Abstract
Introduction:
Pregnancy and childbirth are important periods of women’s life that cause hormonal and bodily changes, and these changes could have significant effects on sexual function.
Aim:
The aim of this study was to assess the effectiveness of PLISSIT-based counselling model on the sexual function of women during the first six months after childbirth.
Material and Methods:
This was a randomized controlled clinical trial study from June to November, 2015. Ninety lactating women,with at least one sexual problem, were included in this study. Samples were recruited and randomized into two groups (intervention group and control group). Demographic and obstetric information, Edinberg postpartum depression, Larson’s sexual satisfaction and female sexual function index questionnaire were used. Data were collected from participants at two points: before consultation and 4weeks after consultation. The statistical analyses were performed using SPSS software and Data were analyzed using the Paired t-test,dependent t-test with parametric data and Chi-square tests.
Results:
Ninety women who were the nulliparous and lactating criteria subjects were randomly divided into two groups and all recruited women completed the questionnaires. Mean score of sexual function was 19.35 before consultation and 27.90 after consultation in experimental group. In the control group, mean score of sexual function was 20.55 before consultation and 22.41 after consultation. These differences were statistically significant in pre-counseling stage and 4 weeks after counseling in the two groups (P<0.001 and P=0.002). Four weeks after consultation, there was significant difference in the mean score of sexual function between the control and experimental groups (P<0.001).
Conclusion:
Based on the result of this study, sexual problems in lactating women decreased by using the PLISSIT model. The use of the PLISSIT model is recommended in health care setting.
Keywords: childbirth, postpartum, PLISSIT model, sexual health, female sexual dysfunction, Iran
1. INTRODUCTION
Sexuality is one of the most important components of health and well-being, and Sexual activity and sexual satisfaction derived from it is one of the most well-known aspect of human life (1). Sexual function is an essential component of life and is recognized as a multidimensional phenomenon which can be influenced by multi biopsychosocial factors (2). “Sexual dysfunctions are a heterogeneous group of disorders that are typically characterized by a clinically significant disturbance in a person’s ability to respond sexually or to experience sexual pleasure. An individual may have several sexual dysfunctions at the same time. In such cases, all of the dysfunctions should be diagnosed”(3). Multiple factors influence sexual function such as hormonal changes, menstrual, pregnancy and childbirth, breast feeding, menopausal and multiparas (4).
Studies have shown that 91.3% of women suffer postpartum sexual problems (5, 6). Several studies conducted in Iran reported the prevalence of physical and sexual problems after delivery to be between 22 and 86% (7-8). During postpartum, the changes such as dyspareunia, lack of libido, vaginal dryness and lack of orgasm can have significant effects on female sexual response cycle and sexual interest and activity tends to be reduced (9). Several factors can have influence on sexual problems in the postpartum period, such as parity, breast feeding, mode of delivery, episiotomy, stress, fatigue and physical and psychological problems such as postpartum depression (10).
In addition, the sociocultural issues and unsuitable performance of health care providers concerning sexual health education can be very important reasons responsible for sexual dysfunction in this period (11). Despite the international emphasis on sexual health, there has been insufficient in developing countries (12). Reasons for this include lack of access to information, education, and health care services, poverty, taboos surrounding discussion of sexuality, and lack of knowledge of service providers in dealing with sexual issues (13). The World Health Organization has recommended the integration of sexual health into existing primary health care services, and also comprehensive sexuality education for young people and health care workers has been proposed as a solution (14).
Several frameworks exist which could be of help to the health care providers in implementing appropriate and effective strategies to address these concerns and sexual problems. One of the methods for handling sexual problems is the PLISSIT model (15). Various internal and external studies have shown that this model reduces the women’s sexual problems (17, 18, 19). Therefore the aim of this study was to assess the effectiveness of PLISSIT-based counseling model on sexual function of women during the first six months after childbirth.
2. METHODS
2.1. Sample recruitment
The present study was performed in Emam Hossien health center in Bandar Abbas, Southeast of Iran, between June 2015 and November 2015. The sample size was calculated at the 5% level of significance. In this single-blinded clinical trial, 120 lactating women who were referred to the Emam Hossien health center in Bandar Abbas were enrolled by the researcher in the study. Finally, 90 mothers completed the study. Women were divided into 2 groups by the researcher using a computer-randomization system. The 2 groups were PLISSIT model and routine care.
2.2. Ethical consideration
The protocol for this study was approved by the ethics and research committee of Shahid Beheshti University of Medical Sciences (No. SBMU2.REC.1394.96, Date 11/06/2015). The trial is registered at Iranian Registry of Clinical Trials (No. IRCT2015062522921N1). After obtaining freely informed written and oral consent, lactating women were allocated by the researcher using a computer-randomization system, in their groups. Participants were allowed to leave the study at any point in time.
2.3. Intervention
A total of 90 participants were eligible for inclusion and written informed consent and phone number was obtained from all women who participated in the study. The questionnaires were answered on a self-reported basis. The participants were assigned simple randomly within two groups according to a preexisting list produced by a computer program.
The inclusion criteria were: (a) age 18–30 years, (b) Primiparous and lactating women after a term singleton delivery (first six months after childbirth), (c) having at least one sexual problemand anxiety and distress among couples, (d) availability during the study. The Exclusion criteria were: becoming pregnant, lack of access to participation, the loss of the baby, history of mental and chronic physical illness, exposure to stressful events during pregnancy and after childbirth, postpartum depression and complications in pregnancy and postpartum, separated from her husband, serious marital dispute and occurrence of undesired life event.
The intervention group received one session of counseling for 2 h by according the first two steps of PLISSIT model, by a trained midwife. Counseling sessions commenced with open-ended questions. Open-ended questions gave the women permission to talk about sexual concerns. Asking questions about sexuality in an initial assessment demonstrated that sexuality is an important issue and showed the practitioner’s comfort level with regards to sexual issues. Based on the results of sexual function and assessment of sexual problem, during permission step, the midwife tried to identify the conditions, such as knowledge deficit, anxiety, pain, body image disturbance and fear. The midwife examined the physical and sexual history in the genital system at any time, if needed. In step 2, based on women’s sexual problems, the midwife explained the physiology of female sexual response, sexual behavior, and sexual intercourse techniques and positions, hormonal changes after childbirth and breast feeding and finally women’s problem. For this purpose, photos, posters and models of the female and male reproductive system were used.
Control group received just routine consultation. In Iran, at the Obstetric units of health centers, midwives provide family planning services and prenatal care as a daily routine work. They have no training and experience about sex education and counseling. Sexual function was evaluated 4 weeks after intervention in the two groups. Counseling sessions for the two groups were being held in a separate and private room in the health center.
2.4. Assessment tools
Demographic and obstetric information, Larson’s sexual satisfaction, Edinberg postpartum depression and Female Sexual Function Index (FSFI) questionnaires were used. The FSFI questionnaire evaluates six domains of female sexual functioning during the last 4 weeks: desire, arousal, lubrication, orgasm, satisfaction, and pain during sexual intercourse. A scoring algorithm was used for assessing each domain, and at the final stage a composite score was generated. The full-scale score range was from 2.0 to 36.0 and cut-off point of maternal sexual dysfunction was considered less than 28 (20). FSFI questionnaire was confirmed via test-retest reliability by Cronbach’s Coefficient Alpha 0.94.
Data were collected from participants at two points: before consultation and 4weeks after consultation. Due to the fact that the postpartum depression and sexual satisfaction were confounding variables, patients with postpartum depression by the Edinburgh questionnaire and Larson’s sexual satisfaction were identified and excluded.
3. STATISTICAL ANALYSIS
The statistical analyses were performed using SPSS(version 16.0, SPSS Inc, Chicago, IL, 2007) software. Data were given as mean and standard deviation. Paired t-test and dependent t-test with parametric data were used for comparison of scores within the groups. Statistical significance was considered at P < 0.05 for all statistical analyses.
4. RESULTS
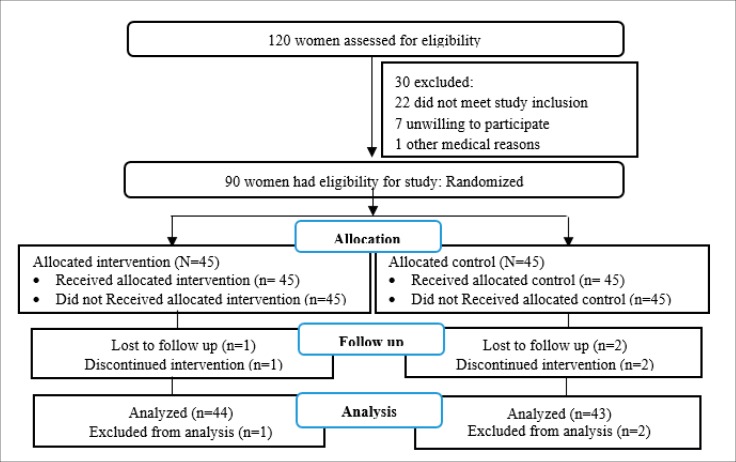
Finally, a total of 90 women who were the nulliparous and lactating criteria subjects were randomly divided into two groups and all recruited women completed the questionnaires. During the study period, three participants dropped out of the study in the control and intervention groups, hence only the data of 87 participants was analyzed (Figure 1).
Figure 1. Design and protocol of the study.
Based on the results of this study, there existed no significant difference between two groups in terms of demographic and obstetric variables (Table 1).
Table 1. Demographic and obstetric characteristics of participants. *Values in parenthesis are percents.
| Characteristics | Intervention M (SD) or No (%) |
Control M (SD) or No (%) |
p-value | |
|---|---|---|---|---|
| Relationship with spouse | Relative Strange |
(48.9 %)22 (51.1 %)23 |
(35.5 %)16 (64.4 %)29 |
0.439 |
| Status of education | Primary school High school Graduate |
(8.9 %)4 (46.7 %)21 (44.4 %)20 |
(8.9 %)4 (48.9 %)22 (42.2 %)19 |
1.000 |
| Status of husband’s education | Primary school High school Graduate |
(13.3 %)6 (48.9%)22 (37.8 %)17 |
(6.7%)3 (42.2 %)19 (51.1 %)23 |
0.463 |
| occupation | housewife Employed |
(80 %)36 (20 %)9 |
(86.7 %)39 (13.3 %)6 |
0.396 |
| Mode of delivery | cesarean section vaginal delivery |
(40 %)18 (60 %)27 |
(48.9 %)22 (51.1 %)23 |
0.396 |
| Age (years) | 24.93 (3.10) | 23.44(2.64) | 0.705 | |
| frequency of intercourse in postpartum period (week) | 1.24(0.75) | 1.40(1.29) | 0.920 | |
| Timing resumption of intercourse (week) | 7.09(2.61) | 6.56(1.58) | 0.561 | |
| Timing after childbirth (month) | 3.56(1.58) | 3.56(1.80) | 0.861 | |
| Postpartum Depression (Edinberg) | 24.53(4.10) | 25.53(3.18) | 0.200 | |
| Sexual satisfaction (Larson) | 11.53(84.76) | 10.70(86.93) | 0.480 | |
There was no statistical difference between sexual satisfaction and Postpartum Depression in two groups before the intervention (P=0.480, P>0.200).
Before intervention, the mean score of sexual function between the two groups was not significantly different. Also, four weeks after consultation, there existed significant difference in the mean score of sexual function between two groups (P<0.001).
In the experimental group, the mean score of sexual function was 19.35 before consultation and 27.90 after consultation, and in the control group, the mean score of sexual function was 20.55 before consultation and 22.41 after consultation. These differences were statistically significant (P<0.001 and P=0.002).In the control group, there was a significant difference in terms of scores of sexual desire, lubrication and pain during the time (P=0.024, P=0.001 and P= 0.004) (Table 2). Further analyses showed after intervention, in the PLISSIT group the female sexual dysfunction was 46.70 %, while in the control group the female sexual dysfunction was 91.10 %. These differences were statistically significant (P<0.001).
Table 2. Comparison of the two groups’ mean scores of FSFI and six domains of female sexual functioning; before and after intervention. *Values are given as mean ± standard deviation (SD).
| groups | ||||||
|---|---|---|---|---|---|---|
| Female Sexual Function Index | intervention | P -value | control | P -value | ||
| Before intervention | 4 weeks after intervention | Before intervention | 4 weeks after intervention | |||
| FSFI total | 19.35±4.63 | 27.90±3.70 | <0.001 | 20.55±3.71 | 22.41±3.86 | 0.002 |
| Desire | 2.80±1.17 | 4.51±0.70 | <0.001 | 3.15±1.07 | 3.47±0.80 | 0.024 |
| Arousal | 3.29±1.07 | 4.81±0.77 | <0.001 | 3.58±0.94 | 3.93±0.84 | 0.052 |
| Lubrication | 3.55±1.27 | 4.96±0.87 | <0.001 | 3.80±1.03 | 4.16±0.84 | 0.001 |
| Orgasm | 2.43±0.99 | 3.46±0.68 | <0.001 | 2.53±0.84 | 2.67±0.73 | 0.117 |
| Satisfaction | 4.38±1.14 | 5.18±0.73 | <0.001 | 4.24±1.01 | 4.27±1.03 | 0.987 |
| Pain | 2.88±1.51 | 4.96±1.01 | <0.001 | 3.19±1.48 | 3.91±1.38 | 0.004 |
5. DISCUSSION AND CONCLUSION
Sexual issue and sexuality are a taboo in majority of the communities. Perceived stigma and embarrassment make people reluctant to discuss and address sexual health issues(21). This was a randomized controlled clinical trial study with the aim to assess the effectiveness of PLISSIT-based counseling model on sexual function of lactating women. Based on the result of this study, sexual problems in lactating women decreased by using the PLISSIT model. Female sexual function is a complex condition that can be affected by social, psychological, hormonal, environmental, and biological factors in a cyclic manner (2).
Farnam et al aimed to evaluate the effectiveness of PLISSIT model and Sexual Health Model on women’s sexual problems that showed the positive impact of this model in improving sexual function and reducing sexual distress (22). Also, Rostamkhani et al. showed that there was significant difference between the control and intervention groups with regard to FSFI mean scores in different domains, before counseling and during 2 and 4 weeks after counseling (19). Nho concluded that sexual health enhancement program is an effective plan in improving sexual function, reducing sexual distress, increasing marital intimacy, and subjecting happiness in women with gynecologic cancer and their husbands (23).
Tutuncu and Yildiz conducted a study in women after hysterectomy and Chun conducted a study in women with Gynecologic Cancer demonstrated that the sexual function improved in the intervention group on the basis of this model (24, 16). Ayaz and Kubilay implemented this model within 8 visits among patients with stoma in which the results showed that the intervention could help to improve sexual function in patients with stoma (18). Also, another study showed that the consultation based on PLISSIT model like cognitive behavior approach can lead to improved sexual function in women suffering from multiple sclerosis (25). According to different literatures, significant effects were found in the treatment of women’s sexual concerns by using the PLISSIT. The significant point was the examination of six domains of sexual function after intervention which showed significant differences between the two groups in all cited studies. While one study showed significant time, differences were found on all domains except for pain in the experimental group because this problem was due to drug complications, and strategies to relieve sexual pain were needed to be considered for greater effectiveness of the program (23). In the control group, there was a significant difference in terms of scores of sexual desire, pain and lubrication during the time, while there was no significant difference in terms of sexual excitement, orgasm and satisfaction. It seems that during those times, more adaptability with postpartum conditions would be created, so their physical and sexual problems would be less than the previous time (22-25).
Despite the willingness of women to receive information about sexual matters from health care centers and health professionals, researches in Iran and other countries have shown that many primary health care providers find it difficult to talk about sexual issues. Embarrassment and lack of confidence, education, and training are considered as the main barriers for opening sexual discussion (26). The most of women referred to health center six weeks after birth for genital examination and reproductive health consultation for choosing a suitable contraceptive method and also, the most of them don’t was express about our sex problems with midwife. So its common sense, sexual consultation begins this period and it is necessary that some plans should be implemented to address this deficiency.
Limitations of this study were first, the lack of consultation with partners. Second, the experimental and control groups and midwives were not blinded to the study. Third, since the accessing to lactation women was difficult (due to fatigue, Disturbing the sleep cycle, physical problem and etc), we follow up once; so a long time follow-up of women exposed to the PLISSIT model would be necessary to determine whether the observed effects were enduring. Forth, Do not use Sexual Distress Scale for sexual distress assessment (According to the expression of person about sexual distress).
Seeking simple and applicable ways of raising and discussing sexual health issues can ease integration and help normalization of sexual health care into a primary health care setting. So the use of the PLISSIT model is recommended in health care setting.
Acknowledgments:
This article is the result of a master’s thesis in midwifery unit of Shahid Beheshti University of Medical Sciences. We appreciate from all the women who had cooperation with researchers of the study and all staff of Emam Hossein’s health center, Bandar Abbas, Iran for facilitating the recruitment of patients and the use of clinical data.
Author’s contribution:
All authors participated in each step of research. N.S.S.H revised it critically. All authors gave confirmation for final reviesed version to be submitted.
Financial support:
This project is funded by the Student Research Committee and Shahid Beheshti University of Medical Sciences.
Conflict of interest:
The authors have no conflict of interest.
REFERENCES
- 1.Liu HL, Hsu P, Chen KH. Sexual activity during pregnancy in Taiwan: a qualitative study. Sexual medicine. 2013 Dec 1;1(2):54–61. doi: 10.1002/sm2.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torkzahrani S, Banaei M, Ozgoli G, Azad M, Emamhadi MA. Postpartum sexual function; conflict in marriage stability: a systematic review. International Journal of Medical Toxicology and Forensic Medicine. IJMTFM. 2015 Dec;6(2):88–98. doi: 10.22037/ijmtfm.v6i2(Spring).10351. [DOI] [Google Scholar]
- 3.American Psychiatric Association. 5th. Washington, DC, London, England: 2013. Diagnostic and Statistical Manual of Mental Disorders. Author. [Google Scholar]
- 4.Yeniel AO, Petri E. Pregnancy, childbirth, and sexual function: perceptions and facts. International urogynecology journal. 2014 Jan 1;25(1):5–14. doi: 10.1007/s00192-013-2118-7. [DOI] [PubMed] [Google Scholar]
- 5.Peck SA. The importance of the sexual health history in the primary care setting. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2001 May 1;30(3):269–274. doi: 10.1111/j.1552-6909.2001.tb01544.x. [DOI] [PubMed] [Google Scholar]
- 6.Acele EÖ, Karaçam Z. Sexual problems in women during the first postpartum year and related conditions. Journal of clinical nursing. 2012 Apr 1;21(7-8):929–937. doi: 10.1111/j.1365-2702.2011.03882.x. [DOI] [PubMed] [Google Scholar]
- 7.Dabiri F, Yabandeh AP, Shahi A, Kamjoo A, Teshnizi SH. The Effect of Mode of Delivery on Postpartum Sexual Functioning in Primiparous Women. Oman Med J. 2014 Jul;29(4):276–279. doi: 10.5001/omj.2014.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirvani MA, Nesami MB, Bavand M. Maternal sexuality after child birth among Iranian women. Pakistan journal of biological sciences: PJBS. 2010 Apr;13(8):385–389. doi: 10.3923/pjbs.2010.385.389. [DOI] [PubMed] [Google Scholar]
- 9.Yıldız H. The relation between prepregnancy sexuality and sexual function during pregnancy and the postpartum period: a prospective study. Journal of sex & marital therapy. 2015 Jan 2;41(1):49–59. doi: 10.1080/0092623X.2013.811452. [DOI] [PubMed] [Google Scholar]
- 10.Brubaker L, Handa VL, Bradley CS, Connolly A, Moalli P, Brown MB, Weber A. Sexual function 6 months after first delivery. Obstetrics and gynecology. 2008 May;111(5):1040. doi: 10.1097/AOG.0b013e318169cdee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilmoth MC. Sexuality: A critical component of quality of life in chronic disease. Nursing Clinics. 2007 Dec 1;42(4):507–514. doi: 10.1016/j.cnur.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Benn RH. London: Department for International Development; 2004. Sexual and reproductive health and rights. A position paper; pp. 1–23. [Google Scholar]
- 13.DeJong J, Jawad R, Mortagy I, Shepard B. The sexual and reproductive health of young people in the Arab countries and Iran. Reproductive health matters. 2005 May 1;13(25):49–59. doi: 10.1016/S0968-8080(05)25181-9. [DOI] [PubMed] [Google Scholar]
- 14.Yelton MM, Delfin NM. Sacramento: California State University; 2015. An Overview of Sexuality in Clinical Practice. Presented to the faculty of the Division of Social Work. [Google Scholar]
- 15.Taylor B, Davis S. The extended PLISSIT model for addressing the sexual wellbeing of individuals with an acquired disability or chronic illness. Sexuality and Disability. 2007 Sep 1;25(3):135–139. doi: 10.1007/s11195-007-9044-x. [DOI] [Google Scholar]
- 16.Chun N. Effectiveness of PLISSIT model sexual program on female sexual function for women with gynecologic cancer. Journal of Korean Academy of Nursing. 2011 Aug 1;41(4):471–480. doi: 10.4040/jkan.2011.41.4.471. [DOI] [PubMed] [Google Scholar]
- 17.Mansour SE, Shebl AM, Waheda SM. The effect of sexual counseling program on pain level and sexual function among women with dyspareunia. J Educ Pract. 2014;5(3):208. [Google Scholar]
- 18.Ayaz S, Kubilay G. Effectiveness of the PLISSIT model for solving the sexual problems of patients with stoma. Journal of Clinical Nursing. 2009 Jan 1;18(1):89–98. doi: 10.1111/j.1365-2702.2008.02282.x. [DOI] [PubMed] [Google Scholar]
- 19.Rostamkhani F, Jafari F, Ozgoli G, Shakeri M. Addressing the sexual problems of Iranian women in a primary health care setting: A quasi-experimental study. Iranian journal of nursing and midwifery research. 2015 Jan;20(1):139. [PMC free article] [PubMed] [Google Scholar]
- 20.Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. Journal of sex & marital therapy. 2005 Jan 1;31(1):1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 21.Shirpak KR, Chinichian M, Maticka-Tyndale E, Ardebili HE, Pourreza A, Ramenzankhani A. A qualitative assessment of the sex education needs of married Iranian women. Sexuality & Culture. 2008 Sep 1;12(3):133–50. doi: 10.1007/s12119-008-9023-0. [DOI] [Google Scholar]
- 22.Farnam F, Janghorbani M, Raisi F, Merghati Khoei E. Compare the effectiveness of PLISSIT and sexual health models on Women’s sexual problems in Tehran, Iran: a randomized controlled trial. The journal of sexual medicine. 2014 Nov 1;11(11):2679–2689. doi: 10.1111/jsm.12659. [DOI] [PubMed] [Google Scholar]
- 23.Nho JH. Effect of PLISSIT Model Sexual Health Enhancement Program for Women with Gynecologic Cancer and Their Husbands. Journal of Korean Academy of Nursing. 2013 Oct 1;43(5) doi: 10.4040/jkan.2013.43.5.681. [DOI] [PubMed] [Google Scholar]
- 24.Tutuncu B, Yildiz H. The influence on women’s sexual functions of education given according to the PLISSIT model after hysterectomy. Procedia-Social and Behavioral Sciences. 2012 Jan 1;47:2000–2004. doi: 10.1016/j.sbspro.2012.06.939. [DOI] [Google Scholar]
- 25.Khakbazan Z, Daneshfar F, Behboodi-Moghadam Z, Nabavi SM, Ghasemzadeh S, Mehran A. The effectiveness of the Permission, Limited Information, Specific suggestions, Intensive Therapy (PLISSIT) model based sexual counseling on the sexual function of women with Multiple Sclerosis who are sexually active. Multiple sclerosis and related disorders. 2016 Jul 1;8:113–119. doi: 10.1016/j.msard.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 26.Munns RA, Weber-Main AM, Lowe MA, Raymond NC. Application of the sexual health model in the long-term treatment of hypoactive sexual desire and female orgasmic disorder. Archives of Sexual Behavior. 2011 Apr 1;40(2):469–478. doi: 10.1007/s10508-010-9673-5. [DOI] [PubMed] [Google Scholar]