Abstract
Purpose
To determine uptake, barriers and outcomes in the follow-up of patients referred for free-of-charge, expedited cataract surgery in the Sao Paulo Eye Study (SPES).
Methods
SPES was a population-based study of urban, low-middle income residents ≥50 years old. Presenting (PVA) and best-corrected (BCVA) visual acuity, refraction, and slit-lamp examination were performed in 3,677 participants. For subjects with cataract as a principal cause of BCVA ≤ 20/40, surgery was offered free-of-charge. Two years after the baseline study, surgery uptake, barriers to surgery, and visual outcomes were analyzed.
Results
Among 210 (5.71%) participants who had cataract surgery indication at baseline, 164 (78.1%) were successfully contacted and 55 (33.5%) reported being operated on for cataract, with 51 agreeing to be re-examined. In a multiple logistic regression model, age, gender, schooling, previous cataract surgery, and PVA at baseline were not significantly associated with surgery uptake. Co-existing health conditions (20.4%), fear of surgery (12.2%) and fear of losing eyesight (11.6%) were the most frequent barriers for cataract surgery adherence. Among the 69 eyes operated on in the interval between baseline and follow-up, PVA ≥20/63 was observed in 50 (72.6%; 95% confidence interval 62.2%-82.3%), PVA <20/63-20/200 in 11 (15.9%; 8.9%-22.9%) and PVA <20/200 in 8 (11.6%; 5.3%-17.9%).
Conclusions
Quality of surgery is an increasing determinant of uptake rates. Although free-of-charge and expedited cataract surgery were offered, surgical outcomes might have influenced the low uptake. Besides cataract surgery campaigns, improvement of surgeon skills, accurate biometry, treatment of ocular comorbidities, postoperative follow-up, and eye-care education are needed.
Keywords: cataract, cataract surgery, uptake, barriers, outcomes
INTRODUCTION
Actions to increase access to modern cataract surgery were implemented in Brazil beginning in 1999 through a national program that increased the annual cataract surgical rate (CSR) throughout the country from approximately 600 per million population in the years immediately prior to 1998 to 1,815 in 2002.1 However, even with free-of-charge surgery becoming more readily available, the Sao Paulo Eye Study (SPES), a 2004–2005 survey of persons ≥50 years of age in the city of Sao Paulo, estimated the prevalence of unilateral blindness due to cataract as 1.73%, and 0.60% for bilateral blindness.2 Cataract blindness continues as a leading cause of blindness, not just in Brazil, but throughout Latin America.3
Even when cataract surgery services are available, there are barriers which keep patients from using and benefiting from these services. Determining barriers to use of eye care services is critical for planning strategies to prevent blindness.4-11 Reasons for poor uptake of cataract surgery have been investigated in previous studies in developing countries with cost or out-of-the-pocket expenses related to cataract surgery identified as a maj or barrier in several studies.12–18 It is still unclear whether there will be any improvement in adherence to a cataract surgery recommendation by offering free-of-charge surgical services.
Along with raising the CSR, the degree of vision restoration achieved with cataract surgery is of increasing concern, as several studies have shown that surgical outcomes in Brazil have not always resulted in optimal post-operative vision.1,19 Although refraction after cataract extraction is a fast and inexpensive way of improving vision outcomes20, refractive error was implicated in the SPES as the cause of visual impairment (presenting visual acuity <20/63) in 58.8% of cataract-operated eyes, with 16.5% blind (presenting visual acuity <20/200) due to inadequate or lack of glasses.1 It is becoming increasingly evident that pre-operative screening of co-morbidities, correction of refractive errors and post-operative follow-up care are key points in achieving the sight-restoring potential of modern cataract surgery.21
We sought to assess surgical outcomes and barriers to the use of expedited and free-of-charge cataract surgical services to investigate possible strategies for more effective service delivery. The data presented here pertain to a follow-up of the 210 participants referred for cataract surgery in SPES, carried out in three low- to middle-income Sao Paulo districts with a 2000 census population of 346,170. As previously described, SPES was fairly representative in socio-economic terms of the urban population throughout Brazil.1
MATERIALS AND METHODS
SPES was based on cluster sampling with random selection of census areas within each of the three study districts, and conducted over a 16-month period beginning in July 2004. A total of 4,224 persons ≥ 50 years of age were enumerated in door-to-door visits with 3,677 (87%) examined. Written informed consent was obtained from all participants at the time of the examination. The study was cleared by the Committee on Ethics in Human Research of Federal University of Sao Paulo (UNIFESP) and the World Health Organization (WHO) Secretariat Committee on Research Involving Human Studies and followed the tenets of the Declaration of Helsinki.
Presenting distance visual acuity was measured using a retro-illuminated logMAR tumbling E chart positioned at 4 meters, followed by an eye examination. For eyes with presenting distance visual acuity 20/40 or worse, refractive error was considered as the cause of visual impairment if best-corrected distance visual acuity after refraction improved to 20/32 or better. For eyes with best-corrected visual acuity 20/40 or worse, the principal cause of visual impairment/blindness was assigned by the examining ophthalmologist using a 14-item list. Cataract was assigned when lens opacity was considered the main cause of reversible visual acuity impairment. Further details regarding enumeration of subjects and the eye examination were presented in a previous article.2
Those with cataract as the main cause of visual impairment in either eye were referred for expedited free-of-charge cataract surgery at Hospital Municipal de Ermelino Matarazzo (HMEM), the local public hospital. Approximately two years after the initial study examination an attempt was made to contact all participants referred for cataract surgery for a personal interview to obtain information regarding whether cataract surgery had been performed. This follow-up field work was carried out over a 10-month period, from March 2007 to January 2008. In order to determine the possible barriers to reaching cataract services, a 13-item questionnaire (WHO, 2001) was translated into Portuguese, and back into English by one of the authors (SRS) who is a trained official translator, and administered to those who reported not being operated on for cataract in the interval between baseline and follow-up. Subjects could report up to four barriers.
Those reported being operated on were invited to an eye examination at HMEM–where participants were queried as to the date and place of surgery for each operated eye. Presenting distance visual acuity was measured by trained ophthalmic technologists using a retro-illuminated logMAR tumbling E chart. Slit-lamp and direct ophthalmoscope examination of the external eye, anterior segment and fundus, including looking for evidence of cataract surgery complications, was performed by one of the authors (MHM). The type of cataract surgery (based on wound size and placement, and the presence of sutures) and posterior capsule status were noted in the examination of cataract-operated eyes. Eyes with presenting distance visual acuity 20/40 or worse were assigned a principal cause of visual impairment/blindness using a 14-item list.
Stata/SE Statistical Software, Release 12.0, 2011 (Stata Corp, College Station, Texas, USA) was used for data tabulations and analysis. WHO visual acuity categories 20/20-20/60 [good visual acuity], <20/60-20/200 [borderline visual acuity] and <20/200 [poor visual acuity] were used in summarizing visual acuity data. Multiple logistic regression was used to investigate the association between the uptake of cataract surgery and age, gender, schooling, previous cataract surgery, and presenting visual acuity. Confidence intervals for regression odds ratios (OR) and visual acuity estimates were calculated taking cluster sampling design effects into account.
RESULTS
From the baseline sample of 3,677 examined participants, 210 (5.71%) were referred for expedited free-of-charge cataract surgery at HMEM (excluding eight additional individuals without reliable baseline visual acuity measurement because of cognitive impairment/stroke). It was not possible to obtain any follow-up information on 15 of the 210 who had moved away from the study area. Of the remaining 195 baseline participants, it was possible to contact 164 of them, as 31 were deceased as reported by household members. Fifty-five of the 164 contacted participants reported having had cataract surgery after the baseline examination, with 51 of these agreeing to be re-examined (Figure 1).
Figure 1.
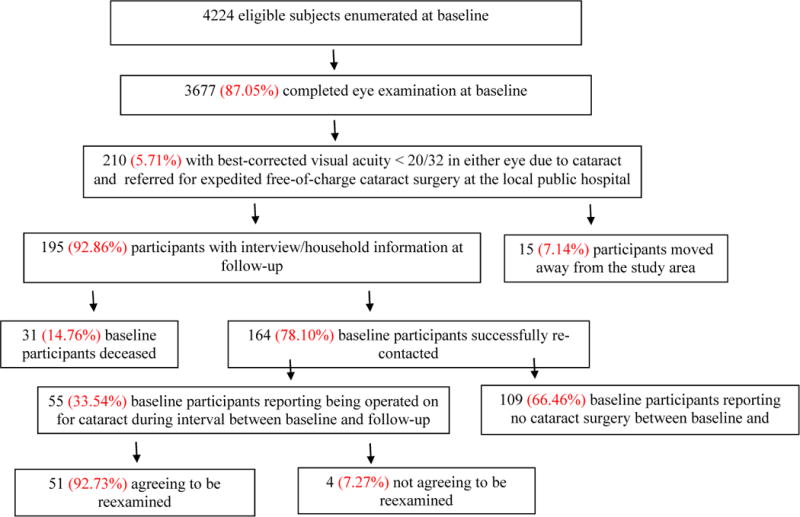
Flowchart for ascertainment of the follow-up study cohort
Table 1 shows the age, gender, and schooling of the 210 referred for cataract surgery, the 164 contacted at follow-up, and the 51 of the 55 reporting having had cataract surgery after the baseline examination willing to be re-examined.
Table 1.
The distribution of age, gender and schooling in participants referred for cataract surgery at baseline, those re-contacted at follow-up, and those having had cataract surgery in the interval between baseline and follow-up and examined at follow-up.
| Referred at baseline | Contacted at follow-up | Examined at follow-up | |
|---|---|---|---|
| Baseline age | |||
| 50-59 | 18 (8.6%) | 14 (8.5%) | 3 (5.9%) |
| 60-69 | 50 (23.8%) | 38 (23.2%) | 19 (37.2%) |
| ≥70 | 142 (67.6%) | 112 (68.3%) | 29 (56.9%) |
| Gender | |||
| Female | 146 (69.5%) | 117 (71.3%) | 38 (74.5%) |
| Male | 64 (30.5%) | 47 (28.7%) | 13 (25.5%) |
| Schooling | |||
| No formal | 85 (40.5%) | 66 (40.2%) | 23 (45.1%) |
| ≥ 1 year | 114 (54.3%) | 92 (56.1%) | 26 (51.0%) |
| No information | 11 (5.2%) | 6 (3.7%) | 2 (3.92%) |
| All | 210 (100.0%) | 164 (100.0%) | 51 (100.0%) |
Barriers And Uptake to Cataract Surgery
Out of the 164 contacted patients, 109 (66.5%) subjects reported not having cataract surgery in the interval between baseline and follow-up – 77 (70.6%) were females and 80 (73.4%) were aged 70 years and older. Reasons for not following the cataract surgery indication are listed in Table 2. Co-existing health conditions contra-indicating cataract surgery (35 positive answers) appeared to be the major factor preventing the attainment of higher cataract surgical uptake in this group, followed by fear of operation and fear of losing eyesight. Lack of escorts, unavailable surgical services and distance of surgical services were some of the main barriers listed by persons between 50 and 59 years old. Lack of awareness of cataract was the main barrier for men.
Table 2.
Barriers reported by the 109 subjects not responding to the cataract surgery indication.
| Barriers | N* | % |
|---|---|---|
| Disease contra-indicating operation | 35 | 20.35 |
| Fear of operation | 21 | 12.21 |
| Fear of losing eyesight | 20 | 11.63 |
| Old age and need not felt | 17 | 9.88 |
| One eye adequate vision / need not felt | 16 | 9.30 |
| No one to accompany | 15 | 8.72 |
| Unaware of cataract | 14 | 8.14 |
| Surgical services not available or very far | 13 | 7.56 |
| No time available / other priorities | 9 | 5.24 |
| Waiting for cataract to mature | 8 | 4.65 |
| Believes it to be a curse | 2 | 1.16 |
| No / delayed information about eye camp | 2 | 1.16 |
| Cannot afford operation | 0 | 0.00 |
| TOTAL | 172 | 100.00 |
Subjects could report up to four reasons/barriers.
Thirty-three (64.7%) of the 51 examined subjects had unilateral cataract surgery in the interval between baseline and follow-up – including 12 who had already been operated in one eye prior to baseline – with 18 (35.3%) having had bilateral cataract surgery.
In a multiple logistic regression model, age (odds ratio [OR], 0.97; 95% confidence interval [CI]: 0.94-1.02, P=231), gender (OR, 1.11; 95% CI: 0.51-2.41, P= 800), schooling (OR, 0.64; 95% CI: 0.30-1.37, P=253), previous cataract surgery (OR, 1.14; 95% CI: 0.47-2.74, P=.775), and presenting visual acuity in both the better (OR, 1.06; 95% CI: 0.95-1.18, P=.287) and worse eye (OR, 1.02; 95% CI: 0.91-1.14, P=.716) were not associated with the uptake of cataract surgery among the 164 contacted at follow-up.
Surgical Outcomes
At the time of the baseline examination, 30 (58.8%; 95% CI: 44.8%-72.9%) of the 51 participants operated on for cataract after baseline had presenting visual acuity (PVA) ≥20/63 in the better eye, with 12 (23.5%; 12.6%-34.4%) having PVA <20/63-20/200 and 9 (17.6%; 6.5%-28.8%) with PVA <20/200. At the follow-up examination, the number with PVA ≥20/63 increased to 42 (82.4%; 68.5%-96.2%) and the number with PVA <20/200 decreased to 3 (5.9%; 1.2%-16.2%). Six (11.8%; 2.2%-21.3%) had PVA <20/63-20/200 at follow-up (Table 3).
Table 3.
Presenting visual acuity (PVA) in the better-eye at baseline and at follow-up for 51 participants and 69 cataract-operated eyes in the interval between baseline and follow-up.
| Baseline PVA | Follow-up PVA | |||
|---|---|---|---|---|
| 20/20-20/63 | <20/63-20/200 | <20/200 | ALL | |
| 20/20-20/63 | 28 (54.8%) | 1 (2.0%) | 1 (2.0%) | 30 (58.8%) |
| 18 (26.1%) | 2 (2.8%) | 0 (0.0%) | 20 (28.9%) | |
| <20/63-20/200 | 10 (19.6%) | 2 (3.9%) | 0 (0.0%) | 12 (23.5%) |
| 16 (23.3%) | 4 (5.7%) | 1 (1.4%) | 21 (30.4%) | |
| <20/200 | 4 (7.9%) | 3 (5.9%) | 2 (3.9%) | 9 (17.7%) |
| 16 (23.2%) | 5 (7.3%) | 7 (10.2%) | 28 (40.7%) | |
| ALL | 42 (82.3%) | 6 (11.8%) | 3 (5.9%) | 51 (100.0%) |
| 50 (72.6%) | 11 (15.8%) | 8 (11.6%) | 69 (100.0%) |
Note: Top line refers to 51 participants and bottom line (italics) refers to cataract-operated eyes.
Sixty-nine eyes were operated on in the 51 participants between baseline and follow-up. Fifty eyes (72.5%; 62.2%-82.3%) presented with good visual acuity (PVA ≥20/63) after cataract surgery, 11 (15.9%; 8.9%-22.9%) with borderline visual acuity (PVA <20/63-20/200), and 8 (11.6%; 5.3%-17.9%) with poor vision (PVA <20/200) (Table 3).
Presenting visual acuity improved by two or more lines in 55 eyes (79.7%), and best corrected visual acuity improved by two or more lines in 59 eyes (85.5%). Presenting visual acuity was worse by two or more lines in 2 eyes (2.9%) and best-corrected visual acuity was worse by two or more lines in 3 eyes (4.3%).
Of the 69 eyes operated on between baseline and follow-up, 59 (85.5%) were performed at HMEM. In examining the type of surgery, phacoemulsification appeared to have been the technique of choice in 61 (88.4%) of these 69 eyes. Eight (11.6%) eyes had extracapsular cataract extraction with IOL.
Evidence of one or more surgical complications was noted in 6 (50.0%) of the 12 eyes that were operated on prior to the baseline examination, and in 13 (18.8%) of the 69 eyes operated on in the interval between baseline and follow-up (Table 4).
Table 4.
Cataract surgery complications in 12 eyes operated on for cataract prior to the baseline examination and in 69 eyes operated on in the interval between baseline and follow-up.
| Complication | Time of cataract surgery | ||
|---|---|---|---|
| Before baseline | After Baseline | ALL | |
| No complication | 6 (50.0%) | 56 (81.2%) | 62 (76.5%) |
| Posterior capsule opacification | 1 (8.33%) | 3 (4.34%) | 4 (4.94%) |
| Comeal decompensation | 1 (8.33%) | 1 (1.45%) | 2 (2.47%) |
| Vitreous in anterior chamber/surgical wound | 1 (8.33%) | 2 (2.90%) | 3 (3.70%) |
| IOL iris (pupilar) capture | 1 (8.33%) | 2 (2.90%) | 3 (3.70%) |
| Posterior capsule rupture | 2 (16.7%) | 3 (4.35%) | 5 (6.17%) |
| Subluxed/deslocated IOL | 2 (16.7%) | 0 (0.00%) | 2 (2.47%) |
| Other/unspecified complication | 4 (33.3%) | 10 (14.5%) | 14 (17.3%) |
| All | 12 (100.0%) | 69 (100.00%) | 81 (100.00%) |
Note: Columns add to more than the total number of eyes because some eyes had multiple complications.
Table 5 shows causes of vision impairment across all 102 eyes in the 51 participants with cataract surgery in one or both eyes between baseline and follow-up. Thirty-one (30.4%) were without vision impairment (visual acuity ≥20/32), and among 71 eyes (69.6%) with vision impairment, refractive error, retinal disorders and un-operated cataract were the most common causes.
Table 5.
Principal cause of presenting visual impairment (visual acuity ≤20/40) in 102 eyes of 51 participants examined at follow-up.
| Principal cause | Time of cataract surgery | All | ||
|---|---|---|---|---|
| Before baseline | After baseline | Not operated | ||
| No visual impairment* | 3 (25.0%) | 25 (36.2%) | 3 (14.3%) | 31 (30.4%) |
| Refractive error | 1 (8.33%) | 14 (20.3%) | 2 (9.52%) | 17 (16.7%) |
| Amblyopia | 0 (0.00%) | 3 (4.35%) | 0 (0.00%) | 3 (2.94%) |
| Cataract | 0 (0.00%) | 0 (0.00%) | 14 (66.7%) | 14 (13.7%) |
| Posterior capsule opacification | 0 (0.00%) | 2 (2.90%) | 0 (0.00%) | 2 (1.96%) |
| Corneal opacity/scar | 0 (0.00%) | 1 (1.45%) | 0 (0.00%) | 1 (0.98%) |
| Absent/disorganized globe | 0 (0.00%) | 0 (0.00%) | 2 (9.52%) | 2 (1.96%) |
| Glaucoma | 1 (8.33%) | 7 (10.1%) | 0 (0.00%) | 8 (7.84%) |
| Other optic atrophy | 0 (0.00%) | 1 (1.45%) | 0 (0.00%) | 1 (0.98%) |
| Macular degeneration | 4 (33.3%) | 4 (5.80%) | 0 (0.00%) | 8 (7.84%) |
| Diabetic retinopathy | 0 (0.00%) | 5 (7.25%) | 0 (0.00%) | 5 (4.90%) |
| Other retinal disorders | 1 (8.33%) | 5 (7.25%) | 0 (0.00%) | 6 (5.88%) |
| Other causes | 2 (16.7%) | 1 (1.45%) | 0 (0.00%) | 3 (2.94%) |
| Undetermined | 0 (0.00%) | 1 (1.45%) | 0 (0.00%) | 1 (0.98%) |
| ALL | 12 (100.0%) | 69 (100.0%) | 21 (100.0%) | 102 (100.0%) |
Presenting visual acuity ≥20/32.
DISCUSSION
The strength of this study is that it is a follow-up of patients referred for cataract surgery within a randomly selected population-based study sample from three representative urban districts of Sao Paulo. Approximately two years after the baseline study, 164 (78.1%) of the 210 participants referred for cataract surgery at baseline were successfully contacted, and 51 (92.7%) of the 55 reporting cataract surgery in the interval between baseline and follow-up were re-examined.
One hundred and nine (66.5%) subjects of the 164 that were contacted did not report having had cataract surgery in the interval between baseline and follow-up. (It should be noted that those not reporting cataract surgery were not re-examined; thus, it is possible that a somewhat greater number actually had cataract surgery considering that some may have decided not to report it.). Although indirect financial obstacles such as transport to hospital/clinic, taking time off work, leaving daily responsibilities and wage earning hours lost by the family could have been taken into consideration, the uptake of free of cost cataract surgery was unexpectedly low. Age, gender, schooling, previous cataract surgery, and presenting visual acuity in both the better and worse eye were not statistically significant for adherence to cataract surgery among the 164 referred for treatment at baseline and contacted at follow-up. However, these results should be cautiously interpreted considering the small study sample. Co-existing health conditions contraindicating cataract surgery appeared as a major barrier especially among those 60 years of age or older and among females, followed by fear of surgery and fear of losing eyesight. The lack of an accompanying escort and unavailability of close-by surgical services were listed as barriers by those between 50 and 59 years of age. Health condition was an important factor in both those with and without any formal education.
Older age, lower levels of education, presence of ocular co-morbidity22,23, surgical complications, worse baseline visual acuity22, along with the need for capsulotomy, spectacle prescription and other care have been shown to be associated with a poorer cataract surgery outcome.23 In a recent study in rural India, the major cause of presenting visual impairment after cataract surgery was incorrect intraocular lens power (42%), with posterior capsule opacification (24%), surgical complications (21%) and age-related macular degeneration (10.3%) being the major causes of best-corrected visual impairment.24 Among studies in Brazil, refractive error1,19, retinal disorders and macular degeneration1, and posterior capsule opacification1,19 were the main causes of visual impairment in cataract operated eyes.
According to WHO Guidelines for monitoring the outcomes of cataract surgery25, at least 80% of eyes should have12-week post-operative PVA ≥20/60 for visual acuity outcomes to be considered good. In our sample surgical visual outcomes were below WHO targets: good outcomes were obtained in 72.5% (62.6%-82.3%) of operated eyes instead of ≥80%, borderline outcomes were present in 15.9% (8.9%-22.9%) instead of ≤15% and poor outcomes were present in 11.6% (5.3%-17.9%) instead of ≤5% (Table 3). Cataract surgery outcomes such as these might have had a negative influence and contributed to poor adherence to the cataract surgery indication.
Visual acuity of 20/40 or better is important in densely populated urban areas such as Sao Paulo, where visual requirements for driving and work purposes can be demanding. Indeed, with cataract surgery being considered a means to achieve refractive correction, visual acuity of 20/20 is the outcome expected by many patients. Among 69 operated eyes, PVA >20/40 was attained in only 25 (36.2%).
Improvement in vision could have been realized to a greater extend were it not for uncorrected refractive error in cataract-operated eyes. Overall, 53 (65.4%) of the 81eyes operated for cataract either before or after baseline had presenting visual acuity ≤20/40, with uncorrected refractive error as the principal cause of vision impairment in 15 (28.3%) of these (Table 5). In the original population-based SPES sample, among the 352 cataract-operated eyes, 58.8% presented with PVA ≤20/40 and 38.1% with best correction.1 Vision impairment due to uncorrected refractive error should be avoided with accurate assessment of IOL power along with provision of adequate spectacles post-operatively.
Retinal disorders were another important cause of visual impairment in cataract-operated eyes. In the 69 eyes operated between baseline and follow-up, 14 (20.3%) had vision impairment caused by macular degeneration, diabetic retinopathy or other retinal disorders. It is widely recognized that pre-operative ocular diseases, such as age-related macular degeneration and various other retinal disorders, can lead to poor visual outcome and patient dissatisfaction after cataract surgery.26-28
Surgical complications are also widely recognized as having negative influences on vision outcomes.29 Most of the patients with cataract surgery in the interval between baseline and follow-up underwent phacoemulsification at HMEM by second and third year residents, with nearly one in five eyes having evidence of one or more surgical complications. Of the eyes operated on prior to baseline, half had evidence of surgical complications. Posterior capsule rupture was relatively frequent and higher than the 2.2% reported in the literature.30
In Brazil, cataract remains an important cause of treatable blindness2,31 with a CSR substantially below that recommended by the WHO.32 Further, unsatisfactory correction of refractive error and high surgical complication rates in some settings contribute to poor post-operative vision outcomes. Strategic components in the achievement of improved cataract surgery outcomes include precise surgical techniques with extensive training, screening for co-existing eye diseases, accurate intraocular lens (IOL) calculation to minimize refractive errors, prescription of appropriate lenses and periodic monitoring to detect late complications such as posterior capsule opacification.
Acknowledgments
Coordenadoria de Apoio a Pessoal de Nivel Superior (CAPES, Brasilia, Brasil) post-doctoral scholarship to MHM; Conselho Nacional de Desenvolvimento Cientifico e Tecnologico (CNPq, Brasilia, Brasil) research scholarships to AB, RB and SRS; World Health Organization (WHO), Geneva, Switzerland (under the National Institutes of Health, Bethesda, Maryland contract no. NEI-EY-2103).
Footnotes
Setting: Dept. of Ophthalmology, Federal University of Sao Paulo, Sao Paulo, Brazil
Proprietary Interest: None
References
- 1.Salomao SR, Soares FS, Berezovsky A, Araujo-Filho A, Mitsuhiro MRKH, Watanabe SES, Carvalho AV, Pokharel GP, Belfort R, Jr, Ellwein LB. Prevalence and Outcomes of Cataract Surgery in Brazil: The Sao Paulo Eye Study. Am J Ophthalmol. 2009;148:199–206. doi: 10.1016/j.ajo.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salomao SR, Cinoto RW, Berezovsky A, Araujo-Filho A, Mitsuhiro MRKH, Mendieta L, Morales PHA, Pokharel GP, Belfort R, Jr, Ellwein LB, et al. Prevalence and Causes of Vision Impairment and Blindness in Older Adults in Brazil: The Sao Paulo Eye Study. Ophthalmic Epidemiol. 2008;15:167–175. doi: 10.1080/09286580701843812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Furtado JM, Lansingh VC, Carter MJ, Milanese MF, Peña BN, Ghersi HA, Bote PL, Nano ME, Silva JC. Causes of Blindness and Visual Impairment in Latin America. Surv Ophthalmol. 2012;57:149–177. doi: 10.1016/j.survophthal.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Chandrashekhar TS, Bhata HV, Paia RP, Naira SK. Coverage, utilization and barriers to cataract surgical services in rural South India: Results from a population-based study. Public Health. 2007;121:130–136. doi: 10.1016/j.puhe.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 5.Nkumbe H. Helping older people get the eye care they need. Community Eye Health. 2008;21:26–28. [PMC free article] [PubMed] [Google Scholar]
- 6.Chibuga E, Massae P, Geneau R, Mahande M, Lewallen S, Courtright P. Acceptance of cataract surgery in a cohort of Tanzanians with operable cataract. Eye. 2008;22:830–833. doi: 10.1038/sj.eye.6702736. [DOI] [PubMed] [Google Scholar]
- 7.Athanasiov PA, Edussuriya K, Senaratne T, Sennanayake S, Selva D, Casson RJ. Cataract in central Sri Lanka: cataract surgical coverage and self-reported barriers to cataract surgery. Clin Experiment Ophthalmol. 2009;37:780–784. doi: 10.1111/j.1442-9071.2009.02152.x. [DOI] [PubMed] [Google Scholar]
- 8.Zhang M, Wu X, Li L, Huang Y, Wang G, Lam J, Lam DSC, Gao Y, Griffiths S, Congdon N. Understanding barriers to cataract surgery among older persons in rural China through focus groups. Ophthalmic Epidemiol. 2011;18:179–186. doi: 10.3109/09286586.2011.580884. [DOI] [PubMed] [Google Scholar]
- 9.Abubakar T, Gudlavalleti MVS, Sivasubramaniam S, Gilbert CE, Abdull MM, Imam AU. Coverage of Hospital-based Cataract Surgery and Barriers to the Uptake of Surgery among Cataract Blind Persons in Nigeria: The Nigeria National Blindness and Visual Impairment Survey. Ophthalmic Epidemiol. 2012;19:58–66. doi: 10.3109/09286586.2011.643271. [DOI] [PubMed] [Google Scholar]
- 10.Odugbo OP, Mpyet CD, Chiroma MR, Aboje AO. Cataract blindness, surgical coverage, outcomes, and barriers to uptake of cataract services in Plateau State, Nigeria. Middle East Afr J Ophthalmol. 2012;19:282–288. doi: 10.4103/0974-9233.97925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Syed A, Polack S, Eusebio C, Mathenge W, Wadud Z, Mamunur AKM, Foster A, Kuper H. Predictors of attendance and barriers to cataract surgery in Kenya, Bangladesh and the Philippines. Disabil Rehabil. 2013;35:1660–1667. doi: 10.3109/09638288.2012.748843. [DOI] [PubMed] [Google Scholar]
- 12.Kara-Jose N, Temporini ER. Cirurgia de catarata: o porque dos excluidos. Rev Panam Salud Publica. 1999;6:242–248. doi: 10.1590/s1020-49891999000900003. [DOI] [PubMed] [Google Scholar]
- 13.Rabiu MM. Cataract blindness and barriers to uptake of cataract surgery in a rural community of northern Nigeria. Br J Ophthalmol. 2001;85:776–780. doi: 10.1136/bjo.85.7.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melese M, Alemayehu W, Friedlander E, Courtright P. Indirect costs associated with accessing eye care services as a barrier to service use in Ethiopia. Trop Med Int Health. 2004;9:426–431. doi: 10.1111/j.1365-3156.2004.01205.x. [DOI] [PubMed] [Google Scholar]
- 15.Shrestha MK, Thakur J, Gurung CK, Joshi AB, Pokhrel S, Ruit S. Willingness to pay for cataract surgery in Kathmandu valley. Br J Ophthalmol. 2004;88:319–320. doi: 10.1136/bjo.2003.026260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mpyet C, Dineen BP, Solomon AW. Cataract surgical coverage and barriers to uptake of cataract surgery in leprosy villages of north eastern Nigeria. Br J Ophthalmol. 2005;89:936–938. doi: 10.1136/bjo.2004.062455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gyasi ME, Amoaku WMK, Asamany DK. Barriers to cataract surgical uptake in the upper east reagion of Ghana. Ghana Med J. 2007;41:167–170. doi: 10.4314/gmj.v41i4.55285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Athanasiov PA, Casson RJ, Newland HS, Shein WK, Muecke JS, Selva D, Aung T. Cataract surgical coverage and self-reported barriers to cataract surgery in a rural Myanmar population. Clin Experiment Ophthalmol. 2008;36:521–525. doi: 10.1111/j.1442-9071.2008.01829.x. [DOI] [PubMed] [Google Scholar]
- 19.De Senne FMB, Cardillo JA, Rocha EM, Kara-Jose N. Long-term visual outcomes in the Cataract-Free Zone Project in Brazil. Acta Ophthalmol Scand. 2002;80:262–266. doi: 10.1034/j.1600-0420.2002.800306.x. [DOI] [PubMed] [Google Scholar]
- 20.Walia T, Yorston D. Improving surgical outcomes. Community Eye Health. 2008;21:58–59. [PMC free article] [PubMed] [Google Scholar]
- 21.Thapa SS, Khanal S, Paudyal I, Twyana SN, Ruit S, van Rens GHMB. Outcomes of cataract surgery: a population-based developing world study in the Bhaktapur district, Nepal. Clin Experiment Ophthalmol. 2011;39:851–857. doi: 10.1111/j.1442-9071.2011.02576.x. [DOI] [PubMed] [Google Scholar]
- 22.Saw S, Tseng P, Chan W, Chan T, Ong S, Tan D. Visual function and outcomes after cataract surgery in a Singapore population. J Cataract Refract Surg. 2002;28:445. doi: 10.1016/s0886-3350(01)01016-1. [DOI] [PubMed] [Google Scholar]
- 23.Hashemi H, Mohammadi S, Z-Mehrjardi H, Majdi M, Ashrafi E, Mehravaran S, Mazouri A, Roohipoor R, KhabazKhoob M. The Role of Demographic Characteristics in the Outcomes of Cataract Surgery and Gender Roles in the Uptake of Postoperative Eye Care: A Hospital-based Study. Ophthalmic Epidemiol. 2012;19:242–248. doi: 10.3109/09286586.2012.691600. [DOI] [PubMed] [Google Scholar]
- 24.Nangia V, Jonas JB, Gupta R, Khare A, Sinha A. Prevalence of cataract surgery and postoperative visual outcome in rural central India. J Cataract Refract Surg. 2011;37:1932–1938. doi: 10.1016/j.jcrs.2011.08.020. [DOI] [PubMed] [Google Scholar]
- 25.http://whqlibdoc.who.int/hq/1998/WHO_PBL_98.68.pdf on 01/15/2014
- 26.Monestam E, Wachtmeister L. Dissatisfaction with cataract surgery in relation to visual results in a population-based study in Sweden. J Cataract Refract Surg. 1999;25:1127–1134. doi: 10.1016/s0886-3350(99)00135-2. [DOI] [PubMed] [Google Scholar]
- 27.Kara-Jose N, Contreras F, Campos MA, Delgado AM, Mowery RL, Ellwein LB. Screening and surgical intervention results from cataract-free-zone projects in Campinas, Brazil and Chimbote, Peru. Int Ophthalmol. 1990;14:155–164. doi: 10.1007/BF00158313. [DOI] [PubMed] [Google Scholar]
- 28.Lavanya R, Wong TY, Aung T, Tan DTH, Saw S, Tay WT, Wang JJ. Prevalence of cataract surgery and post-surgical visual outcomes in an urban Asian population: the Singapore Malay Eye Study. Br J Ophthalmol. 2009;93:299–304. doi: 10.1136/bjo.2008.148650. [DOI] [PubMed] [Google Scholar]
- 29.Lundstrom M, Barry P, Leite E, Seward H, Stenevi U. 1998 European Cataract Outcome Study Report from the European Cataract Outcome Study Group. J Cataract Refract Surg. 2001;27:1176–1184. doi: 10.1016/s0886-3350(01)00772-6. [DOI] [PubMed] [Google Scholar]
- 30.Lundstrom M, Barry P, Henry Y. Visual outcome of cataract surgery; Study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery. J Cataract Refract Surg. 2013;39:673–679. doi: 10.1016/j.jcrs.2012.11.026. [DOI] [PubMed] [Google Scholar]
- 31.Schellini SA, Durkin SR, Hoyama E, Hirai F, Cordeiro R, Casson RJ, Selva D, Padovani CR. BMC Ophthalmol. 2009;9:8. doi: 10.1186/1471-2415-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caligaris LS, Medina NH, Lansingh VC, et al. Analyses of cataract surgery performed by unified health system in Brazil, 2006-2007. Rev Panam Salud Publica. 2011;29:428–432. doi: 10.1590/s1020-49892011000600008. [DOI] [PubMed] [Google Scholar]


