Abstract
Background
Timely and adequate laryngeal elevation along with hyoid bone movement is an essential component of the swallowing movement under normal physiological conditions. The purpose of this study was to verify the reproducibility of using ultrasonography to evaluate hyoid bone displacement during swallowing through the assessment of inter- and intrarater reliability and examine its accuracy by comparing the results with videofluoroscopic swallowing study (VFSS).
Methods
A self-designed water balloon was fixed to the transducer, which provided good contact between the transducer and the submental skin. Ten participants with dysphagia were recruited. The measurements of hyoid bone displacement using ultrasonography were performed by two of the authors. All the participants underwent ultrasonographic examinations and VFSS within 24 hours.
Results
The intrarater intraclass correlation coefficient (ICC) of the two examiners was 0.996 and 0.959, respectively (p < 0.01); the interrater ICC between the two examiners was 0.892 (p < 0.05). ICCs between VFSS and ultrasonography for two researchers were 0.815 and 0.916 (p < 0.01).
Conclusion
Submental ultrasonography is a reliable and accurate method for assessing the hyoid bone movement.
KEYWORDS: dysphagia, hyoid bone, swallowing disorder, ultrasonography, ultrasound
Introduction
Swallowing disorders or dysphagia may result from anatomical abnormalities in the oral cavity, pharynx, larynx, or esophagus or from physiologic disturbances in the control of these structures. These disorders may be congenital or caused by trauma, anatomical abnormalities, or neurological damage of sudden or gradual origin [1,2,3,4,5,6]. Dysphagia may result in malnutrition, dehydration, aspiration pneumonia, and even death [1,2].
Timely and adequate laryngeal elevation along with hyoid bone movement is an essential component of the swallowing movement under normal physiologic conditions [7,8]. Laryngeal elevation ensures occlusion of the larynx and the subsequent opening of the cricopharyngeal muscle [7,9,10]. The upward and forward displacement of the hyoid bone, mediated by the coordinated contraction of the suprahyoid muscles and the relaxation of the infrahyoid muscles, is one of the major contributors to the above-mentioned process [9,10,11].
The most suitable method of screening for dysphagia still remains controversial, although videofluoroscopy is generally regarded as the gold standard [12]. Videofluoroscopy spatial measurements of the hyoid and larynx elevation have been used in large groups of healthy volunteers [13,14]. However, there are concerns about radiation exposure. Moreover, these studies use various consistencies of barium sulfate, which is quite different from real food. Recently, various kinetic high-speed magnetic resonance imaging sequences have been applied to examine some of the anatomical and functional properties of deglutition [15]. However, owing to severe movement artifacts, this technique is not capable of providing exact distance measurements [15].
To circumvent these disadvantages, ultrasonographic techniques have also been applied to the evaluation of hyoid bone movement during swallowing [16,17,18,19,20]. However, most of them lacked the assessment of intra- and interrater reliability [16,17,18] or the comparison with videofluoroscopic swallowing study (VFSS) [16,17,18]. The purpose of this study was to verify the reproducibility of using ultrasonography to evaluate hyoid bone displacement during swallowing through the assessment of inter- and intrarater reliability and examine its accuracy by comparing the results with VFSS.
Materials and methods
Participants
This study was approved by the Ethics Committee of National Taiwan University Hospital, Taipei City, Taiwan. Written informed consent was obtained from each participant. Between May 2016 and August 2016, patients admitted to our hospital with dysphagia, who were conscious and adequately cooperated, were recruited for this study. Participants underwent a clinical examination by a speech therapist, who graded them using the functional oral intake scale (FOIS). FOIS was designed with good reliability, validity, and sensitivity to changes in the swallowing function to document the functional oral intake of individuals with dysphagia [21]. All the participants underwent ultrasonographic examination and VFSS within 24 hours.
Ultrasonographic examination
This study used a self-designed ultrasonographic machine with a curvilinear transducer (Convex Array, 3.5 MHz, P701-C04; LELTEK Corporation, Taipei City, Taiwan). The machine was connected to a laptop computer, placed on a cart, and could be easily used at bedside (LT701 ultrasonographic machine, LT701-000; LELTEK Corporation). The result of each ultrasonographic examination was recorded as a series of dynamic images. Images were recorded at a frame rate of 30/s. Connection of the machine to the laptop enabled prompt storage of the dynamic images.
Participants were assessed when sitting upright comfortably, with their heads leaning back on the chair. The transducer was placed in the midsagittal plane at the submental area (Figure 1A). We capped a self-designed water bag on the transducer to improve the contact between the skin and the transducer (Figure 1B, C). Participants were instructed to hold their head steady during swallowing. Each participant swallowed 5 mL of water for each attempt and repeated it three times. Their hyoid bone movement during swallowing was recorded. The best-recorded images of the three attempts were later analyzed frame by frame to determine the maximum displacement of the hyoid bone from the resting position.
Figure 1.

Submental ultrasonographic examination. (A) The transducer is held in the vertical midsagittal plane at the mandible angle. (B) A self-designed water-filled probe cap, which enables tight and comfortable contact between the submental skin and the transducer. (C) The water balloon could be securely fixed onto the transducer.
The measurements of hyoid bone displacement using ultrasonography were performed by two of the authors. To examine intrarater reliability, each of the two examiners conducted the ultrasonographic measurement on the same participants two times, with an interval of > 48 hours. To examine the interrater reliability, the first measurements conducted by the two researchers were compared with one another. To examine the accuracy, the first measurements conducted by each of the two researchers were separately compared with VFSS. Figure 2 shows the structures observed in the submental ultrasonography at the midsagittal plane. The position of the mandible and the hyoid bone was determined using the acoustic shadows. The mandible was used as the reference point to calculate the hyoid bone displacement (Figure 3A). The reference point was defined as the anterior border of the bottom of the acoustic shadow of the mandible. Using a two-axis coordinate system, the position of the hyoid bone in relation to the mandible in each frame was represented as coordinate pairs. The distance between two coordinates before and during swallowing denoted the hyoid bone displacement (Figure 3B).
Figure 2.
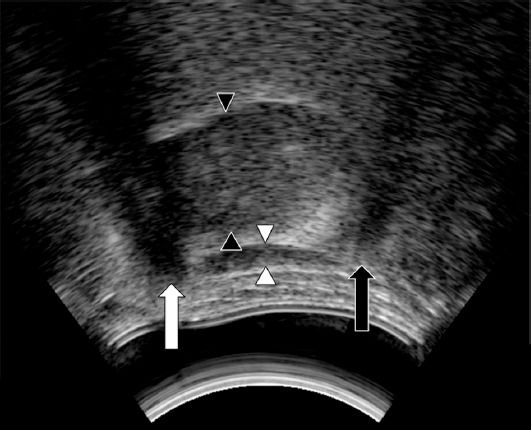
Submental midsagittal ultrasonography image. It shows acoustic shadows behind the hyoid bone (black arrow) and the mandible (white arrow); between them are the suprahyoid muscles (between the white arrowheads). The tongue is above the suprahyoid muscles (between the black arrowheads).
Figure 3.
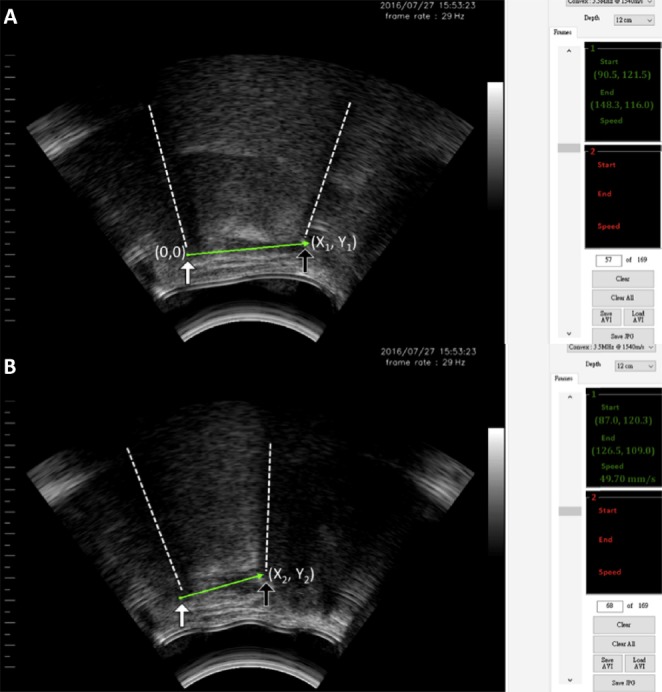
Calculation of the hyoid bone displacement using a self-designed program. (A) The mandible (white arrow) and the hyoid bone (black arrow) were located at the intersections of the acoustic shadows (dashed lines) and suprahyoid muscles. Using a two-axis coordinate system and the mandible as the reference point, the position of the hyoid bone was designated a pair of coordinates (X1, Y1). (B) During swallowing, the recorded images were analyzed frame by frame to determine the maximal displacement of the hyoid bone from the resting position. The new position of the hyoid bone (black arrow) was designated as X2, Y2, with the mandible (white arrow) as the reference point. The distance between the two coordinates before and after swallowing denoted the hyoid bone displacement.
The software employed in this study was developed using the C Sharp programming language (Microsoft Visual Studio 2015; Microsoft, Redmond, WA, USA).
VFSS
All the participants underwent VFSS within 24 hours of the ultrasonographic examination. VFSSs were conducted at our institute using fluoroscopic equipment with a remote control and a high-resolution super-VHS recorder at a frame rate of 30 frames/s. During the examination, participants swallowed 5 mL of thin barium sulfate. The anterior superior margin of the fourth cervical vertebral body was used as the reference point for calculating the hyoid bone displacement. The initial position of the hyoid bone was marked, and the displacement relative to the reference point was calculated frame by frame to determine the maximum hyoid bone displacement during swallowing.
The hyoid bone displacements observed in VFSS were measured using MATLAB (version 7.5.0, R2007b; MathWorks, Inc., Boston, MA, USA).
Statistical analysis
Statistical tests were conducted using SPSS software (SPSS Statistics 20.0; SPSS Inc., Chicago, IL, USA). The intra- and interrater reliability of the submental ultrasonography measurements of changes in hyoid bone displacement were assessed using the intraclass correlation coefficient (ICC). An ICC of < 0.4 indicated poor reproducibility, 0.4–0.7 indicated fair-to-good reproducibility, and > 0.7 indicated excellent reproducibility [22]. To test the accuracy, hyoid bone displacements measured using submental ultrasonography were also compared with those measured using VFSS and whose ICC were calculated.
Results
Participants’ demographic data are shown in Table 1. Of the 10 patients (10 men; mean age, 71.8 years; range, 54–81 years), four had stroke, one had neuromuscular disease, one had traumatic brain injury, one had chronic obstructive pulmonary disease, one had spinal cord injury, one had aspiration pneumonia, and one had gastroesophageal reflux disease. The mean FOIS score was 3. Of the 10 patients, four were dependent on tube feeding and six on oral intake. All the patients underwent VFSS within 24 hours of ultrasonography examination. The hyoid bone displacements of each participant measured by ultrasonography and VFSS were displayed in Table 2.
Table 1.
Basic demographic data.
| Case | Age (y) | Sex | Diagnosis | FOIS | NG tube |
|---|---|---|---|---|---|
| 1 | 54 | Male | Stroke | 2 | Yes |
| 2 | 54 | Male | Neuromuscular disease | 4 | No |
| 3 | 66 | Male | Stroke | 3 | Yes |
| 4 | 69 | Male | Traumatic brain injury | 5 | No |
| 5 | 78 | Male | COPD | 6 | Yes |
| 6 | 79 | Male | Stroke | 2 | No |
| 7 | 69 | Male | Spinal cord injury | 2 | Yes |
| 8 | 80 | Male | Aspiration pneumonia | 2 | Yes |
| 9 | 88 | Male | GERD | 1 | No |
| 10 | 81 | Male | Stroke | 5 | No |
Mean age: 71.8 years, standard deviation: 10.9.
COPD = chronic obstructive pulmonary disease; FOIS = functional oral intake scale; GERD = gastroesophageal reflx disease; NG tube = nasogastric tube.
Table 2.
The hyoid bone displacements (in cm) measured by ultrasonography (US) and videofluoroscopic swallowing study (VFSS).
| Case | Author 1 US | Author 2 US | VFSS |
|---|---|---|---|
| 1 | 1.844 | 1.625 | 1.570 |
| 2 | 1.441 | 1.292 | 1.258 |
| 3 | 1.800 | 1.600 | 1.774 |
| 4 | 2.088 | 2.081 | 1.933 |
| 5 | 1.728 | 1.219 | 1.342 |
| 6 | 1.535 | 1.544 | 1.765 |
| 7 | 1.727 | 1.583 | 1.548 |
| 8 | 1.082 | 1.005 | 1.241 |
| 9 | 1.201 | 1.125 | 1.121 |
| 10 | 1.913 | 1.737 | 1.783 |
The intrarater ICC of the hyoid bone displacement of the two examiners was 0.996 and 0.959 (p < 0.01), respectively (Table 3); the interrater ICC between the two examiners was 0.892 (p < 0.05; Table 4). ICCs between VFSS and ultrasonography for two researchers were 0.815 and 0.916, respectively (p < 0.01; Table 5).
Table 3.
Intrarater intraclass correlation coefficient.
| r | p | |
|---|---|---|
| Author 1 | 0.996 | <0.01 |
| Author 2 | 0.959 | <0.01 |
Table 4.
Interrater intraclass correlation coefficient.
| Author 1 | Author 2 | |
|---|---|---|
| Author 1 | 1 | 0.892* |
| Author 2 | 0.892* | 1 |
* p < 0.05.
Table 5.
Pearson’s correlation coefficient between ultrasonography (US) and videofluoroscopic swallowing study (VFSS).
| VFSS | p | |
|---|---|---|
| Author 1 US | 0.815 | <0.01 |
| Author 2 US | 0.916 | <0.01 |
n = 10.
Discussion
The results demonstrated that submental ultrasonography has good intra- and interrater reliability in the measurements of hyoid bone displacement. Regarding previous studies, Chi-Fishman and Sonies [16] used ultrasonography for observing the swallowing process. They successfully calculated the maximal distance, velocity, and duration of the hyoid bone movement for different swallowing tasks. Later, Yabunaka et al [17] used hand-held ultrasonography to observe the hyoid bone movement during the swallowing process. By tracing the position of the hyoid bone during swallowing frame by frame, the trajectory of the hyoid bone movement was depicted. However, neither intra- nor interreliability was assessed in either of the studies. Our study assessed both the intra- and interrater reliability and found good reproducibility.
Our results also demonstrated that submental ultrasonography has good accuracy in the measurement of hyoid bone displacement when compared with VFSS. Most previous studies using ultrasonography to observe the pharyngeal phase of swallowing did not compare their results with VFSS [16,17,18,23]. The study conducted by Huang et al [19] was the first to compare ultrasonographic examination of hyoid–larynx approximation with VFSS. They used B-mode ultrasonography to measure hyoid–larynx approximation as a parameter to estimate laryngeal elevation. The measurement of the distance between the hyoid bone and the thyroid cartilage using ultrasonography was compared with VFSS in 10 of the dysphagic stroke patients who underwent both the examinations. However, the approximate distance measured using ultrasonography (1.41 ± 0.35 cm) was significantly different from that measured using VFSS (0.88 ± 0.44 cm; p = 0.008). The difference may arise from the lack of an exact reference material in an ultrasonographic setting [19]. The study conducted by Hsiao et al [20] used mandible as the reference point to calculate the hyoid bone displacement. No significant difference existed between the results provided by submental ultrasonography and those by VFSS, with a p value of 0.266 and an ICC of 0.804. Hsiao et al [20] recruited 60 stroke patients and 40 healthy participants for the study sample; however, only 12 stroke patients underwent both VFSS and submental ultrasonography. Although our study tested only 10 participants, our study group represented various disease characteristics and provided a more heterogeneous population for testing the reliability. Our participants underwent VFSS and ultrasonography, and the results showed good accuracy. No significant difference existed between the results provided by submental ultrasonography and those by VFSS, with a p value of 0.437.
Previous studies on using ultrasonography to assess swallowing function often encountered difficulties in maintaining good skin–transducer contact during the swallowing examination. Peng et al [24] created a buffer area between the transducer and the skin by placing a bag filled with water to avoid accidental transducer movement during swallowing. However, the bag was unstable. We solved this problem by fixing a self-designed water balloon to the transducer, which was more pliable, stable, and easier to maneuver, and thus provided good contact between the transducer and the submental skin.
This work supported the idea that submental ultrasonography is both a reliable and an accurate tool in the assessment of hyoid bone displacement. The upward and forward displacement of the hyoid bone, mediated by the coordinated contraction of the suprahyoid muscles and the relaxation of the infrahyoid muscles, is one of the major contributors in the occlusion of the larynx and the stretching open of the cricopharyngeal muscle during the swallowing process [7,8,9,10,11]. Submental ultrasonography enables visualization of the hyoid bone displacement in the pharyngeal phase, thereby aiding in bedside evaluations of swallowing function among patients with differing diagnoses. In addition to the degree of the hyoid bone movement, the timing and velocity of the hyoid bone movement are also important for airway protection. Neither was investigated in this study. Our next study will examine these parameters, and focus on specific patient groups such as nasopharyngeal carcinoma, neuromuscular disease, etc.
This study has several limitations. First, this study used a limited sample size. Further large-scale studies are required to verify the reproducibility and accuracy of submental ultrasonography. Second, only male participants were recruited. Finally, the self-designed software employed in this study may not be applicable to all the ultrasonographic machines.
Conclusion
Using the self-designed ultrasonographic machine combined with a transducer capped with a water-filled cushion and self-designed program, we demonstrated that submental ultrasonography is a reliable and accurate method for assessing the hyoid bone movement and could aid in dysphagia screening and evaluation.
Footnotes
Conflicts of interest: All authors declare no conflicts of interest.
References
- [1].Martino R, Foley N, Bhogal S, et al. Dysphagia after stroke incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63. doi: 10.1161/01.STR.0000190056.76543.eb. [DOI] [PubMed] [Google Scholar]
- [2].Cook IJ. Oropharyngeal dysphagia. Gastroenterol Clin North Am. 2009;38:411–31. doi: 10.1016/j.gtc.2009.06.003. [DOI] [PubMed] [Google Scholar]
- [3].Edwards LL, Quigley EM, Pfeiffer RF. Gastrointestinal dysfunction in Parkinson's disease: frequency and pathophysiology. Neurology. 1992;42:726–32. doi: 10.1212/wnl.42.4.726. [DOI] [PubMed] [Google Scholar]
- [4].Logan WJ, Bosma JF. Oral and pharyngeal dysphagia in infancy. Pediatr Clin North Am. 1967;14:47–61. doi: 10.1016/s0031-3955(16)31942-3. [DOI] [PubMed] [Google Scholar]
- [5].Lazarus C, Logemann A. Swallowing disorders in closed head trauma patients. Arch Phys Med Rehab. 1987;68:79–84. [PubMed] [Google Scholar]
- [6].Logemann JA, Bytell DE. Swallowing disorders in three types of head and neck surgical patients. Cancer. 1979;44:1095–105. doi: 10.1002/1097-0142(197909)44:3<1095::aid-cncr2820440344>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- [7].Logemann JA. Evaluation and treatment of swallowing disorders. Nerang, QLD: Pro-Ed Australia; 1983. [Google Scholar]
- [8].Ekberg O. The normal movements of the hyoid bone during swallow. Invest Radiol. 1986;21:408–10. doi: 10.1097/00004424-198605000-00009. [DOI] [PubMed] [Google Scholar]
- [9].Cook IJ, Dodds WJ, Dantas RO. Opening mechanisms of the human upper esophageal sphincter. Am J Physiol. 1989;257:G748–59. doi: 10.1152/ajpgi.1989.257.5.G748. [DOI] [PubMed] [Google Scholar]
- [10].Sivarao D, Goyal RK. Functional anatomy and physiology of the upper esophageal sphincter. Am J Med. 2000;108:27–37. doi: 10.1016/s0002-9343(99)00337-x. [DOI] [PubMed] [Google Scholar]
- [11].Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002;17:262–72. doi: 10.1007/s00455-002-0064-5. [DOI] [PubMed] [Google Scholar]
- [12].Martino R, Pron G, Diamant N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines. Dysphagia. 2000;15:19–30. doi: 10.1007/s004559910006. [DOI] [PubMed] [Google Scholar]
- [13].Leonard RJ, Kendall KA, McKenzie S, et al. Structural displacements in normal swallowing: a videofluoroscopic study. Dysphagia. 2000;15:146–52. doi: 10.1007/s004550010017. [DOI] [PubMed] [Google Scholar]
- [14].Perlman AL, VanDaele DJ, Otterbacher MS. Quantitative assessment of hyoid bone displacement from video images during swallowing. J Speech Hear Res. 1995;38:579–85. doi: 10.1044/jshr.3803.579. [DOI] [PubMed] [Google Scholar]
- [15].Anagnostara A, Stoeckli S, Weber OM, et al. Evaluation of the anatomical and functional properties of deglutition with various kinetic high-speed MRI sequences. J Magn Reson Imaging. 2001;14:194–9. doi: 10.1002/jmri.1172. [DOI] [PubMed] [Google Scholar]
- [16].Chi-Fishman G, Sonies BC. Kinematic strategies for hyoid movement in rapid sequential swallowing. J Speech Lang Hear Res. 2002;45:457–68. doi: 10.1044/1092-4388(2002/036). [DOI] [PubMed] [Google Scholar]
- [17].Yabunaka K, Sanada H, Sanada S, et al. Sonographic assessment of hyoid bone movement during swallowing: a study of normal adults with advancing age. Radiol Phys Technol. 2011;4:73–7. doi: 10.1007/s12194-010-0107-9. [DOI] [PubMed] [Google Scholar]
- [18].Shawker TH, Sonies B, Hall TE, et al. Ultrasound analysis of tongue, hyoid, and larynx activity during swallowing. Invest Radiol. 1984;19:82–6. doi: 10.1097/00004424-198403000-00003. [DOI] [PubMed] [Google Scholar]
- [19].Huang YL, Hsieh SF, Chang YC, et al. Ultrasonographic evaluation of hyoidelarynx approximation in dysphagic stroke patients. Ultrasound Med Biol. 2009;35:1103–8. doi: 10.1016/j.ultrasmedbio.2009.02.006. [DOI] [PubMed] [Google Scholar]
- [20].Hsiao MY, Chang YC, Chen WS, et al. Application of ultrasonography in assessing oropharyngeal dysphagia in stroke patients. Ultrasound Med Biol. 2012;38:1522–8. doi: 10.1016/j.ultrasmedbio.2012.04.017. [DOI] [PubMed] [Google Scholar]
- [21].Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20. doi: 10.1016/j.apmr.2004.11.049. [DOI] [PubMed] [Google Scholar]
- [22].Nunnally JC. Psychometric theory. New York: McGraw-Hill; 1978. [Google Scholar]
- [23].Miller JL, Watkin KL. Lateral pharyngeal wall motion during swallowing using real time ultrasound. Dysphagia. 1997;12:125–32. doi: 10.1007/PL00009526. [DOI] [PubMed] [Google Scholar]
- [24].Peng CL, Jost-Brinkmann PG, Miethke RR, et al. Ultrasonographic measurement of tongue movement during swallowing. J Ultrasound Med. 2000;19:15–20. doi: 10.7863/jum.2000.19.1.15. [DOI] [PubMed] [Google Scholar]


