Abstract
Background:
Students’ opinions about their medical curriculum is essential process for evaluating program strength and weakness. Aim: We aimed to assess the benefits and effectiveness of PBL in acquisition of knowledge and soft skills during basic (Phase I) and preclinical (Phase II) sciences.
Methods:
Across-sectional study was conducted at the University of Bisha, College of Medicine, Saudi Arabia. Students at Phase I and Phase II were involved. A validated self-administered questionnaire used for data collection. Responses to the questionnaire items regarding PBL benefits, preferences and effectiveness in acquisition of knowledge and soft skills were ordinal following a four-point Likert scale format. Independent and paired t tests were used to compare between the means and SD of each two variables. A p value ≤ 0.05 considered as statistically significant.
Results:
Most of students (86.3%) reported a positive perception on all the items assessing the benefits of PBL approach. Students’ responses on PBL relating to the acquisition of knowledge (3.27±0.46) and soft skill (3.32±0.45) were high. There were no significant differences determined in the mean score and SD of acquisition of knowledge (p=0.768) and soft skills (p=0.297) between second and third year students. PBL was preferred in Phase II comparable to Phase I modules (3.371±0.299 vs. 3.026±0.627; p=0.001).
Conclusion:
Effectiveness of PBL found to be high and increasing after taking a series of modules. Although PBL methodology has impact in acquisition of knowledge and skills, intended program outcome should be determined to assess the effects of PBL.
Keywords: Problem-Based Learning, methods, statistics and numerical data
1. INTRODUCTION
The number of medical schools implementing problem based learning approach has grown progressively all around the globe with many forms and strategies (1). The major educational objectives of PBL include the acquisition of relevant knowledge, skills, and behaviors rather than factual learning and use them in a clinical context (2, 3). Works through PBL strategy motivate students to think critically, generate ideas and acquire the knowledge, skills, and behavior required to become competent doctors (4, 5).
The University of Bisha, College of Medicine (UBCOM) established in 2014 with the rationale to participate in the development of health status in the Saudi Arabia. UBCOM select hybrid PBL curriculum that almost adopted by many medical school in Saudi Arabia to integrate the learning of basic sciences and clinical disciplines (6). A six-year PBL curriculum is offered in UBCOM to the undergraduate medical students. This integrated curriculum composed of second year of basic sciences (Phase I), third and fourth years of preclinical phase (Phase II) and a clerkship in year fifth and sixth (Phase III). These are proceeding by the first year. UBCOM has recently introduced the problem PBL curriculum during Phase I and II.
Medical students are a core part to take into account for planning and assessing the value of teaching and learning methods (7). It well known that evaluation the effects of PBL approach is necessary to introduce into the medical curriculum completely (8). Numerous studies have been conducted to assess the PBL concerning acquiring knowledge, development of core competencies and attitudes (9, 10). Researches indicated that medical students’ opinions about their curriculum have a substantial impact on their academic success and can be an essential process for evaluating medical program strength and weakness (11). Since UBCOM is a new medical college implementing the PBL approach, it is important to determine the flow and the worth of this method for future improvements. Therefore, the aims of this study were to assess the benefits and effectiveness of PBL in acquisition of knowledge and soft skills during basic medical science and preclinical phases (Phase I and Phase II) from students’ points of view.
2. MATERIALS AND METHODS
Study design and setting
Across-sectional study was conducted during academic year 2016-2017 at the UBCOM in Bisha province, Saudi Arabia. Every academic year, up to 40 students at UBCOM registered for MBBS program.
Phase I modules make up the first cycle of the medical curriculum in UBCOM, which is introducing the basis of medical practice in terms of basic level knowledge of human body structure and function in health and disease. It also gives an overview of the processes of diseases, the therapeutic strategies, and understanding of the ethical and cultural dimensions of contemporary medical care. Phase II helps students integrate the knowledge they have acquired during Phase I and prepare them for the subsequent Phase III. Eight modules of body organs/systems and other six modules for covering certain areas in the curriculum are introduced in Phase II.
Study subjects
The study subjects consisted of two groups of medical students. The first group was the students of the second year and were successfully completed eight modules of Phase I. This including, introduction to medicine and medical education, molecular biology and genetics, structure and function of the human body, basic biochemistry man and his environment, growth and development, behavioral science and doctoring and principle of diseases. The second group was comprised of the third-year students those were completed Phase I courses and seven modules of Phase II, including hematology, immunology, musculoskeletal system, nutrition and metabolism, gastrointestinal system, respiratory system and cardiovascular system.
Instrument and collection of data
A self-administered questionnaire was developed and used as a tool to measure specific items that met student’s perception and satisfaction on PBL as an instructional method as described in the literature (11, 12). It consisted of three parts; the first part comprised of 16 items dealing with the student’s perception of PBL session’s benefits during Phase I and Phase II. The second part is consisting of 12 items to evaluate students’ satisfaction regarding knowledge and soft skill. While the third part consisted of 15 items related students’ preferences of PBL among Phase I and II modules.
The questionnaire forms were distributed among the students at the end of the academic year of 2016-2017 and were asked to return the completed questionnaire within three days. The students have been invited to indicate agreement on a four-point Likert scale to increase the chance of obtaining either a positive or negative perception of the activity. This arranged as strongly agree (4), agree (3), disagree (2) and strongly disagree (1). The higher score, the more likely the students considered PBL approach is effective. The questionnaire items have been tested for its reliability and validity and to be sure the questions were measuring the same underlying concept prior the study.
Statistical analysis
Data entry and analysis was performed using Statistical Package for Social Science (SPSS; version 16). The frequency response of the Likert scores was calculated, the relative frequency of scores 4-3, represent a positive agreement and 2-1 scores represent disagreement with question statement. Outcome data of students’ perception about PBL approach in term of acquisition of knowledge, learning process and soft skills were tabulated in the form of proportions; mean scores ± standard deviations (SD). The independent t-test was applied to compare between second and third-year students’ perception about the benefits and effectiveness of PBL. Comparison students’ preference of PBL during Phase I and II modules was determined using paired t test. All p values ≤ 0.05 were considered as statistically significant
Ethical approval
Ethical approval was obtained the research committee at UBCOM. Informed consent had been taken verbally from all the students before data collection. The privacy and confidentiality of the data were considered as the data were collected and manipulated anonymously.
3. RESULTS
Instrument reliability and validity
The Internal consistency (Cronbach’s alpha) for the three parts of questionnaire response was; 0.880 for students’ perception about PBL sessions benefits; 0.853 for acquisition of knowledge and soft skills and 0.830 for students’ preferences in Phase I and II modules. Each item of the questionnaire was checked and found to have high scores.
Characterization of the study subjects
A total of 70 medical students at Phases I and II (second and third years) in UBCOM recruited for the study. Among them, 67 (95.7%) were returned a completed questionnaire. Of these 67 students, 39 were from the second year and 28 from the third year. The age of the students in both groups ranges between 19 to 23 years old. All of the students are Saudi nationality.
Table 1 demonstrates students’ responses about their perceptions on the benefits of PBL approach. Overall, the majority of the students had positive perceptions of all items; the mean value of all the elements was 86.3%, with the maximum of 92.5%. As shown in Table 1, 92.5% agreed and strongly agreed that PBL promoted their curiosity, acquisition of attitude and developed their interpersonal relationship. Moreover, 89.6% perceived that PBL stimulates them to learn basic sciences contents, and promote their teamwork skills, 88.1% felt that PBL developed their independent thinking.
Table 1. Students’ perception about PBL benefits at the College of Medicine, University of Bisha, Saudi Arabia.
| Statement | No. (%) of positive response 4 and/or 3 Likert scale | Mean ± SD of student response |
|---|---|---|
| Stimulating to learn basic science contents | 60 (89.6) | 3.313 ± 0.656 |
| Gathering of knowledge and information | 57 (85.1) | 3.254 ± 0.704 |
| Understanding general principle | 58 (86.6) | 3.164 ± 0.687 |
| Improving learning ability | 57 (85.1) | 3.105 ± 0.631 |
| Increasing personal satisfaction and enjoyment | 58 (86.6) | 3.224 ± 0.755 |
| Promoting level of motivation | 56 (83.6) | 3.134 ± 0.672 |
| Stimulating interest in the subject | 56 (83.6) | 3.179 ± 0.737 |
| Developing interpersonal relationship | 62 (92.5) | 3.343 ± 0.617 |
| Enhancing teamwork and working in small groups behavior | 60 (89.6) | 3.358 ± 0.753 |
| Developing of students and tutor interaction | 56 (83.6) | 3.328 ± 0.786 |
| Improvement of reasoning | 55 (82.1) | 3.209 ± 0.729 |
| Increasing curiosity and acquisition of attitude | 62 (92.5) | 3.254 ± 0.586 |
| Development independent of thinking | 59 (88.1) | 3.358 ± 0.690 |
| Preparation for clinical thinking | 55 (82.1) | 3.179 ± 0.796 |
| Learn different material resources | 54 (80.6) | 3.105 ± 0.819 |
| Overall value | 60 (89.6) | 3.254 ± 0.786 |
| Mean | 58 (86.3) | 3.253±0.682 |
| Maximum | 62 (92.5) | 4.0 |
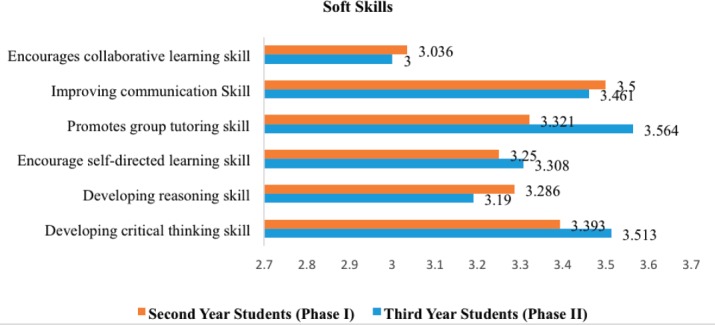
Table 2 demonstrates the students mean scores and SD about the effectiveness of PBL in acquisition of knowledge and soft skills. The overall students’ responses on PBL process relating to the acquisition of knowledge (3.27 ± 0.46) and soft skill (3.32 ± 0.45) were positive. There were no significant differences determined in s mean scores of knowledge (p=0.768) and soft skills (p=0.297) between second and third year students (Table 2).
Table 2. Effectiveness of PBL approach on acquisition of knowledge and soft skills during Phase I and Phase II from medical students’ points of view.
| Statement | Students perception score 1-4 Likert scale (Means ± SD) | Mean differences | 95% Confidence Interval of the Difference | P value | ||
|---|---|---|---|---|---|---|
| Overall students in Phase 1 and II | Year 2 students (Phase I) | Year 3 students (Phase II) | ||||
| Knowledge and learning process | ||||||
| Fulfil educational objectives of the subject | 3.19 ± 0.58 | 3.179±0.670 | 3.205 ± 0.522 | 0.027 | -0.264–0.317 | 0.175 |
| Understanding content knowledge of the subject | 3.25 ± 0.63 | 3.179±0.612 | 3.308 ± 0.655 | 0.129 | -0.186–0.444 | 0.250 |
| Encouraging to learn in context | 3.20 ± 0.73 | 3.250±0.752 | 3.179 ± 0.720 | -0.071 | -0.433–0.292 | 0.366 |
| Enhancing retention of knowledge | 3.27 ± 0.69 | 3.250±0.799 | 3.282 ± 0.605 | 0.032 | -0.310–0.374 | 0.177 |
| Participation in learning process | 3.44 ± 0.63 | 3.357±0.488 | 3.512 ± 0.683 | 0.156 | -0.146–0.457 | 0.110 |
| Making the topic more interesting and fun learning | 3.25 ± 0.80 | 3.214±0.787 | 3.282 ± 0.825 | 0.068 | -0.333–0.468 | 0.797 |
| Overall mean score | 3.27 ± 0.46 | 3.200 ± 0.400 | 3.300 ± 0.500 | - | - | 0.768 |
| Development of soft skills Developing of higher thinking skill of the subject | 3.46 ± 0.68 | 3.393±0.629 | 3.513 ± 0.721 | 0.120 | -0.218–0.458 | 0.434 |
| Promoting of reasoning skill of the subject | 3.22 ± 0.62 | 3.286±0.600 | 3.190 ± 0.644 | -0.106 | -0.416–0.203 | 0.952 |
| Simulating of self-directed learning on the subject | 3.28 ± 0.75 | 3.250±0.701 | 3.308 ± 0.800 | 0.058 | -0.318–0.434 | 0.385 |
| Promoting of problem solving skills | 3.46 ± 0.61 | 3.321±0.612 | 3.564 ± 0.598 | 0.243 | -0.056–0.541 | 0.960 |
| Developing of communication skill | 3.48 ± 0.59 | 3.500±0.509 | 3.461 ± 0.643 | -0.038 | -0.331–0.254 | 0.110 |
| Encouraging collaboration in small groups | 3.15 ± 0.74 | 3.036±1.036 | 3.000 ± 0.688 | -0.036 | -0.630–0.132 | 0.047 |
| Overall mean score | 3.32 ± 0.45 | 3.300 ± 0.400 | 3.300 ± 0.500 | - | - | 0.297 |
Students’ responses to the items assessing knowledge and soft skills
The students mean scores of each item regarding knowledge and soft skill during PBL sessions are represented in Table 2, Figures 1 and 2. Students in each group rated high scores for all the items under investigation. There were no significant differences in students’ responses to the most items when comparing the mean score of the second and third year’s students. However, there is a significant difference of students’ response to collaborative learning. Second year students perceived that PBL is encouraging collaborative learning comparable to the third-year students (3.036±1.036 vs. 3.000 ± 0.688; p=0.047).
Figure 1. Comparison between second and third year students’ responses (presented as mean scores) to the several items assessing the acquisition of knowledge and learning process during PBL sessions.
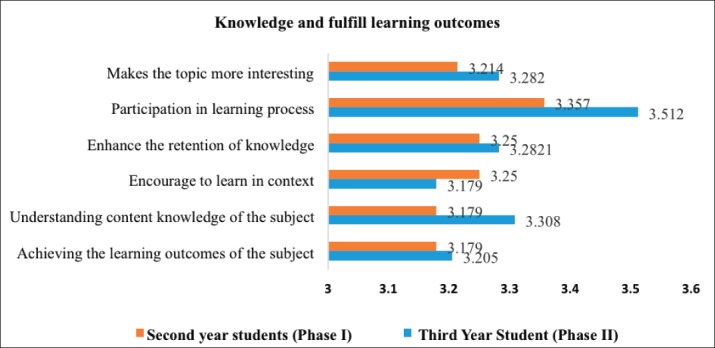
Figure 2. Comparison between second and third year students’ responses (presented as mean scores) to the several items assessing development of soft skills during PBL sessions.
Students preferences of PBL during Phase I and II modules
The total mean score of students (third-year students) preferences of PBL during Phase I modules was compared to their preference in subsequent Phase II (Table 3). PBL most likely to be preferred in Phase II modules comparable to Phase I modules (3.371 ± 0.299 vs. 3.026 ± 0.627; p=0.001).
Table 3. Comparisons of third year students’ preferences of PBL approach during Phase I and II modules.
| Third year students’ preferences | Means ± STD | 95% Confidence Interval of the Difference | P value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Phase I modules | 3.0256 ± 0.627 | -.54662 | -.14349 | 0.001 |
| Phase II modules | 3.370 ± 0.299 | |||
4. DISCUSSIONS
The present study investigated the perception second and third-year students about the PBL approach for teaching basic science and preclinical phases at the UBCOM. In this study, the Cronbach’s alphas for all the instruments items of students’ perception about the PBL were all above 0.80; hence, the questionnaire proved to be a reliable tool for this study. However, the obtained values indicate strong reliability and the questions were measuring the same underlying concepts.
In the present study, the majority (86%) of our medical students were perceived PBL to be an acceptable learning strategy. This in agreement with recent studies published on the acceptance PBL in Saudi’s medical schools (13, 14). Elsewhere a study indicated that medical students valued and expressed a more positive outlook and satisfaction toward the PBL approach (15, 16). These findings with our current results give a strong evidence of the interesting perception of PBL in medical schools from the students’ points of view.
In the present study, 89.6% of students’ felt that PBL stimulate the learning of basic sciences contents. This encouraging rates could be compared with another report from Saudi Arabia, where 84.8% of medical students indicated that the PBL sessions were helpful in understanding basic science concepts (11). Even though there is a consensus that PBL results in the better acquisition of core and preclinical concepts (11, 14), other authors argued that PBL did not impact knowledge acquisition, but impacts the application of knowledge (17). For instance, Nanda and Manjunatha, mentioned that the amount of basic science knowledge that is sufficient to equip an undergraduate to successfully and confidently function as a medical practitioner is difficult to determine (12). Likewise, in earlier a study carried out among medical graduates of McMaster University, found that basic medical sciences are requiring more attention in the curriculum (18).
Students’ opinion about PBL benefits
In this study, students were more attractive in PBL approach, felt motivated and stimulated their attention in the learning of the subject matter. It’s well known that PBL creates a different teaching environment by making learning fun, motivated, enjoyable, and getting students out of the boring routine in the classroom (19). Researchers reported that the PBL sessions promote and enhance students’ knowledge, enthusiasm, and motivation and enjoyable learning medicine (3, 11, 20). According to Khoshnevisas et al. students preferred PBL because of motivation boost, quality learning, knowledge retention, class attractiveness, and practical usefulness of contents (10).
Interactions and collaboration within the small group provide students with opportunities to ask questions, receive clarifications that lead to a deeper understanding of the subject matter (21). A significant number of students in this a study agreed that PBL has beneficial in the development of teamwork skills and interpersonal relationships. This goes with numerous studies reported that the PBL was improving teamwork interpersonal skills, interaction and collaboration in small-group tutorials (11, 20, 22). In the present study, the students perceived PBL encourages them in developing curiosity, reasoning, and independent thinking. This character is significant for efficient patient care in daily practice (19). Our finding in agreement with several studies found that PBL has the potential to enhance the effectiveness of teaching and learning, particularly in developing independent thinking, curiosity and improves student interactions among each other as well as the tutor (12, 22, 23). Studies assumed that the ability of tutors to communicate informally and examining students thinking is crucial in PBL and keeping process moving (12, 24). Therefore, the training of our PBL tutors for mastering essentials PBL process, skills and attitudes may be required to deal with the PBL method.
Effectiveness of PBL in acquisition of knowledge and soft skills
Our medical students found to have positive perceptions toward implementing of PBL in the acquisition of knowledge and in the learning process (3.27 ± 0.46). Recent studies in Saudi Arabia students felt the PBL was improving the learning outcome domains, enhancing of learning abilities (8, 11). Consistent with these findings, elsewhere a study found that most of the students felt that PBL sessions were beneficial in achieving their learning objectives and allowed an in-depth understanding of the topic of learning (25). In contrary, Hartling et al. suggested that PBL does not impact knowledge acquisition; evidence for other outcomes does not provide unequivocal support for enhanced learning. Work is needed to determine the most appropriate outcome measures to capture and quantify the effects of PBL (17).
Obviously, PBL shown to develop different kinds of soft skills needed for their future clinical practice (Table 2). These findings supported by other studies. For example, Ibrahim et al. suggested that PBL provides students with better critical thinking, reasoning, team building, communication, self-directed learning, and summarization skills than do traditional lectures (8). According to Surif et al. PBL could enhance soft skills particularly, on students’ motivation, communication skills, collaboration and independent learning (23). Hmelo-Silver et al. also emphasized the importance of communication skills in aiding group members “negotiate shared meaning” of information, related to the problem at hand (24).
Our finding is consistent with different studies that suggested PBL is effective in fostering students’ development of higher-order thinking, appropriate problem-solving processes and skills (26, 11, 23, 27-39). Furthermore, previous a study indicated that PBL graduates rated themselves better prepared professionally than other non-PBL graduates regarding interpersonal abilities, problem-solving skills and the ability to work and plan efficiently and autonomously (2). In contrary, studies found that PBL requires much time that must be provided to solve complex problems, which lead to a lack of time available for the material/content (16, 28).
In this study significant increase in PBL students’ perception concerning simulating of self-directed learning on the subject. In a previous survey, Tsou et al. stated that students in their study claimed that they were more active in learning and had better learning skills and confidence in self-directed learning as compared with students from the lecture-based curriculum (29).
Comparison of students’ mean scores regarding knowledge and soft skills
PBL found to be effective in acquisition of knowledge and soft skills among second and third-year students. However, almost most of the third-year students rated relatively higher scores for the majority of the investigated items. The possible explanation for that could be due to the third-year students have become more experienced with PBL process and long experience of a student-centered educational context. In a study conducted in interdisciplinary biotechnology courses Steck et al. (2012) found that the students’ mean report of their content knowledge improved after taking this series of courses, but problem-solving strategies and critical-thinking skills did not statistically improve. These are in disagreement with a recent a study found that PBL did not show the expected increase depth in learning approaches over the program years (31).
5. CONCLUSION
PBL was a useful educational methodology and had several learning benefits from students’ points of view. Effectiveness of PBL found to be increased according to students’ experience and after taking a series of modules. Although PBL methodology has impact in acquisition of knowledge and soft skills, intended program should be determined to capture and evaluate the effects of PBL. PBL being active in soft skills improvement, therefore, the training of tutors for mastering essentials process, skills and attitudes may be required to deal with this method effectively.
Acknowledgments:
The authors express their gratitude for medical students those are participated in this a study.
Conflict of Interest:
The authors declare that they have no conflict of interest.
Authors’ contribution:
Mutasim E Ibrahim: conceived and designed the study, conducted research, collected and analyzed data and wrote initial draft of manuscript. Abdullah M AlShahrani: conducted research, collected and analyzed data. Mohamed E Abdalla, Inshirah M Abubaker and Mohamed E Mohamed: revised the manuscript for important intellectual content and approved the final version submitted. All authors have approved the final draft and are responsible for the content and similarity index of the manuscript.
REFERENCES
- 1.Karimi R. Interface between problem-based learning and a learner-centered paradigm. Adv Med Educ Pract. 2011;2:117–125. doi: 10.2147/AMEP.S12794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beachey WD. A comparison of problem-based learning and traditional curricula in baccalaureate respiratory therapy education. Respir Care. 2007;52(11):1497–1506. [PubMed] [Google Scholar]
- 3.Gerzina TM, Worthington R, Byrne S, McMahon C. Student use and perceptions of different learning aids in a problem-based learning (PBL) dentistry course. J Dent Educ. 2003;67(6):641–653. [PubMed] [Google Scholar]
- 4.Choi E, Lindquist R, Song Y. Effects of problem-based learning vs. traditional lecture on Korean nursing students’ critical thinking, problem-solving, and self-directed learning. Nurse Educ Today. 2014 Jan;34(1):52–56. doi: 10.1016/j.nedt.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Zahid MA, Varghese R, Mohammed AM, Ayed AK. Comparison of the problem based learning-driven with the traditional didactic-lecture-based curricula. Int J Med Educ. 2016;7:181–187. doi: 10.5116/ijme.5749.80f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khalid BAA. The current status of medical education in the Gulf Cooperation Council countries. Ann Saudi Med. 2008;28(2):83–88. doi: 10.5144/0256-4947.2008.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Imanieh MH, Dehghani SM, Sobhani AR, Haghighat M. Evaluation of problem-based learning in medical students’ education. J Adv Med Educ Prof. 2013;2(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 8.Ibrahim NK, Banjar S, Al-Ghamdi A, Al-Darmasi M, Khoja A, Turkistani J, et al. Medical students’ preference of problem-based learning or traditional lectures in King Abdulaziz University, Jeddah, Saudi Arabia. Ann Saudi Med. 2014;34(2):128–133. doi: 10.5144/0256-4947.2014.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alessio H. Student perceptions about and performance in problem-based learning. J Scholarsh Teach Learn. 2004;4:23–34. [Google Scholar]
- 10.Khoshnevisasl P, Sadeghzadeh M, Mazloomzadeh S, Hashemi Feshareki R, Ahmadiafshar A. Comparison of Problem-based Learning With Lecture-based Learning. Iran Red Crescent Med J. 2014;16(5) doi: 10.5812/ircmj.5186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Drees AA, Khalil MS, Irshad M, Abdulghani HM. Students’ perception towards the problem based learning tutorial session in a system-based hybrid curriculum. Saudi Med J. 2015;36(3):341–348. doi: 10.15537/smj.2015.3.10216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Masic I, Pandza H. Medical Informatics Education - Past, Today and Future. European Journal for Biomedical Informatics. 2018;14(2):40–45. [Google Scholar]
- 13.Hagi SK, Al-shawwa LA. Medical Students ’ Perception and Acceptance of the. Saudi Med J. 2011;32(10):1060–1065. [PubMed] [Google Scholar]
- 14.AlHaqwi a I, Mohamed T a, Al Kabba a F, Alotaibi SS, Al Shehria M, Abdulghani HM, et al. Problem-based learning in undergraduate medical education in Saudi Arabia: Time has come to reflect on the experience. Med Teach. 2015;37(February 2016):S61–6. doi: 10.3109/0142159X.2015.1006608. [DOI] [PubMed] [Google Scholar]
- 15.Lian J, He F. Improved performance of students instructed in a hybrid PBL format. Biochem Mol Biol Educ. 2013;41(1):5–10. doi: 10.1002/bmb.20666. [DOI] [PubMed] [Google Scholar]
- 16.Joseph N, Sharada R, Animesh J, Nelliyanil M, Kotian SM, Rai S, et al. Perception towards problem based learning among medical students of a private medical college in South India. Br J Med Med Res. 2015;9(5) BJMMR.19200-BJMMR.19200. [Google Scholar]
- 17.Hartling L, Spooner C, Tjosvold L, Oswald A. Problem-based learning in pre-clinical medical education: 22 years of outcome research. Med Teach. 2010 Jan;32(1):28–35. doi: 10.3109/01421590903200789. [DOI] [PubMed] [Google Scholar]
- 18.Woodward CA, Ferrier BM. The content of the medical curriculum at McMaster University: graduates’ evaluation of their preparation for postgraduate training. Med Educ. 1983 Jan;17(1):54–60. doi: 10.1111/j.1365-2923.1983.tb01094.x. [DOI] [PubMed] [Google Scholar]
- 19.Nanda B, Manjunatha S. Indian medical students’ perspectives on problem-based learning experiences in the undergraduate curriculum: One size does not fit all. J Educ Eval Health Prof. 2013;10:11. doi: 10.3352/jeehp.2013.10.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ommar N. Perception of First and Second Year Medical Students on Problem-Based Learning in Universiti Malaysia Sarawak. 2011;14(11):1628–1634. [Google Scholar]
- 21.Shankar PR, Nandy A, Balasubramanium R, Chakravarty S. Small group effectiveness in a Caribbean medical school’s problem-based learning sessions. J Educ Eval Health Prof. 2014;11:5. doi: 10.3352/jeehp.2014.11.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klegeris A, Hurren H. Impact of problem-based learning in a large classroom setting: student perception and problem-solving skills. Adv Physiol Educ. 2011:408–415. doi: 10.1152/advan.00046.2011. [DOI] [PubMed] [Google Scholar]
- 23.Surif J, Ibrahim H, Mokhtar M. Implementation of Problem Based Learning in Higher Education Institutions and Its Impact on Students’ Learning. 4th Int Symp Probl Learn. 2013;2013:66–71. [Google Scholar]
- 24.Hmelo-Silver CE, Barrows HS. Goals and Strategies of a Problem-based Learning Facilitator. Interdiscip J Probl Learn. 2006;1(1):21–39. [Google Scholar]
- 25.Barman A, Jaafar R IN. Problem-Based Learning As Perceived By Dental. Malaysian Journal of Medical Sciences. 2006;13(1):63–67. [PMC free article] [PubMed] [Google Scholar]
- 26.Hung W, Jonassen DH, Liu R. Problem-Based Learning. Handb Res Educ Commun Technol. 2008;3:485–506. [Google Scholar]
- 27.Al-Shaikh G, Al Mussaed EM, Altamimi TN, Elmorshedy H, Syed S, Habib F. Perception of Medical Students Regarding Problem Based Learning. Kuwait Med J. 2015;47(2):133–138. [Google Scholar]
- 28.Emerald NM, Aung PP, Han TZ, Yee KT, Myint MH, Soe TT OS. Students ’ Perception of Problem-based Learning Conducted in Phase1 Medical Program. South East Asian Journal of Medical Education. 2013;7(2):45–48. [Google Scholar]
- 29.Tsou KI, Cho SL, Lin CS, Sy LB, Yang LK, Chou TY, et al. Short-Term Outcomes of A Near-Full PBL Curriculum In A New Taiwan Medical School. Kaohsiung J Med Sci. 2009;25(5):282–293. doi: 10.1016/S1607-551X(09)70075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang C, Boukhtiarov A, DiBiase W, Steck TR. The Use of Open-Ended Problem-Based Learning Scenarios in an Interdisciplinary Biotechnology Class: Evaluation of a Problem-Based Learning Course Across Three Years. J Microbiol Biol Educ. 2012;13(1):2–10. doi: 10.1128/jmbe.v13i1.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Masic I. Quality assessment of medical education at faculty of medicine of Sarajevo University. Med Arh. 2012;66(3, Suppl 1):6–10. [PubMed] [Google Scholar]
- 32.Masic I, Begic E. Efficiency of Implementation of the Bologna Process at Medical Faculty, University of Sarajevo. Mater Sociomed. 2015;27(1):67–70. doi: 10.5455/msm.2015.27.67-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Masic I, Ciric D, Pulja A, Kulasin I, Pandza H. MIE 2009 Proceedings. Sarajevo: 2009. Quality assessment of medical education and use of information technology; pp. 898–902. [PubMed] [Google Scholar]
- 34.Mantas J, Ammenwerth E, Demiris G, Hasman A, Haux R, Hersh W, et al. Recommendations of the International Medical Informatics Association (IMIA) on education in biomedical and health informatics. Methods of Information in Medicine. 2010;49(2):105–20. doi: 10.3414/ME5119. [DOI] [PubMed] [Google Scholar]
- 35.Pandza H, Masic I. Distance learning perspectives. Acta Inform Med. 2010;18(4):229–232. doi: 10.5455/aim.2010.18.229-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masic I. Quality assessment of medical education at faculty of medicine of Sarajevo university - comparison of assessment between students in Bologna process and old system of studying. Acta Inform Med. 2013;21(2):76–82. doi: 10.5455/aim.2013.21.76-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Masic I. E-learning as new method of medical education. Acta Inform Med. 2008;16(2):91–100. doi: 10.5455/aim.2008.16.91.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masic I, Pandza H, Kulasin I, Masic Z, Valjevac S. Tele-education as method of medical education. Med Arh. 2009;63(6):350–353. doi: 10.5455/medarh.2009.63.350-353. [DOI] [PubMed] [Google Scholar]
- 38.Pandza H, Masic I. Distance learning perspectives. Acta Inform Med. 2010;18(4):229. doi: 10.5455/aim.2010.18.229-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haghparast H, Ghorbani A, Rohlin M. Dental students’ perception of their approaches to learning in a PBL programme. Eur J Dent Educ. 2017 Aug;21(3):159–165. doi: 10.1111/eje.12195. [DOI] [PubMed] [Google Scholar]


