Abstract
Aim:
Aim of article was to compare the shear bond strength of indirectly and directly bonded orthodontic brackets.
Materials and methods:
The experimental in vitro study included 60 maxillary and mandibular premolars. Teeth were mounted on cold-cure acrylic blocks for each tooth separately and divided into two groups: directly bonded brackets (30 teeth) and indirectly bonded brackets (30 teeth). Brackets (Discovery, Roth 0.022”, Dentaurum, Ispringen, Germany) were bonded using Transbond XT (3M Unitek, Monrovia, CA, USA) in direct method, while in indirect technique, a combination of Transbond XT and Sondhi Rapid Set (3M Unitek, Monrovia, CA, USA) was used. The shear bond strength and adhesive remnant index (ARI) were evaluated. The in vivo study included 30 subjects - 15 with indirectly bonded brackets and 15 with directly bonded brackets. Survival rate was assessed during the period of 6 months.
Results:
No statistically significant difference in the shear bond strength was found in direct (7.48±1.61 MPa) and indirect labial bonding methods (7.8.2±1.61 MPa). Both methods produced very similar amount of adhesive remnant on tooth surface (median = 1; interquartile range 1–2). There were no significant differences in bracket survival rate between methods.
Conclusion:
Regarding the shear bond strength, adhesive remnant on tooth surface, and survival rate, both indirect and direct methods of orthodontic bracket bonding seem to be equally valuable methods in clinical practice.
Keywords: Shear bond strength, Direct bonding, Indirect bonding
1. INTRODUCTION
The development of adhesive technique leads to transition from banded to bonded edgewise appliances. The minimum shear bond strength range of 6-8 MPa is often cited in the literature as necessary to avoid bracket deboning during application of orthodontic forces (1). Silverman and Cohen first introduced the indirect bracket bonding technique in 1972 (2). They bonded plastic brackets on the plaster model using a methyl methacrylate adhesive, while adhesion between the etched tooth surface and preset adhesive on the bracket was achieved using unfilled Bis-GMA resin. Revolution in the indirect technique was made by Thomas who introduced a method called custom base indirect bonding technique (3). The main characteristic of this technique is the formation of Bis-GMA composite layer (custom base) at a bracket base, shaped according to belonging tooth surface. After removing the transfer tray from the model, the brackets with polymerized composite base adhere to the teeth with two components of sealant. Introduction of custom base indirect technique enabled unlimited operating time and greatly reduced the problem of excess adhesive. However, one of the limitations is the possibility of bond failure because of inadequate share bond strength between custom base and adhesive primer (3). A recent development of orthodontic adhesives especially designed for the usage with the indirect bonding technique has helped a greater applicability of this technique in orthodontics (4, 5). The direct bonding implies a direct fixation of the brackets using orthodontic adhesives, while with the indirect bonding technique the brackets are first placed on the plaster model and later on transferred to the teeth using transfer tray. The indirect method of bracket bonding enables orthodontists to visualize the tooth in three dimensions, which allows a more accurate placement of orthodontic brackets. The indirect bonding also optimizes the doctor’s time spent in the clinic, improves the patient’s comfort, and allows a convenient removal of excess bonding material (6). Despite the fact that indirect technique eliminates most of the limitations of direct technique, indirect technique has not been widely applied in clinical practice. It is supported by the extra expenses and duration of laboratory phase, sensitivity of the multiphase technique, where the error in any phase leads to the weakening of bond strength.
Several studies have been published on the analysis of both direct and indirect techniques in relation to the share bond strength of orthodontic brackets (7-10). Variations in mean bond strength obtained in different studies could be attributed to the fact that many in vitro studies fail to report test conditions that could significantly affect their outcomes (11). A meta-analysis of in vitro orthodontic bond strength testing revealed that each second of photo polymerization time increased bond strength on average by 0.077 MPa, water storage decreased bond strength by 10.7 MPa, and each millimeter per minute of greater crosshead speed increased bond strength by 1.3 MPa (11). Recent systematic review on effectiveness of different bonding materials pointed out generally poor quality of the clinical trial reports (12).
The aim of this study was to assess the differences in share bond strength, failure mode, and survival rate between brackets bonded by direct and indirect techniques. We hypothesized that both techniques produce similar bonding strength in both in vivo and in vitro conditions.
2. MATERIALS AND METHODS
In experimental in vitro study, 60 maxillary and mandibular first premolars with intact buccal enamel surface, extracted for orthodontic purposes were used. Teeth with caries, fillings, fissure sealings, enamel defects, and bleached teeth were excluded.
Twin stainless steel premolar brackets Discovery Roth 0.022’’ (Dentaurum, Ispringen, Germany) with clean laser-treated mesh base of average surface of 14.7 mm2 were used. Maxillary first premolar bracket width was 3.4 mm and mandibular width was 3.3 mm.
After tooth extraction, residual periodontal ligament tissue was removed from the surface of the roots using periodontal scalers; teeth were rinsed with strong jet of water and stored in 0.1% thymol solution at a temperature of 4°C for 7 days. Afterwards, teeth were stored in distilled water in a refrigerator at 4°C until the experiment. Distilled water was changed every week. Teeth whose holding period in distilled water is longer than 12 weeks were not used in the experiment. Before placing in the acrylic blocks, the teeth were cleaned with dental brush mounted on low-speed drill with water cooling. Along the tooth root, the groove is made to prevent possible separation of the teeth from the acrylic block during application of force to the bracket. Each tooth is placed in separate acrylic blocks with dimensions 10×12×15 mm (width × length × height) made from cold cure orthodontic acrylic Orthocryl (Dentaurum, Ispringen, Germany) in specially designed mold and polymerized for 15 min under pressure of two bars in polymerization pressure vessel Polyclav (Dentaurum, Ispringen, Germany).
Specimens were randomly allocated in two groups - direct technique group (N=30) and indirect technique group (N=30). In the direct technique group, buccal surfaces of teeth crowns were cleaned using polishing rubber cones mounted on low-speed drill without abrasive paste usage, followed by rinsing and drying with oil-free air. Buccal enamel was etched with 37% phosphoric acid Unitek etching gel (3M Unitek, Monrovia, CA, USA) for 30 s followed by flushing (5s per tooth) and drying (10s per tooth). Brackets were bonded on teeth using light cured Transbond XT primer and adhesive (3M Unitek, Monrovia, CA, USA) according to the manufacturer’s instructions and polymerized by LED curing unit Unilite II (Bien Air, Bienne, Switzerland) for 20 s from mesial and distal aspect. Excess adhesive material was removed prior to polymerization.
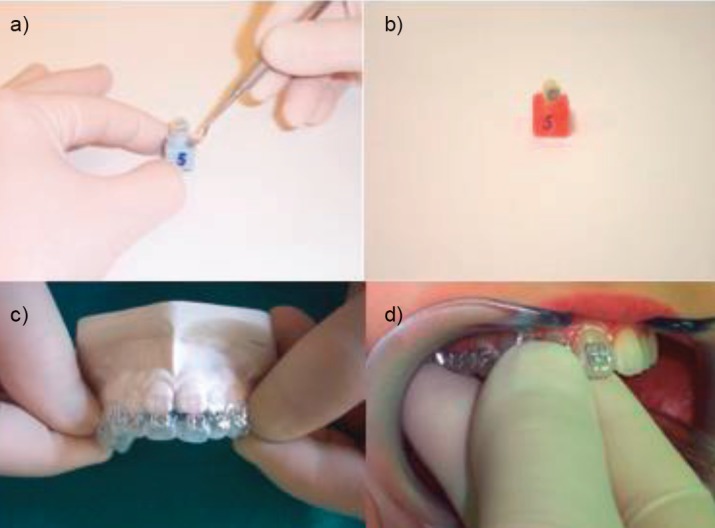
In the indirect technique group, alginate impressions of each tooth in acrylic block were taken and outpoured in hard dental stone Rapidur (Dentaurum, Ispringen, Germany). All the bumps from the surface of each tooth plaster model were removed, and isolation varnish Isolant/C.M.S (Dentsply De Trey, Weybridge, England) was applied and dried for 24 h. Brackets were bonded in proper position on plaster casts using Transbond XT adhesive and placed into a Triad light-curing unit (Dentsply, International, Inc) and cured for 10 minutes. Each cast was set in a vacuum former machine Form 110Vac Former (Discus Dental, Culver City, CA, USA). Transfer tray for indirect technique was formed by heating and vacuuming thermoplastic translucent silicone foil dimensions 5” × 5” × 0.40” (Discus Dental, Culver City, CA, USA) over each cast with bonded bracket according to the manufacturer’s instructions. Plaster block was placed in lukewarm water for 30 min. Translucent foil with bracket was removed from model (Figure 1). Excessive foil material was removed, and each transfer key was cleaned using brush and detergent, flushed with water, and dried thoroughly. Buccal enamel surface of teeth was cleaned, etched, flushed, and dried in the same manner as direct technique group. Chemically cured Sondhi Rapid-Set Resin A (3M Unitek, Monrovia, CA, USA) was applied on etched surface and Resin B on a composite base of bracket fixed in each transfer tray, and tray was placed on tooth in acrylic block for polymerization process and removed after 30 s (Figure 1). Tooth specimens with brackets from both bonding technique groups were kept for 72 h in distilled water at a temperature of 37°C.
Figure 1. a. Removal of translucent transfer key with bracket from plaster model of tooth; b. Bracket bonded on tooth mounted in acrylic bloc; c. Removal of translucent transfer key with brackets from plaster model; d. placement of transfer key with brackets, on teeth in a patient mouth.
Shear bond testing was performed with a universal testing machine Zwick 1435 (Zwick, Ulm, Germany (Figure 2). Apparatus was calibrated by ZAG, Slovenia, and the accuracy was Class 0.5 (i.e., possible 0.5 % deviation in measurement), and the measurement area was from 0 to 5 KN. Following the specimen fixation with a pair of clamps in the lower part of the testing machine, the force administration from the upper part of testing machine was performed with the 0.17×0.25 inch wire applied between the bracket base and bracket wings by loading the specimen until bracket detachment. Constant loading was achieved at 1 mm/min speed. The force direction was gingival-occlusal. The apparatus automatically recorded the force with an accuracy of 0.1 N. The force value was divided by the total surface area of the bracket. Values were presented in N/mm2, i.e., MPa.
Figure 2. Universal testing machine Zwick 1435 (Zwick, Ulm, Germany) for assessment of shear bond strength.

The enamel surfaces after bracket removal were examined using an optical microscope ZKM 01–250C (Carl Zeiss, Jena, Germany) at a magnification of ×30 to assess the amount of adhesive left. Adhesive remnant index (ARI) scores were used: 0, no adhesive left; 1, less than half of adhesive left; 2, half or more; 3, all adhesives were left on the tooth.
The in vivo study included 30 subjects - 15 with directly bonded brackets and 15 with indirectly bonded brackets. The same enamel surface preparation protocol, brackets, adhesive types, and transfer tray were used as in vitro study (Figure 1). Survival rate was assessed during the period of 6 months. Subjects were instructed to avoid eating very hard food (peanuts, almonds, popcorn, etc.) and other types of food that could cause bracket loss.
Mann-Whitney test, t-test, Kaplan-Meier survival analysis, and log-rank test in SPSS 15.0 software (SPSS Inc, Chicago. Ill, USA) were used for statistical analysis, and significance has been predetermined at p<0.05.
3. RESULTS
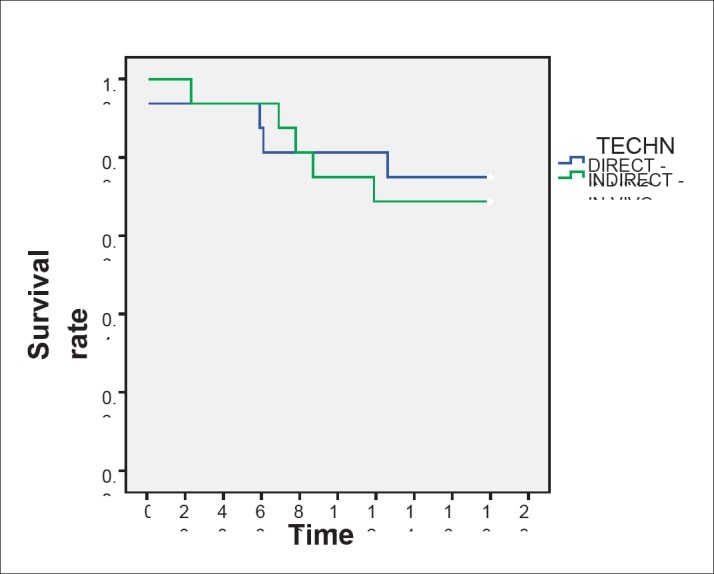
Indirectly bonded specimens showed higher mean shear bond strength (7.82±1.61 MPa) than directly bonded specimens (7.48±1.61 MPa), but the difference was not statistically significant. The results regarding the shear bond strength are shown in Table 1. The comparison of resin remnants between the direct and indirect groups suggests no significant difference in ARI index scores (Table 2). There were no significant differences in brackets survival rate between methods. Average survivor time for directly bonded brackets and indirectly bonded brackets was 148.5±14.7 days and 145.1±13.6 days, respectively, and survival rate was 98.6 and 98.3%, respectively (Figure 3).
Table 1. Shear bond strength values of brackets bonded with direct and indirect technique - in vitro study.
| TECHNIQUE | n | min | max | M | SD | Me |
|---|---|---|---|---|---|---|
| DIRECT | 30 | 4.62 | 10.65 | 7.48 | 1.61 | 0.29 |
| INDIRECT | 30 | 5.30 | 11.56 | 7.82 | 1.61 | 0.29 |
Table 2. Adhesive Remnant Index (ARI) scores by technique.
| TECHNIQUE | N | min | max | M | SD | Me |
|---|---|---|---|---|---|---|
| DIRECT | 30 | 0 | 2 | 1,2 | 0,6 | 0,1 |
| INDIRECT | 30 | 1 | 2 | 1,3 | 0,5 | 0,1 |
Figure 3. Survival rate of directly and indirectly bonded brackets in-vivo in a period of 6 months according to Kaplan Meier survival analysis.
4. DISCUSSION
Indirect bracket bonding technique is still not used by a large number of orthodontists. One of the reasons could be fear that it does not provide sufficient shear bond strength of bracket with the tooth. Voids can be found in composite base in two-thirds of indirectly bonded brackets, which can cause up to 50% lower share bond strength of indirectly bonded brackets (13). Until recently, the indirect technique used adhesive bonding systems originally intended for use in direct bracket placement technique. Currently, there are two adhesive systems presented exclusively designed for indirect technique. The first system uses thermal-cured, fluoride-releasing composite resin to form a custom base and Therma Cure chemically cured adhesive primer Custom IQ (Reliance Orthodontics, USA). Another adhesive system developed exclusively for use in the indirect technique is the Sondhi Rapid-Set, used in this study, where the custom base is formed by light cured Transbond XT composite, while the adhesive primer consists of two chemically cured components.
Average values obtained in this study for the indirect technique using Sondhi Rapid-Set and Transbond XT (7.82 MPa) and the direct technique using Transbond XT (7.48 MPa) are clinically appropriate in terms of power relationships in accordance with generally accepted standards (1). The results of this study coincide with the findings of other studies but the presented values are much lower. Yi et al. using the APC brackets in vitro for the indirect technique reported 11.2 MPa and for direct technique of 10.9 MPa, Linn et al. found 13.8 and 16.3 MPa, and Klocke et al. found 15.0 and 13.9 MPa, respectively (7, 8, 14). They reported higher share bond strength of both Transbond XT adhesive in direct technique and Transbond XT with Sondhi Rapid Set system in indirect technique compared with thermo cured adhesive systems (Therma Cure adhesive and Custom IQ sealant, and Therma Cure in combination with Maximum Cure) (14). On the contrary, Polat et al. presented lower bond strength of Transbond XT-Sondhi Rapid Set than Therma Cure-Custom IQ and direct technique using Transbond XT (10).
Similar failure modes in both techniques were found. ARI index values obtained ranged mostly between 1 and 2, which shows that the detachment was mostly cohesive in character, which means that after debonding, a part of the adhesive remained on the tooth surface, and part of the bracket base. Similar values of bond strength and similar places where detachment has occurred in both techniques show that previously prepared polymerized composite base in an indirect technique is not a weak point in the bracket adhesion. Similar values of ARI index as in our study and insignificant differences between direct and indirect bonding were reported previously (7, 8). Still some authors reported differences in ARI index between two methods after debonding (13-15). In one of the earliest in vitro studies in comparison with direct and indirect bonding methods, 72% of the indirect bonds and 56% of the direct bonds fractured mainly at the enamel-resin interface, which is similar to our data (70% indirect and 66.7% direct, respectively) (13). It seems that the failure site of ceramic brackets usually occurs predominantly in the enamel–resin interface, whereas bond failure with the metal bracket is often in the bracket-resin interface (16). It implies stronger ceramic-adhesive than metal-adhesive bond strength. But, when bond strengths are high, metal bracket failure tends to occur more often at the enamel-adhesive interface, which can cause enamel defects (14). Some authors suggest the use of adhesives with lower bond strength. It ensures easy removal of residual adhesive material from tooth and reduces the possible damage of enamel to a minimum (17).
Numerous factors can influence bond strength, including bracket base design, tooth shape/type, adhesive type, conditioning technique (18, 19, 20). Eliades and Brantley have classified factors that can compromise the credibility of the results of orthodontic bonding testing, such as testing environment, loading mode, bonding substrate, tooth selection, storage and preparation (21). Therefore, our experiment used controlled environmental conditions. Given the long period required to gather the number of teeth needed to perform in vitro tests, teeth were stored in distilled water at 4°C to preserve organic material of enamel. Solution with distilled water was regularly renewed, and the period of storage of extracted teeth was 12 weeks. Teeth stored for longer than this period were not included in the study. Brackets with laser structured base were used because their bond strength was double that of the simple foil mesh base (22).
Results of our in vivo study showed no significant differences between bonding methods, which is in concordance with our in vitro study. Only three clinical trials were conducted to compare the share bond strength and survival rate between direct and indirect bonding methods (3, 23, 24). Survival rates of direct method were reported in the range 94.7-97.5%, and 86-98.7% for indirect method (3, 23, 24). However, it is difficult to make relevant comparisons, because all three studies used different types of adhesives with different periods of observation.
The results of bond strength in vitro studies often do not correlate with the results from clinical studies; so applicability of in vitro studies in clinical practice is questionable (25). Degradation of composites in the mouth is a set of complex interactive processes that cannot be reproduced in vitro; hence, it is essential to develop standardized in vitro and in vivo tests (26).
Taking these findings into consideration, the concordance of findings of our in vitro and in vivo studies indicates the validity of results. This is claimed by a series of authors who believe that the results of in vitro studies serve as a screening test and must be confirmed through identical in vivo studies (21). To date, no study compared these adhesive systems (Transbond XT and Sondhi Rapid-Set) in the two techniques in terms of the oral environment when the quality of interactions was affected by saliva, acids, masticatory, and orthodontic forces.
5. CONCLUSION
According to in vitro and in vivo study, it can be concluded that regarding the shear bond strength, adhesive remnant on tooth surface, and survival rate, both indirect and direct methods of orthodontic bracket bonding seem to be equally valuable methods in clinical practice.
Conflict of interest:
none declared.
Author’s contribution:
Each author participated in each step of manuscript preparing and gave final approval for publishing.
REFERENCES
- 1.Reynolds IR. A review of direct orthodontic bonding. Br J Orthod. 1975;2:171–178. [Google Scholar]
- 2.Silverman E, Cohen M. A universal direct bonding system for both metal and plastic brackets. Am J Orthod Dentofacial Orthop. 1972;62:236–244. doi: 10.1016/s0002-9416(72)90264-3. [DOI] [PubMed] [Google Scholar]
- 3.Thomas RG. Indirect bonding: simplicity in action. J Clin Orthod. 1979;13:93–106. [PubMed] [Google Scholar]
- 4.Sondhi A. Efficient and effective indirect bonding. Am J Orthod Dentofacial Orthop. 1999;115:352–359. doi: 10.1016/s0889-5406(99)70252-0. [DOI] [PubMed] [Google Scholar]
- 5.Alpern MC, Primus C, Alpern AH. The AccuBond system for indirect orthodontic bonding. J Clin Orthod. 2009;43:572–576. [PubMed] [Google Scholar]
- 6.Kalange JT. Indirect bonding: a comprehensive review of the advantages. World J Orthod. 2004;5:301–307. [PubMed] [Google Scholar]
- 7.Yi GK, Dunn WJ, Taloumis LJ. Shear bond strength comparison between direct and indirect bonded orthodontic brackets. Am J Orthod Dentofacial Orthop. 2003;124:577–581. doi: 10.1016/s0889-5406(03)00503-1. [DOI] [PubMed] [Google Scholar]
- 8.Linn BJ, Berzins DW, Dhuru VB, Bradley TG. A comparison of bond strength between direct - and indirect - bonding methods. Angle Orthod. 2006;76:289–294. doi: 10.1043/0003-3219(2006)076[0289:ACOBSB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Shammaa I, Ngan P, Kim H, Kao E, Gladwin M, Gunel E, Brown C. Comparison of bracket debonding force between two conventional resin adhesives and a resin-reinforced glass ionomer cement: an in vitro and in vivo study. Angle Orthod. 1999;69:463–469. doi: 10.1043/0003-3219(1999)069<0463:COBDFB>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Polat O, Karaman AI, Buyukyilmaz T. In vitro evaluation of shear bond strengths and in vivo analysis of bond survival of indirect-bonding resins. Angle Orthod. 2004;74:405–409. doi: 10.1043/0003-3219(2004)074<0405:IVEOSB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Finnema KJ, Ozcan M, Post WJ, Ren Y, Dijkstra PU. In-vitro orthodontic bond strength testing: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2010;137:615–622. doi: 10.1016/j.ajodo.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 12.Mandall NA, Millett DT, Mattick CR, Hickman J, Worthington HV, Macfarlane TV. Orthodontic adhesives: a systematic review. J Orthod. 2002;29:205–210. doi: 10.1093/ortho/29.3.205. [DOI] [PubMed] [Google Scholar]
- 13.Hocevar RA, Vincent HF. Indirect versus direct bonding: bond strength and failure location. Am J Orthod Dentofacial Orthop. 1988;94:367–371. doi: 10.1016/0889-5406(88)90125-4. [DOI] [PubMed] [Google Scholar]
- 14.Klocke A, Shi J, Kahl-Nieke B, Bismayer U. Bond strength with custom base indirect bonding techniques. Angle Orthod. 2003;73:176–180. doi: 10.1043/0003-3219(2003)73<176:BSWCBI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Sinha PK, Nanda RS, Duncanson MG, Hosier MJ. Bond strengths and remnant adhesive resin on debonding for orthodontic bonding techniques. Am J Orthod Dentofacial Orthop. 1995;108:302–307. doi: 10.1016/s0889-5406(95)70025-0. [DOI] [PubMed] [Google Scholar]
- 16.Odegaard J, Segner D. Shear bond strength of metal brackets compared with a new ceramic bracket. Am J Orthod Dentofacial Orthop. 1988;94:201–206. doi: 10.1016/0889-5406(88)90028-5. [DOI] [PubMed] [Google Scholar]
- 17.Martin S, Garcia-Godoy F. Shear bond strength of orthodontic brackets cemented with a zinc oxide-polyvinyl cement. Am J Orthod Dentofacial Orthop. 1994;106:615–620. doi: 10.1016/S0889-5406(94)70086-9. [DOI] [PubMed] [Google Scholar]
- 18.Faltermeier A, Behr M. Effect of bracket base conditioning. Am J Orthod Dentofacial Orthop. 2009;135:12.e1–5. doi: 10.1016/j.ajodo.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 19.Sharma-Sayal SK, Rossouw PE, Kulkarni GV, Titley KC. The influence of orthodontic bracket base design on shear bond strength. Am J Orthod Dentofacial Orthop. 2003;124:74–82. doi: 10.1016/s0889-5406(03)00311-1. [DOI] [PubMed] [Google Scholar]
- 20.Summers A, Kao E, Gilmore J, Gunel E, Ngan P. Comparison of bond strength between a conventional resin adhesive and a resin-modified glass ionomer adhesive: an in vitro and in vivo study. Am J Orthod Dentofacial Orthop. 2004;126:200–206. doi: 10.1016/j.ajodo.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 21.Eliades T, Brantley WA. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur J Orthod. 2000;22:13–23. doi: 10.1093/ejo/22.1.13. [DOI] [PubMed] [Google Scholar]
- 22.Sorel O, El Alam R, Chagneau F, Cathelineau G. Comparison of bond strength between simple foil mesh and laser-structured base retention brackets. Am J Orthod Dentofacial Orthop. 2002;122:260–266. doi: 10.1067/mod.2002.125834. [DOI] [PubMed] [Google Scholar]
- 23.Aguirre MJ, King GJ, Waldron JM. Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. Am J Orthod. 1982;82:269–276. doi: 10.1016/0002-9416(82)90461-4. [DOI] [PubMed] [Google Scholar]
- 24.Thiyagarajah S, Spary DJ, Rock WP. A clinical comparison of bracket bond failures in association with direct and indirect bonding. J Orthod. 2006;33:198–204. doi: 10.1179/146531205225021615. [DOI] [PubMed] [Google Scholar]
- 25.Sunna S, Rock WP. Clinical performance of orthodontic brackets and adhesive systems: a randomized clinical trial. Br J Orthod. 1998;25:283–287. doi: 10.1093/ortho/25.4.283. [DOI] [PubMed] [Google Scholar]
- 26.Oilo G. Biodegradation of dental composites/glass-ionomer cements. Adv Dent Res. 1992;6:50–54. doi: 10.1177/08959374920060011701. [DOI] [PubMed] [Google Scholar]


