Chronic lymphocytic leukemia (CLL) commonly leads to immune dysfunction especially hypogammaglobulinemia, increasing risk of infection. Infection remains a major cause of mortality and morbidity in CLL with studies showing this accounts for a third to a half of all deaths.1–3 Immunoglobulin G (IgG) is the most prevalent and frequently monitored immunoglobulin in relation to immune function in CLL. It is widely accepted that there is a relationship between IgG deficiency and infection, albeit with some dispute in literature.1,4,5
Treatment of CLL has been transformed within the last two decades, firstly by the introduction of chemo-immunotherapeutic regimens and more recently by a range of small molecule inhibitors, including ibrutinib, idelalisib and venetoclax, which target the Brutons tyrosine kinase (Btk), PI3-kinase δ and Bcl-2, respectively. These revolutions in treatment are resulting in unprecedented survival rates among CLL patients. New treatment paradigms and the significant improvements in outcomes have driven a number of recent studies that have re-examined the relationship between immunoglobulin deficiencies in CLL, infection risk and survival.
Andersen et al. in Haematologica, report a Danish nationwide study examining the incidence and predictors of infection in CLL.6 The cohort consisted of 2905 patients from the Danish registry with a median follow up of 2.9 years, which represented all patients diagnosed in Denmark from 2010 to 2016. Infection remained a major cause of mortality and morbidity with around 23% of patients having an infection prior to treatment. Infections were common before and after treatment for CLL, with 11% requiring treatment within a year of a documented infection. Of those patients with an infectious complication, around 10% died within 30 days, and 25% died within a year of their infection. Age, sex, Binet stage, β-2-microglobulin and unmutated IGHV were all associated with higher risk of infection, as were IgA, IgM and IgG deficiency; IgA was found to be the best predictor of infection in the aspects of immune function measured.
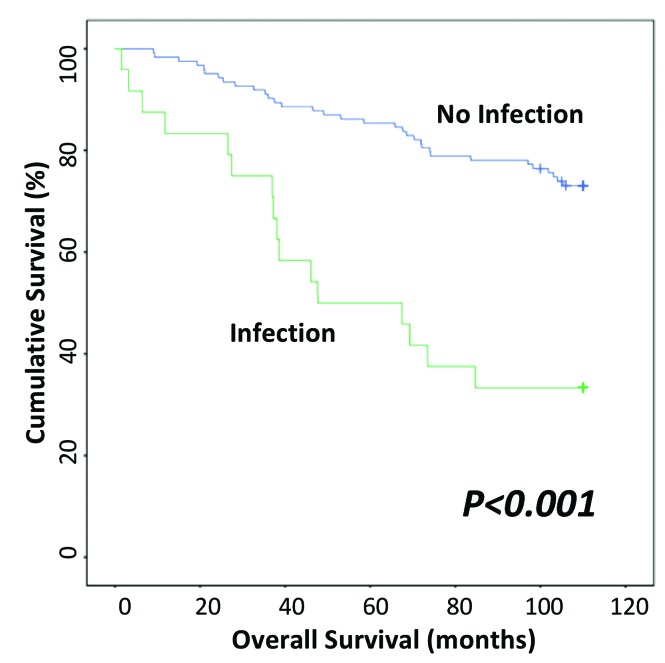
In 2018, we reported long-term follow-up data of 9.5 years on a cohort of 150 patients with CLL, examining the relationship between immunoglobulin deficiency and treatment free and overall survival (OS).7 Disease progression requiring treatment occurred in approximately 45% of these patients. In light of the Danish study, we examined the OS of 147 of the original 150 patients, comparing those with and without infectious complications within the year of observation. The survival curve (Figure 1) illustrates the significant association (P<0.001) between infection and OS, a relationship that retained significance in multivariate analysis (P=0.001). We also confirmed in our patient cohort the relationship between advanced Binet stage and shorter OS.
Figure 1.
Overall survival Kaplan-Meier curve from the time of assessment of immunoglobulin levels until death or follow up for all included patients. Overall survival Kaplan-Meier curve shown by infection (P<0.001) for the whole study cohort.
The data from our study and those of Andersen et al. are remarkably similar despite marked differences in infection documentation; physician assessed “serious or recurrent infection”7 versus having a positive blood culture.6 These studies demonstrate that infection remains a major risk in CLL, with a highly significant impact on survival, and remains a challenge in the management of CLL in spite of the obvious advances in therapy.
Supplementary Material
Footnotes
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
- 1.Andersen MA, Vojdeman FJ, Andersen MK, et al. Hypogammaglobulinemia in newly diagnosed chronic lymphocytic leukemia is a predictor of early death. Leuk Lymphoma. 2016; 57(7):1592–1599. [DOI] [PubMed] [Google Scholar]
- 2.Francis S, Karanth M, Pratt G, et al. The effect of immunoglobulin VH gene mutation status and other prognostic factors on the incidence of major infections in patients with chronic lymphocytic leukemia. Cancer. 2006;107(5):1023–1033. [DOI] [PubMed] [Google Scholar]
- 3.Morrison VA. Infectious complications in patients with chronic lymphocytic leukemia: pathogenesis, spectrum of infection, and approaches to prophylaxis. Clin Lymphoma Myeloma. 2009;9(5):365–370. [DOI] [PubMed] [Google Scholar]
- 4.Molica S. Infections in chronic lymphocytic leukemia: risk factors, and impact on survival, and treatment. Leuk Lymphoma. 1994;13(3-4):203–214. [DOI] [PubMed] [Google Scholar]
- 5.Rossi D, De Paoli L, Rossi FM, et al. Early stage chronic lymphocytic leukaemia carrying unmutated IGHV genes is at risk of recurrent infections during watch and wait. Br J Haematol. 2008;141(5):734–736. [DOI] [PubMed] [Google Scholar]
- 6.Andersen MA, Eriksen CT, Brieghel C, et al. Incidence and predictors of infection among patients prior to treatment of chronic lymphocytic leukemia: a Danish nationwide cohort study. Haematologica. 2018. March 8 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crassini KR, Zhang E, Balendran S, et al. Humoral immune failure defined by immunoglobulin class and immunoglobulin G subclass deficiency is associated with shorter treatment-free and overall survival in Chronic Lymphocytic Leukaemia. Br J Haematol. 2018;181(1):97–101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.