Abstract
Background
Doctors’ empathy is closely related to patients’ health. This study aimed to examine whether patients’ stigma and self-efficacy play a mediating role in the relationship between doctors’ empathy abilities and patients’ cellular immunity in male patients with breast cancer.
Material/Methods
Doctors’ empathy scores and patients’ demographic data, disease condition, stigma, and self-efficacy were measured. Patient T cell subset was tested at admission and 3 months after the operation and was compared by paired t test. The multivariate linear regression model was applied to analyze the factors influencing the immune index. Pearson correlation analysis and structural equation modeling were applied to explore the relationships among patients’ stigma, self-efficacy, and cellular immunity and doctors’ empathy abilities.
Results
At the 2 time points, only the change in NK subset was statistically significant, while the changes in percentage of CD3+, CD4+, CD8+, and B cells were not statistically significant. The doctors’ empathy abilities were negatively correlated with patients’ stigma and were positively related to patients’ self-efficacy. Patients’ stigma was negatively related to NK subset, while self-efficacy was positively associated with NK subset. Patients’ stigma and self-efficacy played a mediating role in the relationship between doctors’ empathy abilities and patients’ NK subset, and stigma had a stronger effect than self-efficacy.
Conclusions
Doctors’ empathy abilities affected breast cancer patients’ NK subset through their stigma and self-efficacy. The mental health of male breast cancer patients need more attention and empathy education needs to be improved.
MeSH Keywords: Breast Neoplasms, Male; Empathy; Immunity, Cellular; Self Efficacy
Background
Breast cancer is one of the most common malignant tumors among women, and it poses a serious threat to their health. However, male breast cancer is a rare disease, accounting for approximately 1% of all breast cancer patients. If a man gets breast cancer, the disease is often more serious and the overall survival (OS) is lower than in female patients [1]. For male patients, breast cancer not only harms their bodies and lives but also causes anxiety, depression, stigma, embarrassment, sense of isolation, and other negative emotions [2]. Published research reported male patients have more mental health problems than female patients, for various reasons. First, breast cancer is considered a disease that exclusively affects women, so it is strange for men to have breast cancer [3]. Second, the location of the disease is the breast, which is a secondary sex characteristic of females. The illness focusses attention on the male breasts, so a man may think this will reduce his masculinity. Third, the male breast has an erotic function and the main function of breasts is related to sexual pleasure, but this is often ignored by doctors [4,5]. So, if a man has breast cancer and receives treatment such as an operation, his sexual pleasure may be negatively affected. Because doctors often ignore this problem, they cannot offer any other intervention, such as reconstruction and psychological intervention [6]. Obviously, this also aggravates the psychological burden and stigma.
At present, mental health surveys and psychological rehabilitation programs for female breast cancer patients are relatively good. However, there has been little research on and psychological intervention for male breast cancer patients focussing on their psychological characteristics [7]. Therefore, more attention should be focused on the psychological health problems of these patients.
Psychoneuroimmunology and psychosocial oncology have become important topics in recent years. Many studies focused on cancer patients’ mental health, such as assessment of psychological health and effects of psychological intervention [8,9]. Some research has confirmed the relationships between mental state and immune function [10]. On this basis, the present study focused on relationships among doctors’ empathy abilities and patients’ psychology and immunity.
Empathy is one of the most important parts of the clinical medical humanities. It refers to the ability to identify with other people’s situations and to respond others’ feelings suitably. It is an important social skill and an individual trait that is relatively stable [11]. To medical personnel, the ability to be empathic is not only associated with patient outcomes [12], quality of care [13], and patient satisfaction [14], but is also related to their own professional quality of life [15].
The present study is innovative and significant in light of the following. First, it integrates psychoneuroimmunology, psychosocial oncology, and clinical medical humanities such as empathy. Second, medical humanities education, such as training in empathy abilities, is lacking in developing countries such as China. This study confirmed the effect of doctors’ empathy on the physical and mental health of patients and shows the need for medical personnel to pay attention to patient mental health and to improve their empathy abilities. Third, the study focused on male breast cancer patients, a population that has received insufficient attention.
This study explored the relationships among male breast patients’ psychological and immunological indexes and their doctors’ empathy abilities in clinical context. In this research, 2 hypotheses are proposed: Hypothesis 1: Doctors’ empathy affects patients’ cellular immunity directly; and Hypothesis 2: Doctors’ empathy affects patients’ cellular immunity through the mediating role of patients’ stigma and self-efficacy.
Material and Methods
Participants
We enrolled 256 male breast cancer patients treated at 58 hospitals in mainland China between July 2015 and April 2018. Inclusion criteria were: 1) Diagnosed with breast cancer and hospitalized for at least 5 days for surgery and 2) Knew their own diagnosis and gave informed consent for this study. Exclusion criteria were: 1) Underwent radiotherapy, chemotherapy, or Chinese traditional medicine within 3 months before the study began and 2) Severely malnourishment. In this study, 256 doctors were responsible for the treatment. During the hospitalization, doctors and patients had at least 2 in-depth conversations focusing on the disease, health education, or mental state. The Peking University Biomedical Ethics Committee approved the study (NO. IRIB00001052-15034).
Procedures
First, on the day of admission (T1), a cross-sectional, anonymous questionnaire covering essential information, disease condition, stigma, and self-efficacy was filled out by the male patients with breast cancer. At T1 and 3 months after the operation (T2), their cellular immunity was measured by collecting blood samples. The doctors’ empathy scores were measured when the research started. Second, the patients’ cellular immunity at T1 and T2 was compared, and the influences of demography and disease condition on immune indexes at T2 were analyzed. Third, the relationships among the patients’ stigma, self-efficacy, and immunity and the doctors’ empathy abilities were explored.
Measures
Patient questionnaire
The questionnaire was used to collect information on patient age, marital status, educational background, place of residence, monthly family income per capita, and family relationships. Disease condition, including transfer or not, and staging of disease was completed according to the medical records.
Patient stigma was measured by the Social Impact Scale (SIS). Fife and Wright invented the scale in 2000 [16]. It is a 4-point Likert scale with 24 items. The score of each response ranges from 1 to 4 and the total score of the scale ranges from 4 to 96, with higher scores indicating greater stigma. It consists of 4 dimensions: Social Rejection, Financial Insecurity, Internalized Shame, and Social Isolation. This scale is widely used and has good reliability and validity. In this study, the Chinese version was used [17].
Patient self-efficacy was measured by the Brief Version of the Cancer Behavior Inventory (CBI-B). It is a 12-item scale derived from the longer 33-item version (CBI-L), which is used to measure cancer patients’ self-efficacy. Heitzmann constructed it in 2011. The scale consists of 4 dimensions: Maintaining Independence and Positive Attitude; Participating in Medical Care; Coping and Stress Management; and Managing Affect. For the 12 questions, each response score ranges from 1 to 9, and the total score ranges from 12 to 108, with higher scores indicating higher self-efficacy [18,19].
Patients’ cellular immunity
Peripheral venous blood samples were collected between 9 a.m. and 10 a.m. before the questionnaires were filled in order to control for diurnal variation. Patients’ cellular immunity tests were completed by the professional staff working at the clinical laboratory of the hospital. T cell subsets, including the percentage of total T cells (CD3+), helper T cells (CD4+), cytotoxic T cells (CD8+), NK cells (CD56+), and B cells (CD19+), were measured. Flow cytometry was used to assess T and NK cell counts with a Cytomics™ FC500 series instrument from Beckman Coulter (USA). Reagents from BD Bio-Engineering Co., Ltd. were used. Cells were fixed in 3% formaldehyde in an isotonic azide-free solution (Beckman Coulter, Luton, UK). Labeled antibodies were added at the recommended concentrations and then cells were washed. Cells were cultured in the dark, and then excess antibodies were washed out.
Doctors’ empathy
The Chinese version of the Jefferson Scale of Empathy (JSE) was applied to measure doctors’ empathy. The scale was first constructed in 2001 by Hojat et al. to measure empathy abilities of medical staff [20]. The scale consists of 3 dimensions (compassion care, perspective taking, and standing in the patient’s shoes). There are 20 items answered on a 7-point Likert scale. Each response is converted to a numerical score ranging from 1 to 7: 1 indicates “Strongly Disagree” and 7 indicates “Strongly Agree” [21]. The total scores on the JSE range from 20 to 140, with higher scores indicating stronger empathy abilities. The JSE has good reliability and validity and is widely used many countries [22]. In this research, the Chinese version of the JSE was used to measure doctors’ empathy abilities. This scale has been widely used in Chinese samples [23].
Statistical analyses
The paired t test was used to compare the immune indices on admission and after 3 months. A multivariate linear regression model was used to analyze the factors influencing the immune index, showing statistically significant differences between T1 and T2. Pearson’s correlation analysis was used to preliminarily measure the relationships among patients’ stigma, self-efficacy, and immune indexes and the doctors’ empathy abilities. In this research, alpha=0.05 and the tests were two-tailed. The above data processing and analysis were carried out using SAS version 9.4 for Windows. Structural equation modeling (SEM) was performed using AMOS version 5 to further explore the relationships among patients’ stigma, self-efficacy, and immune index and doctors’ empathy. The indices of the model’s fit to the data were evaluated with the following statistics: GFI (>0.9), CFI (>0.9), RMSEA (<0.08), and chi-square/df (<2).
Results
Sample
In this research, all the selected doctors agreed to participate. Their median age was 40.21±7.12 years. Three hundred patients received our invitation to participate and 256 patients took part in the research, with a participation rate of 85.55%. The average age of sample patients was (61.10±7.86) years and the average number of hospitalization days was (6.43±0.88) days. Their basic data are shown in Table 1.
Table 1.
Patient demography and disease condition.
| Variable | Number | % |
|---|---|---|
| Educational background | ||
| Primary school or below | 63 | 24.6 |
| Junior middle school | 115 | 44.9 |
| Senior middle school | 61 | 23.8 |
| College or above | 17 | 6.6 |
| Mαριταλ στατυσ | ||
| Unmarried | 6 | 2.3 |
| Married | 220 | 85.9 |
| Divorced or widowed | 30 | 11.7 |
| Homeplace | ||
| Countryside | 81 | 31.6 |
| County town | 40 | 15.6 |
| Urban area | 135 | 52.7 |
| Monthly family income per capita | ||
| <3000 yuan | 90 | 35.2 |
| 3000–5000 yuan | 131 | 51.2 |
| >5000 yuan | 35 | 13.7 |
| Medical insurance stage | ||
| Private health care provision | 58 | 22.7 |
| Social security or commercial insurance | 142 | 55.5 |
| New rural cooperative medical system | 45 | 17.6 |
| Socialized medicine | 11 | 4.3 |
| Self-evaluation family relation | ||
| Poor | 50 | 19.5 |
| General | 90 | 35.2 |
| Good | 116 | 45.3 |
| Transfer | ||
| Yes | 114 | 44.5 |
| No | 142 | 55.5 |
| Long-term drinking | ||
| Yes | 14 | 5.5 |
| No | 242 | 94.5 |
| Smoking | ||
| Yes | 49 | 19.1 |
| No | 207 | 80.9 |
| Insomnia | ||
| Yes | 31 | 12.1 |
| No | 225 | 87.9 |
Comparison of cellular immune indices of patients at admission and 3 months after the operation
The comparison of the patients’ cellular immune indices at admission and 3 months later is shown in Table 2. At the 2 time points, the changes in NK subset showed statistically significant differences (P<0.01). Changes in the proportions of CD3, CD4, CD8, and B cells were not significant (P>0.05).
Table 2.
Comparison of cellular immune indices of patients at admission and 14 days later.
| % | At admission | 14 days later | t | P |
|---|---|---|---|---|
| CD3 | 59.07±7.70 | 60.08±6.97 | −1.68 | 0.10 |
| CD4 | 35.41±6.56 | 35.45±6.58 | −0.06 | 0.95 |
| CD8 | 30.01±5.75 | 29.62±6.93 | 0.78 | 0.43 |
| B | 7.91±2.92 | 8.11±2.57 | −1.13 | 0.26 |
| NK | 19.50±7.79 | 21.35±8.52 | −13.30 | <0.01 |
The effect of demographic characteristics and disease condition on the patients’ NK activity
Table 3 shows the results of the multivariate linear regression analysis. There was a statistically significant difference in NK activity between smokers and non-smokers (P<0.001). This indicates that smoking affects the patients’ NK subset.
Table 3.
The effect of demography and disease on the patients’ NK activity.
| β | Standard error | t | P | |
|---|---|---|---|---|
| Constant term | 19.46 | 7.17 | 2.72 | <0.01 |
| Age | 0.05 | 0.08 | 0.68 | 0.50 |
| Hospitalization days | −0.97 | 0.67 | −1.45 | 0.15 |
| Education (reference group: Primary school or below) | ||||
| Junior middle school | 1.14 | 1.45 | 0.79 | 0.43 |
| Senior middle school | 1.59 | 1.85 | 0.86 | 0.39 |
| College or above | 0.05 | 2.87 | 0.02 | 0.99 |
| Marriage (reference group: Unmarried) | ||||
| Married | 0.66 | 3.68 | 0.18 | 0.86 |
| Divorced or widowed | −0.35 | 3.99 | −0.09 | 0.93 |
| Homeplace (reference group: Countryside) | ||||
| County town | −0.05 | 2.07 | −0.02 | 0.98 |
| Urban area | 1.71 | 2.05 | 0.83 | 0.41 |
| Monthly family income per capita (reference group: <3000 yuan) | ||||
| 3000–5000 yuan | −1.73 | 1.47 | −1.18 | 0.24 |
| >5000 yuan | −2.68 | 2.00 | −1.34 | 0.18 |
| Medical insurance (reference group: Private health care provision) | ||||
| Social security or commercial insurance | −1.68 | 1.06 | −1.05 | 0.30 |
| New rural cooperative medical system | −0.05 | 1.92 | −0.03 | 0.98 |
| Socialized medicine | −2.35 | 2.93 | −0.8 | 0.42 |
| Self-evaluation family relation (reference group: Poor) | ||||
| General | 0.39 | 1.62 | 0.24 | 0.81 |
| Good | 2.61 | 1.76 | 1.49 | 0.14 |
| Transfer (reference group: No) | ||||
| Yes | −1.39 | 1.18 | −1.18 | 0.24 |
| Long-term drinking (reference group: No) | ||||
| Yes | 2.84 | 2.40 | 1.18 | 0.24 |
| Smoking (reference group: No) | ||||
| Yes | 2.25 | 0.68 | 3.3 | 0.001 |
| Insomnia (reference group: No) | ||||
| Yes | 2.84 | 2.40 | 1.18 | 0.24 |
The relationships among doctors’ empathy abilities and patients’ stigma, self-efficacy, and NK subset
Through Pearson’s correlation analysis, the relationships among patients’ stigma, self-efficacy, and NK activity and doctors’ empathy abilities were explored. The results are shown in Table 4. Doctors’ empathy abilities were negatively correlated with patients’ stigma (r=-0.799, P<0.01) and were positively correlated with patients’ self-efficacy and NK activity (r=0.726, r=0.641; P<0.01). Patients’ stigma was negatively correlated with their self-efficacy and NK activity (r=−0.789; r=−0.719; P<0.01), and their self-efficacy was positively correlated with NK activity (r=0.693; P<0.01). Base on these results, the structural equation model method was used in the next step.
Table 4.
The correlations among doctors’ empathy abilities and patients’ stigma, self-efficacy and NK activity.
| Score | Empathy | Stigma | Self-efficacy | NK activity | |
|---|---|---|---|---|---|
| Doctors’ empathy abilities | 104.89±13.766 | 1 | |||
| Patients’ stigma | 64±18.153 | −0.799** | 1 | ||
| Patients’ self-efficacy | 68.14±16.295 | 0.726** | −0.789** | 1 | |
| Patients’ NK activity | 21.35±8.524 | 0.645** | −0.719** | 0.693** | 1 |
P<0.05;
P<0.01.
The structural equation model of the relationship among doctors’ empathy abilities and patients’ stigma, self-efficacy, and NK activity
According to the above analysis, a correlation among doctors’ empathy abilities and patients’ stigma, self-efficacy and NK activity was identified. To further clarify the relationships among these factors, the path analysis method was used to construct multiple intermediary models. The hypotheses were: (1) Doctors’ empathy directly affects patients’ NK activity and (2) Patients’ stigma and self-efficacy mediate the relationship between doctors’ empathy abilities and patients’ NK activity. Based on these 2 hypotheses, the structural equation model was constructed. In this model, the path coefficient through which doctors’ empathy abilities affect patients’ NK activity directly was not significant, indicating that hypothesis 1 was invalid. The final model is shown in Figure 1.
Figure 1.
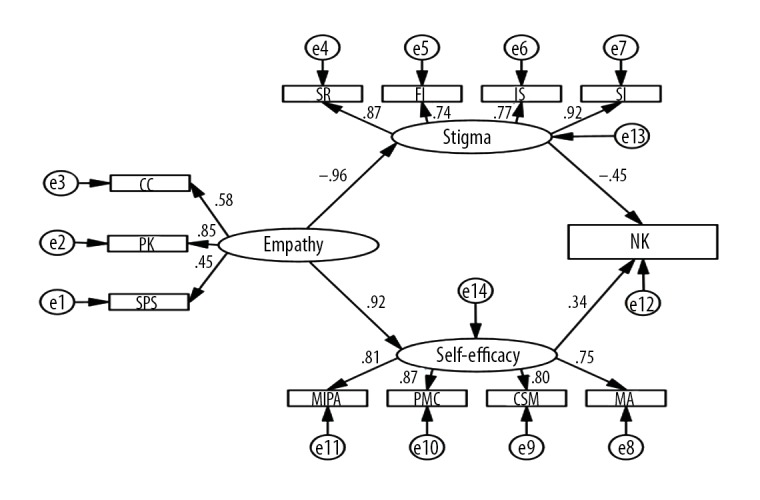
The model of the relationships among doctor’s empathy abilities and patients’ stigma, self-efficacy and NK activity.
To investigate the indices of the hypothesis model described above, AMOS software was used. The model fit result was: χ2=89.619; χ2/df=1.757, RMSEA=0.054, GF=0.937I, AGFI=0.904, CFI=0.982, and NFI=0.940. These values indicate that the data fit the hypothesized model well.
Table 5 shows the normalized path coefficient. The path coefficient for the effects of doctors’ empathy abilities on patients’ stigma was −0.96 and for the effects on patients’ self-efficacy, the path coefficient was 0.918. The path coefficient of the effects of patients’ stigma on their NK activity was −0.455 and for the effects of patients’ self-efficacy on their NK activity, the path coefficient was 0.336. These values were all significant at alpha=0.05.
Table 5.
Normalized path coefficient.
| Path | Normalized path coefficient | S.E. | C.R. |
|---|---|---|---|
| Doctors’ empathy abilities → patients’ stigma | −0.96 | 0.916 | −7.365** |
| Doctors’ empathy abilities → patients’ self-efficacy | 0.918 | 0.433 | 6.919** |
| Patients’ stigma → NK activity | −0.455 | 0.158 | −3.778** |
| Patients’ self-efficacy → NK activity | 0.336 | 0.344 | 2.749* |
Bootstrapping was applied to clarify the mediating effect. The confidence interval was set at 95%, and the number of self-samples was set at 5000. The obtained mediation results are shown in Table 6. The confidence interval of the path between doctors’ empathy abilities and patients’ NK activity was 0.071 (95%CI: −0.017, 0.158), and 0 is included. When 0 was not contained in the confidence interval, the mediating effect was significant. The results showed that the confidence interval of the gross effect was 0.328 (95%CI: 0.246, 0.412). Therefore, doctors’ empathy abilities affected patients’ NK activity through the intermediary factors of patients’ stigma and self-efficacy (full mediation). Stigma and self-efficacy played significant intermediary roles and the effects were 0.192 (95%CI: 0.104, 0.297) and 0.137 (95%CI: 0.058, 0.218).
Table 6.
Bootstrap indirect effects analysis of nonparametric ratios.
| Mediating effect path | Indirect effect | Standard error | 95% CI | |
|---|---|---|---|---|
| BootLLCI | BootULCL | |||
| Doctors’ empathy abilities → NK activity | 0.0708 | 0.444 | −0.0167 | 0.1583 |
| Gross effect | 0.3284 | 0.416 | 0.2461 | 0.4120 |
| Empathy → stigma → NK activity | 0.1915 | 0.0496 | 0.1037 | 0.2967 |
| Empathy → self-efficacy → NK activity | 0.1369 | 0.0413 | 0.0575 | 0.2183 |
Discussion
When the immune indices of the 2 time points were compared, we found that only the changes in NK subset were statistically significant. The reason for this result needs further exploration in the future. Among demography and disease condition, smoking is an influential factor in the patients’ NK subset, which has been confirmed by previous research [24]. This reveals that the patients should quit smoking. Then, the 2 hypotheses on the relationships among patients’ stigma, self-efficacy, NK subset and doctors’ empathy abilities were tested by path analysis. The results are as follows:
On the one hand, the hypothesis that doctors’ empathy abilities affect patients’ cellular immunity directly was rejected. This indicates that patients’ NK activity cannot be affected by doctors’ empathy directly. On the other hand, the hypothesis that doctors’ empathy abilities affect patients’ cellular immunity through the mediated role of patients’ stigma and self-efficacy was accepted. The mechanism of empathy affecting the patients’ immunity can be explained as the following 2 steps. First, doctors’ empathy abilities affected patients’ self-efficacy and stigma directly. Second, patients’ stigma and self-efficacy affected their NK subset directly.
At the first step, results showed doctors’ empathy abilities were negatively related to patients’ stigma and positively related to patients’ self-efficacy. Several studies have confirmed the importance of medical personnel’s empathy to patients’ mental health. For instance, Weiss found that responding empathically helped reduce the anxiety of patients [25]. Flickinger found that the empathy of doctors was related to the self-efficacy of AIDS patients [26]. This phenomenon can be explained as follows: (1) Male breast cancer patients often bear huge psychological burdens and hope to have others’ understanding and support. Doctors with strong empathy abilities are more willing to listen and respect the narration of patients, and to respond to them in the process of conversation [27]. In the narrative, confiding itself is a way to release pressure for the patients, which helps reduce the stigma and improve self-efficacy. On the other hand, doctors with strong empathy abilities and narrative abilities can help patients promote acceptance on the disease and excavate the significance of disease, which may improve the mental health of the patients [28]. (2) With empathy, it is easy to carry out high-quality targeted health education. Doctors with strong empathy abilities can understand the patients’ situation and characteristics and propose appropriate health education suggestions to them. Therefore, patients have greater compliance and faster postoperative recovery. With the recovery of the body, their mental state will be better [29]. (3) Patients can get more targeted psychological counseling and humane care from doctors with strong empathy abilities. Through full empathy, doctors can stand in the patients’ shoes to understand their feelings, such as fear and stigma, so they can comfort and help the patients better [30]. They will also make some suggestions about the psychosocial needs of patients. For example, they can ask social workers, psychologists, or the patient’s family members to participate in the treatment and rehabilitation. Therefore, patients will gain more social support and social capital, which may help them relieve the stigma and improve their self-efficacy [31]. (4) Empathy promotes shared decision-making and patient-centered care [32,33]. This is a manifestation of respect for the patient’s autonomy and can improve their sense of dignity. Thus, patients will feel less stigma and develop more self-efficacy.
At the second step, patients’ stigma and self-efficacy affecting their NK subset was confirmed. The NK subset was negatively associated with stigma and was positively associated with self-efficacy. The relationship between mental state and immunity has been confirmed by many psychoneuroimmunology studies [34]. The impact mechanism includes the HPA axis and sympathetic nervous system [35,36]. Therefore, in this research, as a negative emotion, stigma may make the NK subset decline, while self-efficacy is a positive emotion which may make the NK subset rise.
Previous studies have also supported the impact of empathy on physical parameters of patients. For example, Hojat et al. confirmed that physicians’ empathy helps diabetic patients have good control of hemoglobin A1c and LDL-C levels [37] and reduce disease complications [38]. These conclusions suggest that it is important to improve empathy abilities of medical personnel through multiple ways. It is also necessary to integrate empathy education into medical education, including school education and continuing education. Narrative medicine courses may be suitable and effective [39]. The finding that patient stigma and self-efficacy play a mediated role in the relationship between doctors’ empathy abilities and patients’ NK subset shows that targeted health education focusing on reducing patients’ stigma and improving their self-efficacy should be carried out. Also, health education should be extended to the family members of the patients. In this way, the patients will get more social support, and their physical and mental health will be better.
Another finding was that patients’ stigma affected their NK subset more than their self-efficacy did. Additionally, doctors’ empathy abilities affected patients’ stigma more than their self-efficacy. As stated earlier, since the breast is a male sexual organ and this is often denied by doctors, patients may have more stigma, which may affect their cellular immunity. This reminds us that patients are sensitive to stigma, and doctors themselves should have a more scientific and objective understanding of male breast cancer. On this basis, they can give patients more care, understanding, and love.
There are limitations to this study. First, the human immune system is reexamined, and immune function is influenced by many factors. This study does not cover all possible factors. Second, in this study, the measurement of empathy ability of doctors comes from the perspective of doctors (their self-assessment questionnaire). The measurement of empathy abilities should be combined with more objective evidence.
Third, this study only selected 2 time points. A longer cohort study should be performed in the future.
Conclusions
This research confirms that doctors’ empathy abilities affect patients’ psychological parameters and immunity. Male breast cancer patients’ stigma and self-efficacy play a mediating role in the impact of doctors’ empathy on patients’ immune function. This reveals that the mental health of male breast cancer patients needs more attention, as does empathy training for medical personnel.
Acknowledgements
The authors thank all the patients who generously participated in this study at such a difficult time in their lives, and all of the doctors who participated in the study.
Footnotes
Source of support: Departmental sources
Conflict of interests
None.
References
- 1.Lautrup MD, Thorup SS, Jensen V, et al. Male breast cancer: A nation-wide population-based comparison with female breast cancer. Acta Oncol. 2018;57:613–21. doi: 10.1080/0284186X.2017.1418088. [DOI] [PubMed] [Google Scholar]
- 2.Ruddy KJ, Giobbie-Hurder A, Giordano SH, et al. Quality of life and symptoms in male breast cancer survivors. Breast. 2013;22:197–99. doi: 10.1016/j.breast.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Silva TLD. Male breast cancer: Medical and psychological management in comparison to female breast cancer. A review. Cancer Treat Commun. 2016;7:23–34. [Google Scholar]
- 4.Misery L, Talagas M. Innervation of the male breast: Psychological and physiological consequences. J Mammary Gland Biol Neoplasia. 2017;22:109–15. doi: 10.1007/s10911-017-9380-0. [DOI] [PubMed] [Google Scholar]
- 5.Cazala F, Vienney N, Stoléru S. The cortical sensory representation of genitalia in women and men: A systematic review. Socioaffect. Neurosci Psychol. 2015;5:26428. doi: 10.3402/snp.v5.26428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Staruch RM, Rouhani MJ, Ellabban M. The surgical management of male breast cancer: Time for an easy access national reporting database? Ann Med Surg (Lond) 2016;9:41–49. doi: 10.1016/j.amsu.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiao F, Song X, Chen Q, et al. Effectiveness of psychological interventions on depression in patients after breast cancer surgery: A meta-analysis of randomized controlled trials. Clin Breast Cancer. 2017;17:171–79. doi: 10.1016/j.clbc.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Garssen B, Boomsma MF, Beelen RH. Psychological factors in immunomodulation induced by cancer surgery: A review. Biol Psychol. 2010;85:1–13. doi: 10.1016/j.biopsycho.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Archer S, Buxton S, Sheffield D. The effect of creative psychological interventions on psychological outcomes for adult cancer patients: A systematic review of randomised controlled trials. Psychooncology. 2015;24:1–10. doi: 10.1002/pon.3607. [DOI] [PubMed] [Google Scholar]
- 10.Mcdonald PG, O’Connell M, Lutgendorf SK. Psychoneuroimmunology and cancer: A decade of discovery, paradigm shifts, and methodological innovations. Brain Behav Immun. 2013;30:S1–9. doi: 10.1016/j.bbi.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Preston SD, Waal FBMD. Empathy: Its ultimate and proximate bases. Behav Brain Sci. 2002;25:1–20. doi: 10.1017/s0140525x02000018. [DOI] [PubMed] [Google Scholar]
- 12.Pincus T, Holt N, Vogel SO, et al. Cognitive and affective reassurance and patient outcomes in primary care: A systematic review. Pain. 2013;154:2407–16. doi: 10.1016/j.pain.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Yuguero O, Marsal JR, Buti M, et al. Descriptive study of association between quality of care and empathy and burnout in primary care. BMC Med Ethics. 2017;18(1):54. doi: 10.1186/s12910-017-0214-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menendez ME, Chen NC, Mudgal CS, et al. Physician empathy as a driver of hand surgery patient satisfaction. J Hand Surg Am. 2015;40:1860–65. doi: 10.1016/j.jhsa.2015.06.105. [DOI] [PubMed] [Google Scholar]
- 15.Duarte J, Pintogouveia J, Cruz B. Relationships between nurses’ empathy, self-compassion and dimensions of professional quality of life: A cross-sectional study. Int J Nurs Stud. 2016;60:1–11. doi: 10.1016/j.ijnurstu.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 16.Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. 2000;41:50–67. [PubMed] [Google Scholar]
- 17.Pan AW, Chung L, Fife BL, Hsiung PC. Evaluation of the psychometrics of the Social Impact Scale: A measure of stigmatization. Int J Rehabil Res. 2007;30:235–38. doi: 10.1097/MRR.0b013e32829fb3db. [DOI] [PubMed] [Google Scholar]
- 18.Heitzmann CA, Merluzzi TV, Jeanpierre P, et al. Assessing self-efficacy for coping with cancer: Development and psychometric analysis of the brief version of the Cancer Behavior Inventory (CBI-B) Psychooncology. 2011;10:302–12. doi: 10.1002/pon.1735. [DOI] [PubMed] [Google Scholar]
- 19.Merluzzi TV, Nairn RC, Hegde K, et al. Self-efficacy and coping with cancer: Revision of the Cancer Behavior Inventory (Version 2.0) Psychooncology. 2001;10:206–17. doi: 10.1002/pon.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: Development and preliminary psychometric data. Educ Psychol Meas. 2001;61:349–65. [Google Scholar]
- 21.Hojat M. Empathy in patient care: Antecedents, development, measurement, and outcomes. New York: Springer; 2007. pp. 12–20. [Google Scholar]
- 22.Costa P, de Carvalho-Filho MA, Schweller M, et al. Measuring medical students’ empathy: Exploring the underlying constructs of and associations between two widely used self-report instruments in five countries. Acad Med. 2017;92:860–67. doi: 10.1097/ACM.0000000000001449. [DOI] [PubMed] [Google Scholar]
- 23.Wen D, Ma X, Li H, Xian B. Empathy in Chinese physicians: Preliminary psychometrics of the Jefferson Scale of Physician Empathy (JSPE) Med Teach. 2013;35:609–10. doi: 10.3109/0142159X.2013.774338. [DOI] [PubMed] [Google Scholar]
- 24.Inoue C, Takeshita T, Kondo H, Morimoto K. Cigarette smoking is associated with the reduction of lymphokine-activated killer cell and natural killer cell activities. Environ Health Prev Med. 1996;1:14–9. doi: 10.1007/BF02931167. [DOI] [PubMed] [Google Scholar]
- 25.Weiss R, Vittinghoff E, Fang MC, et al. Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters. J Hosp Med. 2017;12:805–10. doi: 10.12788/jhm.2828. [DOI] [PubMed] [Google Scholar]
- 26.Flickinger TE, Saha S, Roter D, et al. Clinician empathy is associated with differences in patient-clinician communication behaviors and higher medication self-efficacy in HIV care. Patient Educ Couns. 2015;99:220–26. doi: 10.1016/j.pec.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spencer AC. Stories as gift: Patient narratives and the development of empathy. J Genet Couns. 2016;25:687–90. doi: 10.1007/s10897-015-9886-9. [DOI] [PubMed] [Google Scholar]
- 28.Egnew TR. A narrative approach to healing chronic illness. Ann Fam Med. 2018;16:160–65. doi: 10.1370/afm.2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forstater A, Hojat M, Chauan N, et al. Does patient perception of physician empathy affect patient compliance in the emergency department? Ann Emerg Med. 2012;60:S98. [Google Scholar]
- 30.Martin L, Emilie B, Franck Z, Serge S. To be or not to be empathic: the combined role of empathic concern and perspective taking in understanding burnout in general practice. Bmc Fam Practi. 2014;15:1–7. doi: 10.1186/1471-2296-15-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang H, Xiao L, Ren G. Experiences of social support among Chinese women with breast cancer: A qualitative analysis using a framework approach. Med Sci Monit. 2018;24:574–81. doi: 10.12659/MSM.908458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thompson C, Barforoshi S, Kell C, Banerjee D. Uncovering the patient experience: Empathy mapping promotes patient-centered care for improved heart failure patient outcomes. J Card Fail. 2016;22:S87–88. [Google Scholar]
- 33.Quaschning K, Körner M, Wirtz M. Analyzing the effects of shared decision-making, empathy and team interaction on patient satisfaction and treatment acceptance in medical rehabilitation using a structural equation modeling approach. Patient Educ Couns. 2013;91:167–75. doi: 10.1016/j.pec.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 34.Moraes LJ, Miranda MB, Loures LF, et al. A systematic review of psychoneuroimmunology-based interventions. Psychol Health Med. 2018;23:635–52. doi: 10.1080/13548506.2017.1417607. [DOI] [PubMed] [Google Scholar]
- 35.Maier SF, Watkins LR, Fleshner M. Psychoneuroimmunology. The interface between behavior, brain, and immunity. Am Psychol. 1994;49:1004–17. doi: 10.1037//0003-066x.49.12.1004. [DOI] [PubMed] [Google Scholar]
- 36.Maestroni GJ. Sympathetic nervous system influence on the innate immune response. Ann N Y Acad Sci. 2006;1069:195–207. doi: 10.1196/annals.1351.017. [DOI] [PubMed] [Google Scholar]
- 37.Hojat M, Louis DZ, Markham FW, et al. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–64. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 38.Del Canale S, Louis DZ, Maio V, et al. The relationship between physician empathy and disease complications: An empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med. 2012;87:1243–49. doi: 10.1097/ACM.0b013e3182628fbf. [DOI] [PubMed] [Google Scholar]
- 39.Miller E, Balmer D, Hermann MN, et al. Sounding narrative medicine: Studying students’ professional identity development at Columbia University College of physicians and surgeons. Acad Med. 2014;89:335–42. doi: 10.1097/ACM.0000000000000098. [DOI] [PMC free article] [PubMed] [Google Scholar]


