Abstract
Purpose
To compare the effectiveness of different combinations of social comparison feedback and financial incentives to increase physical activity.
Design
Randomized trial (Clinicaltrials.gov number, NCT02030080).
Setting
Philadelphia, Pennsylvania.
Participants
Two hundred eighty-six adults.
Interventions
Twenty-six weeks of weekly feedback on team performance compared to the 50th percentile (n = 100) or the 75th percentile (n = 64) and 13 weeks of weekly lottery-based financial incentive plus feedback on team performance compared to the 50th percentile (n = 80) or the 75th percentile (n = 44) followed by 13 weeks of only performance feedback.
Measures
Mean proportion of participant-days achieving the 7000-step goal during the 13-week intervention.
Analysis
Generalized linear mixed models adjusting for repeated measures and clustering by team.
Results
Compared to the 75th percentile without incentives during the intervention period, the mean proportion achieving the 7000-step goal was significantly greater for the 50th percentile with incentives group (0.45 vs 0.27, difference: 0.18, 95% confidence interval [CI]: 0.04 to 0.32; P = .012) but not for the 75th percentile with incentives group (0.38 vs 0.27, difference: 0.11, 95% CI: −0.05 to 0.27; P = .19) or the 50th percentile without incentives group (0.30 vs 0.27, difference: 0.03, 95% CI: −0.10 to 0.16; P = .67).
Conclusion
Social comparison to the 50th percentile with financial incentives was most effective for increasing physical activity.
Keywords: physical activity, social comparison, performance feedback, teams, financial incentives, behavioral economics, connected health
Purpose
Physical inactivity is a leading risk factor for cardiovascular disease.1–3 Higher levels of physical activity are associated with lower all-cause mortality,4,5 coronary artery disease,1,2,6 diabetes,7 weight gain,8 and breast and colon cancer.9,10 Yet, half of adults in the United States do not engage in enough regular physical activity to achieve health benefits.11 New strategies are needed to increase physical activity levels.12,13
Standard economics assumes that individuals make decisions that are perfectly rational, maximizing long-term value and health. However, many individuals know physical activity is good for their health, yet they do not obtain enough of it. Behavioral economics is a promising field of study that incorporates principles from psychology to help us understand why individuals often make decisions that are not in line with their longer term health goals and that they do so in a predictable manner and from common set of decision errors.14–16 For example, individuals tend to be more motivated by losses than gains,17 by immediate rather than delayed gratification,18 and by variable rewards that induce regret.19 These insights reveal that beyond just the magnitude of the incentive, the design and delivery of an incentive have an important impact on its effectiveness. Prior work has demonstrated that programs using these insights can promote weight loss,20 smoking cessation,21 and medication adherence.22 However, there has been little evaluation of programs directed at increasing physical activity.23
There is also evidence to suggest that health behaviors may be affected by social influences. In a retrospective evaluation of health behaviors among spouses, men and women had 5 times higher odds of becoming physically active if their spouse also became physically active.24 Obesity and smoking behaviors have also been found to be connected through social networks that extend beyond just family members and also to friends.25,26 Physical activity interventions have been found to be more successful when incorporating performance feedback27; however, the use of social comparison feedback has not been well examined. Although it may be common to provide feedback to the level of mean performance (50th percentile), it is unknown whether anchoring feedback to a higher level such as the top quartile (75th percentile) might have different effectiveness. The higher standard might be motivating or demotivating.
Our objective was to compare the effectiveness of different combinations of social comparison feedback and financial incentives to increase physical activity. Although many prior physical activity interventions have focused on harnessing the power of individual goal setting, we enrolled participants in teams to enhance social incentives including peer support, accountability, and unity toward a common goal.28
Methods
Design
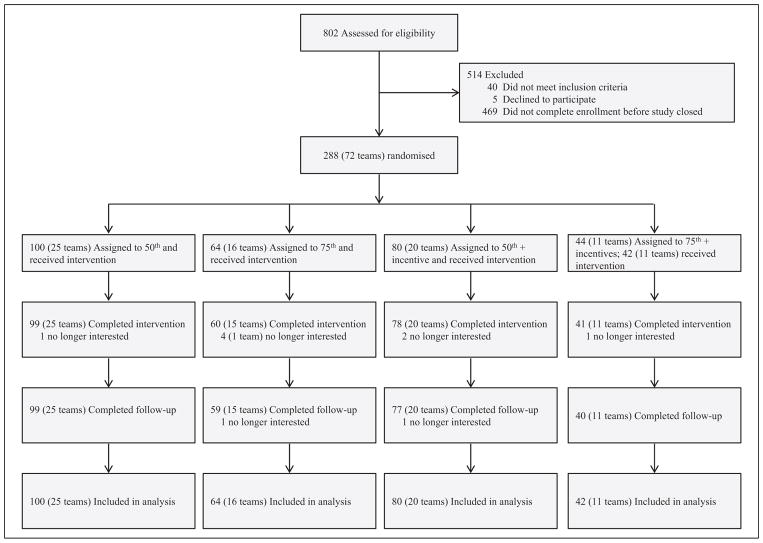
We conducted a 26-week, 2 × 2 factorial, randomized trial between March and September 2014, consisting of a 13-week intervention period and 13-week follow-up period. Two hundred eighty-eight participants gave their informed consent, formed 4-member teams, and were randomly assigned to receive 1 of 2 types of team-based performance feedback either with or without financial incentives (Figure 1). Participants were required to have an iPhone or Android smartphone that they stated they were willing to carry with them the majority of the time while enrolled in the study. Participants were asked to download, install, and give the study team permission to retrieve data from the “Moves” mobile application (ProtoGeo Oy Inc, Helsinki, Finland), which tracks step counts using accelerometers within the smartphone. After installing the application, data tracking and feedback were automated. Our prior work has demonstrated that this smartphone application accurately tracks step counts.29
Figure 1.
Trial profile.
All participants were given a goal of achieving at least 7000 steps per day, a target reflecting several deliberate design elements. First, this level of physical activity is endorsed by the American College of Sports Medicine as an evidence-based recommendation of physical activity to achieve health benefits.30,31 Second, this level is 40% higher than the average daily step count of 5000 among US adults32,33 but may not be so high as to discourage more sedentary individuals from engaging. Prior studies using a goal of 10 000 steps have found that more sedentary individuals may be less likely to participate.27 Third, instead of simply asking participants to walk more, a minimum threshold puts more emphasis on encouraging more sedentary individuals to walk and less emphasis on getting highly active individuals to be even more active. Each participant received daily individual performance feedback on whether they had successfully achieved the goal of 7000 steps on the prior day and could, if they checked their own app, gauge how many steps they had taken at any point during the day. This study was approved by institutional review board of the University of Pennsylvania.
Sample
Eligible participants were employees or family members of employees from the University of Pennsylvania Health System aged 18 or greater with an iPhone or Android smartphone. Participants were excluded if they were already participating in another physical activity study, currently pregnant or lactating, intending to become pregnant within the next 6 months, or stated for any other reasons that they did not expect to be able to complete a 6-month physical activity study.
Potential participants were instructed to form a team of 4 members and select a captain. The captain visited the study website to complete electronic informed consent and an eligibility screening questionnaire. If all eligibility criteria were met, the captain listed the names and contact information for potential team members. The captains were provided with an e-mail template they could modify and use to invite the other members of the team to visit the study website for their own consent and enrollment. The study team also sent e-mails to the potential team members informing them that a captain had invited them. If any of the team members was not interested in participating or deemed ineligible, we informed the captain of the need to identify another potential team member. All participants were asked to complete a basic sociodemographic questionnaire, self-report measures of height and weight, and report physical activity in the last 7 days using the long form of the International Physical Activity Questionnaire (IPAQ).34 The IPAQ was used to calculate the number of metabolic equivalent minutes (MET-min) per participant in the most recent 7 days. The MET is physiologic measure of energy expenditure, with light-intensity activities having an MET <3, moderate-intensity activities having an MET of 3 to 6, and more vigorous-intensity activities with an MET >6.
Measures
The study was conducted using Way to Health, an automated information technology platform that integrates wireless devices, clinical trial randomization and enrollment processes, messaging (text, e-mail, or voice), self-administered surveys, automatic transfers of financial incentives, and secure data capture for research purposes.35,36 Way to Health has been used in prior behavioral intervention studies.37–39 A computer-generated random number sequence was used to assign each team to 1 of 4 study arms using simple randomization. Participants selected whether they preferred to receive study communications via e-mail, text message, or both. Weekly feedback was sent the morning after the end of the week. Daily feedback on performance from the prior day was sent each morning. Neither the participants nor the study coordinator could be blinded to the arm assignment due to the nature of the interventions. All investigators, statisticians, and data analysts were blinded to arm assignments until the entire 26-week study period was completed.
In 2 arms, participants received weekly feedback on team performance (average number of steps per day per team member) and no financial incentives. In 1 of those arms, each team was told how their weekly average step count compared to the 50th percentile (median) in their arm (above or below, as well as average step count at that percentile). In the other arm, each team was told how their performance compared to the 75th percentile (top quartile). In the 2 financial incentives arms, teams received the same weekly performance feedback (either relative to the 50th or the 75th percentile) and were entered in a weekly regret lottery. Teams were randomly assigned a 2-digit number between 00 and 99. If the team’s number had a single-digit match with the winning number (an 18% chance), each team member was rewarded $35. If the team’s number had a 2-digit match with the winning number (a 1% chance), each team member was rewarded $350. The expected daily economic value per participant was designed to be about $1.40, a value similar to that of prior work.39 Participants were eligible to collect the reward only if their average step count per day per team member for the prior week was 7000 steps or higher. Ineligible participants were informed what they would have won had they been adherent to the goal, drawing on evidence that the desire to avoid regret can be motivating.17,19,40,41 Financial incentives were offered for 13 weeks, and then participants were followed for an additional 13 weeks. Feedback on social comparisons was delivered for the entire 26 weeks.
The primary outcome was the mean proportion of participant-days that the 7000-step goal was achieved during the intervention period (weeks 1–13). We hypothesized that participants in the financial incentive arms would have a significantly greater mean proportion achieving goal than participants in the nonfinancial incentive arms and that participants in arms receiving feedback compared to the 75th percentile would have a greater mean proportion achieving goal than participants receiving feedback compared to the 50th percentile. Secondary outcomes were the number of steps per day during the intervention period (weeks 1–13) and follow-up period (weeks 14–26) and the mean proportion of participant-days that the 7000-step goal was achieved during the follow-up period.
All participants received $25 for enrolling in the study and $75 for participating through the primary end point at 13 weeks along with the completion of a survey on their experience in the study. There was no participation incentive during the follow-up period.
Analysis
A priori, we estimated that a sample of at least 280 participants (70 per arm) would ensure 80% power to detect a 0.20 difference between each of the intervention arms and the control arm, using a conservative Bonferroni adjustment of the type I error rate using a 2-sided α of .017. A secondary comparison between each of the intervention arms would require a more conservative Bonferroni adjustment of the type I error rate using a 2-sided α of. 0083. This calculation assumed that the mean proportion of participant-days achieving goal in the control arm would be 0.40 and accounted for clustering by team with an intracluster correlation coefficient of 0.025. Since 70 teams could not be evenly distributed into 4 arms, we enrolled 288 participants to allow for 72 teams (18 teams per arm). However, simple randomization distributed teams unevenly by arm, providing less power to detect differences between arms with less than 70 participants.
Two participants were randomized but switched to phones that were not compatible with the Moves app before the study began and therefore did not receive the intervention. These 2 participants were not included in the analysis. All other participants randomly assigned to a study arm were included in the intention-to-treat analysis. The mean proportion of participant-days meeting goal and mean daily steps were estimated at the level of the team for the intervention period, the follow-up period, and for each week during the study.
In the adjusted model, generalized linear mixed models (via PROC GLIMMIX in SAS) were used to adjust for the repeated measures of daily participant step counts and to adjust the standard errors for clustering by team.42–44 Data could be missing if a participant turned off the smartphone or Moves application, disabled the study team’s permission before data were accessed, or did not carry the smartphone at all. The percentage of missing data by arm during the intervention period was 19% for the 50th percentile feedback without incentives, 25% for the 75th percentile feedback without incentives, 16% for the 50th percentile feedback with incentives, and 20% for the 75th percentile feedback with incentives. For the main analysis, we used only collected data (a step count value was received) that assume missing data occur at random and do not bias outcomes for arms with differing levels of missing data. The main model uses a binary outcome measure (0 or 1) based on achieving the goal of 7000 steps and included fixed effects for arm and week of the study period. Several sensitivity analyses were conducted to assess the robustness of our findings. The main model was further adjusted using fixed effects for smartphone type (iPhone or Android). Second, the model was also evaluated using all data and coding missing data (when a step value was not received) as not achieving goal (in contrast to using only collected data), a method used in prior work.38 For the secondary outcome of mean daily steps, the model was further adjusted using fixed effects for smartphone type (iPhone or Android). Second, evidence suggests that step count values less than 1000 are unlikely to represent accurate data capture of actual activity.33,45,46 Therefore, to avoid these observations from downward biasing mean daily step outcomes, a sensitivity analysis was conducted using the model with values less than 1000 excluded from the sample. All analyses were conducted using SAS, version 9.4 (SAS Institute, Cary, North Carolina).
Results
Figure 1 reports trial enrollment. Participants had a mean age of 41.3 years (standard deviation [SD]: 12.0 years) and using self-reported height and weight had a mean body mass index of 28.4 (SD: 6.5); 80.1% were women. The median self-reported physical activity in the 7 days prior to enrollment was 4533.3 metabolic equivalent minutes (MET-min) ; interquartile range: 2329.5–7929.0). Among all participants, 209 (73.1%) used an iPhone to track activity and 77 (26.9%) used an Android smart-phone. Baseline characteristics were similar across the 4 study arms (Table 1).
Table 1.
Characteristics of Study Participants.
| Characteristic | 50th (n = 25 Teams, 100 Participants) | 75th (n = 15 Teams, 64 Participants) | 50th + Incentives (n = 20 Teams, 80 Participants) | 75th + Incentives (n = 11 Teams, 42 Participants) |
|---|---|---|---|---|
| Female gender, n (%) | 76 (76.0) | 48 (75.0) | 69 (86.3) | 36 (85.7) |
| Age, mean (SD) | 40.9 (12.2) | 43.1 (10.5) | 40.7 (12.2) | 40.8 (13.2) |
| Self-reported baseline measures | ||||
| Body mass index, mean (SD) | 29.0 (7.4) | 28.7 (6.1) | 27.5 (5.8) | 28.5 (6.2) |
| Physical activity in the last 7 days (MET-min), median (IQR) | 4698.0 (2424.0–7740.0) | 4702.5 (2914.5–8071.5) | 4186.0 (1711.5–7173.0) | 3630.0 (2208.0–9588.0) |
| Race/ethnicity, n (%) | ||||
| White non-Hispanic | 65 (65.0) | 49 (76.6) | 50 (62.5) | 28 (66.7) |
| African American non-Hispanic | 21 (21.0) | 11 (17.2) | 15 (18.8) | 11 (26.2) |
| Other non-Hispanic | 13 (13.0) | 1 (1.6) | 12 (15.0) | 3 (7.1) |
| Hispanic | 1 (1.0) | 3 (4.7) | 3 (3.8) | 0 (0.0) |
| Education, n (%) | ||||
| Less than college | 6 (6.0) | 6 (9.4) | 4 (5.0) | 4 (9.5) |
| Some college | 16 (16.0) | 22 (34.4) | 16 (20.0) | 8 (19.0) |
| College graduate | 78 (78.0) | 36 (56.3) | 60 (75.0) | 30 (71.4) |
| Marital status, n (%) | ||||
| Single | 36 (36.0) | 25 (39.1) | 30 (37.5) | 14 (33.3) |
| Married | 55 (55.0) | 35 (54.7) | 39 (48.8) | 24 (57.1) |
| Other | 9 (9.0) | 4 (6.3) | 11 (13.8) | 4 (9.5) |
| Annual household income, n (%) | ||||
| Less than $50 000 | 19 (19.0) | 13 (20.3) | 13 (16.3) | 8 (19.0) |
| $50 000–$100 000 | 31 (31.0) | 17 (26.6) | 28 (35.0) | 20 (47.6) |
| Greater than $100 000 | 35 (35.0) | 30 (46.9) | 29 (36.3) | 12 (28.6) |
| iPhone smartphone, n (%) | 71 (71.0) | 48 (75.0) | 56 (70.0) | 34 (81.0) |
Abbreviations: IQR, interquartile range; MET-min, metabolic equivalent minutes; SD, standard deviation.
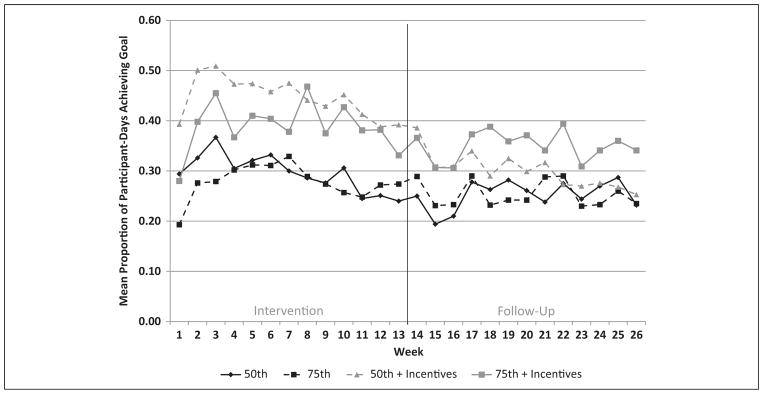
The mean proportion of participant-days achieving the 7000-step goal peaked at about 0.50 in the 50th percentile with incentives arm and 0.45 in the 75th percentile with incentives arm (Figure 2). The 75th percentile without incentives arm had the lowest performance peaking near 0.31, whereas the 50th percentile without incentives arm peaked near 0.37. These levels declined over the intervention period for all arms. Compared to the 75th percentile without incentives, the mean proportion achieving the 7000-step goal was significantly greater for the 50th percentile with incentives group (0.45 vs 0.27, difference: 0.18, 95% confidence interval [CI]: 0.04 to 0.32; P = .012) but not for the 75th percentile with incentives group (0.38 vs 0.27, difference: 0.11, 95% CI: −0.05 to 0.27; P = .19) or the 50th percentile without incentives group (0.30 vs 0.27, difference: 0.03, 95% CI: −0.10 to 0.16; P = .67). These findings were qualitatively similar in adjusted models and sensitivity analyses (Table 2). For the secondary outcome of mean daily steps, there were no statistically significant differences between any of the arms (Table 3).
Figure 2.
Unadjusted mean proportion of participant-days achieving the 7000-step goal displayed by study arm for each week of the study.
Table 2.
| Model | Arm Comparison | Intervention (Weeks 1–13) | Follow-Up (Weeks 14–26) | ||
|---|---|---|---|---|---|
|
|
|
||||
| Odds Ratio (95% CI) | P Value | Odds Ratio (95% CI) | P Value | ||
| Main model | 50th vs 75th | 1.12 (0.44–2.86) | .81 | 0.98 (0.39–2.44) | .97 |
| 50th + incentives vs 75th | 2.50 (0.96–6.67) | .06 | 1.82 (0.70–4.76) | .22 | |
| 75th + incentives vs 75th | 1.61 (0.52–5.00) | .42 | 2.08 (0.66–6.67) | .21 | |
| 50th + incentives vs 50th | 2.25 (0.95–5.33) | .06 | 1.84 (0.80–4.26) | .15 | |
| 75th + incentives vs 50th | 1.43 (0.50–4.08) | .50 | 2.13 (0.74–6.14) | .16 | |
| 50th + incentives vs 75th + | incentives 1.59 (0.53–4.76) | .41 | 0.87 (0.29–2.56) | .80 | |
| Main model—adjusted by device | 50th vs 75th | 1.12 (0.46–2.78) | .81 | 1.08 (0.50–2.33) | .85 |
| 50th + incentives vs 75th | 2.56 (1.01–6.67) | .05 | 1.35 (0.60–3.03) | .47 | |
| 75th + incentives vs 75th | 1.49 (0.50–4.55) | .48 | 1.54 (0.60–4.00) | .37 | |
| 50th + incentives vs 50th | 2.31 (1.00–5.32) | .05 | 1.25 (0.62–2.52) | .53 | |
| 75th + incentives vs 50th | 1.34 (0.48–3.69) | .58 | 1.44 (0.60–3.47) | .41 | |
| 50th + incentives vs 75th + | incentives 1.72 (0.60–5.00) | .31 | 0.87 (0.35–2.17) | .76 | |
| Main model—adjusted by device and with missing data as not meeting goal | 50th vs 75th | 1.39 (0.51–3.85) | .53 | 1.41 (0.56–3.57) | .46 |
| 50th + incentives vs 75th | 3.57 (1.25–10.00) | .02 | 1.96 (0.75–5.00) | .17 | |
| 75th + incentives vs 75th | 1.82 (0.52–6.25) | .35 | 1.32 (0.43–4.17) | .63 | |
| 50th + incentives vs 50th | 2.61 (1.01–6.71) | .05 | 1.38 (0.58–3.24) | .46 | |
| 75th + incentives vs 50th | 1.31 (0.41–4.13) | .65 | 0.93 (0.33–2.65) | .90 | |
| 50th + incentives vs 75th + | incentives 2.00 (0.61–6.67) | .26 | 1.47 (0.50–4.35) | .48 | |
Abbreviation: CI, confidence interval.
Device refers to type of smartphone.
Main model adjusts for repeated measures of daily participant step counts and for temporal trends by week using all collected data. Outcome measure is a binary term (0 or 1) based on not achieving or achieving goal.
Odds ratios represent the ratio of odds of achieving the 7000-step goal for a participant on a random day during either the intervention period (third column) or the follow-up period (fourth column) if a participant was to be assigned to the one specified study arm versus the other specified study arm.
Table 3.
Adjusted Daily Step Differences Between Study Arms During the Intervention and Follow-Up Periods.a,b
| Model | Arm Comparison | Intervention (Weeks 1–13) | Follow-Up (Weeks 14–26) | ||
|---|---|---|---|---|---|
|
|
|
||||
| Difference in Daily Steps (95% CI) | P Value | Difference in Daily Steps (95% CI) | P Value | ||
| Main model | 50th vs 75th | 374 (3706 to 1454) | .50 | 132 (3863 to 1128) | .79 |
| 50th + incentives vs 75th | 1058 (371 to 2188) | .07 | 758 (3282 to 1798) | .15 | |
| 75th + incentives vs 75th | 651 (3676 to 1978) | .34 | 884 (3381 to 2148) | .17 | |
| 50th + incentives vs 50th | 684 (3320 to 1688) | .18 | 626 (3289 to 1541) | .18 | |
| 75th + incentives vs 50th | 277 (3946 to 1499) | .66 | 752 (3412 to 1916) | .21 | |
| 50th + incentives vs 75th + incentives | 407 (3859 to 1673) | .53 | 3126 (31329 to 1076) | .84 | |
| Main model—adjusted by device | 50th vs 75th | 389 (3666 to 1445) | .47 | 156 (3799 to 1110) | .75 |
| 50th + incentives vs 75th | 1090 (313 to 2194) | .05 | 785 (3212 to 1782) | .12 | |
| 75th + incentives vs 75th | 556 (3743 to 1854) | .40 | 784 (3431 to 1998) | .21 | |
| 50th + incentives vs 50th | 701 (3280 to 1682) | .16 | 629 (3248 to 1506) | .16 | |
| 75th + incentives vs 50th | 166 (31031 to 1363) | .79 | 628 (3492 to 1748) | .27 | |
| 50th + incentives vs 75th + incentives | 535 (3706 to 1775) | .40 | 1 (31155 to 1157) | 1.00 | |
| Main model—adjusted by device and excluding step counts less than 1000 | 50th vs 75th | 300 (3665 to 1266) | .54 | 187 (3713 to 1088) | .68 |
| 50th + incentives vs 75th | 983 (326 to 1993) | .06 | 718 (3220 to 1656) | .13 | |
| 75th + incentives vs 75th | 537 (3651 to 1725) | .38 | 655 (3486 to 1796) | .26 | |
| 50th + incentives vs 50th | 683 (3211 to 1577) | .13 | 531 (3296 to 1358) | .21 | |
| 75th + incentives vs 50th | 237 (3856 to 1329) | .67 | 468 (3585 to 1520) | .38 | |
| 50th + incentives vs 75th + incentives | 446 (3686 to 1579) | .44 | 63 (31022 to 1148) | .91 | |
Abbreviation: CI, confidence interval.
Device refers to type of smartphone. Main model adjusts for repeated measures of daily participant step counts and for temporal trends by week using all collected data.
Values are presented as the difference between the specified arms.
During the follow-up period, the mean proportion achieving goal for the 50th percentile with incentives group began near 0.40 and steadily declined to about 0.25, near the level of the groups without incentives during the intervention. In the 75th percentile with incentives group, the mean proportion fluctuated between 0.30 and 0.40. However, there were no significant differences between any of the groups during the follow-up period for mean proportion achieving goal or mean daily steps.
Discussion
In this study, we demonstrated that the design of the engagement strategy can significantly affect physical activity outcomes. In this trial of 2 different social comparisons with and without financial incentives, we found that social comparison to median performance with financial incentives was most effective for increasing physical activity.
These findings expand upon current understanding of using social comparison and financial incentives to increase physical activity. Ball and colleagues found that individuals with higher levels of physical activity were more likely to perceive higher levels of activity among peers in their social network even after adjusting for the level of social support for being physical active.47 However, these findings were limited in their reliance on self-reported activity at 1 time point and the absence of an experimental design.
John and Norton conducted a randomized field experiment in which employees were given a treadmill desk at work and assigned to have access to performance feedback for only themselves, for a single coworker, or for 4 coworkers.48 Over the 6-month period, they found that the individual group had higher levels of activity but that activity among all groups steadily declined over time. Although John and Norton may have hoped that relative performance feedback would spur greater performance among the lower performers in each group, they found that in the group arms, activity tended to decline to the “least common denominator” as performance converged to the level of the lowest performer in the group. Our study builds upon these studies in several important ways. First, our study using smartphones to track activity throughout the day may be more affordable and scalable than providing treadmill desks and measuring activity only while at work. Second, evidence indicates that physical activity interventions are not effective unless individuals are given a goal.27 Although John and Norton did not set a performance goal, our study provided daily feedback on attainment of the 7000-step goal. Third, providing data on others’ performance alone may not achieve goals. In some contexts, feedback is more effective if paired with social approval or disapproval.49 In our study, individuals participated in teams that might provide peer support, accountability, and unity toward a common goal.28 By focusing social comparison feedback on performance relative to other teams, we leverage individuals’ competitive drive to motivate behavior change. Fourth, individuals are often motivated by the experience of past rewards and prospect of future rewards. Our study found that the most effective intervention paired social comparison feedback with financial incentives in the form of a weekly regret lottery. This design leverages individuals’ tendencies to place undue weight on small probabilities, be more engaged by variable reinforcement than constant reinforcement, and to avoid feeling regret from not winning a reward.15,16,28
Although many stakeholders are interested in using team-based interventions, performance feedback, and competitions to drive changes in health behaviors, it is important to conduct careful testing of alternate designs to determine which intervention is most effective. In our study, individuals were given social comparison feedback only once per week. Future studies might test differing frequencies of feedback and increase transparency to allow individuals to access their teammates’ performance in real time rather than once the week is over. Although intervention arms using financial incentives had higher rates of achieving goal, further study is needed to determine the optimal design, frequency, and size of financial incentives to increase physical activity.
Our study is subject to several limitations. First, participants were from a single location, which may limit generalizability as physical activity may be harder in some regions because of differences in climate, outdoor space, and culture. Second, participants in this study were required to have a smartphone, potentially making participation less accessible to those without these devices. Third, participants’ physical activity was not tracked when they were not carrying their smartphones, so captured physical activity levels may be lower than actual activity. However, at the end of the intervention period, 98% of respondents stated that they carried their smartphone most or all of the time. Fourth, randomization resulted in an uneven number of participants across arms, potentially limiting our power for arms with less than 70 participants. Fifth, we did not have baseline physical activity data from these participants, and self-reported data are likely overestimates. However, there were no significant differences among measured sample characteristics across all arms including self-reported physical activity; therefore, the randomized study design should reveal differential effects of the interventions on physical activity outcomes. Sixth, all 4 arms used social comparisons and so the results do not address the incremental value of social incentives.
In conclusion, physical inactivity is a leading risk factor for cardiovascular disease and mortality. New strategies are needed to change these behaviors. In this randomized trial, we found that a team-based intervention using a social feedback that compared team performance to the median with financial incentives was the most effective for increasing physical activity. These findings demonstrate the importance of careful testing of alternate ways of providing feedback and performance incentives to determine the optimal approach for changing health behaviors.
SO WHAT? Implications for Health Promotion Practitioners and Researchers.
What is already known on this topic?
Higher levels of physical activity are associated with numerous health benefits but more than half of adults in the United States do not achieve the minimum recommended level of physical activity. Financial incentives designed using insights from behavioral economics have been effective for changing several health behaviors but have not been well tested with strategies to increase physical activity.
What does this article add?
This is one of the first randomized trials testing different combinations of social comparison feedback and financial incentives designed using insights from behavioral economics to increase physical activity. We found that social comparison to the median with financial incentives was more effective than social comparison to the top quartile without incentives.
What are the implications for health promotion practice or research?
Although many stakeholders are interested in using interventions that incorporate financial incentives and social designs, it is important to carefully test these strategies before expanding more broadly. These findings may help to guide larger evaluations of interventions to increase physical activity using social comparison feedback and financial incentives.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by the National Institute on Aging (RC4 AG039114) to Drs Asch and Volpp. Dr Patel was supported in part by the Department of Veteran Affairs and the Robert Wood Johnson Foundation. Dr. Volpp also has received consulting income from CVS Caremark and research funding from Humana, CVS Caremark, Discovery (South Africa), and Merck, none of which are related to the work described in this manuscript.
Footnotes
The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. M.S.P. had full access to all the data in the study, takes responsibility for the integrity of the data and the accuracy of the data analysis, and had final responsibility for the decision to submit for publication. Dr Volpp and Dr Asch are principals at the behavioral economics consulting firm, VAL health.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Bijnen FC, Caspersen CJ, Mosterd WL. Physical inactivity as a risk factor for coronary heart disease: a WHO and International Society and Federation of Cardiology position statement. Bull World Health Organ. 1994;72(1):1–4. [PMC free article] [PubMed] [Google Scholar]
- 2.Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–1283. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shiroma EJ, Lee IM. Physical activity and cardiovascular health: lessons learned from epidemiological studies across age, gender, and race/ethnicity. Circulation. 2010;122(7):743–752. doi: 10.1161/CIRCULATIONAHA.109.914721. [DOI] [PubMed] [Google Scholar]
- 4.Löllgen H, Böckenhoff A, Knapp G. Physical activity and all-cause mortality: an updated meta-analysis with different intensity categories. Int J Sports Med. 2009;30(3):213–224. doi: 10.1055/s-0028-1128150. [DOI] [PubMed] [Google Scholar]
- 5.Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Impact of physical activity on the world’s major non-communicable disease. Lancet. 2012;380(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sattelmair J, Pertman J, Ding EL, Kohl HW, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–795. doi: 10.1161/CIRCULATIONAHA.110.010710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care. 2007;30(3):744–752. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- 8.Lee I, Djousse L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. JAMA. 2010;303(12):1173–1179. doi: 10.1001/jama.2010.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolin KY, Yan Y, Colditz GA, Lee IM. Physical activity and colon cancer prevention: a meta-analysis. Br J Cancer. 2009;100(4):611–616. doi: 10.1038/sj.bjc.6604917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedenreich CM. Physical activity and breast cancer: review of the epidemiologic evidence and biologic mechanisms. Recent Results Cancer Res. 2011;188:125–139. doi: 10.1007/978-3-642-10858-7_11. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. [Accessed April 1, 2015];Facts about physical activity. Web site. http://www.cdc.gov/physicalactivity/data/facts.html.
- 12.Hallal PC, Bauman AE, Heath GW, Kohl HW, Lee IM, Pratt M. Physical activity: more of the same is not enough. Lancet. 2012;380(9838):190–191. doi: 10.1016/S0140-6736(12)61027-7. [DOI] [PubMed] [Google Scholar]
- 13.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U Lancet Physical Activity Series Working Group. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 14.Volpp KG, Asch DA, Galvin R, Loewenstein G. Redesigning employee health incentives—lessons from behavioral economics. N Engl J Med. 2011;365(5):388–390. doi: 10.1056/NEJMp1105966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 16.Loewenstein G, Asch DA, Volpp KG. Behavioral economics holds potential to deliver better results for patients, insurers, and employers. Health Aff. 2013;32(7):1244–1250. doi: 10.1377/hlthaff.2012.1163. [DOI] [PubMed] [Google Scholar]
- 17.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47(2):263–291. [Google Scholar]
- 18.O’Donoghue T, Rabin M. The economics of immediate gratification. J Behav Decis Making. 2000;13(2):233–250. [Google Scholar]
- 19.Zeelenberg M, Pieters R. Consequences of regret aversion in real life: the case of the Dutch postcode lottery. Organ Behav Hum Decis Process. 2004;93(2):155–168. [Google Scholar]
- 20.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300(22):2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Volpp KG, Troxel AB, Pauly MV, et al. A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360(7):699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 22.Kimmel SE, Troxel AB, Loewenstein G, et al. Randomized trial of lottery-based incentives to improve warfarin adherence. Am Heart J. 2012;164(2):268–274. doi: 10.1016/j.ahj.2012.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell MS, Goodman JM, Alter DA, et al. Financial incentives for exercise adherence in adults. Am J Prev Med. 2013;45(5):658–667. doi: 10.1016/j.amepre.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 24.Jackson SE, Steptoe A, Wardle J. The influence of partner’s behavior on health behavior change: the English longitudinal study of ageing. JAMA Intern Med. 2015;175(3):385–392. doi: 10.1001/jamainternmed.2014.7554. [DOI] [PubMed] [Google Scholar]
- 25.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 26.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007;298(19):2296–2304. doi: 10.1001/jama.298.19.2296. [DOI] [PubMed] [Google Scholar]
- 28.Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 2015;313(5):459–460. doi: 10.1001/jama.2014.14781. [DOI] [PubMed] [Google Scholar]
- 29.Case MA, Burwick HA, Volpp KG, Patel MS. The accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA. 2015;313(6):625–626. doi: 10.1001/jama.2014.17841. [DOI] [PubMed] [Google Scholar]
- 30.Garber CE, Blissmer B, Deschenes MR, et al. on behalf of the American College of Sports Medicine. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently health adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 31.United States Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Hyattsville, MD: US Department of Health and Human Services; 2008. [Google Scholar]
- 32.Bassett DR, Wyatt HR, Thompson H, Peters JC, Hill JO. Pedometer-measured physical activity and health behaviors in U.S. adults. Med Sci Sports Exerc. 2010;42(10):1819–1825. doi: 10.1249/MSS.0b013e3181dc2e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sisson SB, Camhi SM, Tudor-Locke C, Johnson WD, Katzmarzyk PT. Characteristics of step-defined physical activity categories in U.S. adults. Am J Health Promot. 2012;26(3):152–159. doi: 10.4278/ajhp.100326-QUAN-95. [DOI] [PubMed] [Google Scholar]
- 34.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 35.Asch DA, Volpp KG. On the way to health. LDI Issue Brief. 2012;17(9):1–4. [PubMed] [Google Scholar]
- 36.Asch DA, Muller RW, Volpp KG. Automated hovering in health care—watching over the 5000 hours. N Engl J Med. 2012;367(1):1–3. doi: 10.1056/NEJMp1203869. [DOI] [PubMed] [Google Scholar]
- 37.Kullgren JT, Troxel AB, Loewenstein G, et al. Individual- versus group-based financial incentives for weight loss: a randomized, controlled trial. Ann Intern Med. 2013;158(7):505–514. doi: 10.7326/0003-4819-158-7-201304020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kullgren JT, Harkins KA, Bellamy SL, et al. A mixed-methods randomized controlled trial of financial incentives and peer networks to promote walking among older adults. Health Educ Behav. 2014;41(1 suppl):43S–50S. doi: 10.1177/1090198114540464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sen AP, Sewell TB, Riley EB, et al. Financial incentives for home-based health monitoring: a randomized controlled trial. J Gen Intern Med. 2014;29(5):770–777. doi: 10.1007/s11606-014-2778-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chapman GB, Coups EJ. Emotions and preventive health behavior: worry, regret, and influenza vaccination. Health Psychol. 2006;25(1):82–90. doi: 10.1037/0278-6133.25.1.82. [DOI] [PubMed] [Google Scholar]
- 41.Connolly T, Butler DU. Regret in economic and psychological theories of choice. J Behav Decis Mak. 2006;19(2):148–158. [Google Scholar]
- 42.Breslow NE, Clayton DG. Approximate inference in generalized linear mixed models. J Am Stat Assoc. 1993;88(421):9–25. [Google Scholar]
- 43.Schabenberger O, Gregoire TG. Population-averaged and subject-specific approaches for clustered categorical data. J Stat Comput Simulat. 1996;54(1–3):231–253. [Google Scholar]
- 44.SAS Institute Inc. SAS 9.4 Help and Documentation. Cary, NC: SAS Institute Inc; 2002–2004. [Google Scholar]
- 45.Rowe DA, Mahar MT, Raedeke TD, Lore J. Measuring physical activity in children with pedometers: reliability, reactivity, and replacement of missing data. Pediatr Exerc Sci. 2004;16(4):1–12. [Google Scholar]
- 46.Kang M, Zhu W, Tudor-Locke C, Ainsworth B. Experimental determination of effectiveness of an individual information-centered approach in recovering step-count missing data. Meas Phys Educ Exerc Sci. 2004;9(4):233–250. [Google Scholar]
- 47.Ball K, Jeffery RW, Abbott G, McNaughton SA, Crawford D. Is healthy behavior contagious: associations of social norms with physical activity and healthy eating. Int J Behav Nutr Phys Act. 2010;7:86. doi: 10.1186/1479-5868-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.John LK, Norton MI. Converging to the lowest common denominator in physical health. Health Psychol. 2013;32(9):1023–1028. doi: 10.1037/a0033849. [DOI] [PubMed] [Google Scholar]
- 49.Schultz PW, Nolan JM, Cialdini RB, Goldstein NJ, Griskevicius V. The constructive, destructive, and reconstructive power of social norms. Psychol Sci. 2007;18(5):429–434. doi: 10.1111/j.1467-9280.2007.01917.x. [DOI] [PubMed] [Google Scholar]