of standardized protocol, we had to accept the presence of this bias. MRI scanning was also performed at three different imaging facilities, increasing the variability in sequencing and image interpretation. Despite these limitations, our study showed that POCUS appears to be an accurate and reliable initial diagnostic modality to evaluate for medial meniscus and MCL injury. While it is not currently a substitute for MRI, future large-scale studies should evaluate the use of POCUS as a screening tool to potentially eliminate the need for a costly and time-consuming confirmatory MRI in select cases.
Acknowledgments
Melika Hosseini, BS: UC Irvine School of Medicine.
Nicolas Salvatierra, BS: UC Irvine School of Medicine.
Footnotes
Conflicts of interest: There are no conflicts of interest to report.
References
- [1].Blankstein A. Ultrasound in the diagnosis of clinical orthopedics: the orthopedic stethoscope. World J Orthop. 2011;2(2):13–24. doi: 10.5312/wjo.v2.i2.13. http://dx.doi.org/10.5312/wjo.v2.i2.13 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Cook JL, Cook CR, Stannard JP, et al. MRI versus ultrasonography to assess meniscal abnormalities in acute knees. J Knee Surg. 2014;27(4):319–32. doi: 10.1055/s-0034-1367731. http://dx.doi.org/10.1055/s-0034-1367731 . [DOI] [PubMed] [Google Scholar]
- [3].Nadafi J, Bagheri S, Abdolahzedeh L. The value of sonography with micro convex probes in diagnosing meniscal tears compared with arthroscopy. J Ultrasound Med. 2006;25(5):593–7. doi: 10.7863/jum.2006.25.5.593. http://www.jultrasoundmed.org/content/25/5/593.long . [DOI] [PubMed] [Google Scholar]
- [4].Artul S, Khazin F, Hakim J, et al. Ultrasonographic findings in a large series of patients with knee pain. J Clin Imaging Sci. 2014;4(45) doi: 10.4103/2156-7514.139735. http://dx.doi.org/10.4103/2156-7514.139735 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bruyn G, Moller I, Klauser A, et al. Soft tissue pathology: regional pain syndromes, nerves and ligaments. Rheumatology. 2012;51(7):vii22–5. doi: 10.1093/rheumatology/kes330. http://dx.doi.org/10.1093/rheumatology/kes330 . [DOI] [PubMed] [Google Scholar]
- [6].Friedman L, Finlay K, Jurriaans E. Ultrasound of the knee. Skelet Radiol. 2001;30(7):361–77. doi: 10.1007/s002560100380. http://dx.doi.org/10.1007/s002560100380 . [DOI] [PubMed] [Google Scholar]
- [7].Lee D, Bouffard J. Ultrasound of the knee. Eur J Ultrasound. 2001;14(1):57–71. doi: 10.1016/s0929-8266(01)00146-x. http://dx.doi.org/10.1016/S0929-8266(01) 00146-X . [DOI] [PubMed] [Google Scholar]
- [8].Razek A, Fouda N, Elmetwaley N, et al. Sonography of the knee joint. J Ultrasound. 2009;12(2):53–60. doi: 10.1016/j.jus.2009.03.002. http//dx.doi.org/10.1016/j.jus.2009.03.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kleinbaum Y, Blankstein A. Mild to moderate medial collateral ligament (MCL) injuries of the knee: sonographic findings and sonographic valgus stress test. J Musculoskelet Res. 2008;11(1):9–14. http://dx.doi.org/10.1142/S0218957708001912 . [Google Scholar]
- [10].Iagnocco A. Imaging the joint in osteoarthritis: a place for ultrasound? Best Pract Res Clin Rheumatol. 2010;24(1):27–38. doi: 10.1016/j.berh.2009.08.012. [DOI] [PubMed] [Google Scholar]
- [11].Abraham AM, Goff I, Pearce MS, et al. Reliability and validity of ultrasound imaging of features of knee osteoarthritis in the community. BMC Musculoskelet Disord. 2011;12:70. doi: 10.1186/1471-2474-12-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Descamps M, Lim A, Mitchell A. Ultrasound examination of the knee: an illustrated guide. Ultrasound. 2008;16(1):43–7. http://dx.doi.org/10.1179/174313407X215219 . [Google Scholar]
- [13].Kahn Z, Faruqui Z, Ogyunbiyi O, et al. Ultrasound assessment of internal derangement of the knee. Acta Orthop. 2006;72(1):72–6. www.actaorthopaedica.be/acta/download/2006-1/14-Khan.pdf . [PubMed] [Google Scholar]
- [14].Gerngross H, Sohn C. Ultrasound scanning for the diagnosis of meniscal lesions of the knee joint. Arthrosc J Arthrosc Relat Surg. 1992;8(1):105–10. doi: 10.1016/0749-8063(92)90143-y. http://dx.doi.org/10.1016/0749-8063(92)90143-Y . [DOI] [PubMed] [Google Scholar]
- [15].Grifka J, Richter J, Gumtau M. Clinical and sonographic meniscus diagnosis. Der Orthopade. 1994;23(2):102–11. www.ncbi.nlm.nih.gov/pubmed/8190501 . [PubMed] [Google Scholar]
- [16].Shanbhogue AK, Sandhu MS, Singh P, et al. Real time spatial compound ultrasound in the evaluation of meniscal injuries: a comparison study with conventional ultrasound and MRI. Knee. 2009;16(3):191–5. doi: 10.1016/j.knee.2008.10.010. [DOI] [PubMed] [Google Scholar]
- [17].Wareluk P, Szopinski KT. Value of modern sonography in the assessment of meniscal lesions. Eur J Radiol. 2012;81(9):2366–9. doi: 10.1016/j.ejrad.2011.09.013. [DOI] [PubMed] [Google Scholar]
- [18].Acebe C, Romero F, Contreras M, et al. Dynamic ultrasound assessment of medial meniscal subluxation in knee osteoarthritis. Rheumatology. 2013;52(8):1443–7. doi: 10.1093/rheumatology/ket110. Lee et al. Medial collateral ligament injuries of the knee: ultrasonographic findings. J Ultrasound Med. 1996 Sep;15(9): 621-5. http://dx.doi.org/10.1093/rheumatology/ket110 . [DOI] [PubMed] [Google Scholar]
- [19].Chew K, Stevens K, Wang T-G, et al. Introduction to diagnostic musculoskeletal ultrasound: Part 2: examination of the lower limb. Am J Phys Med Rehabil. 2008;87(3):238–48. doi: 10.1097/PHM.0b013e31816198c2. http//dx.doi.org/10.1097/PHM.0b013e31816198c2 . [DOI] [PubMed] [Google Scholar]
- [20].Najafi J, Abdolahzedeh Lahiji F, Bagheri S. The diagnostic value of sonography in bucket handle tear of meniscus and complete MCL tear compared with arthroscopy. Iran J Radiol. 2005;3(1):103–6. www.sid.ir/EN/VEWSSID/J_pdf/98020060206.pdf . [Google Scholar]


