Abstract
Objective
To investigate the ratios of creatine kinase (CK) to aminotransferases as biomarkers of acute liver injury in dystrophinopathy.
Methods
C57 and mdx (dystrophic) mice were treated with a hepatotoxic reagent D-galactosamine (D-GalN). The degrees of liver and muscle injury were assessed using histological examinations. To examine whether serum CK-adjusted aminotransferase levels could indicate liver status in dystrophic mice, the CK/alanine aminotransferase (ALT) and CK/aspartate aminotransferase (AST) ratios were analyzed. Furthermore, we enrolled 658 male patients with dystrophinopathy and 378 male patients without muscle and liver injury as control, whose serum ALT, AST, and CK levels were examined.
Results
Animal experiments indicated that D-GalN treatment could induce acute liver injury but not muscle injury. Additionally, D-GalN decreased the CK/ALT and CK/AST ratios in both C57 mice and mdx mice (P < 0.001). However, there was an overlap of the CK/AST ratio between dystrophic mice with and without acute liver injury. In patients with dystrophinopathy, CK-adjusted ALT diminished the variability associated with age, genotype, clinical phenotype, and motor function (P > 0.05).
Conclusions
CK/ALT is a potential biomarker for the differential evaluation of acute liver injury in dystrophic mice, which highlights the value to further evaluate the practice of CK/ALT in dystrophinopathy patients.
1. Introduction
Dystrophinopathy is the most common type of muscular dystrophy characterized by progressive necrosis, fibrosis, fatty tissue replacement, inflammation, and loss of regenerative capacity in skeletal and cardiac muscles [1, 2]. According to the disease course, it can be divided into Duchenne muscular dystrophy (DMD), intermediate muscular dystrophy (IMD), and Becker muscular dystrophy (BMD) [3]. Eighty percent of patients have large genetic rearrangements in the DMD gene encoding dystrophin, and the rest suffer from small mutations [4]. Glucocorticoid administration can ameliorate the progression of the disease but cannot cure it [5]. Although dystrophinopathy still has no cure and most patients die of heart and respiratory failure, effective health measures that improve life quality and expectancy in patients with dystrophinopathy have been developed in the last 20 years [5].
Health management has focused on the functions of critical organs such as the heart, lung, and kidney, and specific biomarkers to monitor their functional activity have been suggested [6–8]. However, less attention was paid to the liver, which can also be injured in dystrophinopathy. Acute liver failure has been reported in a dystrophinopathy patient treated with paracetamol [9]. Liver failure can also be a significant postoperative complication after tendon lengthening, scoliosis surgery, and heart transplantation which are performed in patients with dystrophinopathy [10–15]. In addition, as an increasing number of preclinical studies and clinical trials for promising treatments such as gene therapy and stem cell therapy have been conducted, it is important to evaluate hepatotoxicity as a criterion of therapeutic safety [16, 17]. Therefore, it is necessary to evaluate liver conditions in dystrophinopathy using reliable diagnostic methods.
Aminotransferases, including alanine aminotransferase (ALT) and aspartate aminotransferase (AST), are widely used in evaluating liver status because of high diagnostic accuracy and low test costs [18]. However, although aminotransferase activity reflects hepatocyte injury [19], there are limitations for its application in dystrophinopathy, such as elevated background levels and age-dependent variability caused by the release of aminotransferases from injured myofibers [20]. Previous studies indicate that serum gamma-glutamyl transferase levels can be a valuable diagnostic tool for screening liver disease in dystrophinopathy; however, its sensitivity is limited, especially in patients with noncholestatic, hepatocellular conditions [21, 22]. Although imaging modalities such as sonography represent well-developed methods to estimate liver status, they are time- and cost-consuming and not appropriate for screening. Therefore, considering an effective worldwide application of serum aminotransferase activity to assess liver injury, aminotransferase levels adjusted by some indexes specifically reflecting muscle injury could be used to evaluate liver status in dystrophinopathy.
Compared to aminotransferases, creatine kinase (CK) is a more specific index of muscle injury [20]; therefore, we hypothesized that CK-adjusted aminotransferase levels may present an even more accurate biomarker of liver damage in dystrophinopathy. In this study, we aimed to establish a mouse model of dystrophinopathy with acute liver injury and examined whether the CK-adjusted aminotransferase levels can indicate acute liver injury in this model. Additionally, a preliminary investigation for the applicability of CK-adjusted aminotransferases in patients with dystrophinopathy was undertaken.
2. Methods
2.1. Establishment of Animal Models for Acute Liver Injury
All experiments were approved by the ethics committee for Clinical Research and Trials of the First Affiliated Hospital of Sun Yat-sen University. C57BL (C57) and C57BL/10ScSn-Dmdmdx/J (mdx, a mouse model of dystrophinopathy) male mice aged 4-5 weeks were obtained from the Guangdong Medical Laboratory Animal Center (Guangzhou, GD, China) and the Model Animal Research Center of Nanjing University (Nanjing, JS, China), respectively. D-Galactosamine (D-GalN), an amino sugar resulting in depletion of uridine moieties within the liver and leading to hepatocyte necrosis, was chosen as an inducer of acute liver injury [23, 24]. Mice were randomly divided into four groups: C57 NS, C57 D-GalN, mdx NS, and mdx D-GalN (n = 10 each). NS and D-GalN mice were injected intraperitoneally with normal saline (NS; China Otsuka Pharmaceutical Company, Tianjin, China) or 2000 mg/kg D-GalN (Sigma-Aldrich, St. Louis, MO, USA) dissolved in NS for inducing hepatotoxicity, respectively [25, 26]. The total injection volume per mouse was 20 mL/kg. After 24 h, blood samples were obtained via tail cut; then, mice were sacrificed by cervical vertebrae dislocation and their livers and tibialis anterior (TA) muscles were extracted.
2.2. Evaluation of Muscle and Liver Lesions
TA is one of the most common muscles used to evaluate muscle lesions in mdx mice as it is easy to extract; therefore, it was used to assess myotoxicity of D-GalN [27, 28]. TA muscles were treated and sectioned and stained with hematoxylin-eosin (HE), adenosine triphosphatase (ATPase) following preincubation pH at 10.6, and nicotinamide adenine dinucleotide tetrazolium reductase (NADH-TR) for morphological analysis as previously described [27, 29]. Myofiber types were classified into type I myofibers (light staining) and type II myofibers (dark staining) using ATPase (pH 10.6) staining. Additionally, myofibers stained with NADH-TR were classified into type I myofibers (dark staining), type IIA myofibers (moderate staining), and type IIB myofibers (light staining). Overall, fiber types were determined with a combination of ATPase staining and NADH-TR staining. Necrotic myofibers, regenerating myofibers, centronucleated myofibers, and a ratio of central versus peripheral nuclei were counted to evaluate necrosis and degeneration/regeneration cycles of TA [30].
Mouse livers were fixed in neutral-buffered formalin, embedded in paraffin, sectioned, and stained with HE as previously described [31]. The histological severity of liver lesions was graded according to the Ishak system using the sum of necroinflammatory scores A, B, C, and D [32].
2.3. Study Participants
Overall, 658 male patients with dystrophinopathy [6 years (4–9)] followed up in our hospital from 2008 to 2016 were included in the study. And 378 male patients without muscle and liver injury [10 years (5–14.75)] were also included as a control. Approval to waive informed parental consent was granted by the ethics committee of the First Affiliated Hospital, Sun Yat-sen University. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. The patients did not exhibit outward clinical manifestations of liver disease, and those with abnormal serum total bilirubin were not included. All dystrophinopathy patients were diagnosed with clinical manifestations, biochemical changes, and molecular/histological diagnosis. Twenty patients were given histological diagnosis (antidystrophin immunohistochemistry staining in muscle biopsy samples), which showed absence or low levels of dystrophin. And the others (n = 638) were given genetic diagnosis. Serum levels of CK, ALT, and AST were examined; typically, the earliest recorded test results were analyzed. Detailed information is shown in Table 1.
Table 1.
Clinical information of patients with dystrophinopathy.
| Parameters | Number | Percentage |
|---|---|---|
| Ethnicity | 658 | |
| East Asian | 658 | 100 |
| Clinical phenotype | 658 | |
| DMD | 464 | 70.52 |
| IMD | 37 | 5.62 |
| BMD | 157 | 23.86 |
| Muscle biopsy and dystrophin staining | 20 | |
| Mutation analysis | 638 | |
| Deletion | 468 | 73.35 |
| Duplication | 96 | 15.05 |
| Small mutations | 74 | 11.60 |
DMD: Duchenne muscular dystrophy; IMD: intermediate muscular dystrophy; BMD: Becker muscular dystrophy.
2.4. Genotyping
DMD genotyping was performed for 638 patients. Multiplex ligation-dependent probe amplification (MLPA) (n = 553) and hotspot region polymerase chain reaction (n = 11) were used to detect large genetic rearrangements (deletions or duplications), and next-generation sequencing was used to detect small mutations.
2.5. Determination of Clinical Phenotypes
Clinical phenotypes were classified according to the age at which walking ability was lost as previously described [3]: DMD, losing walking ability by the age of 13 years; IMD, losing walking ability between 13 and 16 years; and BMD, walking after 16 years. Patients younger than 16 years who retained walking ability were evaluated according to disease severity, serum indexes, muscle biopsy, and molecular tests. Patients who were too young for evaluation were followed up and evaluated later. Patients whose phenotype could not be determined were considered having IMD in this study.
2.6. Determination of Serum Enzyme Activity
Approximately 200 μL of blood from each mouse or 5 mL of blood from each patient was collected, centrifuged at 1810 ×g for 5 min at 24°C, and analyzed for ALT, AST, and CK activities using a Beckman Coulter AU5800 clinical chemistry analyzer (ALT: lactate dehydrogenase method, AST: malate dehydrogenase method, and CK: enzymatic method; Beckman Coulter, Brea, CA, USA). To determine CK levels, serum samples were diluted step-wise 3-, 5-, 10-, and 20-fold because CK activity was beyond the linear range, and the CK level was measured and recorded at the highest dilution.
2.7. Statistical Analysis
Statistical analysis was performed using SPSS version 20.0 (IBM Corp., Chicago, IL, USA) and GraphPad PRISM version 7.01 (GraphPad Software, San Diego, CA, USA). Normal distribution of variables was tested by the Shapiro-Wilk test (n ≤ 50) or Kolmogorov-Smirnov test (n > 50); variables with normal distributions and without normal distributions were presented as the mean and standard deviation (median ± standard deviation) and the median and interquartile range [median (interquartile range)], respectively. To analyze differences between two variables and more than three variables with normal distributions, Student's t-test or one-way analysis of variance was used. To analyze differences between two variables and more than three variables with nonnormal distributions, the Mann-Whitney U test or Kruskal-Wallis H test was used. Differences among more than three variables were analyzed using the Bonferroni method. The correlations between two variables with normal distributions and without normal distributions were analyzed by the Pearson method and Spearman method, respectively. All tests were two-tailed, and P < 0.1 was considered statistically significant in the Shapiro-Wilk and Kolmogorov-Smirnov tests, whereas P < 0.05 was considered significant in other tests.
3. Results
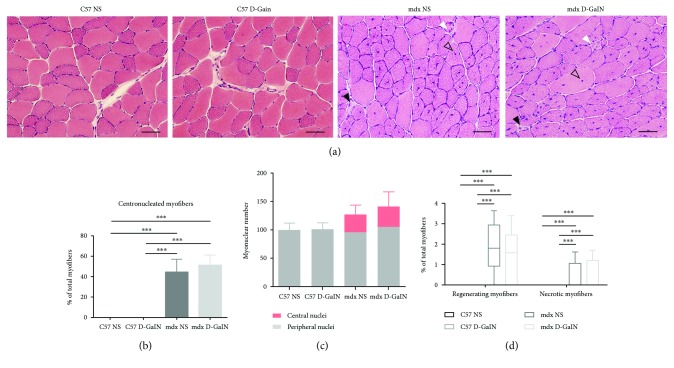
3.1. Muscle Necrosis and Regeneration in Mice
No mice died after 24 h of D-GalN treatment. To detect the myofiber necrosis and regeneration in mice, TA sections were stained with HE. The results showed that necrosis, regeneration, and centronucleated myofibers were observed in mdx mice but not in C57 mice (Figure 1(a)). Additionally, muscle lesions were evaluated using the percentage of centronucleated myofibers, the ratio of central versus peripheral nuclei, and the percentage of regenerating or necrotic myofibers [30]. The differences of above indexes were significant between C57 NS mice and mdx NS mice, and the same was true for C57 D-GalN mice and mdx D-GalN mice (P < 0.001, Figures 1(b)–1(d)). However, these differences could not be observed between the D-GalN treated group and the untreated group in C57 mice or mdx mice (P > 0.05).
Figure 1.
Necrosis and regeneration in the muscle of D-galactosamine-treated and D-galactosamine-untreated mice. Mice were intraperitoneally injected with D-galactosamine (D-GalN) or normal saline (NS), and tibialis anterior (TA) was sectioned for histological analysis 24 h later. (a) HE staining showed normal morphology of TA in both the C57 NS and the C57 D-GalN groups and muscle lesions in both the mdx NS and the mdx D-GalN groups. Solid black arrows: necrotic myofibers with pale and homogenous sarcoplasm and pyknotic nuclei; solid white arrows: regenerating myofibers with a small diameter and vesicular central nuclei; and hollow black arrows: centronucleated myofibers. Scale bar: 100 μm. (b, c) The percentage of centronucleated myofibers in total myofibers (b) and the ratio of central versus peripheral nuclei (c) of different groups. (d) The percentage of regenerating and necrotic myofibers in total myofibers of different groups. ∗∗∗P < 0.001.
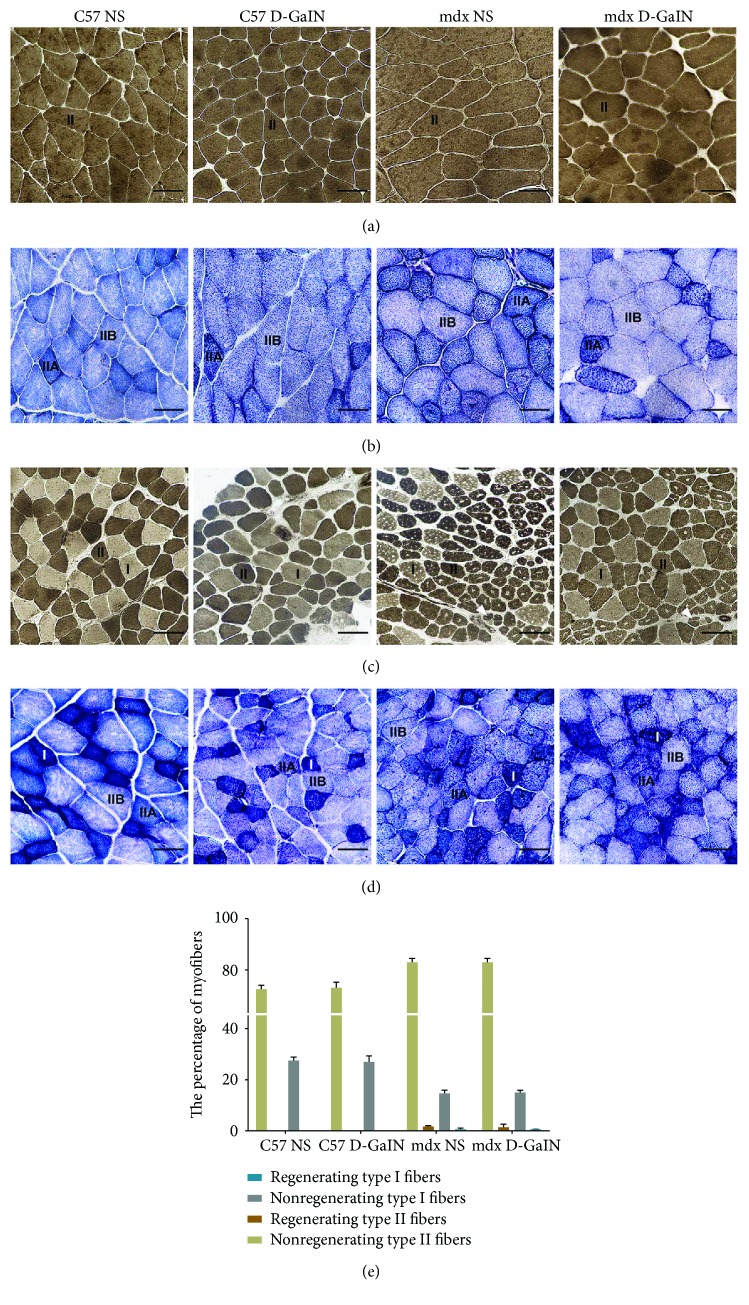
3.2. Myofiber Types in Mice
Myofibers could be mainly classified into two groups: type I myofibers and type II myofibers, of which type II consisted of type IIA and type IIB myofibers. The changes of the proportion of fiber types indicated muscle injury. To detect the fiber type changes and regeneration of different myofiber types in mice, TA sections were stained with ATPase and NADH-TR. The results indicated that almost all myofibers in the superficial area of TA were type II myofibers in both C57 and mdx mice with or without D-GalN treatment (Figures 2(a), 2(b)). Additionally, type II myofibers were also dominant in the deep area of TA, whose proportion was higher in mdx mice than in C57 mice, but D-GalN treatment did not cause an extra increase of type II myofibers neither in C57 nor in mdx mice (72.46% ± 1.43% in C57 NS versus 72.93% ± 2.23% in C57 D-GalN versus 84.66% ± 1.46% in mdx NS versus 84.25% ± 0.83% in mdx D-GalN, P < 0.001, Figures 2(c)–2(e)). Then, we analyzed the regeneration of different fiber types in the deep area of TA in mdx mice. We found that regeneration toward type II myofibers was more common than that toward type I myofibers (P < 0.001, Figure 2(e)), which could be observed in both D-GalN-treated and D-GalN-untreated mdx mice.
Figure 2.
Myofiber types in the muscle of D-galactosamine-treated and D-galactosamine-untreated mice. (a, b) Superficial area of tibialis anterior (TA). (c, d) Deep area of TA. (a, c) Adenosine triphosphatase activity following preincubation pH at 10.6; solid white arrows: regenerating myofibers. (b, d) Nicotinamide adenine dinucleotide tetrazolium reductase. Scale bar: 50 μm. (e) The percentage of different myofiber types in four mouse groups.
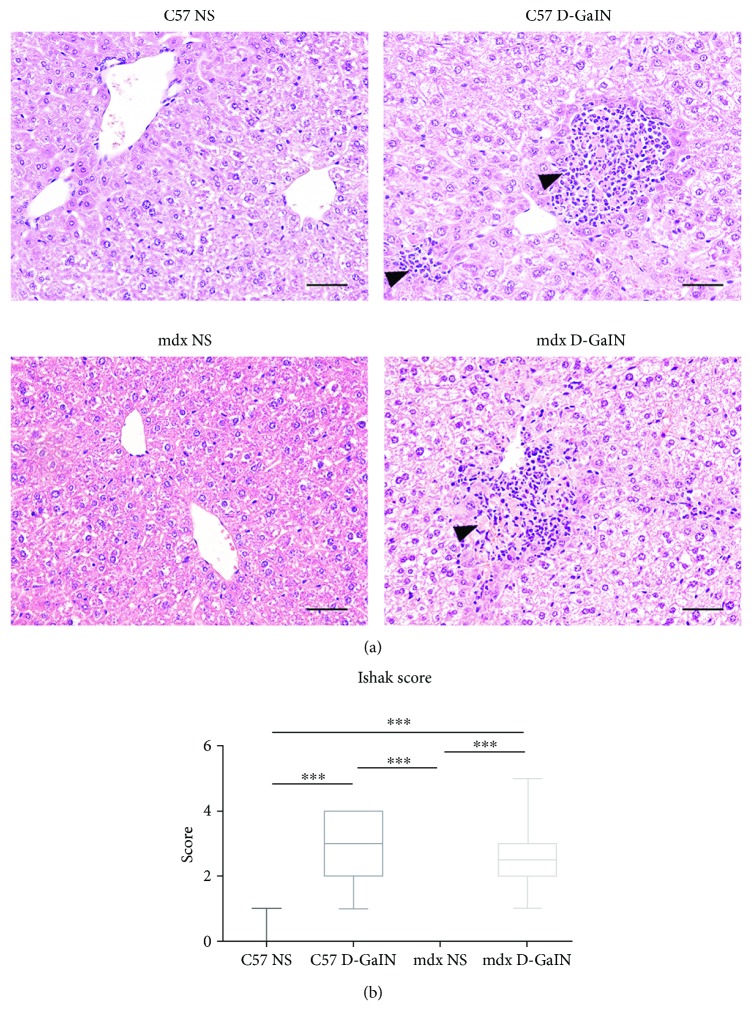
3.3. D-GalN-Induced Hepatic Necrosis in Mice
Liver histology was evaluated to determine liver injury. The results indicated that obvious hepatocyte necrosis could be observed in D-GalN-treated mice (Figure 3(a)). A normal hepatic lobule structure consisted of a regular arrangement of hepatic cells radially around the central vein. The hepatocytes appeared to be necrotic, and inflammation in lesions was observed in 2000 mg/kg D-GalN-treated C57 mice and mdx mice (P < 0.001, Figure 3(b)). Overall, above results indicated that D-GalN caused acute liver injury but no muscle injury in mdx mice; thus, the mouse model of dystrophinopathy with acute liver injury was established successfully.
Figure 3.
Liver necrosis in D-galactosamine-treated and D-galactosamine-untreated mice. (a) HE staining revealed necrotic lesions (hepatic necrosis and inflammation) in the liver of D-GalN-treated mice (solid black arrows). Scale bar: 100 μm. (b) Ishak (pathological) scores of liver lesions. ∗∗∗P < 0.001.
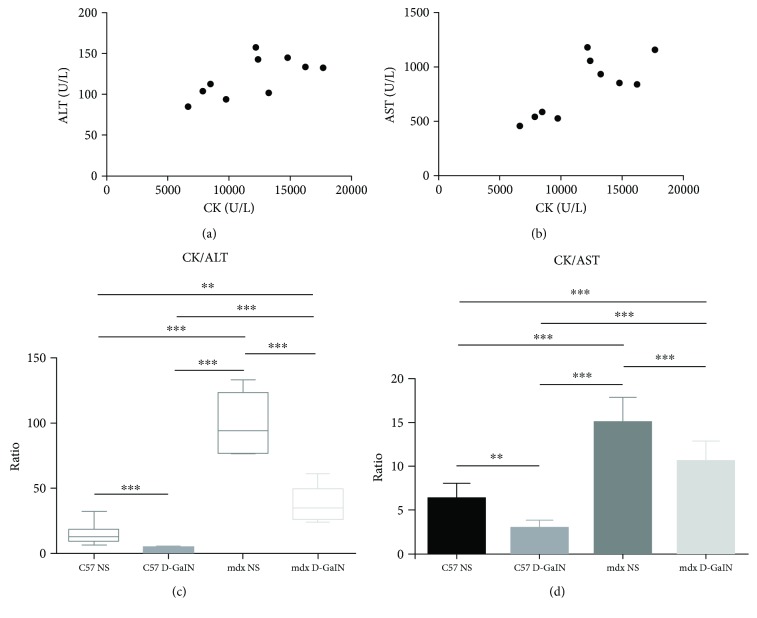
3.4. The Ratio of CK to Aminotransferases Decreased in Mice with Acute Liver Injury
To verify whether CK-adjusted aminotransferases could detect acute liver injury, serum CK, ALT, and AST were analyzed in mice. In the mdx control group (mdx NS), the linear correlation between levels of CK and ALT was observed (P < 0.05, r = 0.65, Figure 4(a)). Similarly, AST level was also correlated with CK level (P < 0.01, r = 0.77, Figure 4(b)). Thus, the ratios of CK to aminotransferases were calculated as CK-adjusted aminotransferases. A significant decrease in CK/ALT and CK/AST could be observed in D-GalN-treated mice compared to control (P < 0.001, Figures 4(c) and 4(d)). Furthermore, a significant difference in CK/ALT was observed among the four mouse groups: 12.50 (9.33–18.33) in C57 NS versus 2.50 (1.68–4.43) in C57 D-GalN versus 94.40 (76.73–123.85) in mdx NS versus 34.70 (25.98–49.78) in mdx D-GalN (P < 0.001, Figure 4(c)). Similarly, a significant difference in CK/AST was also observed among the four mouse groups: 6.33 ± 1.74 in C57 NS versus 2.95 ± 0.98 in C57 D-GalN versus 15.04 ± 2.83 in mdx NS versus 10.65 ± 2.19 in mdx D-GalN (P < 0.001, Figure 4(d)). However, a partial overlap of CK/AST could be observed between mdx mice with and without acute liver injury. In conclusion, these results indicated that the CK/ALT and CK/AST could be used to distinguish among normal liver status, acute injury, and dystrophinopathy without and with acute liver injury. Additionally, CK/ALT was more reliable because there was no overlap of CK/ALT between mice with and without acute liver injury.
Figure 4.
The ratio of creatine kinase to aminotransferase in D-galactosamine-treated and D-galactosamine-untreated mice. (a, b) The scatter plots of creatine kinase (CK) versus alanine aminotransferase (ALT (a)) and CK versus aspartate aminotransferase (AST (b)) in D-GalN-untreated mdx mice. (c, d) The ratio of CK to ALT (c) and CK to AST (d) in four mouse groups. ∗∗P < 0.01 and ∗∗∗P < 0.001.
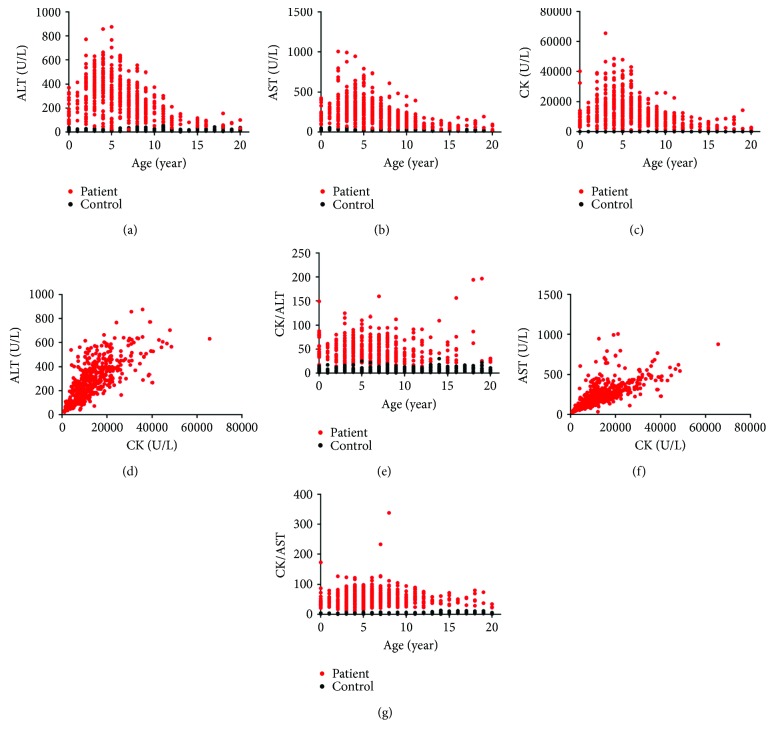
3.5. ALT Adjustment by CK Can Diminish Age Variability in Patients with Dystrophinopathy
To investigate the possible applicability of CK/ALT for patients with dystrophinopathy, we analyzed enzyme profiles in patients of different ages. ALT, AST, and CK levels in dystrophinopathy patients peaked at the age of 5 years (Figures 5(a)–5(c)). Considering that CK could specifically reflect muscle injury, the levels of aminotransaminases were adjusted to those of CK [20]. The linear correlation between ALT and CK was significant (P < 0.001, r = 0.75, Figure 5(d)); therefore, we used the CK/ALT ratio to diminish age-dependent fluctuations and found that the distribution of CK/ALT did not differ between patients of different ages (P = 0.56, Figure 5(e)). A similar linear correlation was also observed between AST and CK (P < 0.001, r = 0.79, Figure 5(f)), but the age-dependent difference in CK/AST was significant (P < 0.001, Figure 5(g)). Thus, our results indicated that the CK/ALT could diminish age variability in dystrophinopathy. Furthermore, CK/ALT could also diminish variability associated with genotype, clinical phenotype, and motor function (data not showed). The 5th percentile for CK/ALT was determined by SPSS software as 22.16.
Figure 5.
Scatter plots of enzyme activity profiles in patients with dystrophinopathy. (a–c) Age versus alanine aminotransferase (ALT (a)), aspartate aminotransferase (AST (b)), and creatine kinase (CK (c)). (d) CK versus ALT. (e) Age versus CK/ALT. (f) CK versus AST. (g) Age versus CK/AST.
4. Discussion
In this study, we established a mouse model of dystrophinopathy with acute liver injury. The results showed that CK/ALT and CK/AST ratios decreased significantly in this model and the overlap of CK/AST ratios between dystrophic mice with and without acute liver injury resulted in the possibility of false discrimination. In addition, the CK/ALT ratio was independent of age and factors associated with muscle injury in patients with dystrophinopathy.
Serum-based enzyme tests have been widely used for various applications in the clinic [33–35]. And a variety of serum enzymes, such as CK, ALT, and AST, were reported to increase in muscular dystrophy [36, 37]. The elevation of serum enzymes in dystrophinopathy is thought to be due to their release from injured myofibers rather than to liver injury as indicated by liver biopsy in patients [38]. It is consistent with the absence of liver damage in D-GalN-untreated mdx mice observed in this study. The elevation of CK and aminotransferase levels in dystrophinopathy is easy to understand due to the organ distribution of enzymes: ALT and AST are distributed mostly in the liver and muscles, while CK is distributed highly in the muscles [18–20, 39–41].
Although aminotransferases are widely applied in the clinic as sensitive biomarkers for hepatocyte injury, the concurrence of increased serum CK and aminotransferases is indicative for muscle injury in most cases in dystrophinopathy [20, 42, 43]. However, the elevated levels of aminotransferases in muscular dystrophy sometimes make clinicians confused, which leads to the misdiagnosis of liver diseases and unnecessary liver biopsy [20, 38]. Thus, the lack of specificity limits the application of aminotransferases in muscular dystrophy. Up till now, hepatocyte injury is still inconvenient to detect in dystrophinopathy due to the lack of excellent highly tissue-specific indexes [19, 21, 22], which results in the challenges of an accurate differential diagnosis of liver injury in dystrophinopathy. Recently, a combination of several serum enzymes to distinguish five types of muscular dystrophy suggested the value of comprehensive evaluation of serum enzyme-based tests for diagnostic purpose in muscular dystrophy [44]. The study gives us a hint that the combination of muscle biomarker and aminotransferases together may be more applicable for the evaluation of hepatocyte injury in dystrophinopathy.
CK is the well-known biomarker closely associated with muscle injury and muscular dystrophy, and elevated levels of CK can differentiate some types of muscular dystrophy [43]. Thus, we chose CK to adjust the baselines of aminotransferases in this study. Considering the obvious linear correlations between CK and aminotransferases in both dystrophic mice and patients with dystrophinopathy, the ratio of CK to aminotransferases may be an appropriate adjustment. Our results indicated that the CK/ALT ratio decreased significantly in dystrophic mice with acute liver injury; thus, decreased CK/ALT could indicate acute liver injury in mice.
In patients with dystrophinopathy, the elevated levels of CK and aminotransferases can vary with age and other factors, such as genotype, clinical phenotype, and motor function, all of which made it difficult to establish applicable baselines of CK and aminotransferase levels for diagnostic purposes [43]. Interestingly, we found that CK-adjusted ALT could diminish the variability associated with age and other factors correlated with muscle injury, which suggests that CK/ALT is less influenced by muscle injury and has the possibility of application for dystrophinopathy. Even though, we need to notice that levels of CK and aminotransferases may be affected by other factors, such as gender, ethnicity, life style, activity levels, surgical procedures, seasonal influences, and medication administration [43, 45], which can lead to an inaccurate diagnosis of acute liver injury. These factors can be easily controlled in a mouse model, but the influence of them must be evaluated when applied in human.
Although AST also had a linear correlation with CK, CK/AST had an overlap between dystrophic mice with and without acute liver injury. And furthermore, CK/AST was still affected by age and factors associated with muscle injury severity in patients, as evidenced by its increase in patients with more severe genotype and phenotype. Compared to ALT, AST has higher concentration in muscle tissue; consistently, it was observed that the increase of serum AST was higher than that of serum ALT after muscle exercise stress [46, 47]. Therefore, serum AST is a less specific indicator of liver injury [42]. Overall, these data suggest that CK/ALT is better for the differential evaluation of acute liver injury in dystrophinopathy.
Mdx mouse is a widely used mouse model of dystrophinopathy, which contributes to numerous understanding of dystrophinopathy [48]. However, a mouse is not a man. The scale, growth pattern, and cell biology of mouse are highly different from human [49, 50]. Besides, as we observed in this study, the distribution of myofiber types in mice is largely different from that in human. Not only limited to TA, higher frequencies of type II myofibers are observed in numerous muscles of mouse compared with human, which adapts to the motor pattern of mouse [50–52]. Additionally, the phenotype and lifespan shortening of mdx mice are milder compared with those of patients [53]. Although the TA of mdx mice exhibits similar pathological changes of dystrophinopathy, such as necrosis, regeneration, various myofiber sizes, and centronucleated myofibers, they are milder and lack obvious fibrosis compared to pathological changes of skeletal muscles in patients [53]. Therefore, we must be cautious to extend the conclusion from animal to human. In this study, the utility of CK/ALT for detecting acute liver injury was verified in dystrophic mice. Although we preliminarily investigated the possibility of CK/ALT for clinical application and determined the lower limit of normal (LLN) of CK/ALT in patients with dystrophinopathy, a further study based on patients' data is necessary before its application in the clinic.
In conclusion, we successfully established a mouse model of dystrophinopathy with acute liver injury. And CK/ALT is a potential biomarker for the differential evaluation of acute liver injury in dystrophic mice, which highlights the value to further evaluate the practice of CK/ALT in patients with dystrophinopathy.
Acknowledgments
The study was funded by the Natural Science Foundation of China (Grant nos. 81771359, 81471280, and 81271401); the Guangdong Provincial Science and Technology Department (Grant no. 2014A020212130); the Guangzhou Science and Technology Project Fund (Grant nos. 1561000153 and 201508020012); the National Key Clinical Department and Key Discipline of Neurology, Guangdong Provincial Key Laboratory for Diagnosis and Treatment of Major Neurological Diseases (no. 2014B030301035); the Southern China International Cooperation Base for Early Intervention and Functional Rehabilitation of Neurological Diseases (no. 2015B050501003); and the Guangdong Provincial Engineering Center for Major Neurological Disease Treatment, Guangzhou Science and Technology Program key projects (no. 201604020010).
Conflicts of Interest
The authors declare that they have no conflict of interest.
Authors' Contributions
Liang Wang and Menglong Chen contributed equally to this work.
References
- 1.Mah J. K., Korngut L., Dykeman J., Day L., Pringsheim T., Jette N. A systematic review and meta-analysis on the epidemiology of Duchenne and Becker muscular dystrophy. Neuromuscular Disorders. 2014;24(6):482–491. doi: 10.1016/j.nmd.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Klingler W., Jurkat-Rott K., Lehmann-Horn F., Schleip R. The role of fibrosis in Duchenne muscular dystrophy. Acta Myologica. 2012;31(3):184–195. [PMC free article] [PubMed] [Google Scholar]
- 3.Hodgson S., Hart K., Abbs S., et al. Correlation of clinical and deletion data in Duchenne and Becker muscular dystrophy. Journal of Medical Genetics. 1989;26(11):682–693. doi: 10.1136/jmg.26.11.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aartsma-Rus A., van Deutekom J. C. T., Fokkema I. F., van Ommen G. J. B., den Dunnen J. T. Entries in the Leiden Duchenne muscular dystrophy mutation database: an overview of mutation types and paradoxical cases that confirm the reading-frame rule. Muscle & Nerve. 2006;34(2):135–144. doi: 10.1002/mus.20586. [DOI] [PubMed] [Google Scholar]
- 5.Annexstad E. J., Lund-Petersen I., Rasmussen M. Duchenne muscular dystrophy. Tidsskrift for den Norske Lægeforening. 2014;134(14):1361–1364. doi: 10.4045/tidsskr.13.0836. [DOI] [PubMed] [Google Scholar]
- 6.Romfh A., Mcnally E. M. Cardiac assessment in Duchenne and Becker muscular dystrophies. Current Heart Failure Reports. 2010;7(4):212–218. doi: 10.1007/s11897-010-0028-2. [DOI] [PubMed] [Google Scholar]
- 7.Viollet L., Gailey S., Thornton D. J., et al. Utility of cystatin C to monitor renal function in Duchenne muscular dystrophy. Muscle & Nerve. 2009;40(3):438–442. doi: 10.1002/mus.21420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Birnkrant D. J., Pope J. F., Eiben R. M. Topical review: management of the respiratory complications of neuromuscular diseases in the pediatric intensive care unit. Journal of Child Neurology. 1999;14(3):139–143. doi: 10.1177/088307389901400301. [DOI] [PubMed] [Google Scholar]
- 9.Pearce B., Grant I. S. Acute liver failure following therapeutic paracetamol administration in patients with muscular dystrophies. Anaesthesia. 2008;63(1):89–91. doi: 10.1111/j.1365-2044.2007.05340.x. [DOI] [PubMed] [Google Scholar]
- 10.Forst J., Forst R. Lower limb surgery in Duchenne muscular dystrophy. Neuromuscular Disorders. 1999;9(3):176–181. doi: 10.1016/S0960-8966(98)00113-8. [DOI] [PubMed] [Google Scholar]
- 11.Burow M., Forst R., Forst J., Hofner B., Fujak A. Perioperative complications of scoliosis surgery in patients with Duchenne muscular dystrophy and spinal muscular atrophy, focussing on wound healing disorders. The International Journal of Neuroscience. 2016;127(6):479–485. doi: 10.1080/00207454.2016.1196688. [DOI] [PubMed] [Google Scholar]
- 12.Birnbaum B. F., Simpson K. E., Canter C. E. Heart transplantation in pediatric cardiomyopathies. Expert Review of Cardiovascular Therapy. 2014;11(12):1677–1690. doi: 10.1586/14779072.2013.847789. [DOI] [PubMed] [Google Scholar]
- 13.Lerman J. Perioperative management of the paediatric patient with coexisting neuromuscular disease. British Journal of Anaesthesia. 2011;107(Supplement 1):i79–i89. doi: 10.1093/bja/aer335. [DOI] [PubMed] [Google Scholar]
- 14.Duckworth A. D., Mitchell M. J., Tsirikos A. I. Incidence and risk factors for post-operative complications after scoliosis surgery in patients with Duchenne muscular dystrophy: a comparison with other neuromuscular conditions. The Bone & Joint Journal. 2014;96-B(7):943–949. doi: 10.1302/0301-620X.96B7.33423. [DOI] [PubMed] [Google Scholar]
- 15.Beck C., Schwartges I., Picker O. Perioperative liver protection. Current Opinion in Critical Care. 2010;16(2):142–147. doi: 10.1097/MCC.0b013e328336ea83. [DOI] [PubMed] [Google Scholar]
- 16.Jarmin S., Kymalainen H., Popplewell L., Dickson G. New developments in the use of gene therapy to treat Duchenne muscular dystrophy. Expert Opinion on Biological Therapy. 2013;14(2):209–230. doi: 10.1517/14712598.2014.866087. [DOI] [PubMed] [Google Scholar]
- 17.Nishiyama T., Takeda S. Induced pluripotent stem (iPS) cell-based cell therapy for muscular dystrophy: current progress and future prospects. Brain and Nerve. 2012;64(1):39–46. [PubMed] [Google Scholar]
- 18.Aragon G., Younossi Z. M. When and how to evaluate mildly elevated liver enzymes in apparently healthy patients. Cleveland Clinic Journal of Medicine. 2010;77(3):195–204. doi: 10.3949/ccjm.77a.09064. [DOI] [PubMed] [Google Scholar]
- 19.Giannini E. G., Testa R., Savarino V. Liver enzyme alteration: a guide for clinicians. CMAJ. 2005;172(3):367–379. doi: 10.1503/cmaj.1040752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mcmillan H. J., Gregas M., Darras B. T., Kang P. B. Serum transaminase levels in boys with Duchenne and Becker muscular dystrophy. Pediatrics. 2011;127(1):e132–e136. doi: 10.1542/peds.2010-0929. [DOI] [PubMed] [Google Scholar]
- 21.Rosales X. Q., Chu M. L., Shilling C., Wall C., Pastores G. M., Mendell J. R. Fidelity of gamma-glutamyl transferase (GGT) in differentiating skeletal muscle from liver damage. Journal of Child Neurology. 2008;23(7):748–751. doi: 10.1177/0883073808314365. [DOI] [PubMed] [Google Scholar]
- 22.Emerick K. M. Use of gamma-glutamyl transferase as a screen for liver disease in muscular dystrophy patients. Journal of Pediatric Gastroenterology and Nutrition. 2009;48(5):643–644. doi: 10.1097/MPG.0b013e31818d7da2. [DOI] [PubMed] [Google Scholar]
- 23.Belanger M., Butterworth R. F. Acute liver failure: a critical appraisal of available animal models. Metabolic Brain Disease. 2005;20(4):409–423. doi: 10.1007/s11011-005-7927-z. [DOI] [PubMed] [Google Scholar]
- 24.Farghali H., Kgalalelo K. M., Wojnarova L., Kutinova C. N. In vitro and in vivo experimental hepatotoxic models in liver research: applications to the assessment of potential hepatoprotective drugs. Physiological Research. 2016;65(Supplement 4):S417–S425. doi: 10.33549/physiolres.933506. [DOI] [PubMed] [Google Scholar]
- 25.Dong M., Hong T., Liu S., Zhao J., Meng Y., Mu J. Hepatoprotective effect of the flavonoid fraction isolated from the flower of Inula britannica against D-galactosamine-induced hepatic injury. Molecular Medicine Reports. 2013;7(6):1919–1923. doi: 10.3892/mmr.2013.1443. [DOI] [PubMed] [Google Scholar]
- 26.Haro C., Zelaya H., Lazarte S., Alvarez S., Aguero G. Lactobacillus casei: influence on the innate immune response and haemostatic alterations in a liver-injury model. Canadian Journal of Microbiology. 2009;55(6):648–656. doi: 10.1139/W09-022. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y., Zhu Y., Li Y., et al. Long-term engraftment of myogenic progenitors from adipose-derived stem cells and muscle regeneration in dystrophic mice. Human Molecular Genetics. 2015;24(21):6029–6040. doi: 10.1093/hmg/ddv316. [DOI] [PubMed] [Google Scholar]
- 28.Whitehead N. P., Kim M. J., Bible K. L., Adams M. E., Froehner S. C. A new therapeutic effect of simvastatin revealed by functional improvement in muscular dystrophy. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(41):12864–12869. doi: 10.1073/pnas.1509536112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suga T., Kimura E., Morioka Y., et al. Muscle fiber type-predominant promoter activity in lentiviral-mediated transgenic mouse. PLoS One. 2011;6(3, article e16908) doi: 10.1371/journal.pone.0016908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duddy W., Duguez S., Johnston H., et al. Muscular dystrophy in the mdx mouse is a severe myopathy compounded by hypotrophy, hypertrophy and hyperplasia. Skeletal Muscle. 2015;5(1):p. 16. doi: 10.1186/s13395-015-0041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi M. K., Kim H. G., Han J. M., et al. Hepatoprotective effect of Terminalia chebula against t-BHP-induced acute liver injury in C57/BL6 mice. Evidence-based Complementary and Alternative Medicine. 2015;2015:11. doi: 10.1155/2015/517350.517350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang D., Wang H., Fu S., et al. Parthenolide ameliorates concanavalin A-induced acute hepatitis in mice and modulates the macrophages to an anti-inflammatory state. International Immunopharmacology. 2016;38:132–138. doi: 10.1016/j.intimp.2016.05.024. [DOI] [PubMed] [Google Scholar]
- 33.Giboney P. T. Mildly elevated liver transaminase levels in the asymptomatic patient. American Family Physician. 2005;71(6):1105–1110. [PubMed] [Google Scholar]
- 34.Brancaccio P., Maffulli N., Buonauro R., Limongelli F. M. Serum enzyme monitoring in sports medicine. Clinics in Sports Medicine. 2008;27(1):1–18. doi: 10.1016/j.csm.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 35.Moghadam-Kia S., Oddis C. V., Aggarwal R. Approach to asymptomatic creatine kinase elevation. Cleveland Clinic Journal of Medicine. 2016;83(1):37–42. doi: 10.3949/ccjm.83a.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burch P. M., Pogoryelova O., Goldstein R., et al. Muscle-derived proteins as serum biomarkers for monitoring disease progression in three forms of muscular dystrophy. Journal of Neuromuscular Diseases. 2015;2(3):241–255. doi: 10.3233/JND-140066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee E. M., Kim D. Y., Kim A. Y., et al. Chronic effects of losartan on the muscles and the serologic profiles of mdx mice. Life Sciences. 2015;143:35–42. doi: 10.1016/j.lfs.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 38.Veropalumbo C., del Giudice E., Esposito G., Maddaluno S., Ruggiero L., Vajro P. Aminotransferases and muscular diseases: a disregarded lesson. Case reports and review of the literature. Journal of Paediatrics and Child Health. 2012;48(10):886–890. doi: 10.1111/j.1440-1754.2010.01730.x. [DOI] [PubMed] [Google Scholar]
- 39.Shatton J. B., Morris H. P., Weinhouse S. Creatine kinase activity and isozyme composition in normal tissues and neoplasms of rats and mice. Cancer Research. 1979;39, 2, Part 1:492–501. [PubMed] [Google Scholar]
- 40.Jadaho S. B., Yang R.-Z., Lin Q., et al. Murine alanine aminotransferase: cDNA cloning, functional expression, and differential gene regulation in mouse fatty liver. Hepatology. 2004;39(5):1297–1302. doi: 10.1002/hep.20182. [DOI] [PubMed] [Google Scholar]
- 41.Jockers-Wretou E., Pfleiderer G. Quantitation of creatine kinase isoenzymes in human tissues and sera by an immunological method. Clinica Chimica Acta. 1975;58(3):223–232. doi: 10.1016/0009-8981(75)90441-6. [DOI] [PubMed] [Google Scholar]
- 42.Kang K. S. Abnormality on liver function test. Pediatric Gastroenterology, Hepatology & Nutrition. 2013;16(4):225–232. doi: 10.5223/pghn.2013.16.4.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rebalka I. A., Hawke T. J. Potential biomarkers of skeletal muscle damage. Biomarkers in Medicine. 2014;8(3):375–378. doi: 10.2217/bmm.13.163. [DOI] [PubMed] [Google Scholar]
- 44.Zhu Y., Zhang H., Sun Y., et al. Serum enzyme profiles differentiate five types of muscular dystrophy. Disease Markers. 2015;2015:7. doi: 10.1155/2015/543282.543282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brancaccio P., Lippi G., Maffulli N. Biochemical markers of muscular damage. Clinical Chemistry and Laboratory Medicine. 2010;48(6):757–767. doi: 10.1515/CCLM.2010.179. [DOI] [PubMed] [Google Scholar]
- 46.Pettersson J., Hindorf U., Persson P., et al. Muscular exercise can cause highly pathological liver function tests in healthy men. British Journal of Clinical Pharmacology. 2008;65(2):253–259. doi: 10.1111/j.1365-2125.2007.03001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bessa A., Nissenbaum M., Monteiro A., et al. High-intensity ultraendurance promotes early release of muscle injury markers. British Journal of Sports Medicine. 2008;42(11):889–893. doi: 10.1136/bjsm.2007.043786. [DOI] [PubMed] [Google Scholar]
- 48.Manning J., O’Malley D. What has the mdx mouse model of Duchenne muscular dystrophy contributed to our understanding of this disease? Journal of Muscle Research and Cell Motility. 2015;36(2):155–167. doi: 10.1007/s10974-015-9406-4. [DOI] [PubMed] [Google Scholar]
- 49.Radermacher P., Haouzi P. A mouse is not a rat is not a man: species-specific metabolic responses to sepsis - a nail in the coffin of murine models for critical care research? Intensive Care Medicine Experimental. 2013;1(1):p. 26. doi: 10.1186/2197-425X-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Partridge T. A. The mdx mouse model as a surrogate for Duchenne muscular dystrophy. FEBS Journal. 2013;280(17):4177–4186. doi: 10.1111/febs.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson M. A., Polgar J., Weightman D., Appleton D. Data on the distribution of fibre types in thirty-six human muscles. An autopsy study. Journal of the Neurological Sciences. 1973;18(1):111–129. doi: 10.1016/0022-510X(73)90023-3. [DOI] [PubMed] [Google Scholar]
- 52.Burkholder T. J., Fingado B., Baron S., Lieber R. L. Relationship between muscle Fiber types and sizes and muscle architectural properties in the mouse hindlimb. Journal of Morphology. 1994;221(2):177–190. doi: 10.1002/jmor.1052210207. [DOI] [PubMed] [Google Scholar]
- 53.Yucel N., Chang A. C., Day J. W., Rosenthal N., Blau H. M. Humanizing the mdx mouse model of DMD: the long and the short of it. npj Regenerative Medicine. 2018;3(1):1–11. doi: 10.1038/s41536-018-0045-4. [DOI] [PMC free article] [PubMed] [Google Scholar]