Abstract
Background
Androgenetic alopecia (AGA) has a negative impact on self-image and decrease in quality of life. However, relatively few men have sought treatment for AGA. Improvement in treatment willingness is important for maintaining long-term management in patients with AGA.
Objectives
We aimed to identify the prevalence of patients' perception of hair loss and evaluate various factors that affect the treatment willingness in patients with AGA.
Methods
We conducted a population-based cross-sectional survey of 503 patients with AGA (329 men, 174 women). We collected the various demographic data, family history of AGA, history of past treatment, self-perception of hair loss and treatment willingness using structured questionnaires. Then, we provided the knowledge about AGA to the half of subjects and compared the treatment willingness between educated group and nond-educated group.
Results
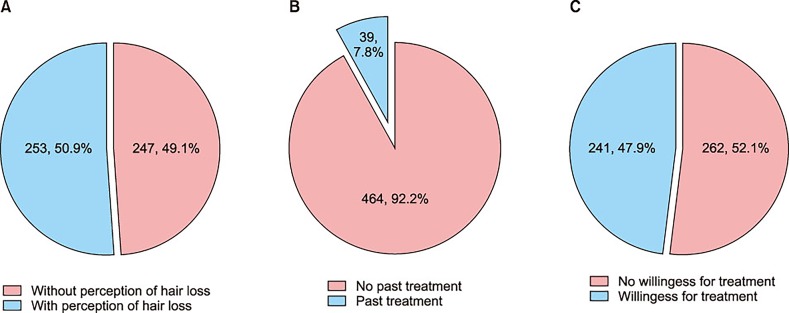
Two-hundred and forty-seven out of 503 patients (49.1%) did not have illness perception and 262 out of 503 patients (52.1%) did not have treatment willingness in future. The patients with perception of hair loss, accurate information on hair loss and severe hair loss showed 1.745-fold, 1.700-fold, and 2.078-fold higher tendency of receiving treatment in future.
Conclusion
Our findings imply that patients with perception and greater understanding of AGA tend to pursue treatment for AGA. Thus, these elements should be taken into account when treating patients. In addition, emphasis on education is needed to increase public awareness of the AGA.
Keywords: Alopecia, Education, Korean, Perception, Treatment willingness
INTRODUCTION
The hair plays a very important role in gender identification and acts as style item, a reference of beauty1,2,3,4. The voluminous hair thus means health and youthfulness and hair loss may adversely affect psychosocial status and quality of life (QOL). There are several previous studies on psychosocial consequences of androgenetic alopecia (AGA) in men and women 3,5,6,7,8,9,10,11,12. The perception of hair loss could be associated with psychologic stress and reduced the QOL. However, the illness perception is not exactly proportional to the degree of hair loss. Several patients of AGA did not recognize the hair loss until they were diagnosed as AGA at dermatologic clinic. This discrepancy between the patient's perception of hair loss and the clinical findings by physicians may be due to different individual's perception of hair loss. Some people considered AGA as normal aging process which might lead to indifference in treatment of hair loss. Although the number of AGA patients has increased, there are still quite few patients who has been treated properly and regularly by dermatologist. In addition, various nonmedical treatments for hair growth, such as herbal medicines, shampoos, and scalp massage have been increased13. Most nonmedical treatments showed temporary or little effect on hair growth, but the cost was similar or higher than those of medical treatments. The patients receiving improper treatment could obtain unsatisfactory results and eventually had no willingness for treatment in future.
Based on this concept, we investigated the current status of perception of hair loss by AGA patients and analyzed various factors associated with perception and treatment willingness in patients with AGA.
MATERIALS AND METHODS
This population-based cross-sectional survey included 503 patients with AGA (329 men, 174 women) who participated in a comprehensive health examination at the Department of Occupational and Environmental Medicine at Wonju Severance Christian Hospital between October 2012 and July 2015. We evaluated the hair status of each subject using visual inspection and included subjects who were diagnosed with AGA. We excluded persons with other types of alopecia or individuals with any condition influencing hair growth, such as fever, severe emotional stress, metabolic disease, or anticancer treatment. All participants signed an informed consent for study participation. The study protocol was approved by the Ethics Committee of the Yonsei Wonju College of Medicine (IRB no. YWMR-15-0-018).
Assessment of hair loss was performed by eight dermatology residents who had been trained in basic and specific (BASP) classification14. The severity of AGA was classified into mild, moderate and severe group using BASP classification. We categorized mild group as L, M0, C0, M1, C1, F1, V1 and moderate group as M2, C2, F2, V2 and severe group as M3, C3, F3, V3, U1~3. On odd days, we educate the patients about possible cause, diagnosing tools, treatment method and prognosis of AGA for 5 minutes using the education material developed by Korean Hair Research Society15. On the contrary, we did not educate the patients who visited the hospital on even days.
We collected information on various factors using structured questionnaires and medical records. The following data were obtained from eligible patients: sex, age, family history of AGA, patient's perception of hair loss, patient's willingness for treatment of AGA in future, history of past treatment for AGA, history of past treatment for other dermatological diseases, history of past treatment for medical co-morbidities including hypertension, diabetes mellitus, dyslipidemia, cardiovascular disease, and cerebrovascular disease. If patients were received the treatment for AGA in the past, we also collected the information on duration and modality of treatment.
We divided the subjects into two groups as follows: the patients who had no desire for treatment of AGA in future were categorized as ‘no willingness’ group and patients who have desire for treatment were categorized as ‘willingness’ group. We compared the distribution of various factors between no willingness group and willingness group.
Age was analyzed as a continuous variable and also analyzed as nominal variables using age group. Family history of AGA, patient's perception of hair loss, history of past treatment for AGA, history of past treatment for other dermatological diseases, history of past treatment for medical co-morbidities and education history about AGA were analyzed as binary (positive or negative) variables.
We used univariate logistic regression to evaluate associations between treatment willingness and the following factors: sex, age, family history of AGA, severity of AGA, patient's perception of hair loss, history of past treatment for AGA, history of past treatment for other dermatological diseases, history of past treatment for medical co-morbidities, and education history on AGA. The statistical significance level was set at 0.05 for each association. All odds ratios and their 95% confidence intervals (CIs) were computed. Statistical analyses were performed with IBM SPSS software ver. 22.0 for Windows (IBM Co., Armonk, NY, USA).
RESULTS
This study included 503 patients with AGA (329 men, 174 women). The mean age of male participants was 57.72 years and mean age of female participants was 62.68 years. Two-hundred and forty-one patients received the education about AGA before collecting the data and 262 patients did not receive the education.
Among 503 patients, 256 patients recognized the hair loss (50.9%; Fig. 1A) and 247 patients did not recognize the hair loss (49.1%; Fig. 1A). The number of patients with treatment desire in future (willingness group) was 241 (47.9%; Fig. 1B) and the number of patients without treatment desire (no willingness group) was 262 (52.1%; Fig. 1B). In the willingness group, most patients showed mild degree of AGA (n=195, 74.4%) and this was followed by moderate (n=45, 17.2%) and severe degree (n=22, 8.4%) (Table 1). The patients with moderate and severe degree of AGA showed 1.853-fold (95% CI, 1.193~2.877) and 2.078-fold (95% CI 1.166~3.704) higher tendency of receiving treatment in future than patients with mild degree of AGA (Table 2). Among 256 patients who recognized the hair loss, 140 patients showed willingness for treatment of AGA in future and 116 patients showed no willingness for treatment (Table 1). By logistic regression, the patients with self-perception of hair loss showed 1.745-fold (95% CI, 1.225~2.484) higher tendency of receiving treatment in future than patients without perception of alopecia (Table 2). Among 189 patients who had history of past treatment for medical co-morbidities, 104 patients showed willingness for treatment of AGA in future and 85 patients showed no willingness for treatment (Table 1). The patients with history of past treatment for medical co-morbidities showed 1.581-fold (95% CI, 1.099~2.273) higher tendency of receiving treatment in future than patients without history of medical co-morbidities (Table 2). Among 241 patients who received the education about AGA at their visit, 132 patients showed willingness for treatment of AGA in future and 109 patients showed no willingness for treatment (Table 1). The patients having information about AGA showed 1.700-fold (95% CI, 1.194~2.420) higher tendency of receiving treatment in future than patients without information (Table 2). There were no statistical differences in distribution of sex, age, family history of AGA, history of past treatment for AGA and other dermatological diseases between willingness group and no willingness group. We also investigated the reason for no willingness for treatment in no willingness group.
Fig. 1. Distribution of perception of alopecia, treatment history and treatment willingness. (A) Among 503 patients, 256 patients recognized the hair loss (50.9%) and 247 patients did not recognize the hair loss (49.1%). (B) The number of patients with treatment desire in future (willingness group) was 241 (47.9%) and the number of patients without treatment desire (no willingness group) was 262 (52.1%). (C) Among 503 patients, 39 patients (7.8%) had a past history of treatment for androgenetic alopecia.
Table 1. Comparison of clinical characteristics between willingness and no willingness group.
| Variable | No willingness group (n=262) | Willingness group (n=241) |
|---|---|---|
| Sex | ||
| Male | 174 (66.4) | 155 (64.3) |
| Female | 88 (33.6) | 86 (35.7) |
| Age (yr) | 58.84±12.44 | 59.95±12.18 |
| 20~29 | 4 (1.5) | 3 (1.2) |
| 30~39 | 15 (5.7) | 11 (4.6) |
| 40~49 | 37 (14.1) | 31 (12.9) |
| 50~59 | 68 (26.0) | 67 (27.8) |
| 60~69 | 82 (31.3) | 64 (26.6) |
| ≥70 | 56 (21.4) | 65 (27.0) |
| Family history of AGA | ||
| No | 180 (68.7) | 149 (61.8) |
| Yes | 82 (31.3) | 92 (38.2) |
| Severity of AGA | ||
| Mild | 195 (74.4) | 145 (60.2) |
| Moderate | 45 (17.2) | 62 (25.7) |
| Severe | 22 (8.4) | 34 (14.1) |
| Self-perception of hair loss | ||
| No | 146 (55.7) | 101 (41.9) |
| Yes | 116 (44.3) | 140 (58.1) |
| History of past treatment for AGA | ||
| No | 246 (93.9) | 218 (90.5) |
| Yes | 16 (6.1) | 23 (9.5) |
| History of past treatment for other dermatological diseases | ||
| No | 230 (87.8) | 210 (87.1) |
| Yes | 32 (12.2) | 31 (12.9) |
| History of past treatment for other medical diseases | ||
| No | 177 (67.6) | 137 (56.8) |
| Yes | 85 (32.4) | 104 (43.2) |
| Education about AGA | ||
| No | 153 (58.4) | 109 (45.2) |
| Yes | 109 (41.6) | 132 (54.8) |
Values are presented as number (%) or mean±standard deviation. AGA: androgenetic alopecia.
Table 2. Univariate analyses of the associations between willingness and no willingness group.
| Variable | OR (95% CI) | p-value |
|---|---|---|
| Age | 1.007 (0.993~1.022) | 0.311 |
| Sex | ||
| Male | 1 | 0.621 |
| Female | 1.097 (0.760~1.585) | |
| Family history of AGA | ||
| No | 1 | 0.106 |
| Yes | 1.355 (0.938~1.959) | |
| Severity of AGA | ||
| Mild | 1 | Mild-moderate 0.006*/Mild-severe 0.013* |
| Moderate | 1.853 (1.193~2.877) | |
| Severe | 2.078 (1.166~3.704) | |
| Self-perception of hair loss | ||
| No | 1 | 0.002* |
| Yes | 1.745 (1.225~2.484) | |
| History of past treatment for AGA | ||
| No | 1 | 0.153 |
| Yes | 1.622 (0.835~3.150) | |
| History of past treatment for other dermatological diseases | ||
| No | 1 | 0.826 |
| Yes | 1.061 (0.626~1.799) | |
| History of past treatment for other medical diseases | ||
| No | 1 | 0.013* |
| Yes | 1.581 (1.099~2.273) | |
| Education for AGA | ||
| No | 1 | 0.003* |
| Yes | 1.700 (1.194~2.420) |
OR: odd ratio, CI: confidence interval, AGA: androgenetic alopecia. *Asterisk indicates statistical significance.
Among 503 patients, 39 patients (7.8%) had a past history of treatment for AGA (Fig. 1C). The duration of past treatment was presented as follows: over 1 year (n=13, 33.3%), 4~6 months (n=12, 30.8%), 1~3 months (n=7, 17.9%), 6~12 months (n=4, 10.3%), less than 1 month (n=3, 7.7%).
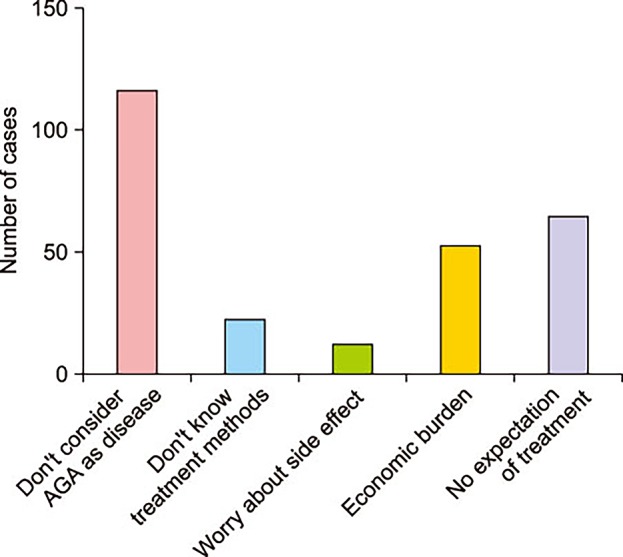
Among 262 patients who did not pursue treatment, 116 patients noted that they did not consider AGA as ‘treatable disease’. Sixty-three patients answered that treatment may not have effect on hair growth. Fifty-one patients did not want treatment because of economic burden. Twenty-one patients noted that they did not know the treatment methods and 11 patients worried about side effect (Fig. 2).
Fig. 2. Reasons for no willingness for treatment in no willingness group. Among 262 patients who did not pursue treatment, 116 patients noted that they did not consider androgenetic alopecia (AGA) as ‘treatable disease’. Sixty-three patients answered that treatment may not have effect on hair growth. Fifty-one patients did not want treatment because of economic burden. Twenty-one patients noted that they did not know the treatment methods and 11 patients worried about side effects.
DISCUSSION
AGA has a negative impact on self-image such as shame feeling and aging which leads to decrease in QOL 2,3,5,6,7,8,9,11,12,16,17,18,19,20,21,22,23,24,25. The previous studies revealed that decrease in the amount of hair was associated with increased perceptions of aging and decreased perceptions of attractiveness and aggressiveness2,3,6. Many studies have addressed the impact of AGA on QOL, but relatively little is known about the treatment willingness in patients with AGA. The illness perception could cause psychological distress and decrease in QOL in patients with AGA5,18,19,22,23. As with most chronic diseases, treatment willingness may play an important role for maintaining long-term management in patients with AGA26,27,28,29,30,31,32,33,34,35,36. Thus, we identified the portion of self-perceived patients and the factors that affect the treatment willingness in community-based patients with AGA. Our survey used community sampling to decrease the possible bias associated with effects of patients who visit dermatologic clinic for treatment.
We found that 247 out of 503 patients (49.1%) did not have illness perception and 262 out of 503 patients (52.1%) did not have treatment willingness (Fig. 1A, B). Despite the fact that AGA caused negative impact on QOL, we found that less than a half of subjects answered that they did not have treatment desire. The main reason for lack of treatment willingness was that they did not consider AGA as a treatable disease (116 out of 262 subjects [44.3%]; Fig. 2).
We found that perception of hair loss increased the treatment willingness in patients with AGA. In our study, 247 out of 503 patients of AGA (49.1%) could not recognize the hair loss until they were diagnosed as AGA at physical examination by physician (Fig. 1A). This discrepancy between the patient's perception of hair loss and the clinical findings by physicians may have various reasons including different individual's perception of hair loss8. The degree of hair loss is determined by objective methods such as physical examination by physicians and folliscope, whereas the perception of hair loss is mostly depends on patients' subjective feeling or perceived noticeability from others. We also found that the patients with perception of hair loss showed 1.75-fold higher tendency of receiving treatment in future than patients without perception (Table 2). Franzoi et al.8 reported that men with high public self-consciousness were more likely to perceive thinning hair and more willing to try treatment than low self-consciousness counterparts. Thus, self-perception of hair loss plays an import role on treatment willingness.
The severity of hair loss could affect the treatment willingness7. Our results suggested that men with severe hair loss are more likely to receive treatment in future. Although the perception is not exactly proportional to the degree of hair loss, we speculated that greater amount of hair loss raised the greater dissatisfaction leading to increase the treatment willingness.
We found that accurate knowledge about AGA had positive effect on the treatment willingness. In our study, educated subjects significantly showed 1.7-fold higher tendency of receiving treatment in future than non-educated subjects (Table 2). Similarly, Zeremski et al.37 found that treatment willingness was associated with previous attendance at an educational activity and a higher level of knowledge in patients with hepatitis C virus infection.
We also found that patients with history of past treatment for medical co-morbidities showed 1.58-fold higher tendency of receiving treatment than patients without history of medical co-morbidities. However, we did not find a relationship between history of past treatment for AGA and treatment willingness. This result may be due to the unsatisfactory results from improper past treatment of AGA. In our study, 63 out of 262 patients (24.0%) answered that treatment may not have effect on hair growth and 22 out of 39 previously treated patients (56.4%) received treatment for less than 6 months. We speculated that improper past treatment might cause a decrease in treatment desire. The gender may affect the treatment willingness. Although women are genetically less susceptible to AGA, women tend to be more sensitive in perceiving the hair loss possibly due to cultural and behavioral factors than men16,18,22. However, we found no difference in treatment willingness according to gender.
We identified the prevalence of patients' perception of hair loss and various factors that affect the treatment willingness though the population-based cross-sectional survey of 503 patients with AGA (329 men, 174 women). In this study, 247 out of 503 patients (49.1%) did not have illness perception and 262 out of 503 patients (52.1%) did not have treatment willingness in future. We found that patients' perception of hair loss, severe hair loss and accurate knowledge about AGA could increase the willingness to receive the treatment. The most important factor was patients' perception of hair loss. Interestingly, gender and past treatment history of AGA had no significant association with treatment willingness in this study. Due to limitation of the cross-sectional study, we cannot find the causal inferences between these factors and treatment willingness. Our findings imply that patients with perception of hair loss and accurate understanding of AGA could have more chance to receive treatment in future. Thus, these elements should be taken into account when treating patients to achieve the satisfactory treatment results. In addition, physicians should make more efforts to provide the accurate information about hair loss to the community members.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
References
- 1.Ayob SM, Messenger AG. Androgens, hair loss and eugenics: a tale of discovery and American social history. Exp Dermatol. 2015;24:412–413. doi: 10.1111/exd.12702. [DOI] [PubMed] [Google Scholar]
- 2.Muscarella F, Cunningham MR. The evolutionary significance and social perception of male pattern baldness and facial hair. Ethol Sociobiol. 1996;17:99–117. [Google Scholar]
- 3.Neave N, Shields K. The effects of facial hair manipulation on female perceptions of attractiveness, masculinity, and dominance in male faces. Pers Indiv Differ. 2008;45:373–377. [Google Scholar]
- 4.Lee WS, Lee HJ. Characteristics of androgenetic alopecia in asian. Ann Dermatol. 2012;24:243–252. doi: 10.5021/ad.2012.24.3.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmitt JV, Ribeiro CF, Souza FH, Siqueira EB, Bebber FR. Hair loss perception and symptoms of depression in female outpatients attending a general dermatology clinic. An Bras Dermatol. 2012;87:412–417. doi: 10.1590/s0365-05962012000300010. [DOI] [PubMed] [Google Scholar]
- 6.Lee HJ, Ha SJ, Kim D, Kim HO, Kim JW. Perception of men with androgenetic alopecia by women and nonbalding men in Korea: how the nonbald regard the bald. Int J Dermatol. 2002;41:867–869. doi: 10.1046/j.1365-4362.2002.01446.x. [DOI] [PubMed] [Google Scholar]
- 7.Girman CJ, Rhodes T, Lilly FR, Guo SS, Siervogel RM, Patrick DL, et al. Effects of self-perceived hair loss in a community sample of men. Dermatology. 1998;197:223–229. doi: 10.1159/000018001. [DOI] [PubMed] [Google Scholar]
- 8.Franzoi SL, Anderson J, Frommelt S. Individual differences in men's perceptions of and reactions to thinning hair. J Soc Psychol. 1990;130:209–218. doi: 10.1080/00224545.1990.9924571. [DOI] [PubMed] [Google Scholar]
- 9.Dixson BJ, Brooks RC. The role of facial hair in women's perceptions of men's attractiveness, health, masculinity and parenting abilities. Evol Hum Behav. 2013;34:236–241. [Google Scholar]
- 10.Chiang YZ, Bundy C, Griffiths CE, Paus R, Harries MJ. The role of beliefs: lessons from a pilot study on illness perception, psychological distress and quality of life in patients with primary cicatricial alopecia. Br J Dermatol. 2015;172:130–137. doi: 10.1111/bjd.13259. [DOI] [PubMed] [Google Scholar]
- 11.Cash TF. The psychosocial consequences of androgenetic alopecia: a review of the research literature. Br J Dermatol. 1999;141:398–405. doi: 10.1046/j.1365-2133.1999.03030.x. [DOI] [PubMed] [Google Scholar]
- 12.Alfonso M, Richter-Appelt H, Tosti A, Viera MS, García M. The psychosocial impact of hair loss among men: a multinational European study. Curr Med Res Opin. 2005;21:1829–1836. doi: 10.1185/030079905X61820. [DOI] [PubMed] [Google Scholar]
- 13.Olsen EA, Messenger AG, Shapiro J, Bergfeld WF, Hordinsky MK, Roberts JL, et al. Evaluation and treatment of male and female pattern hair loss. J Am Acad Dermatol. 2005;52:301–311. doi: 10.1016/j.jaad.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 14.Lee WS, Ro BI, Hong SP, Bak H, Sim WY, Kim DW, et al. A new classification of pattern hair loss that is universal for men and women: basic and specific (BASP) classification. J Am Acad Dermatol. 2007;57:37–46. doi: 10.1016/j.jaad.2006.12.029. [DOI] [PubMed] [Google Scholar]
- 15.Group KHRS. Diagnosis and treatment guideline of androgenetic alopecia [Internet] Wonju: The Korean Hair Research Society; 2011. Nov 06, [updated 2011 Dec 6]. [cited 2012 Aug 12]. Available from: http://www.khrs.or.kr/library/operation. [Google Scholar]
- 16.Robbins C, Mirmirani P, Messenger AG, Birch MP, Youngquist RS, Tamura M, et al. What women want - quantifying the perception of hair amount: an analysis of hair diameter and density changes with age in caucasian women. Br J Dermatol. 2012;167:324–332. doi: 10.1111/j.1365-2133.2012.11010.x. [DOI] [PubMed] [Google Scholar]
- 17.Wogalter MS, Hosie JA. Effects of cranial and facial hair on perceptions of age and person. J Soc Psychol. 1991;131:589–591. doi: 10.1080/00224545.1991.9713892. [DOI] [PubMed] [Google Scholar]
- 18.van der Donk J, Passchier J, Knegt-Junk C, van der Wegen-Keijser MH, Nieboer C, Stolz E, et al. Psychological characteristics of women with androgenetic alopecia: a controlled study. Br J Dermatol. 1991;125:248–252. doi: 10.1111/j.1365-2133.1991.tb14749.x. [DOI] [PubMed] [Google Scholar]
- 19.Van Der Donk J, Hunfeld JA, Passchier J, Knegt-Junk KJ, Nieboer C. Quality of life and maladjustment associated with hair loss in women with alopecia androgenetica. Soc Sci Med. 1994;38:159–163. doi: 10.1016/0277-9536(94)90311-5. [DOI] [PubMed] [Google Scholar]
- 20.Hunt N, McHale S. The psychological impact of alopecia. BMJ. 2005;331:951–953. doi: 10.1136/bmj.331.7522.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grimalt R. Psychological aspects of hair disease. J Cosmet Dermatol. 2005;4:142–147. doi: 10.1111/j.1473-2165.2005.40218.x. [DOI] [PubMed] [Google Scholar]
- 22.Cash TF, Price VH, Savin RC. Psychological effects of androgenetic alopecia on women: comparisons with balding men and with female control subjects. J Am Acad Dermatol. 1993;29:568–575. doi: 10.1016/0190-9622(93)70223-g. [DOI] [PubMed] [Google Scholar]
- 23.Cash TF. The psychological effects of androgenetic alopecia in men. J Am Acad Dermatol. 1992;26:926–931. doi: 10.1016/0190-9622(92)70134-2. [DOI] [PubMed] [Google Scholar]
- 24.Stough D, Stenn K, Haber R, Parsley WM, Vogel JE, Whiting DA, et al. Psychological effect, pathophysiology, and management of androgenetic alopecia in men. Mayo Clin Proc. 2005;80:1316–1322. doi: 10.4065/80.10.1316. [DOI] [PubMed] [Google Scholar]
- 25.Cartwright T, Endean N, Porter A. Illness perceptions, coping and quality of life in patients with alopecia. Br J Dermatol. 2009;160:1034–1039. doi: 10.1111/j.1365-2133.2008.09014.x. [DOI] [PubMed] [Google Scholar]
- 26.Warren RB, Kleyn CE, Gulliver WP. Cumulative life course impairment in psoriasis: patient perception of disease-related impairment throughout the life course. Br J Dermatol. 2011;164(Suppl 1):1–14. doi: 10.1111/j.1365-2133.2011.10280.x. [DOI] [PubMed] [Google Scholar]
- 27.Randell RL, Long MD, Martin CF, Sandler RS, Chen W, Anton K, et al. Patient perception of chronic illness care in a large inflammatory bowel disease cohort. Inflamm Bowel Dis. 2013;19:1428–1433. doi: 10.1097/MIB.0b013e3182813434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piana N, Battistini D, Urbani L, Romani G, Fatone C, Pazzagli C, et al. Multidisciplinary lifestyle intervention in the obese: its impact on patients' perception of the disease, food and physical exercise. Nutr Metab Cardiovasc Dis. 2013;23:337–343. doi: 10.1016/j.numecd.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 29.Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN. Awareness, perception, and knowledge of heart disease risk and prevention among women in the United States. American Heart Association Women's Heart Disease and Stroke Campaign Task Force. Arch Fam Med. 2000;9:506–515. doi: 10.1001/archfami.9.6.506. [DOI] [PubMed] [Google Scholar]
- 30.Metz U, Welke J, Esch T, Renneberg B, Braun V, Heintze C. Perception of stress and quality of life in overweight and obese people--implications for preventive consultancies in primary care. Med Sci Monit. 2009;15:PH1–PH6. [PubMed] [Google Scholar]
- 31.Linder D, Dall'olio E, Gisondi P, Berardesca E, Gennaro ED, Pennella AR, et al. Perception of disease and doctor-patient relationship experienced by patients with psoriasis: a questionnaire-based study. Am J Clin Dermatol. 2009;10:325–330. doi: 10.2165/11311190-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 32.Daudén E, Conejo J, García-Calvo C. [Physician and patient perception of disease severity, quality of life, and treatment satisfaction in psoriasis: an observational study in Spain] Actas Dermosifiliogr. 2011;102:270–276. doi: 10.1016/j.ad.2010.04.018. Spanish. [DOI] [PubMed] [Google Scholar]
- 33.Esteban y Peña MM, Hernandez Barrera V, Fernández Cordero X, Gil de Miguel A, Rodríguez Pérez M, Lopez-de Andres A, et al. Self-perception of health status, mental health and quality of life among adults with diabetes residing in a metropolitan area. Diabetes Metab. 2010;36:305–311. doi: 10.1016/j.diabet.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 34.Choi H, Park JY, Yeo JK, Oh MM, Moon du G, Lee JG, et al. Population-based survey on disease insight, quality of life, and health-seeking behavior associated with female urinary incontinence. Int Neurourol J. 2015;19:39–46. doi: 10.5213/inj.2015.19.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Litaker D, Mion L, Planavsky L, Kippes C, Mehta N, Frolkis J. Physician - nurse practitioner teams in chronic disease management: the impact on costs, clinical effectiveness, and patients' perception of care. J Interprof Care. 2003;17:223–237. doi: 10.1080/1356182031000122852. [DOI] [PubMed] [Google Scholar]
- 36.Le Grande MR, Elliott PC, Worcester MU, Murphy BM, Goble AJ, Kugathasan V, et al. Identifying illness perception schemata and their association with depression and quality of life in cardiac patients. Psychol Health Med. 2012;17:709–722. doi: 10.1080/13548506.2012.661865. [DOI] [PubMed] [Google Scholar]
- 37.Zeremski M, Dimova RB, Zavala R, Kritz S, Lin M, Smith BD, et al. Hepatitis C virus-related knowledge and willingness to receive treatment among patients on methadone maintenance. J Addict Med. 2014;8:249–257. doi: 10.1097/ADM.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]