Abstract
Purpose
To estimate the prevalence, potential determinants, and proportion of met need for near vision impairment (NVI) correctable with refraction approximately 2 years after initial examination of a multi-country cohort.
Design
Population-based, prospective cohort study.
Participants
People aged ≥35 years examined at baseline in semi-rural (Shunyi) and urban (Guangzhou) sites in China; rural sites in Nepal (Kaski), India (Madurai), and Niger (Dosso); a semi-urban site (Durban) in South Africa; and an urban site (Los Angeles) in the United States.
Methods
Near visual acuity (NVA) with and without current near correction was measured at 40 cm using a logarithm of the minimum angle of resolution near vision tumbling E chart. Participants with uncorrected binocular NVA ≤20/40 were tested with plus sphere lenses to obtain best-corrected binocular NVA.
Main Outcome Measures
Prevalence of total NVI (defined as uncorrected NVA ≤20/40) and NVI correctable and uncorrectable to >20/40, and current spectacle wearing among those with bilateral NVA ≤20/63 improving to >20/40 with near correction (met need).
Results
Among 13 671 baseline participants, 10 533 (77.2%) attended the follow-up examination. The prevalence of correctable NVI increased with age from 35 to 50–60 years and then decreased at all sites. Multiple logistic regression modeling suggested that correctable NVI was not associated with gender at any site, whereas more educated persons aged >54 years were associated with a higher prevalence of correctable NVI in Nepal and India. Although near vision spectacles were provided free at baseline, wear among those who could benefit was <40% at all but 2 centers (Guangzhou and Los Angeles).
Conclusions
Prevalence of correctable NVI is greatest among persons of working age, and rates of correction are low in many settings, suggesting that strategies targeting the workplace may be needed.
Although yet to be included in the Global Vision 2020 initiative,1 the most common cause of near vision impairment (NVI) in middle-aged and elderly populations is presbyopia,2 an age-related and progressive loss of accommodation. It is believed that loss of accommodative amplitude begins early in life, is greatest between 40 and 48 years, and is almost complete by age 50 to 55 years.3 Near vision impairment, the most common symptom of presbyopia, can be safely and effectively treated with presbyopic convex lenses.
Studies in a number of settings have suggested that a high proportion of near vision may go uncorrected in areas of limited resources.4–8 A significant burden of impaired visual function has been reported to be associated with uncorrected NVI, including greater difficulty with activities of daily living and diminished accomplishment due to vision, even when adjusting for age, gender, and distance vision.6
In 2008 and 2009, we conducted a multi-country study to evaluate the prevalence of NVI using a standardized protocol among people aged.≥35 years in 7 study sites located in China, Nepal, India, South Africa, Niger, and the United States. In this study, we found that the majority of participants developed NVI by the age of 50 years, with apparently relatively early onset in Indian and South African populations.9 Convex presbyopic lenses were provided free of charge to those in need of them.
As with impaired distance vision, not all NVI is correctable. Vision in people with media opacities, such as cataract and corneal diseases or retinal disorders, is often not correctable to normal vision with refraction alone. To more accurately project the need for near-vision spectacles, it is useful to distinguish between those with correctable and uncorrectable NVI. The purpose of the current study was to better understand the age distribution of spectacle-correctable and uncorrectable NVI, and near-vision spectacle wear among those with correctable NVI (met need) among persons aged >35 years in a multi-center, multiethnic, population-based cohort reexamined approximately 2 years after initial assessment.
Methods
Study Sites and Sampling
The study sites and sampling methods used in the baseline MultiCountry Study of Presbyopia have been described.9 In brief, the study was conducted at 7 sites in 6 countries: 1 urban site (Guangzhou) and 1 semi-rural site (Shunyi) in China; 1 rural site (Kaski) in Nepal; 1 rural site (Madurai District) in India; 1 semiurban site (Durban) in South Africa; 1 semi-urban site (Dosso) in Niger; and 1 urban site (Los Angeles) in the United States. Study participants were identified using random cluster sampling, except in Los Angeles where the study cohort was drawn from the previously identified Los Angeles Latino Eye Study cohort.10
Re-contact for Follow-up Examination
An attempt was made to re-contact all of the study participants who attended the baseline examination and invite them to participate in the follow-up study by phone (Guangzhou, Los Angeles) or door-to-door visits (Shunyi, Kaski, Madurai, Durban, Dosso). Those contacted were categorized as accepting or refusing the follow-up examination, or confirmed as being deceased or having moved out of the area according to information from other household members or community informants.
Eye Examination
Follow-up examinations took place at local clinics and other community facilities, depending on the field setting, after informed consent was obtained. The identity of the participant was confirmed on the basis of name, age (birthday), gender, and an identity card if available. Eye examinations were carried out according to the same protocol as that used at baseline, but with no baseline examination information provided to the follow-up examination team.
Binocular near visual acuity (NVA), both with and without correction (where available), was measured at 40 cm using a logarithm of the minimum angle of resolution near vision tumbling E chart (Precision Vision, La Salle, IL) under ambient light conditions. In Dosso, visual acuity was measured outdoors in sunlight because of a lack of reliable indoor lighting. The visual acuity was recorded as the smallest line read with 1 or no errors. Subjects with uncorrected binocular NVA ≤20/40 underwent binocular refraction at 40 cm, with best-corrected NVA obtained by testing with spherical lenses of increasing plus power.
Participants were asked to bring any currently used spectacles with them to the examination site, where the presence or absence of near and distance correction was recorded. At baseline, those with uncorrected NVA ≤20/63 that could be improved by ≥2 lines were given free spectacles (e.g., convex presbyopic lenses), unless they were already wearing an appropriate correction, or were referred to the closest eye care center for further examination and management if presenting with binocular distance visual acuity ≤20/40. An exception to this protocol is that free spectacles were not given in Guangzhou and Los Angeles, because spectacle use was already high among those in need. In Shunyi, Kaski, Madurai, and Dosso, participants also were interviewed as to whether they ever had spectacles (including those given during the baseline examination) and whether they wore them. The total number of persons bringing spectacles to the follow-up examination and for participants in Shunyi, Kaski, Madurai, and Dosso those reporting use of spectacles was tabulated. Reasons for not wearing spectacles among those with correctable NVI were not solicited.
Approval for the follow-up survey was obtained from the responsible institutional review board/ethics committee at each study site. Approval of the protocol was also provided by the World Health Organization Secretariat Committee on Research Involving Human Subjects. The study adhered to the tenets of the World Medical Association’s Declaration of Helsinki. Written, informed consent was obtained from all participants.
Definitions
The NVI was defined as uncorrected bilateral NVA ≤20/40. The NVI was subdivided into correctable NVI if best-corrected bilateral NVA was >20/40 or uncorrectable if it was ≤20/40. For the purposes of assessing met need among persons with correctable NVI, only persons with bilateral NVA ≤20/63 whose bilateral NVA could be improved to >20/40 with spectacles were considered as requiring near correction. (i.e., those with bilateral NVA 20/40 or 20/50 were not included among those considered as needing correction).
Data Management and Statistical Methods
Computerized data entry was carried out at each site using standardized programs. Data ranges, frequency distributions, and consistency among related measurements were checked with a series of data-cleaning programs.
Crude and age- and sex-standardized prevalence rates of total NVI, correctable NVI, and uncorrectable NVI were calculated separately in the follow-up cohort. The prevalence of NVI, correctable NVI, and uncorrectable NVI was graphed as a function of age for each site using local linear smoothed (Lowess) plots. The Lowess procedure imputes smoothed values for age-specific rates using a locally weighted regression of the prevalence of visual impairment on age. The association of age, gender, and educational level with correctable NVI was investigated with multiple logistic regression.
The met need for near vision correction among persons with bilateral NVA ≤20/63 correctable to >20/40 was defined as the proportion of such persons wearing any near vision spectacles at the follow-up examination.
All statistical analyses were performed using Stata/SE Statistical Software: Release 9.0 (StataCorp LP, College Station, TX). Confidence intervals (CIs) and P values (significant at the P ≤0.05 level) were calculated with adjustment for the clustering effects associated with the cluster sampling design.
Results
Among the 13 671 participants who were examined across the 7 study sites at baseline, 10553 (77.2%) were present at the followup examination (Table 1). The average interval between baseline and follow-up ranged from 27 to 32 months at the different sites. Follow-up response rates ranged from 87.7% in Guangzhou and 87.5% in Madurai to 57.5% in Durban and 57.2% in Los Angeles.
Table 1.
Baseline Examined and Follow-up Examined Participants by Gender, Baseline Age, and Education
| Gender
|
Baseline Age (Yrs)
|
Education
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 35–49 | 50–64 | 65–79 | 80+ | None | Less than Primary | Primary | Secondary | High School or More | No Information | All | |
| Shunyi | |||||||||||||
| Baseline* | 1103 | 1317 | 783 | 1088 | 472 | 77 | 357 | 153 | 441 | 1206 | 261 | 2 | 2420 |
| Follow-up | 889 | 1114 | 663 | 937 | 364 | 39 | 248 | 121 | 369 | 1036 | 228 | 1 | 2003 |
| % Examined at FU | 80.6 | 84.6 | 84.7 | 86.1 | 77.1 | 50.7 | 69.5 | 79.1 | 83.7 | 85.9 | 87.4 | 50.0 | 82.8 |
| Guangzhou | |||||||||||||
| Baseline | 836 | 981 | 803 | 645 | 292 | 77 | 30 | 64 | 134 | 388 | 1113 | 88 | 1817 |
| Follow-up | 720 | 874 | 694 | 590 | 256 | 54 | 25 | 57 | 126 | 344 | 973 | 69 | 1594 |
| % Examined at FU | 86.1 | 89.1 | 86.4 | 91.5 | 87.7 | 70.1 | 83.3 | 89.1 | 94.0 | 88.7 | 87.4 | 78.4 | 87.7 |
| Kaski | |||||||||||||
| Baseline | 810 | 1347 | 860 | 766 | 437 | 94 | 1396 | 179 | 262 | 79 | 217 | 24 | 2157 |
| Follow-up | 605 | 1057 | 636 | 638 | 337 | 51 | 1071 | 144 | 207 | 57 | 166 | 17 | 1662 |
| % Examined at FU | 74.7 | 78.5 | 74.0 | 83.3 | 77.1 | 54.3 | 76.7 | 80.5 | 79.0 | 72.2 | 76.5 | 70.8 | 77.1 |
| Madurai | |||||||||||||
| Baseline | 1068 | 1562 | 1334 | 819 | 425 | 52 | 1262 | 478 | 467 | 278 | 143 | 2 | 2630 |
| Follow-up | 914 | 1388 | 1224 | 724 | 327 | 27 | 1096 | 408 | 419 | 251 | 128 | 0 | 2302 |
| % Examined at FU | 85.6 | 88.9 | 91.8 | 88.4 | 77.0 | 51.9 | 86.9 | 85.4 | 89.7 | 90.3 | 89.5 | 0.0 | 87.5 |
| Durban | |||||||||||||
| Baseline | 483 | 1456 | 836 | 776 | 293 | 34 | 111 | 645 | 513 | 251 | 144 | 275 | 1939 |
| Follow-up | 250 | 865 | 451 | 473 | 170 | 21 | 57 | 403 | 291 | 163 | 80 | 121 | 1115 |
| % Examined at FU | 51.8 | 59.4 | 54.0 | 61.0 | 58.0 | 61.8 | 51.4 | 62.5 | 56.7 | 64.9 | 55.6 | 44.0 | 57.5 |
| Dosso | |||||||||||||
| Baseline | 771 | 1274 | 1141 | 594 | 241 | 69 | 1352 | 231 | 210 | 171 | 74 | 7 | 2045 |
| Follow-up | 545 | 953 | 822 | 463 | 172 | 41 | 1008 | 168 | 160 | 112 | 46 | 4 | 1498 |
| % Examined at FU | 70.7 | 74.8 | 72.0 | 78.0 | 71.4 | 59.4 | 74.6 | 72.7 | 76.2 | 65.5 | 62.2 | 57.1 | 73.3 |
| Los Angeles | |||||||||||||
| Baseline | 232 | 431 | 192 | 273 | 168 | 30 | 22 | 111 | 152 | 109 | 250 | 19 | 663 |
| Follow-up | 136 | 243 | 103 | 152 | 109 | 15 | 9 | 60 | 92 | 61 | 149 | 8 | 379 |
| % Examined at FU | 58.6 | 56.4 | 53.7 | 55.7 | 64.9 | 50.0 | 40.9 | 54.1 | 60.5 | 56.0 | 59.6 | 42.1 | 57.2 |
| All Sites | |||||||||||||
| Baseline | 5303 | 8368 | 5949 | 4961 | 2328 | 433 | 4530 | 1861 | 2179 | 2482 | 2202 | 417 | 13,671 |
| Follow-up | 4059 | 6494 | 4593 | 3977 | 1735 | 248 | 3514 | 1361 | 1664 | 2024 | 1770 | 220 | 10,553 |
| % Examined at FU | 76.5 | 77.6 | 77.2 | 80.2 | 74.5 | 57.3 | 77.6 | 73.1 | 76.4 | 81.6 | 80.4 | 52.8 | 77.2 |
FU = follow-up.
Does not include 2 clusters (with 1134 baseline participants) that were not part of the follow-up study.
In multiple regression modeling for each site, better follow-up response was associated with the following: female gender in Shunyi (odds ratio [OR], 1.48; 95% CI, 1.33–1.64; P < 0.001), Guangzhou (OR, 1.32; 95% CI, 1.08–1.62; P = 0.013), and Durban (OR, 1.46; 95% CI, 1.14–1.87; P = 0.005); younger age in Madurai (OR, 0.96; 95% CI, 0.95–0.97; P < 0.001) and older age in Durban (OR, 1.01; 95% CI, 1.00–1.02; P = 0.035); and a higher education level in Shunyi (OR, 1.34; 95% CI, 1.24–1.45; P < 0.001) and a lower education level in Dosso (OR, 0.90; 95% CI, 0.81–1.00; P = 0.051).
For each of the 7 study sites, the age-specific prevalence of correctable and uncorrectable NVI is shown in Figure 1. Correctable NVI, representing NVI due to refractive causes (presbyopia), increases steadily from 40 years until a maximum prevalence of approximately 80% by 55 years of age at most sites, after which it declines with age, markedly at some sites. Uncorrectable NVI, representing the age-related onset of nonrefractive causes of vision impairment (e.g., cataract, corneal and retinal diseases), increases steadily from age 55 to 60 years onward, although this increase is least pronounced in Los Angeles, Durban, and Madurai.
Figure 1.
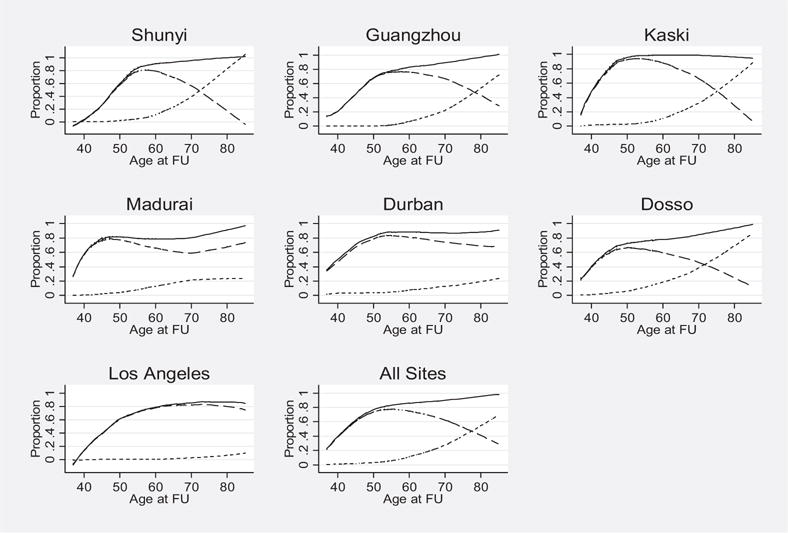
Lowess smoothed age-specific prevalence of NVI ≤20/40 (solid curve), correctable NVI (large dashes), and uncorrectable NVI (fine dashes) by study site in participants examined at follow-up in 7 study sites. FU = follow-up.
The associations among age, gender, and educational level with correctable NVI are reported separately in the ≤54- and ≥55-year age groups in Table 2, given the different age-related trends of correctable NVI in these 2 cohorts. Correctable NVI increased significantly with age in the ≤54-year age group and decreased with age in those aged ≥55 years, consistently at all sites. Correctable NVI was not associated with gender, except in Madurai where it was lower among female subjects in the ≤54–year age group. Lower educational level was significantly associated with a higher prevalence of correctable NVI in the ≤54-year age group in Durban and a higher education level with more correctable NVI in the ≥55-year age group in Kaski and Madurai.
Table 2.
Association of Age, Gender, and Education with Correctable Near Vision Impairment Stratified by Age
| Population Aged ≤54 Yrs
|
Population Aged ≥55 Yrs
|
|||||
|---|---|---|---|---|---|---|
| Study Site | N* Age (Yrs) | Female Gender | Education Level | N* Age (Yrs) | Female Gender | Education Level |
| Shunyi | 904 1.45 (1.31–1.61) | 1.70 (0.91–3.18) | 0.94 (0.61–1.46) | 1098 0.89 (0.84–0.94) | 0.94 (0.69–1.29) | 1.21 (0.98–1.50) |
| P < 0.001 | P – 0.082 | P – 0.753 | P = 0.003 | P – 0.661 | P – 0.069 | |
| Guangzhou | 811 1.27 (1.18–1.35) | 1.24 (0.90–1.71f) | 1.10 (0.92–1.31) | 714 0.95 (0.92–0.97) | 0.77 (0.56–1.05) | 1.06 (0.79–1.43) |
| P < 0.001 | P – 0.164 | P – 0.276 | P = 0.001 | P – 0.090 | P – 0.660 | |
| Kaski | 778 1.43 (1.32–1.54) | 1.42 (0.82–2.44) | 0.93 (0.81–1.05) | 867 0.86 (0.84–0.88) | 0.87 (0.58–1.29) | 1.28 (1.05–1.55) |
| P < 0.001 | P – 0.198 | P – 0.204 | P< 0.001 | P – 0.464 | P = 0.018 | |
| Madurai | 1365 1.13 (1.10–1.16) | 0.71 (0.54–0.93) | 1.03 (0.95–1.13) | 937 0.99 (0.97–1.01) | 1.12 (0.93–1.37) | 1.19 (1.05–1.33) |
| P < 0.001 | P = 0.015 | P – 0.433 | P – 0.396 | P – 0.224 | P = 0.007 | |
| Durban | 491 1.16 (1.11–1.21) | 1.34 (0.80–2.25) | 0.68 (0.56–0.83) | 503 0.95 (0.92–0.98) | 1.04 (0.55–1.97) | 1.08 (0.87–1.34) |
| P < 0.001 | P – 0.248 | P = 0.004 | P = 0.002 | P – 0.894 | P – 0.492 | |
| Dosso | 971 1.15 (1.12–1.18) | 1.9 (0.83–1.71) | 1.06 (0.92–1.22) | 523 0.94 (0.92–0.97) | 1.32 (0.84–2.08) | 1.11 (0.93–1.32) |
| P < 0.001 | P – 0.324 | P – 0.420 | P< 0.001 | P – 0.213 | P – 0.235 | |
| Los | 124 1.31 (1.14–1.49) | 3.74 (0.98–14.2) | 0.79 (0.51–1.23) | 247 0.99 (0.96–1.01) | 1.41 (0.62–3.22) | 1.06 (0.81–1.40) |
| Angeles | P = 0.006 | P – 0.052 | P – 0.217 | P – 0.201 | P – 0.311 | P – 0.536 |
| All Sites† | 5444 1.22 (1.20–1.25) | 1.15 (0.99–1.34) | 0.98 (0.92–1.03) | 4889 0.93 (0.92–0.94) | 1.02 (0.91–1.16) | 1.21 (1.13–1.29) |
| P < 0.001 | P – 0.066 | P – 0.382 | P< 0.001 | P – 0.690 | P< 0.001 | |
Data are given as ORs (95% CI). Bold values indicate a significant difference at the P < 0.050 level.
Number of participants included in the multiple logistic regression (corresponding to the number with education data).
Site was included as a covariate in the multiple logistic regression with data from all 7 study sites.
Uncorrectable NVI in the ≥55-year age group increased with older age at all sites, among female subjects in Dosso, and among those with less education in Shunyi, Guangzhou, Kaski, and Madurai (Table 3). Among those aged ≤54 years, uncorrectable NVI was associated with older age in Madurai (OR, 1.20; 95% CI, 1.12–1.30; P < 0.001) and Dosso (OR, 1.18; 95% CI, 1.10–1.26; P < 0.001), but was unassociated with gender or education at any site.
Table 3.
Association of Age, Gender, and Education with Near Vision Impairment Not Correctable with Refraction (Uncorrectable Near Vision Impairment) for People Aged ≥55 Years
| Population Aged≥55 Yrs
|
||||
|---|---|---|---|---|
| Study Site | N* | Age (Yrs) | Female Gender | Education Level |
| Shunyi | 1098 | 1.18 (1.11–1.25) P < 0.001 | 1.16 (0.68–2.00) P = 0.521 | 0.71 (0.53-0.95) P = 0.029 |
| Guangzhou | 714 | 1.16 (1.13–1.20) P < 0.001 | 1.57 (0.92–2.69) P = 0.091 | 0.66 (0.50–0.87) P = 0.008 |
| Kaski | 867 | 1.16 (1.14–1.18) P < 0.001 | 1.20 (0.79–1.85) P = 0.373 | 0.77 (0.63–0.95) P = 0.019 |
| Madurai | 937 | 1.05 (1.02–1.08) P = 0.003 | 1.07 (0.74–1.53) P = 0.724 | 0.76 (0.63–0.92) P = 0.007 |
| Durban | 503 | 1.08 (1.04–1.12) P < 0.001 | 1.42 (0.62–3.22) P = 0.387 | 0.75 (0.53–1.04) P = 0.084 |
| Dosso | 523 | 1.13 (1.09–1.16) P < 0.001 | 1.68 (1.01–2.79) P = 0.045 | 0.89 (0.68–1.15) P = 0.352 |
| Los Angeles | 247 | 1.13 (1.01–1.28) P = 0.044 | 0.57 (0.20–1.60) P = 0.203 | 1.25 (0.34–4.50) P = 0.660 |
| All Sites† | 4889 | 1.13 (1.12–1.14) P < 0.001 | 1.23 (1.03–1.46) P = 0.020 | 0.70 (0.64–0.76) P < 0.001 |
Data are given as ORs (95% CI). Bold values indicate a significant difference at the P < 0.050 level.
Number of participants included in the multiple logistic regression (corresponding to the number with education data).
Site was included as a covariate in the multiple logistic regression with data from all 7 study sites.
The met need for near vision correction among persons with bilateral NVA <20/63 correctable with spectacles to >20/40 was <40% at all but 2 centers (Los Angeles and Guangzhou) and was lower in several cases (Table 4).
Table 4.
Observed and Reported Spectacle Use in Those with Near Vision ≤20/63 Improving to >20/40 with Refraction
| Study Site | Total No. | No. (%) Wearing Spectacles at the Time of Examination | No. (%) Including Those Reporting Spectacles Use* |
|---|---|---|---|
| Shunyi | 607 | 4 (0.66) | 211 (34.8) |
| Guangzhou | 459 | 321 (69.9) | – |
| Kaski | 942 | 122 (13.0) | 279 (29.6) |
| Madurai | 937 | 175 (18.7) | 214 (22.8) |
| Durban | 425 | 170 (40.0) | – |
| Dosso | 144 | 23 (16.0) | 24 (16.7) |
| Los Angeles | 147 | 141 (95.9) | – |
Includes those wearing spectacles at the time of the examination and those not bringing glasses to the follow-up examination but reporting that they had glasses and were using them.
Discussion
This study provides, for the first time to the best of our knowledge, prevalence data on NVI in multiple ethnic groups in whom correctable and uncorrectable impairment are distinguished. These data demonstrate that correctable NVI (due to refractive causes) mostly affects people of working age, increasing from a low prevalence at 35 years to a peak at 55 years and decreasing afterward because of the onset of uncorrectable age-related ocular diseases. Although previous population-based studies5–7 have identified older age as a risk factor for presbyopia, this peak and subsequent decline have generally not been identified.
It is useful and important when assessing the prevalence of NVI to distinguish clearly between correctable and uncorrectable impairment. The former, which also has been referred to in the past as “functional presbyopia,”4,11 indicates an isolated NVI reversible with refractive correction, whereas the latter likely reflects impairment at both near and distance uncorrectable with spectacles and due to cataract or other ocular comorbidities. The health care resources required to manage these 2 entities differ significantly. The high incidence of this readily manageable condition in the critical working-age population across sites in our study combined with low observed rates of successful treatment highlight the widespread need for targeted programs to reduce the burden of uncorrected presbyopia.
Although a similar inverse U pattern for correctable NVI was consistently found across sites, we did observe some variation. The prevalence rates of correctable NVI were higher among younger cohorts in the Kaski, Madurai, Durban, and Dosso cohorts, suggesting an earlier onset of presbyopia in subcontinental and African populations. Although data on behavioral and environmental factors affecting refractive error were not collected in this study, given the fact that the prevalence of correctable NVI in Chinese centers in Shunyi and Guangzhou was similar despite a semi-rural environment in the former and an urban one in the latter, and that education was not consistently associated with correctable NVI in the 35- to 54-year age group, the observed earlier high prevalence of correctable NVI in the subcontinent and Africa may more likely be due to ethnic variation than environmental differences.
Early onset and higher prevalence of presbyopia among woman have been reported in some studies,5,7,12,13 although this finding is not consistent. Our study suggests that gender is not a risk factor for correctable NVI among younger or older age groups. A recent meta–analysis14 has suggested that although there may be a weak association between presbyopia and female sex, this is unlikely due to physiologic differences in accommodation because accommodative amplitude does not differ between men and women.
In common with previous studies,4–8 the current study found the rate of met need among persons who could benefit from near correction was low at most centers, and generally very low in rural areas. Guangzhou and Los Angeles were exceptions to these low rates of wear, the former suggesting that widespread access to near correction is available in at least some urban areas in the developing world. The fact that the Shunyi site, also in China, had the lowest observed rates of wear suggests that provision of near refractive services for all remains a challenge there as in many other parts of the world. Reports of diminished visual function among even rural persons without needed presbyopic correction6 underscore the need for comprehensive eye care services that target this problem.
Study Strengths and Limitations
The results and implications of this study must be understood in the context of its strengths and limitations. Strengths include the population-based design and the use of a standard protocol across multiple sites involving several different ethnicities. Limitations include the fact that, for pragmatic reasons, some measurements were not performed strictly according to the prescribed protocol, such as in the necessity of testing near vision outdoors in Dosso because of the irregular availability of electricity. Because of the lack of full distance refraction, our protocol would tend to have misclassified persons with astigmatism as having uncorrectable rather than correctable NVI. This problem also meant that the amplitude of accommodation loss was not objectively measured. Some people with low or moderate myopia may develop objective presbyopia (loss of accommodation) but never have NVI. With regard to our assessment of met need among those with correctable NVI, we counted persons who owned glasses that they did not bring to the examination site as being uncorrected, which may in some cases have led to overestimates of the unmet need. This tendency may have been exacerbated by suboptimal communication of the requirement to bring glasses to the examination site at some centers. Finally, our protocol did not allow for an investigation of causes for not wearing near spectacles among those needing them because of difficulties in creating a standard list of potential reasons relevant to all 7 sites.
In conclusion, this multi–country, population-based study underscores the high prevalence of unmet need for near vision correction, most strikingly in the economically important population of working-aged persons. These results highlight the need for programs to reduce the burden of diminished visual function resulting from one of the most common ocular morbidities in the world.
Acknowledgments
Funding: Supported by the World Health Organization, Geneva, Switzerland (under National Institutes of Health, Bethesda, MD, contract No. N01-EY-2103).
Footnotes
Financial Disclosure(s):
The author(s) have no proprietary or commercial interest in any materials discussed in this article.
References
- 1.Pararajasegaram R. VISION 2020-the Right to Sight: from strategies to action. Am J Ophthalmol. 1999;128:359–60. doi: 10.1016/s0002-9394(99)00251-2. [DOI] [PubMed] [Google Scholar]
- 2.Holden BA, Fricke TR, Ho SM, et al. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008;126:1731–9. doi: 10.1001/archopht.126.12.1731. [DOI] [PubMed] [Google Scholar]
- 3.Glasser A, Kaufman PL. Accommodation and presbyopia. In: Kaufman PL, Alm A, editors. Adler’s Physiology of the Eye: Clinical Application. 10th. St. Louis, MO: Mosby; 2002. pp. 197–233. [Google Scholar]
- 4.Sherwin JC, Keeffe JE, Kuper H, et al. Functional presbyopia in a rural Kenyan population: the unmet presbyopic need. Clin Experiment Ophthalmol. 2008;36:245–51. doi: 10.1111/j.1442-9071.2008.01711.x. [DOI] [PubMed] [Google Scholar]
- 5.Nirmalan PK, Krishnaiah S, Shamanna BR, et al. A population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 2006;47:2324–8. doi: 10.1167/iovs.05-1192. [DOI] [PubMed] [Google Scholar]
- 6.Lu Q, He W, Murthy GV, et al. Presbyopia and near-vision impairment in rural northern China. Invest Ophthalmol Vis Sci. 2011;52:2300–5. doi: 10.1167/iovs.10-6569. [DOI] [PubMed] [Google Scholar]
- 7.Burke AG, Patel I, Munoz B, et al. Population-based study of presbyopia in rural Tanzania. Ophthalmology. 2006;113:723–7. doi: 10.1016/j.ophtha.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 8.Marmamula S, Keeffe JE, Rao GN. Uncorrected refractive errors, presbyopia and spectacle coverage: results from a rapid assessment of refractive error survey. Ophthalmic Epidemiol. 2009;16:269–74. [PubMed] [Google Scholar]
- 9.He M, Abdou A, Naidoo KS, et al. Prevalence and correction of near vision impairment at seven sites in China, India, Nepal, Niger, South Africa, and the United States. Am J Ophthalmol. 2012;154:107–16. doi: 10.1016/j.ajo.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 10.Varma R, Paz SH, Azen SP, et al. Los Angeles Latino Eye Study Group The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004;111:1121–31. doi: 10.1016/j.ophtha.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Lu Q, Congdon N, He X, et al. Quality of life and near vision impairment due to functional presbyopia among rural Chinese adults. Invest Ophthalmol Vis Sci. 2011;52:4118–23. doi: 10.1167/iovs.10-6353. [DOI] [PubMed] [Google Scholar]
- 12.Patel I, Munoz B, Burke AG, et al. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology. 2006;113:728–34. doi: 10.1016/j.ophtha.2006.01.028. [DOI] [PubMed] [Google Scholar]
- 13.Morny FK. Correlation between presbyopia, age and number of births of mothers in the Kumasi area of Ghana. Ophthalmic Physiol Opt. 1995;15:463–6. [PubMed] [Google Scholar]
- 14.Hickenbotham A, Roorda A, Steinmaus C, Glasser A. Metaanalysis of sex differences in presbyopia. Invest Ophthalmol Vis Sci. 2012;53:3215–20. doi: 10.1167/iovs.12-9791. [DOI] [PMC free article] [PubMed] [Google Scholar]


