Abstract
Elephantiasis is a condition featured by gross enlargement of body parts to massive proportions. Neurofibromatosis type 1 (NF1) is a multisystem genetic disorder. Vascular anomaly is one among the complications of NF1. We report a case of NF1 who had a left hand vascular pseudoaneurysm with left hand swelling mimicking elephantiasis. The characteristics of sonography make it an excellent imaging modality to investigate this sort of superficial vascular lesion.
KEYWORDS: Ultrasound, Elephantiasis, Neurofibromatosis, Pseudoaneurysm
Introduction
Elephantiasis is a condition featured by gross enlargement of body parts to massive proportions. The most frequent affected areas are the limbs and the external genitals. A number of diseases such as lymphatic filariasis have been recognized to present this symptom. Neurofibromatosis type 1 (NF1) is a multisystem genetic disorder that is characterized by café-au-lait spots on the skin, skeletal dysplasias, and neurofibromas. Vascular abnormalities can also be noted as the complications of NF1. These include aneurysms, stenoses, arteriovenous malformations, fistulae, etc. We report a case of a female with long-standing NF1 who had a left hand pseudoaneurysm arising from the left ulnar artery and left hand swelling mimicking elephantiasis, and illustrate the imaging studies during diagnosis and treatment.
Case report
A 41-year-old female was diagnosed of neurofibromatosis for 20 years. She was brought to hospital due to gradually swelling of left hand. In addition, ecchymosis and objective pulsation at left hand were also found (Fig. 1). Initial ultrasonography (US) revealed a hypoechoic, well-defined saccular lesion measuring about 1.5 × 1.4 cm at palmar side of her left hand. The lesion was found connecting to the ulnar artery and Doppler spectral analysis further revealed arterial wave form. Besides, engorged veins as well as soft tissue swelling were noted at her left hand and distal forearm (Fig. 2). Computed tomography (CT) confirmed a vascular saccule at the ulnar side of wrist, consistent with an aneurysm, with adjacent hematomas and soft tissue hypertrophy (Fig. 3). Left upper limb angiography was conducted and disclosed a 1.5 cm-sized pseudoaneurysm fed by ulnar artery. The pseudoaneurysm was then treated with coil embolization successfully (Fig. 4).
Figure 1.

Swelling and discoloring of the palmar side of left hand was noted.
Figure 2.
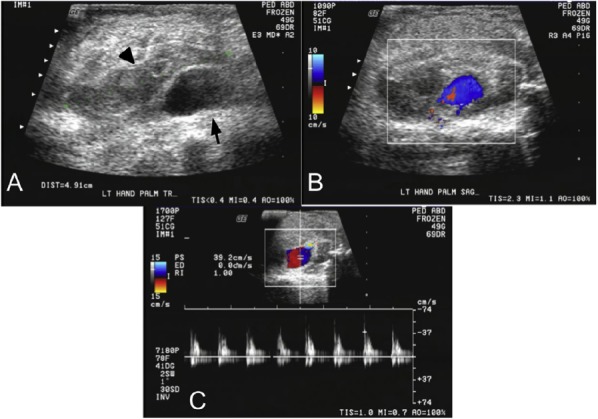
A and B, Ultrasonography showed a vascular saccule (arrow) with surrounding hematomas (arrow head) at the ulnar side of left palm. C, Color Doppler spectral analysis revealed arterial wave form in the vascular saccule.
Figure 3.

A, Computed tomography (CT) imaging before intravenous contrast media administration revealed a hypodense area (black arrow) surrounded by a relatively hyperdense structures (black arrow heads) at left palm. B and C, After intravenous contrast medium administration, the initially hypodense area was opacified (white arrow), indicative of pseudoanerysm with surrounding nonenhanced hematoma. Engorged veins (white arrow heads) and increased soft tissue in the subcutaneous fat were also noted, suggestive of subcutaneous hypertrophy (red arrowheads).
Figure 4.

A, Angiography of the left upper limb disclosed a 1.5 cm-sized pseudoaneurysm (black arrow) fed by ulnar artery at left palm. B, The pseudoaneurysm was no longer opacified with contrast media infusion (white arrow) after coil embolization was done successfully. C, Coils were placed into the pseudoaneurysm with endovascular embolization techniques.
Discussion
Neurofibromatosis type 1 (NF1), also known as von Recklinghausen’s disease, is an autosomal dominant genetic disorder caused by a mutation on chromosome 17. It is characterized by multisystemic involvement including café-au-lait spots, neurofibromas at the skin, and skeletal dysplasias [1,2]. On the other hand, though uncommon, vascular complications are a well-recognized condition induced by NF1. Vascular abnormalities usually affect medium- and large-sized vessels and may present as aneurysms, arterial stenoses, arteriovenous malformations (AVM), arteries compressed or invaded by neural tumors, and abnormalities of the heart valves. The pathogenesis, clinical spectrum, and natural history of these abnormalities are unknown [3]. Most patients with NF1 vascular abnormalities are asymptomatic but multiple vascular involvements may occur. Symptoms usually occur in childhood or early adulthood. The renal artery is the most frequent site of involvement, and renovascular hypertension is the most common presentation [4,5,6].
The patient we described presents left ulnar artery complication, which is rare in NF1 associated vascular complications while reviewing literature. Among the wide spectrum of vascular abnormalities noted in patients with NF1, ulnar arterial aneurysm is very rare. In a review of 76 vascular abnormalities in 31 patients (15 males, 16 females) with clinical NF1 and vascular abnormalities identified from imaging or operative findings between 1976 and 2005, Oderich et al. noticed that there were totally 38 aneurysms, 20 arterial stenoses, 5 arteriovenous malformations (AVM), 5 arteries compressed or invaded by neural tumors, and 6 abnormalities of the heart valves. Arterial lesions were located in the aorta (n = 17) and in the renal (n = 12), mesenteric (n = 12), carotid-vertebral (n = 10), intracerebral (n = 4), and subclavian-axillary and iliofemoral arteries (3 each). Interventions were requires in 23 patients (74%); 15 underwent 24 arterial reconstructions, including 9 renal, 8 aortic, 4 mesenteris, 2 carotid, and 1 femoral. None of the aneurysms developed in the ulnar artery [3]. Swelling and discoloring of left hand further makes the disfiguring appearance mimicking elephantiasis.
One of the characteristics of sonography being attractive is its lack of ionizing radiation, which is important in obstetric as well as pediatric patient population. Another advantage of sonography is its excellent resolution of superficial structures. That patient’s lesion locates in the hand benefits greatly from this feature. The real-time nature and Doppler techniques for qualitative and quantitative evaluation of blood flow further make sonography excellent tool to investigate the patient’s vascular anomaly. The lesion appeared to be an arterial aneurysm with typical wave form which can be easily and clearly shown with ultrasound and its Doppler spectral analysis. Ultrasound’s noninvasiveness also makes it more favorable than other image modality such as angiography. The multiplanar imaging capability of ultrasound is also critical aspect while carrying out the examination of the patient because it allows for rapid determination of the origin of pathologic mass and analysis of spatial relationships of its surrounding structures. Meanwhile, the portable nature of ultrasound makes it superior to other cross-sectional modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) [7].
Treatment of the vascular complications relies on the patient’s age and the type and location of the lesion, and may involve open surgery, endovascular techniques, or medical therapy, most notably aneurysms or stenoses of the aortic, renal, and mesenteric circulation. Operative treatment of symptomatic patients with vascular lesions or large aneurysms is safe, effective, and durable [3]. Endovascular treatment frequently provides less invasive and quicker recovery comparing to surgery [4,5], therefore it is widely adopted in many circumstances, including the patient we present here.
Because clinically significant vascular lesions are relatively uncommon (2%), selective imaging for individuals with clinical suspicion is recommended instead of periodic vascular assessment for all NF1 patients [3]. Since the patient had encountered peripheral vascular complication, systemic vascular survey would be reasonable for her.
Conclusion
Although rare, vascular manifestations are also recognized complications in NF1 patients. Any fast growing lump or swelling on the body parts, especially presents concomitantly with pulsation or bruit, should be well examined to rule out vascular anomalies. Modern image techniques provide precise diagnosis, and treatment depends on the type and the location of the disease, and the patient’s individual clinical condition.
Footnotes
Conflict of interest disclosure statement: The authors have no conflicts of interest and have received no funding in support of this work. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- [1].Onkendi E, Moghaddam MB, Oderich GS. Internal carotid artery aneurysms in a patient with neurofibromatosis type 1. Vasc Endovasc Surg. 2010;44:511–4. doi: 10.1177/1538574410369567. [DOI] [PubMed] [Google Scholar]
- [2].Seow VK, Chong CF, Wang TL, et al. Ruptured left subclavian artery aneurysm presenting as upper airway obstruction in von Recklinghausen's disease. Resuscitation. 2007;74:563–6. doi: 10.1016/j.resuscitation.2007.02.002. [DOI] [PubMed] [Google Scholar]
- [3].Oderich GS, Sullivan TM, Bower TC, et al. Vascular abnormalities in patients with neurofibromatosis syndrome type I: clinical spectrum, management, and results. J Vasc Surg. 2007;46:475–84. doi: 10.1016/j.jvs.2007.03.055. [DOI] [PubMed] [Google Scholar]
- [4].Lin AE, Birch P, Korf BR, et al. Cardiovascular malformations and other cardiovascular abnormalities in Neurofibromatosis type I. Am J Med Genet. 2000;95:108–17. doi: 10.1002/1096-8628(20001113)95:2<108::aid-ajmg4>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- [5].Friedman JM, Arbiser J, Epstein JA, et al. Cardiovascular disease in neurofibromatosis 1: report of the NF1 cardiovascular task force. Genet Med. 2002;4:105–11. doi: 10.1097/00125817-200205000-00002. [DOI] [PubMed] [Google Scholar]
- [6].Hamilton SJ, Friedman JM. Insights into the pathogenesis of neurofibromatosis 1 vasculopathy. Clin Genet. 2000;58:341–4. doi: 10.1034/j.1399-0004.2000.580501.x. [DOI] [PubMed] [Google Scholar]
- [7].William DM, Alfred BK, Barbara SH. Ultrasound. 2nd ed. St. Louis: Mosby; 2004. pp. 3–4. [Google Scholar]


