Abstract
Introduction/ Goals:
The aim of our study was to point out the importance of the risk factors associated with cervical cancer in an asymptomatic population.
Methodology:
The study included 860 patients in the period from January 2017 to January 2018, which covered more than 80% of the targeted population in this municipality over the one year study, according to the National Program for Cervical Cancer Prevention in Montenegro.
Results:
The incidence of PAP III results was statistically significantly higher in women between 40 and 45 years of age compared to other age groups (p< 0.001). PAP III was statistically significant high in subjects who had vaginal delivery (p<0.001), and was statistically significantly more frequent in women with more than two children (p = 0.011), while all the subjects with positive PAP results III had children. PAP III results were statistically significantly higher in subjects who had sexual intercourse before the age of 18 (p< 0.001), and were statistically significantly more frequent in subjects who were on oral contraceptives (p< 0.001). PAP III test results also show a significant difference related to cigarette consumption (p< 0.001). PAP III results were significantly more frequent in subjects with grade III vaginal cleanliness compared to grade II vaginal cleanliness (p<0.001).
Conclusion:
The number of patients with cervical cancer in Montenegro increased in the period from June 2016 to June 2017, compared to previous years, even though the National Program for Cervical Cancer Prevention that aimed to reduce the number of such patients has been in use in Montenegro since 2011.
Keywords: cervical cancer, pap test
1. INTRODUCTION
Cervical cancer is still one of the most common malignant diseases in the world, ranked second in its frequency, which is indicative of the pandemic characteristic of this type of cancer, with more than 80% of cases being detected in the developing countries (Montenegro being one of them). According to the data available to the World Health Organization (WHO), about half a million women worldwide develop cervical cancer each year, accounting for 12% of all malignant diseases in women. Every two minutes one women dies from cervical cancer which leads us to conclude that for 230 000 of these women this disease is terminal (1, 2, 3). According to the data from 2015, in Europe 12-30/100,000 women are affected by cervical cancer. The frequency is higher in poorly developed countries, while it is declining in most of the highly developed countries due to well-organized screening. The incidence of cervical cancer is at the second inglorious place among other malignant diseases affecting women in Montenegro, immediately after breast cancer. According to the available data for 2016, in Montenegro more than 100 women are affected annually, with a terminal outcome in 30-40 of them (2. 3).
For comparison, the regional data show that in Croatia 16/100 000 women are affected, while in Serbia 24.3/100 000 women are affected, making Serbia one of the leading countries in Southeastern Europe in the frequency of cervical cancer (2.4). It should be emphasized that there has been an increase in incidence and mortality rate of this disease among the younger population in the recent years (2).
2. AIM
The aim of our study was to point out the importance of risk factors and to determine the prevalence of the most important risk factors associated with the development of cervical cancer in asymptomatic (general) population.
3. MATERIALS AND METHODS
A clinical study was conducted at the Department of Obstetrics and Gynecology of the Community Health Center in Rozaje, with the purpose of a timely detection, treatment, and reduction of incidence and mortality rate of cervix cancer in Montenegro, in accordance with the ethical principles of the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Medicine in Podgorica.
The study included 860 patients in the period from January 2017 to January 2018, which covered more than 80% of the targeted population in this municipality over the one year study, according to the National Program for Cervical Cancer Prevention in Montenegro. The subjects were examined for the well-known, long-defined factors and co-factors, which are the main causes of cervical cancer (the number of births, the type of delivery, smoking, the number of children, the use of oral contraceptives, bacterial-viral infections, the time of first sexual intercourse, and the use of an intrauterine device).
Data Analysis
For the analysis of primary data we used descriptive statistical methods and analytical methods. Among the descriptive statistical methods used were the absolute and relative numbers, chi-square test for the analysis of frequency differences and Fisher’s exact probability test. Statistical hypotheses were tested at the level of statistical significance (alpha level) of 0.05. For the purpose of statistical data analysis, SPSS Statistics 22 (SPSS Inc., Chicago, IL, USA) software package was used.
4. RESULTS
Class 2 Pap smear (PAP II) results were highly prevalent in all age groups, with the incidence of over 95% in most groups. PAP II results were detected in all the subjects belonging to the 22-27 and 58-63 age groups, while the subjects belonging to the 40-45 age group had the lowest incidence of PAP II, amounting to 89% (Table 1).
Table 1. Characteristics of subjects in relation to Pap II results.
| Characteristics of subjects | PAP II | |
|---|---|---|
| No | Yes | |
| Total number n (%) | 17 (2%) | 843 (98%) |
| Years of age | ||
| 16-21 years of age n(%) | 1 (7.7) | 12 (92.3) |
| 22-27 years of age n(%) | 0 (0.0) | 78 (100.0) |
| 28-33 years of age n(%) | 2 (1.8) | 112 (98.2) |
| 34-39 years of age n(%) | 1 (0.6) | 166 (99.4) |
| 40-45 years of age n(%) | 16 (11.3) | 125 (88.7) |
| 46-51 years of age n(%) | 4 (3.0) | 129 (97.0) |
| 52-57 years of age n(%) | 5 (4.3) | 112 (95.7) |
| 58-63 years of age n(%) | 0 (0.0) | 66 (100.0) |
| 64-69 years of age n(%) | 1 (3.2) | 30 (96.8) |
| Type of delivery | ||
| No delivery n(%) | 0 (0.0) | 22 (100.0) |
| Vaginal n(%) | 29 (4.4) | 635 (95.6) |
| Caesarean n(%) | 1 (0.6) | 173 (99.4) |
| Number of children | ||
| No children n(%) | 0 (0.0) | 22 (100.0) |
| Up to two n(%) | 4 (1.6) | 250 (98.4) |
| More than two n(%) | 26 (4.5) | 558 (95.5) |
| Women without children | ||
| No n(%) | 30 (3.6) | 814 (96.4) |
| Yes n(%) | 0 (0.0) | 16 (100.0) |
| Sexual intercourse before the age of 18 | ||
| No n(%) | 15 (1.9) | 767 (98.1) |
| Yes n(%) | 15 (19.2) | 63 (80.8) |
| Oral contraception | ||
| No n(%) | 21 (2.6) | 793 (97.4) |
| Yes n(%) | 9 (19.6) | 37 (80.4) |
| Intrauterine device | ||
| No n(%) | 27 (3.5) | 752 (96.5) |
| Yes n(%) | 3 (3.7) | 78 (96.3) |
| Smoking | ||
| No n(%) | 13 (2.0) | 629 (98.0) |
| Yesn(%) | 17 (7.8) | 201 (92.2) |
| Colposcopy | ||
| Not done | 2 (0.2) | 843 (99.8) |
| Satisfactory | 3 (100.0) | 0 (0.0) |
| Low-grade | 12 (100.0) | 0 (0.0) |
| Grade of vaginal cleanliness | ||
| Group I | 0 (0.0) | 1 (100.0) |
| Group II | 9 (1.4) | 655 (98.6) |
| Group III | 20 (10.3) | 174 (89.7) |
| Group VI | 1 (100.0) | 0 (0.0) |
The incidence of PAP II results was statistically significantly higher in women with vaginal delivery (p = 0.007). PAP III results were confirmed only in subjects with vaginal delivery with an incidence of 4.4%. PAP III results were statistically significantly higher in subjects with vaginal delivery (p<0.001) (Table 2). PAP III results were statistically significantly more frequent in women with more than two children (p = 0.011). All subjects with positive PAP III results had given birth, and all PAP III results were present only in subjects with vaginal delivery.
Table 2. Characteristics of subjects in relation to Pap III results.
| Characteristics of subjects | PAP II | |
|---|---|---|
| No | Yes | |
| Total number n (%) | 844 (98%) | 16 (2%) |
| Years of age | ||
| 16-21years of age n(%) | 13 (100.0) | 0 (0.0) |
| 22-27 years of age n(%) | 78 (100.0) | 0 (0.0) |
| 28-33 years of age n(%) | 112 (98.2) | 2 (1.8) |
| 34-39 years of age n(%) | 166 (99.4) | 1 (0.6) |
| 40-45 years of age n(%) | 125 (88.7) | 16 (11.3) |
| 46-51 years of age n(%) | 129 (97.0) | 4 (3.0) |
| 52-57 years of age n(%) | 112 (95.7) | 5 (4.3) |
| 58-63 years of age n(%) | 66 (100.0) | 0 (0.0) |
| 64-69 years of age n(%) | 30 (96.8) | 1 (3.2) |
| Type of delivery | ||
| No delivery n(%) | 22 (100.0) | 0 (0.0) |
| Vaginal n(%) | 635 (95.6) | 29 (4.4) |
| Caesarean n(%) | 174 (100.0) | 0 (0.0) |
| Number of children | ||
| No children n(%) | 22 (100.0) | 0 (0.0) |
| Up to twon(%) | 251 (98.8) | 3 (1.2) |
| More than two n(%) | 558 (95.5) | 26 (4.5) |
| Women without children | ||
| No n(%) | 815 (96.5) | 29 (3.4) |
| Yes n(%) | 16 (100.0) | 0 (0.0) |
| Sexual intercourse before the age of 18 | ||
| No n(%) | 768 (98.2) | 14 (1.8) |
| Yes n(%) | 63 (80.8) | 15 (19.2) |
| Oral contraception | ||
| No n(%) | 794 (97.5) | 20 (2.5) |
| Yes n(%) | 37 (80.4) | 9 (19.6) |
| Intrauterine device | ||
| No n(%) | 753 (96.7) | 26 (3.3) |
| Yes n(%) | 78 (96.3) | 3 (3.7) |
| Smoking | ||
| No n(%) | 630 (98.1) | 12 (1.9) |
| Yes n(%) | 201 (92.2) | 17 (7.8) |
| Colposcopy | ||
| Not done | 831 (99.9) | 1 (0.1) |
| Satisfactory | 0 (0.0) | 10 (100.0) |
| Low-grade | 0 (0.0) | 18 (100.0) |
| Grade of vaginal cleanliness | ||
| Group I | 1 (100.0) | 0 (0.0) |
| Group II | 656 (98.8) | 8 (1.2) |
| Group III | 174 (89.7) | 20 (10.3) |
| Group IV | 0 (0.0) | 1 (100.0) |
The incidence of PAP III results was statistically significantly higher in the 40-45 age group compared to other age groups (p<0.001) (Table 2).
PAP II results were statistically significantly more frequent in subjects who did not have sexual intercourse before the age of 18 (p<0.001). The incidence of PAP III results was statistically significantly higher in subjects who had sexual intercouse before the age of 18 (p<0.001). PAP II results were statistically significantly more frequent in subjects that did not use intraoral contraceptives (p<0.001). The incidence of PAP III results was statistically significantly more frequent in subjects who used oral contraceptives (p <0.001). PAP II results were statistically significantly more frequent in non-smoker subjects (p <0.001). PAP II results were statistically significantly more frequent in subjects with grade II vaginal cleanliness compared to subjects with grade III vaginal cleanliness (p <0.001). PAP III results were statistically significantly more frequent in subjects with grade III vaginal cleanliness compared to subjects with grade II vaginal cleanliness (p < 0.001), which again confirms the significance, or rather the role the infection plays in the development of cervical cancer.
The incidence of PAP III results were statistically significantly different with respect to the consumption of cigarettes (p <0.001). PAP II findings are statistically significantly more frequent in subjects with grade II vaginal cleanliness compared to subjects with grade III vaginal cleanliness (p <0.001). Two thirds of the purposfully targeted subjects with positive PAP III results had low-grade colposcopy findings, while the findings were satisfactory in 34.5% of the subjects. (Figure 1). The incidence of abnormalities that were confirmed in low-grade colposcopy findings is shown in Figure 2, with two abnormalities confirmed in some of the subjects.
Figure 1. The distribution of colposcopic findings in subjects with Pap III results.
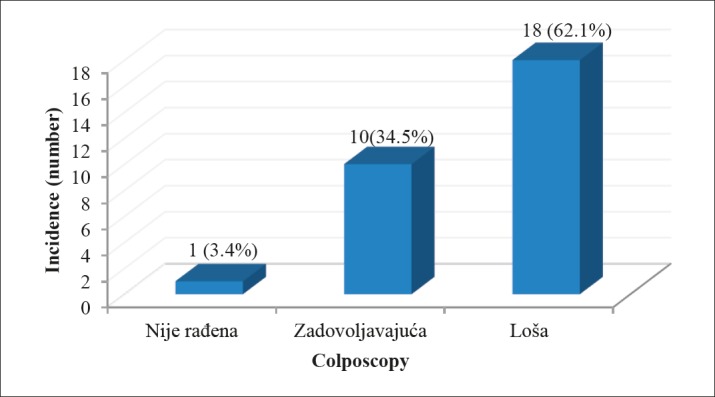
Figure 2. The distribution of low-grade colposcopic findings in subjects with Pap III results.
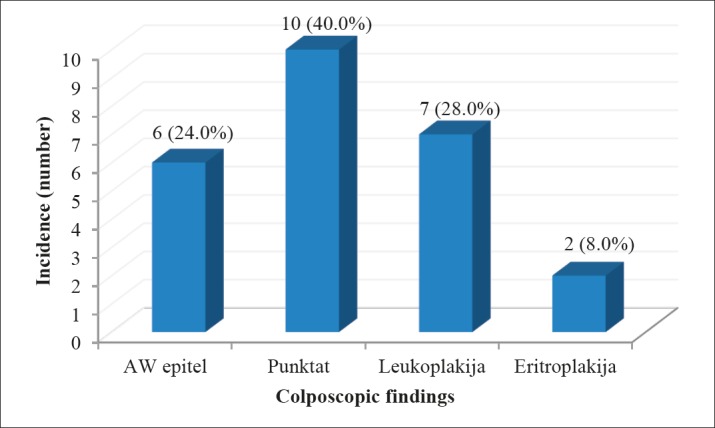
The most frequent colposcopic abnormalities were punctate lesions (40%), followed by leukoplakia lesions (28%) and AW epithelium (24%). Erythroplakia lesions made up 8% of all colposcopic abnormalities. Biopsy was performed on 25 targeted subjects with positive Class 3 Pap smear results. Histopathological analysis (Hp) was performed in 28 subjects, of which 25 (89.3%) with cervicitis chronica and 3 (10.7%) subjects with a confirmed carcinoma in situ.
Microbiological analysis of cervical smear was also performed only in patients with positive PAP III results. Half of the subjects had a heterogeneous group of bacteria, none of which was dominant, while heterogeneous flora with no dominance but with a lot of leukocytes was present in 21% of women. 14% tested positive for Candida albicans while Esherichia Coli was isolated in 11% of subjects. 3.6% of women were diagnosed with Proteus mirabilis.
HPV typing was performed in 25 subjects, all with positive PAP III results, and 3 (12%) of those subjects tested positive.
5. DISCUSSION
It has been determined that HPV infection is the most powerful epidemic factor. This virus is needed, but not sufficient for the development of cervical cancer.
The difference in the incidence of PAP results in subjects who did not have sexual intercourse before the age of 18 points to a high incidence of PAP II results in all age groups (over 92%), while PAP III results were present only in the 45-50 age group, with the incidence of 7.7%. 60% of the subjects who had sexual intercourse before the age of 18 tested positive for PAP III, while the highest statistically significant incidence of 50% was recorded in the 45-60 age group compared to other groups (chi-square = 9,195, <0.01).
A different study investigated the relationship between cervical cancer and the time of first sexual intercourse using the data on monogamous women from the International Collaboration of Epidemiological Studies on Cervical Cancer. The odds ratio for invasive cervical cancer is approximately proportional to the square of the time of the first sexual intercourse (7).
Literature data on the use of oral contraceptives are contradictory. The use of oral contraceptives for more than five years has been associated with an increased risk of cervical cancer, but this risk has disappeared after the adjustment to HPV, smoking and age. Since it is postulated that oral contraceptives act via influencing the folate status (Butterworth et al, 1982; Harper et al, 1994), the possibility of an interaction between the oral contraceptives and the folate status was studied and it was determined that the risk of CIN III was not associated with the use of oral contraceptives in women with high or low folate intake (7).
Another study found that taking oral contraceptives barely increases the risk of cervical cancer, if at all, because women who use them are more active, less likely to use condoms and more often undergo PAP tests in order to be prescribed a suitable contraceptive by a gynecologist (8, 18).
The role of contraception has been a subject of a huge number of multicenter studies (9). The role of contraception remains controversial, but an increased incidence of unusual histological types in women with a long-term use of contraceptives has been observed (10), which is in accordance with our research results.
Tobacco smoking and the development of cervical cancer are positively related. The reason may be found in the direct mutagenic effect of decomposed products of tobacco smoking (cocaine, nicotine), making the risk 2-4 times higher in women who smoke. Women who smoke 15 and more cigarettes a day are at a 2 times higher risk of HPV infection than non-smokers, the incidence higher in women aged between 45 and 50 and at about 37% in women under 35. Women older than 65 make up 10% of patients (7, 14, 15).
The highest mortality rate was detected in the group of women over 65 years of age due to the advanced stage of the disease at the time the diagnosis was made, where 50% of subjects smoked tobacco and 50% were non-smokers (11).
In subjects who were smokers the incidence of PAP II results was high in all age groups (over 83%), almost 15% higher than in non-smokers of all age groups, while PAP III results had the highest frequency of 16.7% in the 45-60 age group, (12) which coincides with our results.
A study conducted at the WHO Collaborative Center at Uppsala University determined that tobacco smoking, alcohol consumption and the use of narcotics were risk factors, but not causative agents. HPV was detected in 66 (6.8%) of 972 women who were admitted for counseling.
Among women with confirmed HPV infection, 33 (50%) were smokers, while there were 307 (33.9%) smokers in the group of HPV negative women (13, 16).
Plummer et al. published a multicenter study in 2003. By analyzing 8 invasive cancer studies and 2 carcinoma in situ studies, the authors concluded that consistent smokers had an increased risk of cervical cancer and added that planocellular cervical cancer should be added to the list of nicotine-related carcinomas, while additional data would be needed to reach the same conclusion for adenocarcinoma (20).
Studies of the relationship between bacterial-viral infections and PAP results conducted so far showed the incidence of infection of 15% for PAP I positive subjects and 33% for PAP III positive subjects. The study showed that the incidence of bacterial vaginosis was statistically significantly higher in patients with precancerous lesions on the cervix or with cervical cancer than in healthy women (14, 19).
6. CONCLUSION
The results obtained by examining individual risk factors for the disease and premalignant cervical lesions lead to the conclusion that, according to all investigated factors, cervical cancer is most frequent in the 35-50 age group, which does not deviate significantly from the results in other countries in the region. In Serbia, the incidence of the onset of the disease is highest in the 48-52 age group, while in the rest of Europe it is in the 25-44 age group (among the European countries, the lowest incidence was detected in Scandinavia) (17).
Tobacco smoking, the use of contraceptives, and the number of births are factors that showed no statistically significant deviations in the studied population compared to other countries in the region, as well as European countries. They have an equal statistical significance in all age groups, as can be seen from the discussion. There was a close association between subjects with bacterial-viral infections and the incidence of PAP abnormalities that were followed by low-grade colposcopy findings in the subjects, especially PAP III in the subjects over the age of 40. In the studied population, PAP III results were statistically significant in patients between the ages of 40 and 45, while the European study showed the incidence of PAP III results of above 33%, but in a slightly younger population (under 30 years of age) with untreated infections.
The National Program for Cervical Cancer Prevention in Montenegro did not make adequate progress in the early diagnosis of cervical cancer, which is reflected in an increase in the number of patients, so it is our recommendation to take adequate measures and activities for the proper implementation of the program.
Authors contribution:
All authors are included in all pahases of preparation of this article. Final proof reading was made by the first author.
Conflict of interests:
none declared.
REFERENCES
- 1.Ministarstvo zdravlja Crne Gore. Nacionalni program ranog otkrivanja raka grlića materice. 2011. pp. 3–4.
- 2.Vukićević D, Mitić R, Mijović M, Mitić N, Vitković L, Đerković B, Nedeljković V. Deskriptivno-epidemiološke karakteristike karcinoma grlića materica. str. 68.
- 3.Colaković B, Colaković-Popović V. Incidence of cervical cancer in Montenegro. Clin Exp Obstet Gynecol. 2008;35(4):275–278. [PubMed] [Google Scholar]
- 4.Beograd: 2013. Incidencija i mortalitet od raka u centralnoj Srbiji 2011. Institut za javno zdravlje Srbije „Dr Milan Jovanović Batut”. [Google Scholar]
- 5.Arbyn M, Anttila A, Jordan J, Ronco G, Schenck U, Segnan N, Wiener A, Herbert A, von Karsa L. 2nd. Brussels, Luxembourg: European Community, Office for Official Publicationas of the European Communities; 2008. European guidelines for quality assurance in cervical cancer screening. [Google Scholar]
- 6.Sasieni P, Castanon A, Parkin DM. How many cervical cancers are prevented by treatment of screen-detected disease in young women? (link is external) Int J Cancer. 2009;124(2):461–464. doi: 10.1002/ijc.23922. [DOI] [PubMed] [Google Scholar]
- 7.Kjellberg L, Hallmans G, Åhren AM, Johansson R, Bergman F, Wadell G, Ångström T, Dillner J. Smoking, diet, pregnancy and oral contraceptive use as risk factors for cervical intra-epithelial neoplasia in relation to human papillomavirus infection. British Journal of Cancer. 2000;82(7):1332–1338. doi: 10.1054/bjoc.1999.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gierisch JM, Coeytaux RR, Urrutia RP, et al. Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: a systematic review Cancer Epidemiol Biomarkers Prev. 2013;22(11):1931–1943. doi: 10.1158/1055-9965.EPI-13-0298. [DOI] [PubMed] [Google Scholar]
- 9.La Vecchia C, Boccia S. Oral contraceptives, human papillomavirus and cervical cancer (link is external) Eur J Cancer Prev. 2014;23(2):110–112. doi: 10.1097/CEJ.0000000000000000. [DOI] [PubMed] [Google Scholar]
- 10.Centre for Cancer Prevention et al. Cancers attributable to exposure to hormones in the UK in 2010 (link is external) Br J Cancer. 2011;105(Suppl 2):S42–48. doi: 10.1038/bjc.2011.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeng XT, Xiong PA, Wang F, Li CY, Yao J, Guo Y. Passive smoking and cervical cancer ris; a meta-analysis based on 3,230 cases and 2,982 controls. Asian Pac J Cancer Prev. 2012;13(6):2687–2693. doi: 10.7314/apjcp.2012.13.6.2687. [DOI] [PubMed] [Google Scholar]
- 12.Vacarela S, Herrero R, Snijders PJ, et al. Smoking and human papillomavirus infection: pooled analysis of the International Agency for Research on Cancer HPV Prevalence Surveys (link is external) Int J Epidemiol. 2008;37(3):536–546. doi: 10.1093/ije/dyn033. [DOI] [PubMed] [Google Scholar]
- 13.Anderson L, O’Rorke M, Jamison J, Wilson R, Gavin A. HPV Working Group members Prevalence of human papillomavirus in women attending cervical screening in the UK and Ireland: new data from nothern Ireland and a systematic review and metaanalysis (link is external) J Med Virol. 2013;85(2):295–308. doi: 10.1002/jmv.23459. [DOI] [PubMed] [Google Scholar]
- 14.Jensen KE, Thomsen LT, Schmiedel S, et al. Chlamydia trachomatis and risk of cervical intraepithelial neoplasia grade 3 or worse in women with persistent human papillomavirus infection: a cohort study (link is external) Sex Transm Infect. 2014. [DOI] [PubMed]
- 15. https://www.cancer.org/cancer/cervical-cancer/causes-risks-prevention/risk-factors.html.
- 16.Sherris J, Herdman C, Elias C. Cervical cancer in the developing world. West J Med. 2001 Oct;175(4):231–233. doi: 10.1136/ewjm.175.4.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vaccarella S, Franceschi S, Engholm G, Lönnberg S, Khan S, Bray F. 50 years of screening in the Nordic countries: quantifying the effects on cervical cancer incidence. Br J Cancer. 2014 Aug 26;111(5):965–969. doi: 10.1038/bjc.2014.362. Epub 2014 Jul 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vaccarella S, Lortet-Tieulent J, Plummer M, Franceschi S, Bray F. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013 Oct;49(15):3262–3273. doi: 10.1016/j.ejca.2013.04.024. Epub 2013 Jun 8. [DOI] [PubMed] [Google Scholar]